Abstract
Primate lentiviruses exhibit narrow host tropism, reducing the occurrence of zoonoses but also impairing the development of optimal animal models of AIDS. To delineate the factors limiting cross-species HIV-1 transmission, we passaged a modified HIV-1 in pigtailed macaques that were transiently depleted of CD8+ cells during acute infection. During adaptation over four passages in macaques, HIV-1 acquired the ability to antagonize the macaque restriction factor tetherin, replicated at progressively higher levels and ultimately caused marked CD4+ T-cell depletion and AIDS-defining conditions. Transient treatment with anti-CD8 during acute HIV-1 infection caused rapid progression to AIDS, while untreated animals exhibited an elite controller phenotype. Thus, an adapted HIV-1 can cause AIDS in macaques, and stark differences in outcome can be determined by immunological perturbations during early infection.
HIV-1 replicates well in humans, but like other primate lentiviruses, it encounters impediments to replication in atypical host species (1–3). This fact has limited the development of optimal animal models of AIDS (4, 5). To delineate the requirements for primate lentivirus to colonize a divergent host and to aid development of better animal models of AIDS, we adapted HIV-1 to replicate efficiently and cause AIDS in a monkey species.
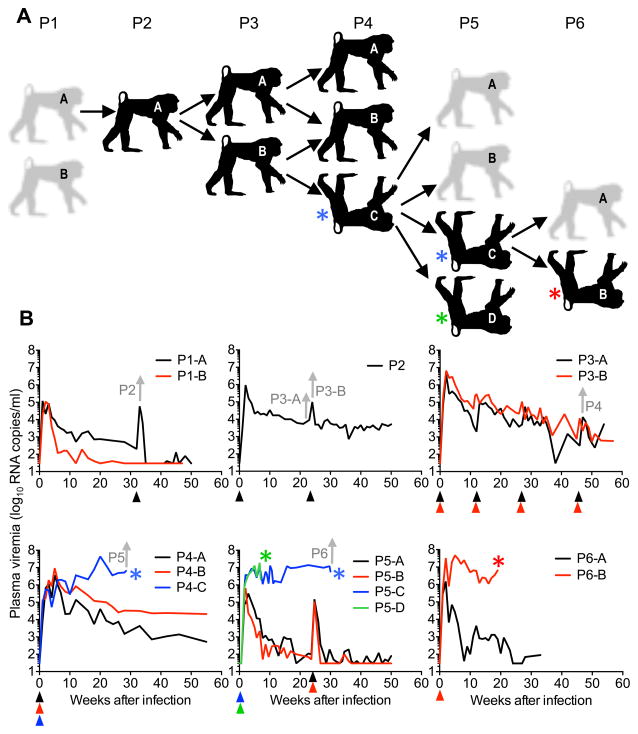
We inoculated pigtailed macaques (Maccaca nemestrina), which lack an HIV-1 restricting TRIM5 protein (6–9), with HIV-1 clones encoding SIVMAC Vif, which antagonizes several macaque APOBEC3 proteins that would otherwise restrict HIV-1 replication (10). The inoculum contained four clonal HIV-1NL4-3-derived viruses, each encoding a gp120 envelope protein from a prototype HIV-1 strain that utilizes the CCR5 co-receptor (Fig. 1A, fig. S1). In two passage-1 (P1) animals, acute plasma viremia reached ~105 viral RNA (vRNA) copies/ml and declined thereafter (Fig. 1B). This outcome was similar to our previous findings using an HIV-1 derivative encoding a primarily CXCR4-utilizing envelope protein (KB9) (11). One P1 animal (P1-A), in which viremia of ~103 vRNA copies/ml was maintained for 32 weeks (Fig. 1B), was treated with a monoclonal antibody to deplete CD8+ T cells to relieve immune pressure and thereby increase the viral population size. Its blood was used to initiate P2 infection (Fig. 1A, B, fig. S2). For P2, and each passage thereafter, recipient animals were treated with anti-CD8, at the time of inoculation and one week later, to augment early viremia (12). This treatment caused transient CD8+ T-cell depletion in blood and lymph nodes, without major impact on CD8+ T-cells in gut-associated lymphoid tissue (GALT) (Fig. S2, S3). In P2-A, acute viremia reached 106 vRNA copies/ml, declining to ~104 vRNA copies/ml at 5 to 6 weeks after infection (Fig. 1B). In P1 and P2 animals, the levels of blood CD4+ T-cells appeared unperturbed (Fig. 2A).
Fig. 1. Adaptation of HIV-1 to pigtail macaques.
(A) Outline of serial animal-to-animal HIV-1 passages. Animals colored black were transiently depleted of CD8+ cells at the time of inoculation. Inverted animals with colored asterisks indicate animals that were euthanized for clinical cause, including AIDS defining conditions. (B) Viremia in the plasma of HIV-1 infected macaques. Color-coded arrowheads indicate anti-CD8 treatment and asterisks indicate deaths (color code is the same for panel (A)). Grey arrows indicate times at which blood was taken to initiate the subsequent passage.
Fig. 2. HIV-1 pathogenesis in pigtail macaques.
(A) CD4+ T-cell counts in blood of HIV-1 infected macaques. Color codes, arrowheads and asterisks are as described in Fig. 1. (B) CD4+ T-cell subset frequencies in GALT at the indicated weeks after infection. ‘Pre’ = 0 to 1 week before infection. (C) Immunohistochemical staining of CD4+ T-cells (brown) and myeloid cells (CD68+/CD163+; red) in the GALT of P4-C. Scale bar = 100μm. (D) Immunohistochemical staining (brown) of CD3+ T-cells (top) CD20+ B-cells (bottom) in tumor (marked T) effacing normal kidney tissue (marked N) in P4-C. Scale bar = 200μm. (E) Grocott’s methenamine silver stain revealing Pneumocystis organisms (black spots) in P4-C lung tissue. Scale bar = 50μm.
Animal P3-A was inoculated with blood taken from P2-A at 23 weeks post infection whereas animal P3-B was inoculated with blood taken 1 week later, after CD8+ cell depletion of P2-A (Fig. 1A, B). P3 recipients exhibited acute viremia at ~106 to 107 vRNA copies/ml. Blood CD4+ T-cells numbers and the proportion of CD4+ T-cells in GALT decreased following infection (Fig. 2A, B) but these perturbations were transient or modest in magnitude. Moreover, viremia declined over the ensuing 50–60 weeks (Fig. 1B). We depleted CD8+ cells in P3 macaques on three subsequent occasions (fig. S2). Although transient increases in plasma viremia followed antibody administration (Fig. 1B), neither animal exhibited disease.
P4 animals were inoculated with blood taken from either or both P3 macaques at 50 weeks post infection (Fig. 1A, B). Each developed acute viremia at ~106–107 vRNA copies/ml (Fig. 1B). Notably, marked and sustained CD4+ T-cell depletion occurred in the blood of 2 out of 3, and in the GALT of all P4 animals (Fig. 2A, B, C). Additional indications of HIV-1-induced pathogenesis included immune activation, as evidenced by more frequent Ki67 expression in GALT CD4+ cells (fig. S4A), as well as fibrotic disruption and frequent Ki67 expression in T-cell zones of lymph nodes (fig. S4 B, C, D). In P4-C, pathology was especially evident, and viremia continued to increase after the acute phase, approaching ~108 vRNA copies/ml (Fig 1B). Loss of blood and GALT CD4+ T-cells in P4-C was virtually complete at 28 weeks (Fig 2A, B, C). At this point, P4-C succumbed to an AIDS-defining, multifocal extranodal B-cell lymphoma with large retro-orbital and paraspinal tumors, and extensive epicardial and renal involvement (Fig. 2D, fig. S5A, B, C). Such tumors, associated with SIV-induced AIDS in macaques have been linked to opportunistic lymphocryptoviruses or rhadinoviruses and are analogous to B-cell neoplasms in humans co-infected with HIV-1 and Kaposi’s sarcoma-associated herpesvirus (KSHV) (13). AIDS-defining Pneumocystis pneumonia was also detected in P4-C lung biopsies (Fig. 2E) but not in controls (fig S6A).
To confirm that HIV-1 had adapted to replicate efficiently and cause AIDS in macaques, 4 animals (P5-A-D, Fig 1A) were inoculated with blood from P4-C. Two macaques that were transiently depleted of CD8+ cells at inoculation (P5-C and P5-D, Fig. 1A, fig. S2) developed persistently high viremia (~107 vRNAcopies/ml) with blood and GALT CD4+ T-cell depletion (Fig. 1B, Fig 2A). P5-C was euthanized at week 30 after infection, with Pneumocystis pneumonia (fig. S6B), whereas P5-D was euthanized at week 7 following onset of severe bilateral hind limb weakness with wasting. In P5-A and P5-B, which were not CD8 depleted, acute viremia reached ~106 vRNA copies/ml, but was controlled thereafter (Fig. 1B). Blood and GALT CD4+ T-cells were depleted but recovered thereafter (Fig. 2 A, B). Subsequent CD8+ cell depletion in P5-A and P5-B at week 23 (fig. S2), caused transient increases (103-fold) in viremia, and blood CD4+ cell depletion in P5-A, but did not recapitulate the effect of CD8+ cell depletion during acute infection (Fig. 1B, Fig. 2A). Rather, as CD8+ cells recovered in P5-A and P5-B, viremia and CD4+ T-cells returned to pre-depletion levels (Fig. 1B, Fig. 2A).
This dichotomous outcome of HIV-1 infection was reproduced in animals that received blood from P5-C. Specifically, P6-A, (no CD8 depletion), showed acute viremia that was subsequently controlled with modest and transient GALT CD4+ T-cell depletion (Fig. 1A, B, Fig 2A, B). Conversely, in P6-B (CD8 depleted at infection, fig. S2), viremia persisted at 106–107 vRNA copies/ml while blood and GALT CD4+ cells were nearly completely depleted (Fig. 1B, Fig. 2A, B). P6-B was euthanized at 9 weeks with symptoms of nephropathy or glomerulonephritis (azotemia, hyperphosphatemia, hypoproteinemia and anemia). Necropsy revealed myocardial fibrosis, lymphoid depletion with histiocytosis, and diffuse expansion of the glomerular mesangial matrix. Although not AIDS defining, these conditions have frequently been described in human AIDS patients (14) and occasionally in SIV-infected macaques (15).
Single viral genome amplification and sequencing (SGA) (16–18) at various points during adaptation revealed that one envelope gene in the initial inoculum (AD8) dominated the viral population in P1-A and was the only strain detected in P2 to P6 (Fig. 3A). Indeed, Env sequences in P2-P6 macaques sampled over ~3.5 years exhibited only ~2% divergence from AD8. Additionally, although T-cells constituted the dominant infected cell type in lymph nodes, the propensity of AD8 to infect macrophages in GALT was preserved throughout P3-P6 (fig. S7A, B, C). In P5-C, that succumbed following a precipitous decline in blood CD4+ T-cells (Fig. 2A), about half of the envelope sequences had a four amino-acid deletion in the V3 loop (Fig. 3B), a determinant of coreceptor utilization (19). This deletion was associated with a change in coreceptor utilization, as evidenced by viral sensitivity to Maraviroc (CCR5 antagonist) or AMD3100 (CXCR4 antagonist) (Fig. 3C, D). Thus, HIV-1 infection in P5-C recapitulated a common feature of HIV-1 disease, namely coreceptor switching, that rarely occurs in non-human primate lentivirus infections (20). Interestingly, the V3 loop deletion associated with CXCR4 utilization was not detected in P6-A or P6-B, both of which received blood from P5-C.
Fig. 3. Envelope evolution and coreceptor switching in HIV-1 infected macaques.
(A) Phylogenetic analysis of Env sequences (using SGA and neighbor joining method) found in plasma of HIV-1 infected macaques. (B) V3 loop amino acid sequences from the AD8 inoculum and representative viral genomes in P5-C plasma at week 27 after infection. (C, D) Infectivity of HIV-1 ΔEnv-GFP pseudotyped with control X4 (NL4-3) or R5 (AD8) or P5-C-derived Env proteins in the presence of Maraviroc (8nM) (C) or AMD3100 (1μM) (D) relative to no inhibitor. Values are mean ± S.D. of three independent experiments.
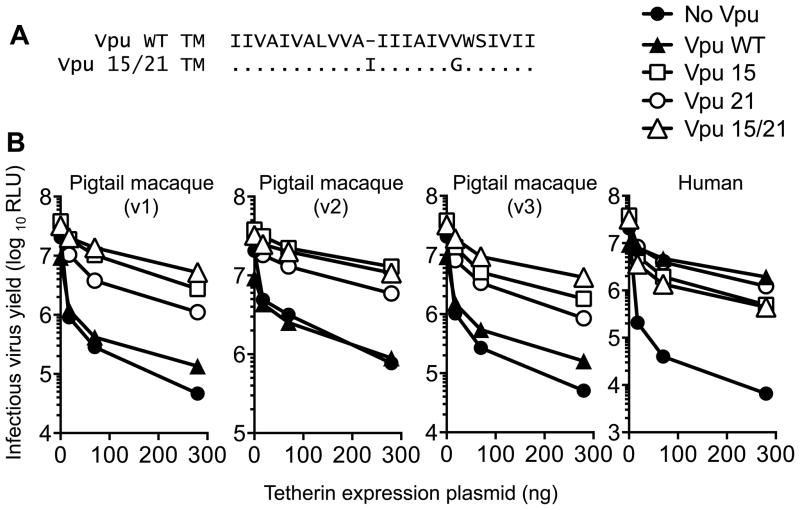
Although the initial virus was not restricted by TRIM5α and APOBEC3, HIV-1 Vpu does not antagonize macaque tetherin, rendering the initial inoculum sensitive to this potential host-range restriction (21, 22). Notably, an insertion of an amino-acid at position 15 in the Vpu transmembrane (TM) domain (Fig. 4A) was detected in P1-A and was found in 100% of P2-A sequences at 52 weeks, and all sequences thereafter. Another Vpu TM mutation, V21G, (Fig. 4A) was detected in P3 animals and in all sequences from P4 onwards. TM domains govern Vpu:tetherin interaction (21) and each of the TM domain mutations contributed to the ability of Vpu 15/21 to antagonize pigtailed macaque tetherin (Fig. 4B). We previously showed that Vpu gained the ability to antagonize human tetherin during the emergence of HIV-1(23), and the passage of HIV-1 in pigtailed macaques apparently resulted in an analogous adaptation (Fig. 4B).
Fig. 4. Adaptation of HIV-1 Vpu to antagonize Tetherin in macaques.
(A) Amino acid alignment of the Vpu transmembrane domain from the initial viral clone, and after adaptation in pigtailed macaques. (B) Infectious virion yield from 293T cells transfected with HIV-1 proviral plasmids encoding the indicated Vpu proteins and plasmids expressing human or three naturally occurring variants (v1-v3) of pigtailed macaque Tetherin.
Antibodies to HIV-1 proteins were apparent in P4-A beginning at week 4, but were not detected until week 16 after infection in P4-B, which had higher viremia and some degree of blood CD4+ T-cell depletion (fig. S8, Fig. 1B, Fig. 2A). Animal P4-C, the first to succumb to AIDS, did not seroconvert (fig. S8). In fact, each macaque that progressed to AIDS following transient CD8 depletion did not seroconvert, whereas those that were not CD8 depleted and did not progress to AIDS mounted robust antibody responses (fig. S8). Previously, failure to seroconvert has been associated with rapid progression in SIV infection (24). HIV-1-induced loss of CD4+ helper T-cells in CD8-depleted animals may play a role in the failure to mount an antibody response in macaques that developed AIDS (12).
The approaches employed herein have enabled HIV-1 infection of macaques to recapitulate salient features of HIV-1 infection in humans. Our findings suggest that evasion or antagonism of antiretroviral proteins is key for the colonization of new hosts by primate lentiviruses. Because transient depletion of CD8+ cells during acute infection determined whether macaques became rapid progressors or elite controllers, our findings suggest that the immunological insult during acute HIV-1 infection can determine subsequent clinical course. It is also possible that adaptation to the host major histocompatibility complexes, and evasion of adaptive immune responses may be required for HIV-1 pathogenesis in immunologically intact hosts. Finally, because the viral strain used herein contains nearly all the targets of HIV-1 vaccines and drugs, further development of a pigtailed macaque-based model could facilitate the evaluation of novel clinical HIV-1 therapies, prevention strategies and interventions for virus eradication.
Supplementary Material
Acknowledgments
This work was supported by grants from the NIH; R37AI64003 and R01AI50111 (to P.D.B.), R01AI078788 (to T.H.), DFG fellowship BI1540/1-1 to JB, by the Howard Hughes Medical Institute, and in part with federal funds from the National Cancer Institute, National Institutes of Health, under Contract No. HHSN261200800001E. We thank Vicky Coalter, Adam Wiles, Rodney Wiles, and Donald Johnson for assistance with study coordination and sample processing. Histology support was provided by the Pathology/Histotechnology Laboratory core service located at the Frederick National Laboratory for Cancer Research, Leidos Biomedical Research, Inc., Frederick MD.
Footnotes
The data presented in this paper are tabulated in the main paper and in the supplementary materials. HIV-1 Env sequences used in Fig. 3 have been deposited in Genbank (accession numbers KJ201545 through KJ201764) Sequences encompassing the full-length viral genome for P5 and P6 have also been deposited in GenBank (accession numbers KJ767573 through KJ767592).
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
References and Notes
- 1.Blanco-Melo D, Venkatesh S, Bieniasz PD. Intrinsic cellular defenses against human immunodeficiency viruses. Immunity. 2012;37:399–411. doi: 10.1016/j.immuni.2012.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stremlau M, Owens CM, Perron MJ, Kiessling M, Autissier P, Sodroski J. The cytoplasmic body component TRIM5alpha restricts HIV-1 infection in Old World monkeys. Nature. 2004;427:848–853. doi: 10.1038/nature02343. [DOI] [PubMed] [Google Scholar]
- 3.Mariani R, Chen D, Schrofelbauer B, Navarro F, Konig R, Bollman B, Munk C, Nymark-McMahon H, Landau NR. Species-specific exclusion of APOBEC3G from HIV-1 virions by Vif. Cell. 2003;114:21–31. doi: 10.1016/s0092-8674(03)00515-4. [DOI] [PubMed] [Google Scholar]
- 4.Ambrose Z, KewalRamani VN, Bieniasz PD, Hatziioannou T. HIV/AIDS: in search of an animal model. Trends in biotechnology. 2007;25:333–337. doi: 10.1016/j.tibtech.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Hatziioannou T, Evans DT. Animal models for HIV/AIDS research. Nature reviews Microbiology. 2012;10:852–867. doi: 10.1038/nrmicro2911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liao CH, Kuang YQ, Liu HL, Zheng YT, Su B. A novel fusion gene, TRIM5-Cyclophilin A in the pig-tailed macaque determines its susceptibility to HIV-1 infection. AIDS. 2007;21(Suppl 8):S19–26. doi: 10.1097/01.aids.0000304692.09143.1b. [DOI] [PubMed] [Google Scholar]
- 7.Virgen CA, Kratovac Z, Bieniasz PD, Hatziioannou T. Independent genesis of chimeric TRIM5-cyclophilin proteins in two primate species. Proceedings of the National Academy of Sciences of the United States of America. 2008;105:3563–3568. doi: 10.1073/pnas.0709258105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brennan G, Kozyrev Y, Hu SL. TRIMCyp expression in Old World primates Macaca nemestrina and Macaca fascicularis. Proceedings of the National Academy of Sciences of the United States of America. 2008;105:3569–3574. doi: 10.1073/pnas.0709511105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newman RM, Hall L, Kirmaier A, Pozzi LA, Pery E, Farzan M, O’Neil SP, Johnson W. Evolution of a TRIM5-CypA splice isoform in old world monkeys. PLoS pathogens. 2008;4:e1000003. doi: 10.1371/journal.ppat.1000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Virgen CA, Hatziioannou T. Antiretroviral activity and Vif sensitivity of rhesus macaque APOBEC3 proteins. Journal of virology. 2007;81:13932–13937. doi: 10.1128/JVI.01760-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatziioannou T, Ambrose Z, Chung NP, Piatak M, Jr, Yuan F, Trubey CM, Coalter V, Kiser R, Schneider D, Smedley J, Pung R, Gathuka M, Estes JD, Veazey RS, KewalRamani VN, Lifson JD, Bieniasz PD. A macaque model of HIV-1 infection. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:4425–4429. doi: 10.1073/pnas.0812587106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veazey RS, Acierno PM, McEvers KJ, Baumeister SH, Foster GJ, Rett MD, Newberg MH, Kuroda MJ, Williams K, Kim EY, Wolinsky SM, Rieber EP, Piatak M, Jr, Lifson JD, Montefiori DC, Brown CR, Hirsch VM, Schmitz JE. Increased loss of CCR5+ CD45RA- CD4+ T cells in CD8+ lymphocyte-depleted Simian immunodeficiency virus-infected rhesus monkeys. Journal of virology. 2008;82:5618–5630. doi: 10.1128/JVI.02748-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orzechowska BU, Powers MF, Sprague J, Li H, Yen B, Searles RP, Axthelm MK, Wong SW. Rhesus macaque rhadinovirus-associated non-Hodgkin lymphoma: animal model for KSHV-associated malignancies. Blood. 2008;112:4227–4234. doi: 10.1182/blood-2008-04-151498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rao TK. Human immunodeficiency virus (HIV) associated nephropathy. Annual review of medicine. 1991;42:391–401. doi: 10.1146/annurev.me.42.020191.002135. [DOI] [PubMed] [Google Scholar]
- 15.Stephens EB, Tian C, Li Z, Narayan O, Gattone VH., 2nd Rhesus macaques infected with macrophage-tropic simian immunodeficiency virus (SIVmacR71/17E) exhibit extensive focal segmental and global glomerulosclerosis. Journal of virology. 1998;72:8820–8832. doi: 10.1128/jvi.72.11.8820-8832.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simmonds P, Balfe P, Ludlam CA, Bishop JO, Brown AJ. Analysis of sequence diversity in hypervariable regions of the external glycoprotein of human immunodeficiency virus type 1. Journal of virology. 1990;64:5840–5850. doi: 10.1128/jvi.64.12.5840-5850.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Palmer S, Kearney M, Maldarelli F, Halvas EK, Bixby CJ, Bazmi H, Rock D, Falloon J, Davey RT, Jr, Dewar RL, Metcalf JA, Hammer S, Mellors JW, Coffin JM. Multiple, linked human immunodeficiency virus type 1 drug resistance mutations in treatment-experienced patients are missed by standard genotype analysis. Journal of clinical microbiology. 2005;43:406–413. doi: 10.1128/JCM.43.1.406-413.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keele BF, Giorgi EE, Salazar-Gonzalez JF, Decker JM, Pham KT, Salazar MG, Sun C, Grayson T, Wang S, Li H, Wei X, Jiang C, Kirchherr JL, Gao F, Anderson JA, Ping LH, Swanstrom R, Tomaras GD, Blattner WA, Goepfert PA, Kilby JM, Saag MS, Delwart EL, Busch MP, Cohen MS, Montefiori DC, Haynes BF, Gaschen B, Athreya GS, Lee HY, Wood N, Seoighe C, Perelson AS, Bhattacharya T, Korber BT, Hahn BH, Shaw GM. Identification and characterization of transmitted and early founder virus envelopes in primary HIV-1 infection. Proceedings of the National Academy of Sciences of the United States of America. 2008;105:7552–7557. doi: 10.1073/pnas.0802203105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choe H, Farzan M, Sun Y, Sullivan N, Rollins B, Ponath PD, Wu L, Mackay CR, LaRosa G, Newman W, Gerard N, Gerard C, Sodroski J. The beta-chemokine receptors CCR3 and CCR5 facilitate infection by primary HIV-1 isolates. Cell. 1996;85:1135–1148. doi: 10.1016/s0092-8674(00)81313-6. [DOI] [PubMed] [Google Scholar]
- 20.Sina ST, Ren W, Cheng-Mayer C. Coreceptor use in nonhuman primate models of HIV infection. Journal of translational medicine. 2011;9(Suppl 1):S7. doi: 10.1186/1479-5876-9-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McNatt MW, Zang T, Hatziioannou T, Bartlett M, Fofana IB, Johnson WE, Neil SJ, Bieniasz PD. Species-specific activity of HIV-1 Vpu and positive selection of tetherin transmembrane domain variants. PLoS pathogens. 2009;5:e1000300. doi: 10.1371/journal.ppat.1000300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jia B, Serra-Moreno R, Neidermyer W, Rahmberg A, Mackey J, Fofana IB, Johnson WE, Westmoreland S, Evans DT. Species-specific activity of SIV Nef and HIV-1 Vpu in overcoming restriction by tetherin/BST2. PLoS pathogens. 2009;5:e1000429. doi: 10.1371/journal.ppat.1000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sauter D, Schindler M, Specht A, Landford WN, Munch J, Kim KA, Votteler J, Schubert U, Bibollet-Ruche F, Keele BF, Takehisa J, Ogando Y, Ochsenbauer C, Kappes JC, Ayouba A, Peeters M, Learn GH, Shaw G, Sharp PM, Bieniasz P, Hahn BH, Hatziioannou T, Kirchhoff F. Tetherin-driven adaptation of Vpu and Nef function and the evolution of pandemic and nonpandemic HIV-1 strains. Cell host & microbe. 2009;6:409–421. doi: 10.1016/j.chom.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hirsch VM, Santra S, Goldstein S, Plishka R, Buckler-White A, Seth A, Ourmanov I, Brown CR, Engle R, Montefiori D, Glowczwskie J, Kunstman K, Wolinsky S, Letvin NL. Immune failure in the absence of profound CD4+ T-lymphocyte depletion in simian immunodeficiency virus-infected rapid progressor macaques. Journal of virology. 2004;78:275–284. doi: 10.1128/JVI.78.1.275-284.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang YJ, Hatziioannou T, Zang T, Braaten D, Luban J, Goff SP, Bieniasz PD. Envelope-dependent, cyclophilin-independent effects of glycosaminoglycans on human immunodeficiency virus type 1 attachment and infection. Journal of virology. 2002;76:6332–6343. doi: 10.1128/JVI.76.12.6332-6343.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tabb B, Morcock DR, Trubey CM, Quinones OA, Hao XP, Smedley J, Macallister R, Piatak M, Jr, Harris LD, Paiardini M, Silvestri G, Brenchley JM, Alvord WG, Lifson JD, Estes JD. Reduced inflammation and lymphoid tissue immunopathology in rhesus macaques receiving anti-tumor necrosis factor treatment during primary simian immunodeficiency virus infection. The Journal of infectious diseases. 2013;207:880–892. doi: 10.1093/infdis/jis643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Del Prete GQ, Kearney MF, Spindler J, Wiegand A, Chertova E, Roser JD, Estes JD, Hao XP, Trubey CM, Lara A, Lee K, Chaipan C, Bess JW, Jr, Nagashima K, Keele BF, Macallister R, Smedley J, Pathak VK, Kewalramani VN, Coffin JM, Lifson JD. Restricted replication of xenotropic murine leukemia virus-related virus in pigtailed macaques. Journal of virology. 2012;86:3152–3166. doi: 10.1128/JVI.06886-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brenchley JM, Vinton C, Tabb B, Hao XP, Connick E, Paiardini M, Lifson JD, Silvestri G, Estes JD. Differential infection patterns of CD4+ T cells and lymphoid tissue viral burden distinguish progressive and nonprogressive lentiviral infections. Blood. 2012;120:4172–4181. doi: 10.1182/blood-2012-06-437608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ortiz AM, Klatt NR, Li B, Yi Y, Tabb B, Hao XP, Sternberg L, Lawson B, Carnathan PM, Cramer EM, Engram JC, Little DM, Ryzhova E, Gonzalez-Scarano F, Paiardini M, Ansari AA, Ratcliffe S, Else JG, Brenchley JM, Collman RG, Estes JD, Derdeyn CA, Silvestri G. Depletion of CD4(+) T cells abrogates post-peak decline of viremia in SIV-infected rhesus macaques. The Journal of clinical investigation. 2011;121:4433–4445. doi: 10.1172/JCI46023. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.