Abstract
“Bath salts” are synthetic stimulant “legal highs” that have recently been banned in the U.S. Epidemiological data regarding bath salts use are limited. In the present study, 113 individuals in the U.S. reporting use of bath salts completed an anonymous, online survey characterizing demographic, experiential, and psychological variables. Respondents were more often male, 18–24 years old, and Caucasian/white with some college education. Past year use was typically low (≤ 10 days), but marked by repeated dosing. Intranasal was the most frequently reported administration route and subjective effects were similar to other stimulants (e.g., cocaine, amphetamines). Bath salts use was associated with increased sexual desire and sexual HIV risk behavior, and met DSM-5 diagnostic criteria for disordered use in more than half of respondents. Bath salts use persists in the U.S. despite federal bans of cathinone-like constituents. Self-reported stimulant-like effects of bath salts suggest their use as substitutes for traditional illicit stimulants. Data revealed more normative outcomes vis-à-vis extreme accounts by media and medical case reports. However, indications of product abuse potential and sexual risk remain, suggesting bath salts pose potential public health harm.
Keywords: Bath salts, synthetic cathinones, mephedrone, MDPV, sexual risk
Introduction
“Bath salts” are synthetic stimulants similar to cathinones that have recently gained attention as “legal highs” (Vandrey et al. 2013). These products are not used as bath water additives. Rather, they are labeled as “bath salts” and other terms (e.g., “plant food,” “glass cleaner”) to conceal their use as drugs. Among the most common psychoactive constituents of bath salts are mephedrone, methylone, and methylenedioxypyrovalerone (MDPV), which are amphetamine-like derivatives of the naturally occurring stimulant cathinone (present in Catha edulis; khat). Beginning in 2010, the frequency of bath salts use in the U.S. increased rapidly (Yin & Ho 2012), resulting in a concomitant increase in local poison control center calls and emergency department toxicity presentations (Warrick et al. 2013; Wood 2013; Forrester 2012; Bronstein et al. 2011). In response, the U.S. Drug Enforcement Administration (DEA) temporarily classified the aforementioned constituents as Schedule I controlled substances in October 2011. In July 2012, Congress passed the Synthetic Drug Abuse Prevention Act, retaining mephedrone and MDPV in Schedule I; the DEA permanently placed methylone in Schedule I as of April 2013. However, as is characteristic of the legal high industry, novel second generation compounds have since been introduced to circumvent legislation (Rosenbaum, Carreiro & Babu 2012; De Paoli, Maskell & Pounder 2011; Spiller et al 2011).
Cathinone-like compounds found in bath salts elicit a variety of sympathomimetic responses via their activity at brain sites regulating monoamine release and transport (Baumann et al. 2013; Cameron et al. 2013; Eshleman et al. 2013; Simmler et al. 2013; López-Arnau et al. 2012). Behavioral assays conducted in nonhuman models show increased locomotor activity, tachycardia, and hypertension (Baumann, Partilla & Lehner, 2013; Fantegrossi et al. 2013; Gatch, Taylor & Forster 2013; Marusich et al. 2012), a profile of symptoms that is largely consistent with clinically reported intoxication in humans (Warrick et al. 2013; Murphy et al. 2013; Prosser & Nelson 2012; Ross et al. 2012). Perhaps one of the most important findings in this literature is that cathinone-like compounds serve as potent reinforcers and are readily self-administered, indicating a high likelihood of abuse liability (Aarde et al. 2013; Motbey et al. 2013; Watterson, Hood et al. 2012; Watterson, Kufahl et al. 2012).
Despite the potential dangers posed by bath salts, epidemiological data regarding their use are limited, a fact that is perhaps not surprising given the clandestine nature of their use and questionable legal status. One methodological approach to collecting these data is to conduct online user surveys, a strategy employed for predominantly European samples (Carhart-Harris, King & Nutt 2011; Winstock, Mitcheson, Deluca et al. 2011) to characterize mephedrone, the cathinone-like compound most prevalent in Europe (Wood & Dargan 2012). A thoroughgoing examination of bath salts use in the U.S. is timely because, compared to Europe, relatively less is known about these substances and the nature of their effects. Furthermore, quantitative analyses of bath salts ingredients have found that MDPV is more common than mephedrone in U.S. samples, suggesting that geographic differences are non-trivial (Shanks et al. 2012; Spiller et al. 2011). While recent U.S.-based surveys of drug use have included items pertaining to bath salts, their results were confined to prevalence estimates (Johnston et al. 2014; Johnston et al. 2013; Kelly et al. 2013; Stogner & Miller 2013). Our goal was to characterize through an online survey the demographic, experiential, and psychological variables present among U.S.-based adult bath salts users.
Methods
An online survey hosted by SurveyMonkey.com was available between December 11, 2012 and April 9, 2013. Respondents were recruited via drug-related (www.bluelight.ru, www.drugs-forum.com, www.reddit.com/r/drugs) and volunteer-opportunity oriented (www.craigslist.org) websites. Participation was voluntary, anonymous (no name or IP address recorded), and uncompensated. This implied consent study was approved by the Johns Hopkins University Institutional Review Board.
The survey featured 91 questions about demographics, bath salts use patterns, procurement, subjective effects, use disorders for bath salts and other substances, and beliefs regarding the safety and legality of bath salts (survey available from first author on request). Respondents were allowed to skip questions if they felt uncomfortable answering, could not accurately recall, or did not know the answer. Respondents were able to access the survey if they were at least 18 years of age, were fluent in English, currently resided in the U.S., had previously used bath salts, were not currently under the influence of bath salts, and had not completed the survey previously.
Data analysis
For most survey items, descriptive statistics (e.g., percent, mean, standard deviation) were used to characterize respondent data. In a section querying bath salts effects, respondents were asked, with respect to their most frequent route of administration, to estimate the time until onset of drug effects, peak effects, and resolution of drug effects following administration. For these data, medians and interquartile ranges were calculated. For an assessment of behavioral economic demand for bath salts, respondents were asked how many milligrams of their preferred bath salts would be hypothetically purchased at a series of prices per milligram (USD). Respondents were instructed to purchase only amounts they would personally use within the next month, with potential responses ranging from 0 to 499 mg. Median amounts purchased were plotted as a function of price and fitted by an exponential demand equation (Hursh & Silberberg 2008) using GraphPad Prism version 6.03 for Windows (GraphPad Software, La Jolla, CA). Finally, criteria for DSM-5 substance use disorders for a range of drugs were assessed using a modified checklist (Hudziak et al. 1993). Diagnoses were determined according to DSM-5 guidelines (American Psychiatric Association 2013).
Results
Sample size and demographic information
One hundred and sixteen respondents met inclusion criteria and completed the survey. Three individuals who reported exclusive use of a non-cathinone-like compound (e.g., 2C-I) were excluded, resulting in a sample size of 113. Although respondents were allowed to skip questions, they did so infrequently (the median response count per question was n = 111). Nonetheless, percent calculations were based on the response count for each question. The average participation duration was approximately 22 minutes (SD ≈ 9 min.).
Table 1 shows respondent demographics. Respondents were typically male (68%), 18–24 years old (50%), Caucasian/white (92%), and non-Hispanic (87%). They were most likely to have at least some college education (65%), to never have been married (72%), to earn less than $30,000 annually (46%), and to work full-time (44%). Less than one quarter reported a lifetime psychiatric diagnosis (23%). Respondents were from 37 states and the District of Columbia.
Table 1.
Demographic information
| Characteristic | Response Count (%) |
|---|---|
| Sex (n = 111) | |
| Male | 75 (68) |
| Female | 36 (32) |
| Age (years; n = 113) | |
| 18–24 | 57 (50) |
| 25–30 | 33 (29) |
| 31–40 | 18 (16) |
| > 40 | 5 (4) |
| Race (n = 112) | |
| Caucasian/White | 103 (92) |
| Asian | 2 (2) |
| Native American | 2 (2) |
| Mixed | 4 (4) |
| Prefer not to answer | 1 (1) |
| Ethnicity (n = 109) | |
| Non-Hispanic | 95 (87) |
| Hispanic | 12 (11) |
| Prefer not to answer | 2 (2) |
| Education (years; n = 113) | |
| 9–12 | 27 (24) |
| 13–16 | 74 (65) |
| > 16 | 12 (11) |
| Marital status (n = 113) | |
| Never married | 81 (72) |
| Married | 16 (14) |
| Remarried | 1 (1) |
| Separated | 3 (3) |
| Divorced | 12 (11) |
| Household income (past year in dollars; n = 111) | |
| < $30,000 | 51 (46) |
| $30,000–$60,000 | 24 (22) |
| $61,000–$100,000 | 19 (17) |
| > $100,000 | 17 (15) |
| Employment status (n = 113) | |
| Full-time (≥ 35 hours/week) | 50 (44) |
| Part-time (< 35 hours/week) | 18 (16) |
| Student | 24 (21) |
| Retired/Disabled | 5 (4) |
| Unemployed | 16 (14) |
| Psychiatric diagnosis in lifetime? (n = 113) | |
| Yes | 26 (23) |
| No | 87 (77) |
Note. Parenthetical values represent the percent of respondents and may not sum to 100 due to rounding.
Procurement and availability
Bath salts were most commonly procured via the Internet (28%) and from “head” shops (27%), but were also obtained from drug dealers (15%), gas stations/convenience stores (14%), friends/relatives (12%), or other locations such as tattoo shops (4%). Sixty-four respondents (57%) reported that a ban was currently in place, while 35% and 8% endorsed “I don’t know” and “no,” respectively. Among those respondents reporting a ban (n = 64), 53% reported that bath salts were harder to obtain because of the ban. Also among those reporting a ban (n = 64), 53% reported having used bath salts in the post-ban period. Of those who reported post-ban use (n = 34), 38% did not notice whether the drug quality was the same or different as before the ban, while others reported that the drug quality was the same as before the ban (35%) or that the drug quality had decreased since the ban (26%). None reported that the drug quality increased after the ban.
Frequency of use
Among all respondents (N = 113), 26% reported no use of bath salts in the past year. Of those who reported use in the past year (n = 84), 62%, 26%, and 12% of respondents reported using bath salts on ≤ 10 days (62%), 11–30 days (26%), and > 30 days (12%). We also asked how many times the drug was administered on a typical day when used. Among those reporting past year use (n = 84), 22% reported use only once daily, 54% reported 2–5 administrations, 21% reported 6–20 administrations, and 4% reported > 20 administrations. Reported use over the past month and past week was low among all respondents (N = 113), as 84% reported no use in the past month and 94% reported no use in the past week. Of those respondents who used bath salts at least once during these more recent time periods, the distribution of uses per day was consistent with estimates from administrations over the past year.
For the remaining items in this section, respondents were instructed to skip questions if they were unfamiliar with the unit of measure (milligrams). When asked to estimate the average and greatest amounts of bath salts consumed on a typical day when the drug was used, 58 respondents provided data. Of these 58 respondents, 14% reported using ≤ 5 mg, 19% used 6–20 mg, 26% used 21–100 mg, and 41% used > 100 mg. Regarding greatest amount used, the 54 respondents completing this item used a maximum of ≤ 5 mg (15%), 6–20 mg (15%), 21–100 mg (22%), and > 100 mg (48%).
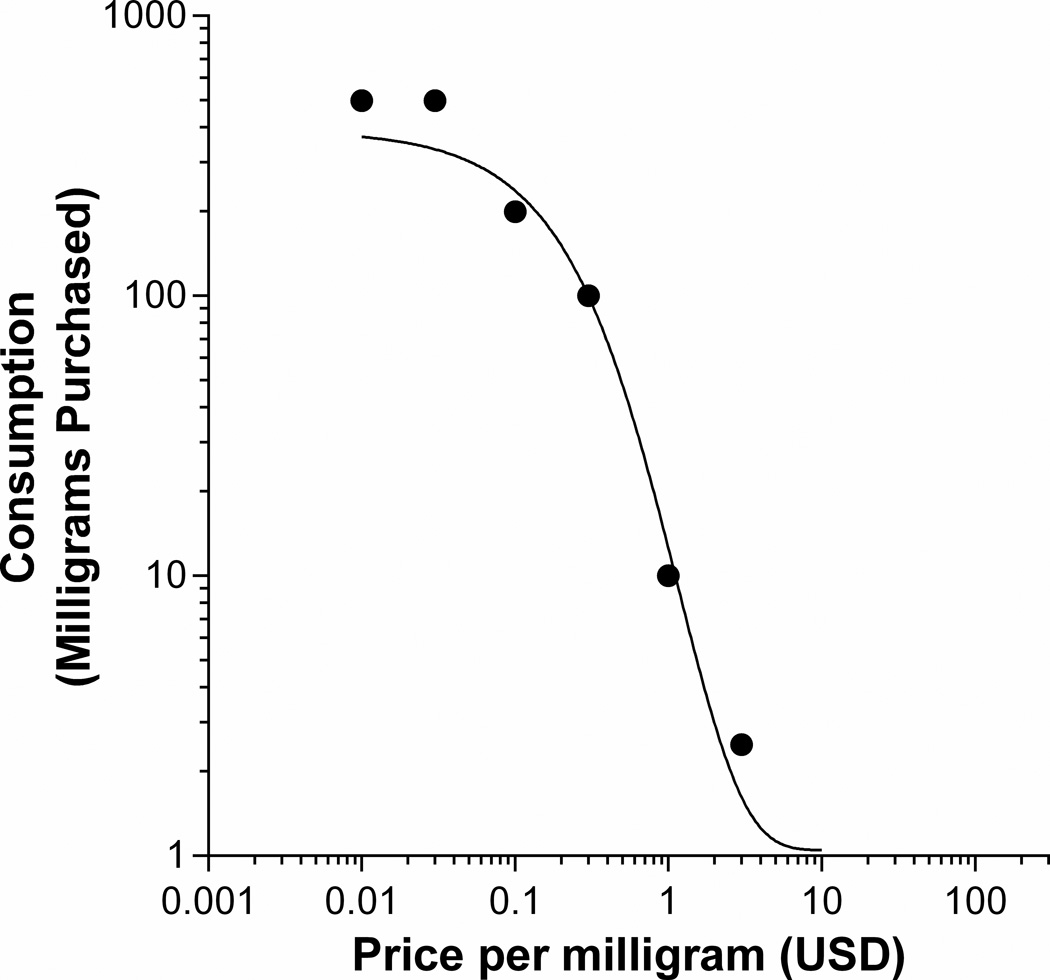
Figure 1 shows data from the assessment of behavioral economic demand for bath salts. Of the 66 individuals who responded in this section, 36 (55%) provided answers for every price, and provided non-zero values at $0.01/mg. Only data from these 36 respondents were analyzed. Median consumption, which decreased with price, was well-described by an exponential demand equation (R2 = .99).
Figure 1.
Economic demand for preferred bath salts product (n = 36). Data plotted on log-log axes are medians of milligrams purchased hypothetically at each of the prices shown on the x-axis. USD = United States dollars.
Use patterns
For all respondents (N = 113), the most popular route of administration was intranasal (i.e., snorting, 71%). Smoking/vaporizing (11%) and oral routes (15%) were not uncommon.
Among those who reported whether they used bath salts alone or with others (n = 110), 56% used with one or two close friends or relatives, 22% reported using by oneself, 18% reported using in large gatherings, and 4% reported using under other circumstances such as when bath salts were assumed to be another drug (e.g., MDMA).
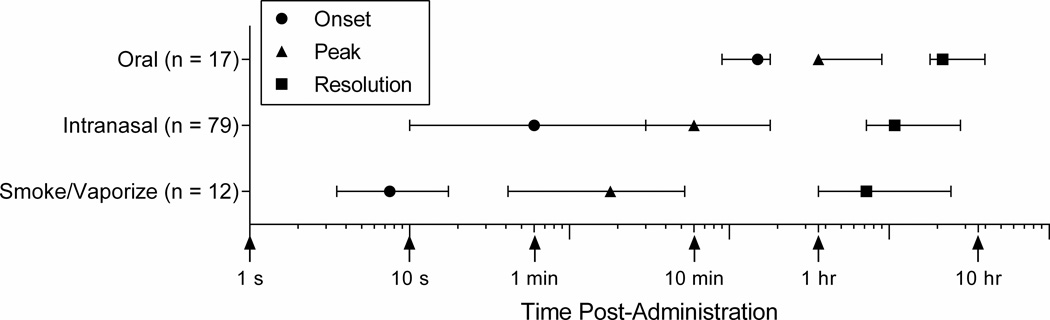
Figure 2 shows median estimated time to onset, peak effects, and resolution of drug effects for select primary routes of administration. Of the routes shown (i.e., those endorsed by ≥ 10 respondents), onset was most rapid for smoking/vaporizing (7.5 s), followed by intranasal (1 min), and least rapid for oral administration (25 min). Median time to peak drug effects was ordered identically: smoking/vaporizing (3 min), intranasal (10 min), and oral administration (1 hr). Depending on route of administration, bath salts effects were reported to resolve completely as early as 1 hr post-administration and, in some cases, as long as 10 hr.
Figure 2.
Estimated time to onset, peak effects, and resolution of bath salts effects for select primary routes of administration. Data are medians with error bars representing the interquartile range. Note the logarithmic x-axis, which plots time post-administration in seconds but features important intervals of the time course.
Among all respondents (N = 113), 79% reported using bath salts because they were curious or wanted to try them. Other reasons included using bath salts to help stay awake (22%), to improve sexual experience (21%), to avoid positive drug tests (26%), to explore the mind/brain (52%), and because the respondent liked the effect (53%).
Subjective effects
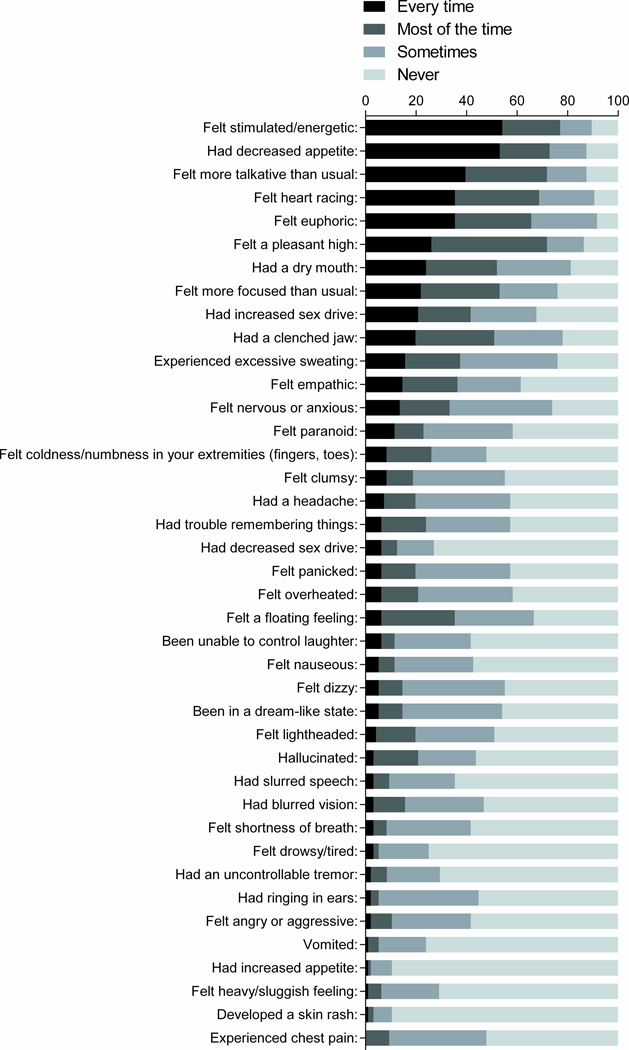
Figure 3 illustrates subjective effects of bath salts. The percent of respondents endorsing each of the four frequency categories was calculated using as the denominator the total number of respondents who responded to every subjective effect item (n = 96). Feeling stimulated or energetic (54%) and having a decreased appetite (53%) were the only two items that > 50% of respondents reported occurring every time bath salts were used. At least half of those who responded to every subjective effect item (n = 96) endorsed feeling more talkative than usual (72%), feeling a pleasant high (72%), feeling their heart racing (69%), feeling euphoric (66%), feeling more focused than usual (53%), having a dry mouth (52%), and having a clenched jaw (52%) as occurring at least “most of the time.” Notably, 42% reported having increased sex drive at least “most of the time.” By comparison, psychotic-like effects were less commonly reported. Less than one quarter felt paranoid (23%) or hallucinated (21%), and 15% reported being in a dream-like state “every time” or “most of the time” bath salts were used.
Figure 3.
Subjective effects reported following administration of bath salts. Items are sorted in descending order according to the percentage of respondents endorsing “every time” for a given subjective effect.
Respondents were also asked to specify drugs with subjective effects very similar to those of bath salts. Among those who responded to this item (n = 107), amphetamines (e.g., Adderall®) were endorsed the most (65%). Similarly, cocaine, MDMA, methamphetamine, and methylphenidate (e.g., Ritalin®) were specified by 58%, 53%, 41%, and 26% of respondents, respectively.
Violence and sexual risk
When asked about urges to engage in violent behavior (N = 113), 78% reported never having felt the urge to be more violent than normal after using bath salts. However, 16% reported that they had felt the urge to be more violent, but had not acted on the urge, and only one respondent (< 1%) reported that they had acted on the urge to be more violent. No respondents reported engaging in self-injury, attempting suicide, becoming violent toward an animal, or engaging in cannibalism.
Among all respondents (N = 113), 54% reported having felt the urge to take more sexual risks than normal after using bath salts. Of those (n = 61), 48% reported acting on this urge. All of the items in the follow-up question specifying sexual risk behaviors were endorsed by at least one respondent.
Other drug use and prevalence of substance use disorders
Among all respondents (N = 113), other drugs used in the past year were most often alcohol (95%), marijuana (85%), and tobacco (73%). Other drugs used by fewer respondents included amphetamines (54%), hallucinogens (54%), and prescription pain relievers (53%).
Prevalence of substance use disorders (American Psychiatric Association 2013) for bath salts and other drugs was assessed for respondents endorsing at least 1 criterion across all drugs or indicating “no additional drug use” (n = 111). Of these respondents, 53% (n = 59) met criteria for a substance use disorder related to “bath salts” use. Of the 59, 37%, 24% and 39% met criteria for mild, moderate, and severe substance use disorder, respectively. Eighty-one respondents endorsed the occurrence of at least one withdrawal symptom upon cutting down or stopping use of bath salts, the most common of which were desire or craving to use bath salts (54%), fatigue (52%), and depression (52%). Among all respondents, only 3% reported seeking or receiving treatment for problems related to bath salts.
Of 112 respondents who endorsed at least 1 DSM-5 substance use disorder criterion for drugs other than bath salts, at least one respondent met criteria for at least a mild substance use disorder for each of the other drugs assessed. Marijuana, endorsed by 21% of respondents, was the drug (excluding bath salts) associated with the most frequent mild substance use disorder diagnoses. Both the most moderate and severe substance use disorder diagnoses were associated with alcohol, with 15% and 22% of respondents, respectively, meeting criteria. Respondents were asked if they had ever received treatment for drug or alcohol problems: 29% reported they had received treatment, and the modal number of separate treatment occasions was 1.
Beliefs regarding bath salts
When asked to rate the accuracy of media representations of bath salts as it relates to the average user’s experience (0 = not accurate at all, 10 = extremely accurate), the average perceived accuracy was 1.99 (SD = 2.02). The majority of respondents (86%) agreed most with the statement that media representations were exaggerated (consequences less severe than portrayed). Conversely, 14% agreed most with the statement that media representations were understated (consequences more severe than portrayed).
When asked to rate the risk of people harming themselves or others when using bath salts (0 = no risk, 10 = extreme risk), respondents rated the average risk as 5.28 (SD = 2.78). Few respondents (13%) believed that bath salts are approved for human use, 19% believed that bath salts are safe for human use, 90% believed that bath salts are potentially dangerous or harmful if used, and 11% believed that if bath salts were not safe to use, they would not be sold commercially. Based on their firsthand experiences, 94% agreed that bath salts produce a noticeable “high” or feeling of intoxication, 51% agreed that bath salts produce an effect that is different than any other legal or illegal drug they have tried, and 71% agreed that using the same bath salts results in generally the same effect every time the product is used. Regarding the overall quality of their experiences, 80% reported positive/enjoyable effects after using bath salts, and 68% reported negative/unwanted effects.
When asked about the legal status of bath salts, 35% agreed that bath salts should be illegal; 23% agreed that bath salts should be legal, but available only for adult use; 37% agreed that bath salts should be legal, but subject to standard quality control and regulation guidelines; and 4% agreed that bath salts should be legal and available to anyone to use without any restrictions such as age. Overall, 47% of respondents reported that their current opinion of bath salts was that they did not like them, and although they had tried them in the past, they do not plan to use them in the future. Less than a quarter (23%) endorsed the opinion that bath salts are acceptable substitutes when respondents do not have access to other more preferred drugs. Respondents endorsing this opinion were asked to specify for which drugs bath salts substitute. For 22 who responded, the five most common were all stimulants: cocaine (59%), MDMA (59%), amphetamines (50%), methamphetamine (32%), and methylphenidate (18%).
Discussion
This online survey is the first to our knowledge to address the paucity of data surrounding the use of bath salts in a U.S.-based sample. We identified several important demographic, economic, psychological, behavioral, and cultural features of this obscure drug-using population. Collectively, our data describe a drug profile with remarkable similarity to classic dopaminergic psychomotor stimulants with corresponding abuse potential. These data include subjective effects of stimulation, decreased appetite, and increased sex drive; subjective similarity to other stimulants; binging patterns; and sexual risk behavior. Also consistent with a stimulant profile, the data suggest potential positive effects including improved concentration (e.g. as in the treatment of ADHD) and the ability to stay awake (e.g., as in the treatment of narcolepsy), consistent with the therapeutic use of amphetamine-like stimulants.
Previous survey-based characterizations of cathinone-like compound use beyond basic prevalence estimates have focused on predominantly European samples and mephedrone specifically (Carhart-Harris et al. 2011; Winstock, Mitcheson, Deluca et al. 2011). However, bath salts users in our U.S.-based sample were comparable to European mephedrone users along a number of dimensions including sex (predominantly male), age (predominantly early- to mid-twenties), and preferred administration route (predominantly intranasal). This demographic profile is also identical to clinical presentations of bath salts toxicities to emergency departments and poison control centers in the U.S. (Warrick et al. 2013; Wood 2013; Forrester 2012; Bronstein et al. 2011).
Nationwide efforts to criminalize mephedrone in the United Kingdom resulted in decreased procurement and use likelihood without noticeable changes in availability (Carhart-Harris et al. 2011). By contrast, respondents in our survey reported decreased availability of bath salts following the implementation of bans without any apparent decrease in likelihood of use (51% of respondents reported having used these products after the ban was in place). While the decreased commercial presence of bath salts may reflect the reluctance of U.S. brick-and-mortar retailers (e.g., head shops, gas stations) to continue selling them, the lack of respondent compliance with the ban is suggestive of a reallocation of supply to online marketplaces (e.g., Silk Road; Barratt 2012), making law enforcement difficult or impossible to maintain.
Respondents reported using on a low number of days, but also reported multiple administrations on these occasions. Repeated dosing may promote acute tolerance, thereby motivating compulsive use of the drug. This pattern of administration is consistent with binge use (O’Brien 2011) and has been documented elsewhere in association with mephedrone (Winstock, Mitcheson, Ramsey et al. 2011). This pattern may also explain the average respondent in the present study consuming in excess of 100 mg of bath salts per occasion. Binge use is typical of other psychomotor stimulant drugs of abuse such as cocaine and methamphetamine. Ultimately, drug administration rate is related to drug time course. For the most commonly reported route (snorting), peak effects of bath salts were estimated to occur after 10 minutes. Similarly, peak effects of intranasal cocaine and methamphetamine in human laboratory studies occur after 10–15 minutes (Hart et al. 2008; Volkow et al. 2000). Median reported effect onset was extremely rapid: 7.5 and 60 seconds for smoked/vaporized and intranasal routes of administration, respectively. This is clinically concerning given that a more rapid onset suggests higher abuse liability (Hatsukami & Fischman 1996). Strong reinforcing effects associated with rapid onset, combined with relatively long effect duration (~4 hours), suggests the potential for binging episodes accompanied by accumulating drug blood levels, which may be responsible for reports of psychoses following bath salts binges (Miotto et al. 2013; Penders, Gestring & Vilensky 2012; Thornton, Gerona & Tomaszewski 2012).
While the relation between cocaine and methamphetamine use and sexual risk behavior is established (Gonzales, Mooney & Rawson 2010; Brown, Domier & Rawson 2005; Hoffman et al., 2000; Bux, Lamb & Iguchi 1995; Booth, Watters & Chitwood 1993), the present study is the first to document this association as an under-emphasized risk of bath salts use. A majority of respondents felt the urge to take more sexual risks than normal after using bath salts and slightly less than half acted on their urge, suggesting transmission potential for HIV and other sexually transmitted infections. These findings are contrasted against the low prevalence of acting on violent urges (1%), despite the sensational and often gruesome content of recent U.S. news reports (e.g., erroneous attribution of cannibalism to bath salts in Miami, FL case; Martinez 2012). While most respondents agreed that media representations of bath salts use inaccurately portrayed the harms associated with use, a majority reported unwanted effects of bath salts and believed that bath salts were potentially dangerous and should be at least regulated or made illegal. Perhaps most telling was the finding that slightly less than half of respondents did not like bath salts despite having used them in the past and had no intention of future use.
Although the data are consistent with bath salts being a public health concern, the data also suggest more normative patterns and outcomes vis-à-vis extreme accounts by media and medical case reports which understandably tend to focus on extraordinary cases. The clinical prevalence of sexual risk relative to violence is in line with expectations of traditional dopaminergic stimulants like cocaine and methamphetamine. Similar to all drug classes, a non-trivial minority (33%) of users appeared to have moderate/severe use disorders (compare to dependence among extra-medical users in Anthony, Warner & Kessler 1994), suggesting many users regulate use. The demand curve analysis also indicates that bath salts use is typically lawful and, as with other drugs, is regulated by environmental factors such as price. These similarities notwithstanding, it should be acknowledged that we did not inquire in depth about legal (e.g., arrests) or some types of clinical (e.g., emergency department visits) consequences of bath salts use. It is also likely that the occurrence of psychotic-like effects of bath salts such as paranoia and hallucinations, while not typically reported in our survey, is related to the dose and specific compound administered and could be precipitated by a pre-existing psychiatric disorder in combination with drug use. Until additional data on these topics are collected, we recommend that caution be exercised in generalizing the present findings to bath salts use universally.
Several limitations should be considered. First, our sample was relatively small. As a result, the strength of our findings may lie in the systematic observations within our sample, rather than as a demographic characterization of the entire population of U.S. bath salts users. That is, within our survey, there were multiple opportunities to assess the internal validity of our results. For instance, estimates of the timecourse of bath salts effects were orderly for each route of administration (i.e., onset < peak effects < resolution). Between routes of administration, temporal features were similarly ordered, with more rapid onset following smoking/vaporizing relative to snorting and then swallowing. Second, some respondents were possibly regular members of drug-related fora with above-average drug knowledge. Given the online environment in which the survey was conducted, there may have also been the potential for selection bias in favor of younger, more technologically advanced users who may be more likely to obtain bath salts over the Internet than through alternative mediums (see Khey et al 2014). Third, web-based research, while efficient and cost-effective, is restricted in its ability to confirm response accuracy. Self-reports are also inevitably susceptible to memory deficits and so should be interpreted cautiously. A fourth limitation is that we allowed respondents to skip questions given the sensitivity of the topic. However, except in those cases in which respondents were directly encouraged to skip a question in the event of a knowledge deficit (e.g., unsure of dose), missing data were rare and did not affect interpretation of the results. Also, due to the lack of data regarding typical bath salts doses, maximum values of 100 and 499 mg were set for questions about daily use and hypothetical consumption, respectively. Respondents often endorsed maximum values, signaling that the accuracy of these estimates could have been improved by a wider range of possible values. Finally, we could have further probed positive effects. For example, amphetamine-like stimulants increase vigilance and arousal and are approved for ADHD and narcolepsy treatment. Therefore it is not implausible that constituents of bath salts might hold promise as therapeutic agents. While some respondents reported using bath salts to either help concentrate better or stay awake, it would have been valuable to describe the nature of these effects beyond their endorsement as reasons for use.
Despite these methodological concerns, the use of bath salts has significant implications for public health in the U.S. In lieu of human pharmacology and toxicology of cathinone-like compounds, clinicians and researchers may benefit from descriptive approaches like the one adopted here. Compared to other data collection methods, online surveys confer an information-gathering advantage in the characterization of novel legal highs and associated obscure user populations. The feasibility of alternative approaches designed to minimize bias and other threats to internal validity should be explored in future studies investigating legal high phenomena.
ACKNOWLEDGEMENTS
The authors thank Drs. Ryan Vandrey and Kelly Dunn for valuable resources and feedback. Forum moderators Tronica (www.bluelight.ru), Phenoxide (www.drugs-forum.com), and Borax (www.reddit.com/r/drugs) were invaluable regarding recruitment.
FUNDING
Funding for this study was provided by NIDA grants R01 DA032363, R21 DA032717, and T32 DA07209.
References
- Aarde SM, Huang PK, Creehan KM, Dickerson TJ, Taffe MA. The novel recreational drug 3.4-methylenedioxypyrovalerone (MDPV) is a potent psychomotor stimulant: self-administration and locomotor activity in rats. Neuropharmacology. 2013;71:130–140. doi: 10.1016/j.neuropharm.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Experimental and Clinical Psychopharmacology. 1994;2(3):244–268. [Google Scholar]
- Barratt MJ. Silk Road: eBay for drugs. Addiction. 2012;107(3):683. doi: 10.1111/j.1360-0443.2011.03709.x. [DOI] [PubMed] [Google Scholar]
- Baumann MH, Partilla JS, Lehner KR. Psychoactive “bath salts”: not so soothing. European Journal of Pharmacology. 2013;698(1–3):1–5. doi: 10.1016/j.ejphar.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumann MH, Partilla JS, Lehner KR, Thorndike EB, Hoffman AF, Holy M, Rothma RB, Goldberg SR, Lupica CR, Sitte HH, Brandt SD, Tella SR, Cozzi NV, Schindler CW. Powerful cocaine-like actions of 3,4-methylenedioxypyrovalerone (MDPV), a principal constituent of psychoactive 'bath salts' products. Neuropsychopharmacology. 2013b;38(4):552–562. doi: 10.1038/npp.2012.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth RE, Watters JK, Chitwood DD. HIV risk-related sex behaviors among injection drug users, crack smokers, and injection drug users who smoke crack. American Journal of Public Health. 1993;83(8):1144–1148. doi: 10.2105/ajph.83.8.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Dart RC. 2010 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 28th Annual Report. Clinical Toxicology. 2011;49(10):910–941. doi: 10.3109/15563650.2011.635149. [DOI] [PubMed] [Google Scholar]
- Brown AH, Domier CP, Rawson RA. Stimulants, sex, and gender. Sexual Addiction & Compulsivity. 2005;12(2–3):169–180. [Google Scholar]
- Bux DA, Lamb RJ, Iguchi MY. Cocaine use and HIV risk behavior in methadone maintenance patients. Drug and Alcohol Dependence. 1995;37(1):29–35. doi: 10.1016/0376-8716(94)01058-s. [DOI] [PubMed] [Google Scholar]
- Cameron KN, Kolanos R, Solis E, Jr, Glennon RA, De Felice LJ. Bath salts components mephedrone and methylenedioxypyrovalerone (MDPV) act synergistically at the human dopamine transporter. British Journal of Pharmacology. 2013;168(7):1750–1757. doi: 10.1111/bph.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris RL, King LA, Nutt DJ. A web-based survey on mephedrone. Drug and Alcohol Dependence. 2011;118(1):19–22. doi: 10.1016/j.drugalcdep.2011.02.011. [DOI] [PubMed] [Google Scholar]
- De Paoli G, Maskell PD, Pounder DJ. Naphyrone: analytical profile of the new “legal high” substitute for mephedrone. Journal of Forensic and Legal Medicine. 2011;18(2):93. doi: 10.1016/j.jflm.2010.12.001. [DOI] [PubMed] [Google Scholar]
- Eshleman AJ, Wolfrum KM, Hatfield MG, Johnson RA, Murphy KV, Janowsky A. Substituted methcathinones differ in transporter and receptor interactions. Biochemical Pharmacology. 2013;85(12):1803–1815. doi: 10.1016/j.bcp.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fantegrossi WE, Gannon BM, Zimmerman SM, Rice KC. In vivo effects of abused ‘bath salt’ constituent 3,4-methylenedioxypyrovalerone (MDPV) in mice: drug discrimination, thermoregulation, and locomotor activity. Neuropsychopharmacology. 2013;38(4):563–573. doi: 10.1038/npp.2012.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrester MB. Synthetic cathinone exposures reported to Texas poison centers. The American Journal of Drug and Alcohol Abuse. 2012;38(6):609–615. doi: 10.3109/00952990.2012.677890. [DOI] [PubMed] [Google Scholar]
- Gatch MB, Taylor CM, Forster MJ. Locomotor stimulant and discriminative stimulus effects of ‘bath salt’ cathinones. Behavioral Pharmacology. 2013;24(5–6):437–447. doi: 10.1097/FBP.0b013e328364166d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales R, Mooney L, Rawson RA. The methamphetamine problem in the United States. Annual Review of Public Health. 2010;31:385–398. doi: 10.1146/annurev.publhealth.012809.103600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart CL, Gunderson EW, Perez A, Kirkpatrick MG, Thurmond A, Comer SD, Foltin RW. Acute physiological and behavioral effects of intranasal methamphetamine in humans. Neuropsychopharmacology. 2008;33(8):1847–1855. doi: 10.1038/sj.npp.1301578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatsukami DK, Fischman MW. Crack cocaine and cocaine hydrochloride. Are the differences myth or reality? JAMA: The Journal of the American Medical Association. 1996;276(19):1580–1588. [PubMed] [Google Scholar]
- Hoffman JA, Klein H, Eber M, Crosby H. Frequency and intensity of crack use as predictors of women’s involvement in HIV-related sexual risk behaviors. Drug and Alcohol Dependence. 2000;58(3):227–236. doi: 10.1016/s0376-8716(99)00095-2. [DOI] [PubMed] [Google Scholar]
- Hudziak JJ, Helzer JE, Wetzel MW, Kessel KB, McGee B, Janca A, Przybeck T. The use of the DSM-III-R Checklist for initial diagnostic assessments. Comprehensive Psychiatry. 1993;34(6):375–383. doi: 10.1016/0010-440x(93)90061-8. [DOI] [PubMed] [Google Scholar]
- Hursh SR, Silberberg A. Economic demand and essential value. Psychological Review. 2008;115(1):186–198. doi: 10.1037/0033-295X.115.1.186. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2012. Ann Arbor, Michigan: University of Michigan Institute for Social Research; 2013. [Google Scholar]
- Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use: 1975–2013: Overview, key findings on adolescent drug use. Ann Arbor, Michigan: University of Michigan Institute for Social Research; 2014. [Google Scholar]
- Kelly BC, Wells BE, Pawson M, Leclair A, Parsons JT, Golub SA. Novel psychoactive drug use among younger adults involved in US nightlife scenes. Drug and Alcohol Review. 2013;32(6):588–593. doi: 10.1111/dar.12058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khey DN, Stogner J, Miller BL. Emerging Trends in Drug Use and Distribution. Cham, Switzerland: Springer International Publishing; 2014. [Google Scholar]
- López-Arnau R, Martínez-Clemente J, Pubill D, Escubedo E, Camarasa J. Comparative neuropharmacology of three psychostimulant cathinone derivatives: butylone, mephedrone and methylone. British Journal of Pharmacology. 2012;167(2):407–420. doi: 10.1111/j.1476-5381.2012.01998.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez M. Tests in cannibalism case: Zombie-like attacker used pot, not ‘bath salts’. [accessed on August 27, 2013];2012 http://www.cnn.com/2012/06/27/us/florida-cannibal-attack. [Google Scholar]
- Marusich JA, Grant KR, Blough BE, Wiley JL. Effects of synthetic cathinones contained in “bath salts” on motor behavior and a functional observational battery in mice. Neurotoxicology. 2012;33(5):1305–1313. doi: 10.1016/j.neuro.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miotto K, Striebel J, Cho AK, Wang C. Clinical and pharmacological aspects of bath salt use: A review of the literature and case reports. Drug and Alcohol Dependence. 2013;132(1–2):1–12. doi: 10.1016/j.drugalcdep.2013.06.016. [DOI] [PubMed] [Google Scholar]
- Motbey CP, Clemens KJ, Apetz N, Winstock AR, Ramsey J, Li KM, Wyatt N, Callaghan PD, Bowen MT, Cornish JL, McGregor IS. High levels of intravenous mephedrone (4-methylmethcathinone) self-administration in rats: neural consequences and comparison with methamphetamine. Journal of Psychopharmacology. 2013;27(9):823–836. doi: 10.1177/0269881113490325. [DOI] [PubMed] [Google Scholar]
- Murphy CM, Dulaney AR, Beuhler MC, Kacinko S. “Bath salts” and “plant food” products: the experience of one regional US poison center. Journal of Medical Toxicology. 2013;9(1):42–48. doi: 10.1007/s13181-012-0243-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien CP. Drug addiction. In: Brunton LL, Chabner BA, Knollman BC, editors. Goodman & Gilman’s Pharmacologic Basis of Therapeutics. 12th ed. New York: McGraw-Hill; 2011. [Google Scholar]
- Penders TM, Gestring RE, Vilensky DA. Excited delirium following use of synthetic cathinones (bath salts) General Hospital Psychiatry. 2012;34(6):647–650. doi: 10.1016/j.genhosppsych.2012.06.005. [DOI] [PubMed] [Google Scholar]
- Prosser JM, Nelson LS. The toxicology of bath salts: a review of synthetic cathinones. Journal of Medical Toxicology. 2012;8(1):33–42. doi: 10.1007/s13181-011-0193-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum CD, Carreiro SP, Babu KM. Here today, gone tomorrow2026;and back again? A review of herbal marijuana alternatives (K2, Spice), synthetic cathinones (bath salts), kratom, Salvia divinorum, methoxetamine, and piperazines. Journal of Medical Toxicology. 2012;8(1):15–32. doi: 10.1007/s13181-011-0202-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross EA, Reisfield GM, Watson MC, Chronister CW, Goldberger BA. Psychoactive “bath salts” intoxication with methylenedioxypyrovalerone. The American Journal of Medicine. 2012;125(9):854–858. doi: 10.1016/j.amjmed.2012.02.019. [DOI] [PubMed] [Google Scholar]
- Shanks KG, Dahn T, Behonick G, Terrell A. Analysis of first and second generation legal highs for synthetic cannabinoids and synthetic stimulants by ultra-performance liquid chromatography and time of flight mass spectrometry. Journal of Analytical Toxicology. 2012;36(6):360–371. doi: 10.1093/jat/bks047. [DOI] [PubMed] [Google Scholar]
- Simmler LD, Buser TA, Donzelli M, Schramm Y, Dieu LH, Huwyler J, Chaboz S, Hoener MC, Liechti ME. Pharmacological characterization of designer cathinones in vitro. British Journal of Pharmacology. 2013;168(2):458–470. doi: 10.1111/j.1476-5381.2012.02145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiller HA, Ryan ML, Weston RG, Jansen J. Clinical experience with and analytical confirmation of “bath salts” and “legal highs” (synthetic cathinones) in the United States. Clinical Toxicology. 2011;49(6):499–505. doi: 10.3109/15563650.2011.590812. [DOI] [PubMed] [Google Scholar]
- Stogner JM, Miller BL. Investigating the ‘bath salt’ panic: the rarity of synthetic cathinone use among students in the United States. Drug and Alcohol Review. 2013;32(5):545–549. doi: 10.1111/dar.12055. [DOI] [PubMed] [Google Scholar]
- Thornton SL, Gerona RR, Tomaszewski CA. Psychosis from a bath salt product containing flephedrone and MDPV with serum, urine, and product quantification. Journal of Medical Toxicology. 2012;8(3):310–313. doi: 10.1007/s13181-012-0232-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandrey R, Johnson MW, Johnson PS, Khalil MA. Novel drugs of abuse: A snapshot of an evolving marketplace. Adolescent Psychiatry. 2013;3(2):123–134. doi: 10.2174/2210676611303020003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Fischman MW, Foltin R, Fowler JS, Franceschi D, Franceschi M, Logan J, Gatley SJ, Wong C, Ding YS, Hitzemann R, Pappas N. Effects of route of administration on cocaine induced dopamine transporter blockade in the human brain. Life Sciences. 2000;67(12):1507–1515. doi: 10.1016/s0024-3205(00)00731-1. [DOI] [PubMed] [Google Scholar]
- Warrick BJ, Hill M, Hekman K, Christensen R, Goetz R, Casavant MJ, Wahl M, Mowry JB, Spiller H, Anderson D, Aleguas A, Gummin D, Thomas R, Nezlek C, Smolinske S. A 9-state analysis of designer stimulant, “bath salt,” hospital visits reported to poison control centers. Annals of Emergency Medicine. 2013;62(3):244–251. doi: 10.1016/j.annemergmed.2012.12.017. [DOI] [PubMed] [Google Scholar]
- Watterson LR, Hood L, Sewalia K, Tomek SE, Yahn S, Johnson CT, Wegner S, Blough BE, Marusich JA, Olive MF. The reinforcing and rewarding effects of methylone, a synthetic cathinone commonly found in “bath salts”. Journal of Addiction Research & Therapy. 2012;(Suppl 9):002. doi: 10.4172/2155-6105.S9-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watterson LR, Kufahl PR, Nemirovsky NE, Sewalia K, Grabenauer M, Thomas BF, Marusich JA, Wegner S, Olive MF. Potent rewarding and reinforcing effects of the synthetic cathinone 3,4-methylenedioxypyrovalerone (MPDV) Addiction Biology. 2012;19(2):165–174. doi: 10.1111/j.1369-1600.2012.00474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstock AR, Mitcheson LR, Deluca P, Davey Z, Corazza O, Schifano F. Mephedrone, new kid for the chop? Addiction. 2011;106(1):154–161. doi: 10.1111/j.1360-0443.2010.03130.x. [DOI] [PubMed] [Google Scholar]
- Winstock A, Mitcheson L, Ramsey J, Davies S, Puchnarewicz M, Marsden J. Mephedrone: use, subjective effects and health risks. Addiction. 2011;106(11):1991–1996. doi: 10.1111/j.1360-0443.2011.03502.x. [DOI] [PubMed] [Google Scholar]
- Wood KE. Exposure to bath salts and synthetic tetrahydrocannabinol from 2009 to 2012 in the United States. The Journal of Pediatrics. 2013;163(1):213–216. doi: 10.1016/j.jpeds.2012.12.056. [DOI] [PubMed] [Google Scholar]
- Wood DM, Dargan PI. Mephedrone (4-methylmethcathinone): What is new in our understanding of its use and toxicity. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2012;39(2):227–233. doi: 10.1016/j.pnpbp.2012.04.020. [DOI] [PubMed] [Google Scholar]
- Yin S, Ho M. Monitoring a toxicological outbreak using Internet search query data. Clinical Toxicology. 2012;50(9):818–822. doi: 10.3109/15563650.2012.729667. [DOI] [PubMed] [Google Scholar]