Abstract
Background:
Mesh hernia repair is one of the most frequently performed procedures in general surgery. Recently, use of the self-gripping mesh demonstrated a beneficial effect on postoperative pain in inguinal hernia repairs. However, in intra-abdominal placement, the use of this novel mesh requires greater laparoscopic skill and dexterity because of the mesh's tendency to fold and adhere to itself and to any surrounding tissues. We hypothesized that gel-like coverage of a self-gripping mesh with a water-soluble film would allow delaying the immediate surface adhesion of the mesh to the tissue, which may allow greater freedom and ease in mesh placement for laparoscopic surgeons.
Methods:
In this ex vivo animal study, gel-coated self-gripping mesh (ProGrip) was compared with a control uncoated mesh in bovine and porcine tissue specimens and assessed for dislodgement shear forces before and after dissolving of the gel.
Results:
Gel coating of the mesh reduced preperitoneal dislodgement forces in a porcine abdominal wall specimen by 81% (8.05 ± 0.66 vs 1.53 ± 0.82 N, P < .01). Dissolving the gel markedly increased the anchoring forces (10.62 ± 3.70 vs 1.53 ± 0.82 N, P < .0001), and after dissolving the gel, the mesh shear dislodgement forces were similar and noninferior to the control mesh (8.05 ± 0.66 vs 10.62 ± 3.70 N, P = NS).
Conclusions:
We believe that water-soluble gel coating does not impair the adhesive features of the self-gripping mesh and may simplify its use in open and laparoscopic procedures by allowing controlled activation of the self-gripping mechanism.
Keywords: Hernia repair, Self-gripping mesh, Biomechanical testing, Animal study, Biomaterials
INTRODUCTION
Mesh hernia repair is one of the most frequently performed procedures in general surgery.1 More than 1.2 million inguinal hernia operations are performed each year in the United States, Europe, and Australia,2–6 and >20 million hernias are estimated to be repaired annually worldwide.7 The use of mesh in hernia repair has reduced the recurrence rate by 50% to 75%.8 There are >50 different commercial varieties of mesh: polypropylene, polyglactin, polypropylene-polyglactin, β-D-glucan, titanium-coated polypropylene, polypropylene-poliglecapron, polytetrafluoroethylene, collagen, and so on.
The past decade has seen rapid growth in laparoscopic mesh repair of inguinal hernias. Laparoscopic repair is a commonly recommended procedure for recurrent and bilateral inguinal hernias and is used successfully also in unilateral inguinal hernia repair.9 The laparoscopic approach is characterized by less postoperative pain and a quicker recovery.10 Postsurgical complications include hernia recurrence and chronic postoperative pain, which partially correlate with the dissection technique, the mesh type, and mainly the technique of mesh fixation.11–14
In recent years, a novel self-gripping mesh made of lightweight polyester and polylactic acid containing microgrips has become commercial and is indicated for inguinal hernia repair. Kapischke et al15 demonstrated its beneficial effect on postoperative pain in Lichtenstein-type open hernia repairs, and recently, several research teams have shown favorable results in transabdominal preperitoneal (TAPP) laparoscopic hernia repair using the ProGrip self gripping mesh (Covidien, Dublin, Ireland).16–18 However the use of this novel mesh requires greater laparoscopic skill and dexterity because of the rapid adhesive qualities of the mesh.
We hypothesized that gel-like coverage of the Parietene ProGrip mesh with a water-soluble film would allow controlled delay in the immediate surface adhesion of the mesh to the tissue. We decided to examine the ease of use and adherence efficacy of gel-covered self-gripping mesh on bovine myofascial tissue and porcine abdominal wall, which might allow greater understanding of possible clinical applications in general hernia repair and in laparoscopic hernia surgery in particular.
MATERIALS AND METHODS
Gel Preparation
Gelatin film was prepared by dissolving 28 g of purified gelatin (bovine) in 120 mL water at 80°C.
Mesh Preparation
Four quadrangular identical pieces of ProGrip mesh (55 × 60 mm) were prepared. Three pieces were covered with the heated liquid gelatin (approximately 1.5 mm) and left to cool and solidify.
Bovine Tissue Preparation
A fresh myofascial specimen from the paravertebral region was resected and sized to 200 × 100 mm. The specimen contained muscle, fat tissue, and fascia.
Porcine Abdominal Wall Preparation
A fresh abdominal wall specimen was resected, ex vivo, from a female pig, domestic breed (large white X Landrace, Sus scrofa domestica). The specimen contained all layers of the abdominal wall, including muscle, fat tissue, and fascia. The peritoneal layer was removed using blunt and sharp dissection with a No. 20 scalpel blade (Figure 1), after which a 400 × 300 mm preperitoneal surface was exposed.
Figure 1.
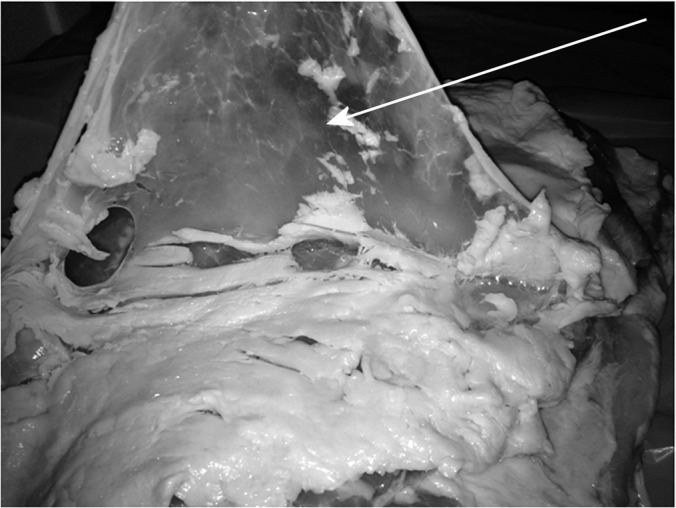
Preparation of porcine abdominal wall specimen: removal of peritoneal layer.
Mechanical Force Testing
For the bovine tissue, mesh pieces were placed on the fascial surface. For the porcine tissue, mesh pieces were placed preperitoneally on the porcine abdominal wall. Dislodgement shear force (DSF) was defined as the maximal applicable force before the initiation of movement. DSF was measured using a Mark-10 dynamometer (50 × 0.02 N) (BG Series; Mark-10 Corporation, Copiague, NY).
Mesh Dissolution
After DSF measurement, the gel film from the gel-coated mesh pieces was dissolved by irrigating 15 mL of saline solution warmed to 37°C. Fixation of the mesh was achieved by gently pressing the mesh against the underlying tissue. After mesh fixation, DSF measurement was repeated.
Data Acquisition and Statistical Analysis
DSF measurements were repeated approximately 3 consecutive times for each of the mesh pieces in each tissue type. Six measurements were recorded for the control meshes, 16 measurements for the gel-coated meshes, and 15 measurements for the dissolved-gel meshes. Ease and quickness of use were also qualitatively assessed and recorded. Data were analyzed with the R Language and Environment for Statistical Computing version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria). Continuous data are expressed as mean ± SD. Continuous data were compared by using Mann-Whitney U tests. P values < 0.05 was defined as significant.
RESULTS
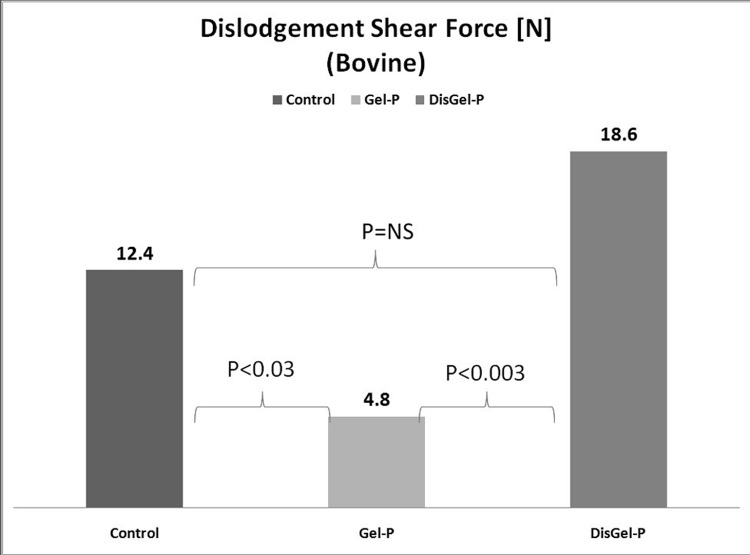
Institutional review board bioethics approval was obtained before commencement of the study. Mesh pieces and tissue specimens were prepared as previously specified. Analysis of the results from the bovine specimen revealed that gel coating of the mesh reduced dislodgement forces by 61% (12.39 ± 2.16 vs 4.76 ± 2.17 N, P < .03). Dissolving the gel markedly increased the DSF (18.60 ± 4.56 vs 4.76 ± 2.17 N, P < .003), and after dissolving the gel, the DSFs were similar and noninferior to the control mesh (12.39 ± 2.16 vs 18.60 ± 4.56, P = NS). A summary of these results is presented in Figure 2.
Figure 2.
Dislodgement shear force measurement in bovine myofascial specimen (control vs gel-covered [Gel-P] vs dissolved gel [DisGel-P]).
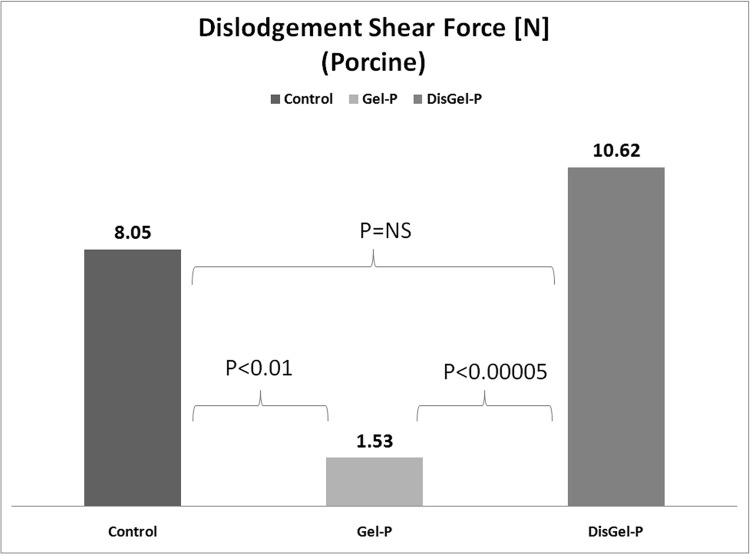
Analysis of the results from the porcine abdominal wall specimen revealed that gel coating of the mesh reduced dislodgement forces by 81% (8.05 ± 0.66 vs 1.53 ± 0.82, P < .01). Dissolving the gel markedly increased the DSF (10.62 ± 3.70 vs 1.53 ± 0.82 N, P < .0001), and after dissolving the gel, the DSFs were similar and noninferior to the control mesh (8.05 ± 0.66 vs 10.62 ± 3.70 N, P = NS). A summary of these results is presented in Figure 3.
Figure 3.
Dislodgement shear force measurement in porcine abdominal wall (control vs gel-covered [Gel-P] vs dissolved gel [DisGel-P]).
DISCUSSION
Hernia recurrence and chronic postoperative pain are the most common complications after hernia repair.19 Suitable mesh selection, accurate mesh placement, and prevention of mesh migration have been noted as factors affecting the recurrence of hernia.20 However, the technique of mesh fixation remains controversial because it has been demonstrated that pain after laparoscopic inguinal hernia repair is a significant problem that might be associated with the type of fixation.21 Recent studies have shown that mesh fixation with metal tacks results in increased rates of chronic postoperative pain, and some support the use of fibrin glue as an adhesive for mesh fixation.13,14
In view of these challenges, the 2008 introduction of the ProGrip self-gripping mesh was a welcome event. However, the use of this mesh in laparoscopic inguinal hernia repair has so far been limited to TAPP repair and requires greater dexterity and manual skill than the use of regular mesh. According to Birk et al,18 because of the self-gripping qualities of the ProGrip mesh, it folds and attaches to itself when inserted through the trocar and requires disentanglement and straightening to avoid mesh folding or twisting during placement.
In this study, we set out to modulate the self-gripping design of the ProGrip mesh to transform it into an easily applicable mesh for totally extraperitoneal and TAPP repairs. This was achieved by using a thin, water-soluble gel coating to limit the contact of the tissue with the microgrip surface.
This study's results show that tissue adhesion was markedly lowered by the gel coating and that removal of the gel allowed the mesh to regain full self-gripping abilities without any reduction compared with the control mesh. Further in vivo trials (open and laparoscopic) are needed to assess the clinical relevance of this model. If these trials prove efficacious, use of this modification to TAPP hernia repair can allow the surgeon to preoperatively prepare the gel film coating, roll and insert the mesh through the trocar, easily place the mesh on the exposed preperitoneal window, dissolve the mesh with warmed saline, and close the peritoneal flap. A similar procedure may be used in totally extraperitoneal hernia repair, without need for tacks or glue.
Our study was preliminarily designed to assess control of the mesh's self-gripping ability, which has been implicated as a causative factor in the difficult operative handling of the mesh. Although critical for clinical assessment, operative ease of use in the laparoscopic setting was not an end point of our study, because of the obvious addition of biasing factors, and future studies assessing the laparoscopic use of our modification of the self-gripping mesh are warranted. Although more tests are needed for in vivo evaluation of this mesh in TAPP and totally extraperitoneal repairs, as well as histologic assessment of tissue response to the mesh, we believe this modification holds great promise and certainly merits further testing.
CONCLUSIONS
Water-soluble gel coating significantly decreases attachment forces of the ProGrip mesh and does not impair self-gripping properties after dissolving of the gel. This technology may simplify the use of self-gripping mesh in open and laparoscopic hernia repair by controlling the time of activation of the self-gripping properties of the mesh. Further in vivo studies are required to assess the full impact of this technology.
Acknowledgments
The authors wish to thank the Lahav CRO (Kibbutz Lahav, Israel) and Mr Ofer Doron for assistance in donating the porcine specimen.
Contributor Information
Avinoam Nevler, Department of Surgery and Transplantation, Chaim Sheba Medical Center, Tel-Hashomer, Israel (affiliated to the Sackler School of Medicine, Tel-Aviv University, Tel-Aviv, Israel); The Dr. Pinchas Borenstein Talpiot Medical Leadership Program 2012, Chaim Sheba Medical Center, Tel-Hashomer, Israel..
Mordechai Gutman, Department of Surgery and Transplantation, Chaim Sheba Medical Center, Tel-Hashomer, Israel (affiliated to the Sackler School of Medicine, Tel-Aviv University, Tel-Aviv, Israel).
Alexander Lebedyev, Department of Surgery and Transplantation, Chaim Sheba Medical Center, Tel-Hashomer, Israel (affiliated to the Sackler School of Medicine, Tel-Aviv University, Tel-Aviv, Israel).
References:
- 1. Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83(5):1045–1051. [DOI] [PubMed] [Google Scholar]
- 2. Schumpelick V, Treutner KH, Arlt G. Inguinal hernia repair in adults. Lancet. 1994;344(8919):375–379. [DOI] [PubMed] [Google Scholar]
- 3. Kingsnorth AN, Gray MR, Nott DM. Prospective randomised trial comparing the Shouldice technique and plication darn for inguinal hernia. Br J Surg. 1992;79:1068–1070. [DOI] [PubMed] [Google Scholar]
- 4. Levard H, Boudet MJ, Hennet H, Hay JM. Inguinal hernia repair: a prospective multicentre trial on 1706 hernias. Br J Surg. 1996;83(Suppl 2):72.8653371 [Google Scholar]
- 5. Geissler B, Anthuber M. Chirurgie der Leisten- und Schenkelhernien [Inguinal and femoral hernia repair]. Chirurg. 2011;82(5):451–64. [DOI] [PubMed] [Google Scholar]
- 6. Smart P, Castles L. Quantifying the cost of laparoscopic inguinal hernia repair. ANZ J Surg. 2012;82(11):809–812. [DOI] [PubMed] [Google Scholar]
- 7. Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. 362(9395):1561–1571. [DOI] [PubMed] [Google Scholar]
- 8. Scott N, Go PM, Graham P, McCormack K, Ross SJ, Grant AM. Open mesh versus non-mesh for groin hernia repair. Cochrane Database Syst Rev. 2001;(3):CD002197. [DOI] [PubMed] [Google Scholar]
- 9. Bisgaard T, Bay-Nielsen M, Kehlet H. Re-recurrence after operation for recurrent inguinal hernia: a nationwide 8-year follow-up study on the role of type of repair. Ann Surg. 2008;247:707–711. [DOI] [PubMed] [Google Scholar]
- 10. McCormack K, Scott N, Go PM, Ross SJ, Grant A, Collaboration the EU Hernia Trialists. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003;(1):CD001785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schopf S, von Ahnen T, von Ahnen M, Schardey H. Chronic pain after laparoscopic transabdominal preperitoneal hernia repair: a randomized comparison of light and extralight titanized polypropylene mesh. World J Surg. 2011;35:302–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sajid MS, Leaver C, Baig MK, Sains P. Systematic review and meta-analysis of the use of lightweight versus heavyweight mesh in open inguinal hernia repair. Br J Surg. 2012;99:29–37. [DOI] [PubMed] [Google Scholar]
- 13. Brügger L, Bloesch M, Ipaktchi R, Kurmann A, Candinas D, Beldi G. Objective hypoesthesia and pain after transabdominal preperitoneal hernioplasty: a prospective, randomized study comparing tissue adhesive versus spiral tacks. Surg Endosc. 2012;26:1079–1085. [DOI] [PubMed] [Google Scholar]
- 14. Fortenly RH, Petter-Puchner AH, May C, et al. The impact of atraumatic fibrin sealant vs staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc. 2012;26:249–254. [DOI] [PubMed] [Google Scholar]
- 15. Kapischke M, Schulze H, Caliebe A. Self-fixating mesh for the Lichtenstein procedure—a prestudy. Langenbecks Arch Surg. 2010;395(4):317–322. [DOI] [PubMed] [Google Scholar]
- 16. Kosai N, Sutton PA, Evans J, Varghese J. Laparoscopic preperitoneal mesh repair using a novel self-adhesive mesh. J Minim Access Surg. 2011;7(3):192–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fumagalli Romario U, Puccetti F, Elmore U, Massaron S, Rosati R. Self-gripping mesh versus staple fixation in laparoscopic inguinal hernia repair: a prospective comparison. Surg Endosc. 2013;27:1798–1802. [DOI] [PubMed] [Google Scholar]
- 18. Birk D, Hess S, Garcia-Pardo C. Low recurrence rate and low chronic pain associated with inguinal hernia repair by laparoscopic placement of Parietex ProGrip™ mesh: clinical outcomes of 220 hernias with mean follow-up at 23 months. Hernia. In press. [DOI] [PubMed] [Google Scholar]
- 19. Pokorny H, Klinder A, Schmid T, et al. Recurrence and complications after laparoscopic versus open inguinal hernia repair: results of a prospective randomized multicenter trial. Hernia. 2008;12(4):385–389. [DOI] [PubMed] [Google Scholar]
- 20. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc. 2011;25(9):2773–2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dickinson KJ, Thomas M, Fawole AS, Lyndon PJ, White CM. Predicting chronic post-operative pain following laparoscopic inguinal hernia repair. Hernia. 2008;12(6):597–601. [DOI] [PubMed] [Google Scholar]