Abstract
Objective
Living in adverse neighborhood conditions has been linked with greater prevalence of cardiovascular disease (CVD). We aimed to learn whether perceived neighborhood problems are related to attenuated nocturnal blood pressure (BP) dipping, a risk factor for CVD morbidity.
Method
A sample of 133 adults (71 male, 62 female; 80 White, 53 Black) underwent 24-hr ambulatory blood pressure monitoring. The neighborhood problem scale (NPS) was used to assess neighborhood environmental stressors.
Results
Nocturnal dipping in systolic (SBP), diastolic (DBP) and mean arterial (MAP) blood pressure was reduced in individuals with higher NPS scores (p < .05). Hierarchical regression analyses revealed that neighborhood problems explained 4%–6% of the variance in SBP, DBP, and MAP dipping (p < .05) even after adjusting for several theoretical confounders such as social status, age, gender, race, body mass index (BMI), smoking, exercise, depression and discrimination.
Conclusion
Neighborhood problems may contribute to attenuated BP dipping beyond the effect of known risk factors.
Keywords: nocturnal blood pressure dipping, neighborhood problems, hypertension, cardiovascular disease, environmental stressors
Several studies have linked adverse neighborhood conditions with cardiovascular disease (CVD) risk factors and greater prevalence of CVD morbidity (Chaix, 2009; Chaix et al., 2010; Diez Roux, 2007; Diez Roux et al., 2001). Most of these studies have characterized the neighborhood status in terms of aggregate measures of socioeconomic status (SES) or indices of deprivation constructed by combined aggregate measures (Diez Roux, 2001). A different view on relationships between neighborhood and health has been provided by evaluating individuals’ experience of adverse neighborhood conditions in terms of perceived neighborhood problems (Elo, Mykyta, Margolis, & Culhane, 2009; Steptoe & Feldman, 2001). Researchers have developed scales to assess the self-reported severity of neighborhood characteristics such as safety, litter, noise, poor availability of services, vandalism, or poor social cohesion—all of which may relate to chronic stress. Self-reported neighborhood problems have been related to important CVD predictors/risk factors such as poor self-rated health, smoking, psychological distress, impaired physical function, higher blood pressure (BP) and depressive symptoms (Gary et al., 2008; Mujahid et al., 2008; Steptoe & Feldman, 2001; Yen, Michael, & Perdue, 2009; Yen, Yelin, Katz, Eisner, & Blanc, 2008).
Attenuated nocturnal BP dipping is considered a significant risk factor for developing CVD, hypertensive cardiovascular complications, cardiovascular organ damages, and all-cause mortality (Cuspidi et al., 2004; Fagard et al., 2009, 2008; Liu et al., 2003; Mancia et al., 2007; Palatini et al., 1992; Phillips, Sheinart, Godbold, Mahboob, & Tuhrim, 2000; Rizzoni et al., 1992). There is evidence that measures of nocturnal BP dipping can be more predictive of cardiovascular outcomes than daytime or overall BP (Ohkubo et al., 2002; Staessen et al., 1999; Thomas, Nelesen, & Dimsdale, 2004). Although associations between nocturnal BP dipping and a number of factors that may be related to neighborhood problems have been studied (e.g., global measures of perceived stress, individual/neighborhood SES, violence, discrimination) (Hickson et al., 2011; Stepnowsky, Nelesen, DeJardin, & Dimsdale, 2004; Tomfohr, Cooper, Mills, Nelesen, & Dims-dale, 2010; Wilson, Kliewer, Teasley, Plybon, & Sica, 2002), little research has been done on whether the comprehensive experience of neighborhood problems is related to nocturnal BP dipping. To address this issue, we examined association patterns between the severity of perceived neighborhood problems and nocturnal systolic blood pressure (SBP) dipping, diastolic blood pressure (DBP) dipping, and mean arterial pressure (MAP) dipping. We hypothesized that individuals with more perceived neighborhood problems would exhibit reduced nocturnal BP dipping.
Method
Participants and Procedures
Participants were volunteers from a larger study on health, stress and ethnicity. The study was approved by the University of California, San Diego (UCSD) Institutional Review Board. Patients were prescreened for eligibility and examined by a physician. They were then consented and completed a number of demographic and psychosocial assessments, including body mass index (BMI). Fifty-eight women (24 African Americans and 34 Caucasian Americans) and 68 men (27 African Americans and 41 Caucasian Americans) between 19 and 53 years underwent 24-hr ambulatory blood pressure monitoring (ABPM) during the work week (see Table 1 for sample characteristics). Participants were recruited between 2006 and 2010 using advertisements and announcements. Since we aimed to examine the relationship between neighborhood problems and BP dipping in a nonclinical sample and to reduce the likelihood of confounding variables intervening in associations of study variables, a number of exclusion criteria were applied. Exclusionary criteria were: Current diagnoses of a clinical illness other than hypertension, history of psychosis or sleep disorder, current alcohol or drug abuse, moderate or heavy smoking (>10 cigarettes/day), increased caffeine intake (>600 mg/day), hormonal medication (including the contraceptive pill or hormone replacement therapy), BP ≥170/105 mmHg and any medication use. Two subjects with antihypertensive medication were accepted for participation and enrolled after a 3-week drug washout period supervised by the study physician.
Table 1.
Descriptive Statistics of Study Variables (N = 133)
| Age, years | 35.0 (9.9) |
| Body mass index, kg/m2 | 25.7 (4.2) |
| Females, N (%) | 62 (46.6) |
| African Americans, N (%) | 53 (39.8) |
| Caucasian Americans, N (%) | 80 (60.2) |
| Current smoker, N (%) | 15 (11.3) |
| Neighborhood Problems scale | 14.3 (3.6) |
| Socioeconomic status (Hollingshead Two-Factor Index) | 41.4 (14.9) |
| High social class: I (%) | 4 (3) |
| High-medium social class: II (%) | 23 (17.2) |
| Medium social class: III (%) | 50 (37.3) |
| Low-medium social class: IV (%) | 42 (31.2) |
| Low social class: V (%) | 15 (11.2) |
| Subjective social status (MacArthur Scale) | 5.5 (2.1) |
| Center for Epidemiologic Studies Depression Scale | 12.1 (9.3) |
| Everyday discrimination scale | 1.2 (0.9) |
| Leisure Time Exercise Questionnaire | 77.4 (144.4) |
| Awake SBP, mm Hg | 119.5 (10.3) |
| Sleep SBP, mm Hg | 105.8 (10.2) |
| SBP dipping, mm Hg | 13.7 (7.0) |
| Awake DBP, mm Hg | 74.5 (7.6) |
| Sleep DBP, mm Hg | 60.8 (8.2) |
| DBP dipping, mm Hg | 13.7 (6.3) |
| Awake MAP, mm Hg | 89.7 (7.9) |
| Sleep MAP, mm Hg | 76.2 (8.0) |
| MAP dipping, mm Hg | 13.5 (6.2) |
Note. Values shown as mean (SD) unless otherwise noted. DBP = diastolic blood pressure; MAP = mean arterial pressure; SBP = systolic blood pressure
Nocturnal BP Dipping
The ABPM device (Spacelabs Model 90207, Redmond, WA) was programmed to measure BP at 15-min intervals between 6 a.m. and 10 p.m. and at 30-min intervals between 10 p.m. and 6 a.m. ABPM readings were examined for artifacts through standard Spacelab default and visual inspection. BP readings that differed by more than 35 mmHg from one reading to the next reading were deleted (total number of valid readings, M = 69.8, SD = 11.8). Timeframes for sleep and wake were based on the participant's self-reported bedtime. Nocturnal SBP, DBP, and MAP dipping was calculated by subtracting the average of sleep readings from the average of wake readings. The described procedure generates dipping values with adequate reliability (Dimsdale et al., 2000).
Neighborhood Problems
The 10-item neighborhood problems scale (NPS) was used to measure neighborhood stressors. The NPS has been described in detail elsewhere (Steptoe & Feldman, 2001). In short, participants are asked to rate the degree of 10 neighborhood conditions that may result in chronic stress (e.g., litter, noise, poor availability of services, crime, vandalism) using a 3-point scale from 1 (not a problem) to 2 (some problem) to 3 (serious problem). Scores can range from 10 to 30, with higher scores representing greater neighborhood problems. The NPS shows acceptable to good internal consistency. Principle components analysis indicated that all items load on a single factor (Feldman & Steptoe, 2004; Steptoe & Feldman, 2001).
Covariate Measures
Socioeconomic conditions are strongly related to neighborhood problems and have been suggested to influence health in part via the perceived neighborhood strain (Feldman & Steptoe, 2004). However, socioeconomic conditions may also affect cardiovascular health through other pathways; for example, negative emotions that result from a low perceived social position (Cooper et al., 2010; Euteneuer, Mills, Rief, Ziegler, & Dimsdale, 2012; Ghaed & Gallo, 2007). Thus, socioeconomic status was considered as a covariate by calculating the Hollingshead Two-Factor Index (HTFI), a well-established indicator of socioeconomic status, which is based on weighted values (1 to 7) of education and occupation levels (Hollingshead, 1957). HTFI scores can range from 11 to 77, with lower scores representing higher SES. This social index corresponds to social class categories that are illustrated for characterization of the sample in Table 1: I (high social class); II (high-medium social class); III (medium social class); IV (low-medium social class); V (low social class). All analyses are based on the continuous HTFI scores. Since subjective measures of socioeconomic status have frequently been shown to be more strongly related to cardiovascular health outcomes than objective measures, the MacArthur Scale for Subjective Social Status was also used to assess subjective social status (Adler, Epel, Castellazzo, & Ickovics, 2000). In short, subjects are asked to rate their place on the rung of a “social ladder” in relation to those who are the best and worst off with respect to money, education, and respected jobs in the United States. Lower scores indicate lower subjective social status.
Daytime BP, sociodemographic and health-related variables such as age, race, smoking status, body mass index (BMI), depression, and everyday discrimination may influence nocturnal blood pressure dipping (Cuspidi et al., 2008; Profant & Dimsdale, 1999; Scuteri et al., 2009; Smart Richman, Pek, Pascoe, & Bauer, 2010; Spruill et al., 2009; Tomfohr et al., 2010), and may in part be confounded with perceived neighborhood problems (Feldman & Steptoe, 2004; Steptoe & Feldman, 2001; Thomas, Nelesen, Ziegler, Natarajan, & Dimsdale, 2009). Thus, these variables were also considered as control variables.
The severity of depressive symptoms was assessed with the well-established 20-item Center of Epidemiological Studies–Depression Scale (Radloff, 1977). Scores range from 0 to 60, with higher scores indicating more severe depressive symptoms. Discrimination was measured using the 10-item Everyday Discrimination Scale, which asks individuals to indicate the frequency with which they experience various forms of subtle discrimination in their daily live. Scores range from 0 to 5, with higher scores indicating greater perceived discrimination (Williams, Yu, Jackson, & Anderson, 1997). Habitual exercise was quantified through the weekly activity-score of the Godin Leisure Time Exercise Questionnaire (Godin & Shephard, 1997). This score is calculated by multiplying frequencies of weekly exercise of different intensity by 9 (strenuous), 5 (moderate), and 3 (mild); higher scores reflect more regular exercise.
Statistical Analyses
Statistical analyses were carried out with SPSS version 17.0 for Windows (Chicago, IL, SPSS, Inc.). Boxplots were used to control for extreme univariate outliers. One case was considered as a multivariate outlier (NPS and SBP/DBP/MAP dipping) on the basis of studentized deleted residuals and centered leverage values and excluded (Fox, 1991). Pearson correlation analyses were used to examine associations between study variables. A number of hierarchical regression analyses were conducted to examine if neighborhood problems explain variance in nocturnal SBP, DBP, and MAP dipping after adjusting for awake BP (Model 1), after additionally taking into account gender, age, race, and CVD risk factors (BMI, smoking status, exercise) (Model 2), and after additionally adjusting for psychosocial factors (socioeconomic status, subjective social status, depression, discrimination) (Model 3). Variance inflation factors were below 1.7 for all variables in all models indicating that multi-collinearity did not appear to be a concern.
Results
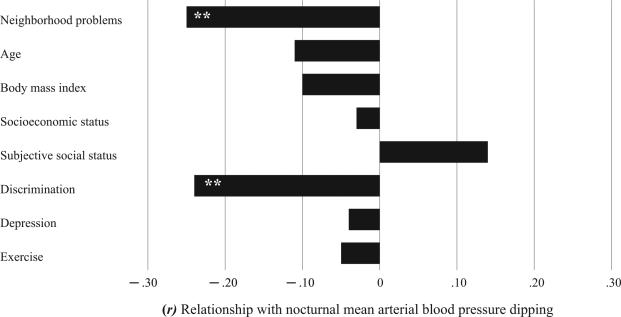
Mean values and standard deviations for all study variables are shown in Table 1. Bivariate relationships between study variables are presented in Table 2. With respect to neighborhood problems, correlation analyses revealed significant linear associations between NPS scores and nocturnal BP dipping. Individuals with higher perceived neighborhood problems exhibited reduced SBP dipping (r = –.24, p < .01), DBP dipping (r = –.25, p < .01), and MAP dipping (r = –.25, p < .01). It is noteworthy that neighborhood problems were not significantly related to awake SBP, DBP, or MAP (p > .1), but were related to higher BMI (r = .22, p < .05), lower subjective social status (r = –.23, p < .01), and greater everyday discrimination (r = .18, p < .05). With respect to BP dipping and further psychosocial variables, everyday discrimination was related to SBP dipping (r = –.21, p < .05), DBP dipping (r = –.23, p < .01), and MAP dipping (r = –.24, p < .01), while subjective social status was only related to DBP dipping (r = .21, p < .05). Figure 1 illustrates the strength of correlations between metric study variables and nocturnal BP dipping (i.e., MAP dipping).
Table 2.
Pearson Correlations (Metric Variables) and Point-Biserial Correlations (Dichotomous Variables) Between Study Variables
| Variable | Gender | Race | Smoking | Age | BMI | SES | SSS | EDS | CES-D | LTE | Awake SBP |
Sleep SBP |
SBP dipping |
Awake DBP |
Sleep DBP |
DBP dipping |
Awake MAP |
Sleep MAP |
MAP dipping |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NPS | –.08 | .25** | .07 | .10 | .22* | .02 | –.23** | .18* | .14 | –.08 | .10 | .28** | –.24** | .08 | .28** | –.25** | .09 | .30** | –.25** |
| Gender | — | –.04 | –.10 | .04 | .09 | –.02 | .20* | –.06 | –.08 | –.12 | –.40*** | .35*** | –.07 | –.19* | –.19* | .03 | –.28** | –.26** | –.01 |
| Race | — | –.19* | –.29** | –.40*** | –.23** | .20* | –.19* | –.01 | –.08 | –.05 | –.19* | .20* | [–.16] | –.33*** | .23*** | –.12 | –.29** | .22** | |
| Smoking | — | .06 | .02 | .15 | –.06 | .24** | .06 | .02 | .18* | [.16] | .03 | .19* | .23** | –.07 | .20* | .22* | –.04 | ||
| Age | — | .41*** | .00 | –.18* | –.07 | –.05 | .23 | .10 | .18* | –.11 | .27** | .37*** | [–.16] | .22* | .31*** | –.11 | |||
| BMI | — | –.12 | [–.16] | .08 | .05 | .05 | .27** | .32*** | –.08 | .24** | .33*** | –.10 | .29** | .36** | –.10 | ||||
| SES | — | –.23* | .24** | .14 | .04 | .05 | .08 | –.03 | –.06 | –.02 | –.08 | –.03 | .03 | –.03 | |||||
| SSS | — | –.30** | –.33*** | –.10 | [–.15] | –.26** | .12 | –.08 | –.28** | .21* | [–.16] | –.28** | .14 | ||||||
| EDS | — | .47*** | .10 | .06 | .21* | –.21* | –.09 | [.16] | –.23** | –.01 | .19* | –.24** | |||||||
| CES-D | — | .09 | –.05 | –.00 | –.06 | .03 | .04 | –.04 | –.02 | .01 | –.04 | ||||||||
| LTE | — | .05 | .08 | –.04 | .04 | .09 | -.06 | .06 | .11 | –.05 |
Note. BMI = body mass Index; CES-D = Center for Epidemiologic Studies Depression scale; DBP = diastolic blood pressure; EDS = Everyday Discrimination scale; LTE = Leisure time exercise; MAP = mean arterial pressure; NPS = Neighborhood Problem scale; SBP = systolic blood pressure; SES = socioeconomic status (Hollingshead Two-Factor Index); SSS = Subjective social status.
p < .05 (two-tailed)
p < .01
p < .001. p < in brackets
Figure 1.
Bar charts illustrating Pearson correlation coefficients (r) between mean arterial blood pressure dipping and metric study variables. ** p < 0.01
Hierarchical regression analyses were separately conducted for SBP, DBP, and MAP dipping. Results of the final steps, which always include neighborhood problems, are summarized in Table 3. In Model 1, NPS values were entered after adjusting for awake SBP, DBP, and MAP, respectively. Results indicated that NPS remained significantly related to SBP, DBP, and MAP dipping (p < .001) and explained 8% of the variance in SBP dipping (β = –0.29), 8% of the variance in DBP dipping (β = –0.29), and 9% of the variance in MAP dipping (β = –0.29). When additionally adjusting for age, gender, race, and CVD risk factors (BMI, smoking status, exercise) (Model 2), NPS remained significantly related to BP dipping (p < .01) and explained 6% of the variance in SBP dipping (β = –0.25), 5% of the variance in DBP dipping (β = –0.24), and 5% of the variance in MAP dipping (β= –0.24). In this model, gender also was significantly related to MAP dipping (β= 0.17, p < .05).
Table 3.
Regression of Neighborhood Problems on Nocturnal Blood Pressure Dipping After Adjusting for Theoretical Confounders
| Independent variable: |
Dependent variable: Nocturnal blood pressure dipping |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Neighborhood Problems scale | systolic |
diastolic |
mean |
||||||
| β | R2 | Δ R2 | β | R2 | Δ R2 | β | R2 | Δ R2 | |
| Model 1, adjusted for Awake blood pressurea | –0.29 | 0.26 | 0.08*** | –0.29 | 0.21 | 0.08*** | –0.29 | 0.27 | 0.09*** |
| Model 2, adjusted for Awake blood pressurea | –0.25 | 0.31 | 0.06** | –0.24 | 0.32 | 0.05** | –0.24 | 0.35 | 0.05** |
| Age, gender, race | |||||||||
| CVD risk factorsb | |||||||||
| Model 3, adjusted for Awake blood pressurea | –0.26 | 0.42 | 0.06** | –0.21 | 0.40 | 0.04* | –0.22 | 0.46 | 0.04** |
| Age, gender, race | |||||||||
| CVD risk factorsb | |||||||||
| Psychosocial confoundersc | |||||||||
Note. β = standardized regression coefficient; R2 = total variance explained by the model; ΔR2 = variance explained by neighborhood problems after adjusting for confounders.
systolic dipping is adjusted for awake systolic blood pressure, diastolic dipping is adjusted for awake diastolic blood pressure, mean dipping is adjusted for awake mean arterial pressure.
Cardiovascular disease risk factors: body mass index, leisure time exercise, and smoking status.
Socioeconomic status (Hollingshead Two-Factor Index), subjective social status, depression, and everyday discrimination.
p < .05 (two-tailed)
p < .01.
p < .001. p < .1 in brackets
Since we wanted to examine whether neighborhood problems explain variance in BP dipping beyond what was accounted for by known sociodemographic and psychosocial measures, we ran further regression analyses: Model 3 was additionally adjusted for social status (socioeconomic status, subjective social status) and psychological factors (depression, discrimination). After taking these covariates into account, NPS remained significantly related to SBP, DBP, and MAP dipping respectively (p < .05), and explained 6% of the variance in SBP dipping (β = –0.26), 4% of the variance in DBP dipping (β = –0.21), and 4% of the variance in MAP dipping (β = –0.22). SBP dipping (β = –0.28, p < .01), DBP dipping (β = –0.22, p < .05), and MAP dipping (β= –0.27, p < .01) were also related to discrimination. Moreover, DBP dipping was predicted by age (β = –0.21, p < .05) and MAP dipping was predicted by gender (β= 0.16, p < .05).
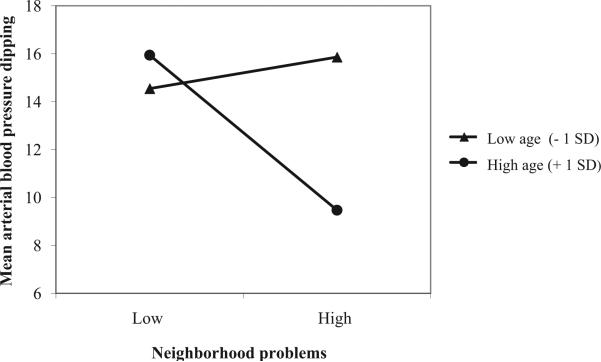
Finally, a number of exploratory moderation analyses were conducted to examine whether there are significant interactions between neighborhood problems and potential covariates (gender, age, race, CVD risk factor, and psychosocial variables) in the prediction of BP dipping. Interaction terms of centered NPS scores and centered (or dummy coded) study variables were entered on step 3 after accounting for the effect of both variables on step 2 and awake SBP, DBP, or MAP on step 1. These moderation analyses were rerun with the remaining covariates on step 1. Results indicated that interaction terms did not significantly explain additional variance (p > .1; results of nonsignificant exploratory analyses not shown) with one exception: NPS × age interaction terms accounted for significant increments of variance in SBP dipping (β = –0.21, p < .01, ΔR2 = 0.04), DBP dipping (β = –0.30, p < .001, ΔR2 = 0.09), and MAP dipping (β = –0.29, p < .001, ΔR2 = 0.08) beyond what was accounted for by age, NPS, and awake BP. Figure 2 illustrates the significant NPS × age interaction for the prediction of MAP dipping by plotting the relationship between NPS scores and MAP dipping at low age (one standard deviation below mean) and at high age (one standard deviation above mean) (Aiken & West, 1991). NPS × age interaction terms remained significantly related to SBP dipping (β = –0.16, p < .05, ΔR2 = 0.02), DBP dipping (β = –0.28, p < .001, ΔR2 = 0.07), and MAP dipping (β = –0.26, p < .01, ΔR2 = 0.06) after additionally accounting for gender, race, CVD risk factor, and psychosocial variables.
Figure 2.
Age as a moderator of the relation between neighborhood problems (neighborhood problem scale) and nocturnal mean arterial blood pressure dipping (adjusted for awake mean arterial blood pressure). *** p < 0.001.
Discussion
The aim of this study was to examine whether perceived neighborhood problems are related to attenuated nocturnal BP dipping, a risk factor for CVD morbidity and mortality (Cuspidi et al., 2004; Fagard et al., 2009, 2008; Liu et al., 2003; Mancia et al., 2007; Palatini et al., 1992; Phillips et al., 2000; Rizzoni et al., 1992). Our main finding is that nocturnal SBP, DBP, and MAP dippings are reduced in individuals with more severe self-reported neighborhood problems. These relationships persisted after adjusting for several theoretical covariates including social status, age, gender, race, BMI, smoking, exercise, depression, and discrimination. Thus, our findings support previous research showing that perceived neighborhood problems are related to cardiovascular risk factors (Gary et al., 2008; Mujahid et al., 2008; Steptoe & Feldman, 2001; Yen et al., 2008). To our knowledge, this is the first study that examined associations between perceived neighborhood problems and nocturnal BP dipping.
Interaction analyses indicated that the relationship between perceived neighborhood problems and BP dipping strengthens with increasing age. A potential explanation for this finding might be that diurnal BP regulation in older individuals is more sensitive to environmental stressors such as poor neighborhood conditions. This would be in line with the notion of age as an important CVD risk factor, a decline of coping abilities with age, and previous findings of increasing autonomic responsiveness to stressors with age (Chobanian et al., 2003; Folkman, Lazarus, Pimley, & Novacek, 1987; Garwood, Engel, & Capriotti, 1982; Palmer, Ziegler, & Lake, 1979; Steptoe, Moses, & Edwards, 1990). A further explanation might be that the prolonged perception of poor neighborhood conditions may be of relevance, and that older individuals have been exposed to their neighborhood for a longer time. Because we have not longitudinally assessed perceived neighborhood problems and BP dipping, these explanations are speculative and further research is necessary to clarify this issue.
There are diverse pathways linking adverse social environmental conditions with poor health outcomes. Health behavior (i.e., smoking, physical inactivity, poor diet) and psychophysiological mechanisms (i.e., chronic stress) have been regarded as very important mediators (Adler & Matthews, 1994; Ross, 2000; Steptoe & Feldman, 2001). With respect to health behavior, we found a relationship of perceived neighborhood problems with BMI (r = .22, p < .05) but not with smoking or leisure time exercise (p > .1). It is noteworthy that a lack of associations between smoking and both neighborhood problems and BP dipping may be due to the reduced range of smokers because people who smoke more than 10 cigarettes per day were not included in this study. However, in a previous study using the NPS, neighborhood problems were also not significantly related to health behavior factors such as smoking, diet, alcohol consumption, or physical activity (Steptoe & Feldman, 2001). Moreover, in our study the relationship between neighborhood problems and BP dipping remained significant after taking into account health behavior factors. In sum, these findings confirm the suggestion that psychophysiological mechanisms may link neighborhood conditions and health, at least in part, independent from health behaviors. Possible mechanisms that underlie this association are speculative but may involve several stress-related features that have also been shown to affect diurnal blood pressure regulation such as autonomic imbalance, neurohormonal alterations (e.g., decreased diurnal variation in cortisol and catecholamines), and sleep disruptions (Holt-Lunstad & Steffen, 2007; Yano & Kario, 2012).
It might be relevant to note the absence of relations between BP dipping and study variables previously shown to be associated with BP dipping. For example, socioeconomic status has been related to BP dipping earlier (Fortmann et al., 2012; Rodriguez et al., 2013; Stepnowsky et al., 2004). In the present study, we have used the HTFI as a well-established weighted measure of socioeconomic status that combines levels of occupation and education (see methods section). Although the HTFI was not related to BP dipping, exploratory analyses indicated that not occupation (p > .1) but education was indeed related to BP dipping: Participants with lower education exhibited reduced SBP dipping (r = –.18, p < .05), DBP dipping (r = –.19, p < .05), and MAP dipping (r = –.18, p < .05). Thus inconsistent findings may in part result from different indicators of socioeconomic status. Regarding BMI, it is unclear why some studies found a link to BP dipping (e.g., Cuspidi et al., 2008; Stepnowsky et al., 2004), while our and other data did not indicate this association (e.g., Loredo, Ancoli-Israel, & Dimsdale, 2001; Rodriguez et al., 2013), and further research is necessary to clarify this issue.
Our findings are limited because our cross-sectional design allows no causal interpretation. Prospective studies that focus on the longitudinal relationship between neighborhood problems and nocturnal BP dipping, changing neighborhood conditions, and possibly on the mediating role of BP dipping between neighborhood conditions and cardiovascular outcomes may be promising. A further important limitation is the generalizability of our findings. Since we have examined the relationship between perceived neighborhood problems and BP dipping in a nonclinical sample of African Americans and Caucasian Americans, it would be of interest if the observed associations are also prominent in clinical populations (e.g., CVD patients) or other ethnic groups. An additional limitation is that we have only assessed perceived neighborhood problems. Although self-reported neighborhood measures have been shown to be highly reliable (Elo et al., 2009), inclusion of additional objective neighborhood factors (e.g., neighborhood socioeconomic status or indices for quality of health care) may be beneficial.
In conclusion, our findings suggest that neighborhood problems may contribute to attenuated BP dipping beyond the effect of known risk factors.
Acknowledgments
This work was supported, in part, by Grants HL36005, HL57269, HL44915 and 1UL1RR031980 from the National Institutes of Health (J.E.D.).
Contributor Information
Frank Euteneuer, Department of Psychiatry, University of California, San Diego and Division of Clinical Psychology and Psychotherapy, Philipps Universität, Marburg, Germany.
Winfried Rief, Division of Clinical Psychology and Psychotherapy, Philipps Universität, Marburg, Germany.
Paul J. Mills, Department of Psychiatry, University of California, San Diego
Meredith A. Pung, Department of Psychiatry, University of California, San Diego
Joel E. Dimsdale, Department of Psychiatry, University of California, San Diego.
References
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy White women. Health Psychology. 2000;19:586–592. doi: 10.1037//0278-6133.19.6.586. doi:10.1037/0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Adler NE, Matthews K. Health psychology: Why do some people get sick and some stay well? Annual Review of Psychology. 1994;45:229–259. doi: 10.1146/annurev.ps.45.020194.001305. doi:10.1146/annurev.ps.45.020194.001305. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Thousand Oaks, CA: 1991. [Google Scholar]
- Chaix B. Geographic life environments and coronary heart disease: A literature review, theoretical contributions, methodological updates, and a research agenda. Annual Review of Public Health. 2009;30:81–105. doi: 10.1146/annurev.publhealth.031308.100158. doi:10.1146/annurev.publhealth.031308.100158. [DOI] [PubMed] [Google Scholar]
- Chaix B, Bean K, Leal C, Thomas F, Havard S, Evans D, Pannier B. Individual/neighborhood social factors and blood pressure in the RECORD Cohort study: Which risk factors explain the associations? Hypertension. 2010;55:769–775. doi: 10.1161/HYPERTENSIONAHA.109.143206. doi:10.1161/HYPER-TENSIONAHA.109.143206. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, National High Blood Pressure Education Program Coordinating Committee The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Journal of the American Medical Association. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. doi:10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- Cooper DC, Milic MS, Mills PJ, Bardwell WA, Ziegler MG, Dimsdale JE. Endothelial function: The impact of objective and subjective socioeconomic status on flow-mediated dilation. Annals of Behavioral Medicine. 2010;39:222–231. doi: 10.1007/s12160-010-9181-9. doi:10.1007/s12160-010-9181-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuspidi C, Meani S, Salerno M, Valerio C, Fusi V, Severgnini B, Zanchetti A. Cardiovascular target organ damage in essen tial hypertensives with or without reproducible nocturnal fall in blood pressure. Journal of Hypertension. 2004;22:273–280. doi: 10.1097/00004872-200402000-00010. doi:10.1097/00004872-200402000-00010. [DOI] [PubMed] [Google Scholar]
- Cuspidi C, Meani S, Valerio C, Negri F, Sala C, Maisaidi M, Mancia G. Body mass index, nocturnal fall in blood pressure and organ damage in untreated essential hypertensive patients. Blood Pressure Monitoring. 2008;13:318–324. doi: 10.1097/MBP.0b013e32830d4bf8. doi:10.1097/MBP.0b013e32830d4bf8. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV. Investigating neighborhood and area effects on health. American Journal of Public Health. 2001;91:1783–1789. doi: 10.2105/ajph.91.11.1783. doi:10.2105/AJPH.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux A-V. Neighborhoods and health: Where are we and where do we go from here? Revue d'Épidémiologie et de Santé Publique. 2007;55:13–21. doi: 10.1016/j.respe.2006.12.003. doi:10.1016/j.respe.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Watson RL. Neighborhood of residence and incidence of coronary heart disease. The New England Journal of Medicine. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. doi:10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- Dimsdale JE, Von Känel R, Profant J, Nelesen R, Ancoli-Israel S, Ziegler M. Reliability of nocturnal blood pressure dipping. Blood Pressure Monitoring. 2000;5:217–221. doi: 10.1097/00126097-200008000-00004. doi:10.1097/00126097-200008000-00004. [DOI] [PubMed] [Google Scholar]
- Elo IT, Mykyta L, Margolis R, Culhane JF. Perceptions of neighborhood disorder: The role of individual and neighborhood characteristics. Social Science Quarterly. 2009;90:1298–1320. doi: 10.1111/j.1540-6237.2009.00657.x. doi:10.1111/j.1540-6237.2009.00657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euteneuer F, Mills PJ, Rief W, Ziegler MG, Dimsdale JE. Subjective social status predicts in vivo responsiveness of [H9252]-adrenergic receptors. Health Psychology. 2012;31:525–529. doi: 10.1037/a0025990. doi:10.1037/a0025990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagard RH, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Night-day blood pressure ratio and dipping pattern as predictors of death and cardiovascular events in hypertension. Journal of Human Hypertension. 2009;23:645–653. doi: 10.1038/jhh.2009.9. doi:10.1038/jhh.2009.9. [DOI] [PubMed] [Google Scholar]
- Fagard RH, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Prognostic significance of ambulatory blood pressure in hypertensive patients with history of cardiovascular disease. Blood Pressure Monitoring. 2008;13:325–332. doi: 10.1097/MBP.0b013e32831054f5. doi:10.1097/MBP.0b013e32831054f5. [DOI] [PubMed] [Google Scholar]
- Feldman PJ, Steptoe A. How neighborhoods and physical functioning are related: The roles of neighborhood socioeconomic status, perceived neighborhood strain, and individual health risk factors. Annals of Behavioral Medicine. 2004;27:91–99. doi: 10.1207/s15324796abm2702_3. doi:10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS, Pimley S, Novacek J. Age differences in stress and coping processes. Psychology and Aging. 1987;2:171–184. doi: 10.1037//0882-7974.2.2.171. doi:10.1037/0882-7974.2.2.171. [DOI] [PubMed] [Google Scholar]
- Fortmann AL, Gallo LC, Roesch SC, Mills PJ, Barrett-Connor E, Talavera GA, Matthews KA. Socioeconomic status, nocturnal blood pressure dipping, and psychosocial factors: A cross-sectional investigation in Mexican-American women. Annals of Behavioral Medicine. 2012;44:389–398. doi: 10.1007/s12160-012-9387-0. doi:10.1007/s12160-012-9387-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox J. Regression diagnostics: An introduction. Sage publications; Newbury Park, CA: 1991. [Google Scholar]
- Garwood M, Engel BT, Capriotti R. Autonomic nervous system function and aging: Response specificity. Psychophysiology. 1982;19:378–385. doi: 10.1111/j.1469-8986.1982.tb02491.x. doi:10.1111/j.1469-8986.1982.tb02491.x. [DOI] [PubMed] [Google Scholar]
- Gary TL, Safford MM, Gerzoff RB, Ettner SL, Karter AJ, Beckles GL, Brown AF. Perception of neighborhood problems, health behaviors, and diabetes outcomes among adults with diabetes in managed care: The Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care. 2008;31:273–278. doi: 10.2337/dc07-1111. doi:10.2337/dc07-1111. [DOI] [PubMed] [Google Scholar]
- Ghaed SG, Gallo LC. Subjective social status, objective socioeconomic status, and cardiovascular risk in women. Health Psychology. 2007;26:668–674. doi: 10.1037/0278-6133.26.6.668. doi:10.1037/0278-6133.26.6.668. [DOI] [PubMed] [Google Scholar]
- Godin G, Shephard RJ. Godin Leisure-Time Exercise Questionnaire. Medicine and Science in Sports and Exercise. 1997;29:36–38. doi:10.1097/00005768-199706001-00009. [Google Scholar]
- Hickson DA, Diez Roux AV, Wyatt SB, Gebreab SY, Ogedegbe G, Sarpong DF, Wofford MR. Socioeconomic position is positively associated with blood pressure dipping among African-American adults: The Jackson Heart Study. American Journal of Hypertension. 2011;24:1015–1021. doi: 10.1038/ajh.2011.98. doi:10.1038/ajh.2011.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Two factor index of social position. Yale University Press; New Haven, CT: 1957. [Google Scholar]
- Holt-Lunstad J, Steffen PR. Diurnal cortisol variation is associated with nocturnal blood pressure dipping. Psychosomatic Medicine. 2007;69:339–343. doi: 10.1097/PSY.0b013e318050d6cc. doi:10.1097/PSY.0b013e318050d6cc. [DOI] [PubMed] [Google Scholar]
- Liu M, Takahashi H, Morita Y, Maruyama S, Mizuno M, Yuzawa Y, Matsuo S. Non-dipping is a potent predictor of cardiovascular mortality and is associated with autonomic dysfunction in haemodialysis patients. Nephrology, Dialysis, Transplantation. 2003;18:563–569. doi: 10.1093/ndt/18.3.563. doi:10.1093/ndt/18.3.563. [DOI] [PubMed] [Google Scholar]
- Loredo JS, Ancoli-Israel S, Dimsdale JE. Sleep quality and blood pressure dipping in obstructive sleep apnea. American Journal of Hypertension. 2001;14:887–892. doi: 10.1016/s0895-7061(01)02143-4. doi:10.1016/S0895-7061(01)02143-4. [DOI] [PubMed] [Google Scholar]
- Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Zamorano JL. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). European Heart Journal. 2007;28:1462–1536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, Shea S. Neighborhood characteristics and hypertension. Epidemiology. 2008;19:590–598. doi: 10.1097/EDE.0b013e3181772cb2. doi:10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Imai Y. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: The Ohasama study. Journal of Hypertension. 2002;20:2183–2189. doi: 10.1097/00004872-200211000-00017. doi:10.1097/00004872-200211000-00017. [DOI] [PubMed] [Google Scholar]
- Palatini P, Penzo M, Racioppa A, Zugno E, Guzzardi G, Anaclerio M, Pessina AC. Clinical relevance of nighttime blood pressure and of daytime blood pressure variability. Archives of Internal Medicine. 1992;152:1855–1860. doi:10.1001/archinte.1992.00400210081013. [PubMed] [Google Scholar]
- Palmer GJ, Ziegler MG, Lake CR. Response of norepinephrine and blood pressure to stress increases with age. Journal of Gerontology. 1978;33:482–487. doi: 10.1093/geronj/33.4.482. doi:10.1093/geronj/33.4.482. [DOI] [PubMed] [Google Scholar]
- Phillips RA, Sheinart KF, Godbold JH, Mahboob R, Tuhrim S. The association of blunted nocturnal blood pressure dip and stroke in a multiethnic population. American Journal of Hypertension. 2000;13:1250–1255. doi: 10.1016/s0895-7061(00)01217-6. doi:10.1016/S0895-7061(00)01217-6. [DOI] [PubMed] [Google Scholar]
- Profant J, Dimsdale JE. Race and diurnal blood pressure patterns. A review and meta-analysis. Hypertension. 1999;33:1099–1104. doi: 10.1161/01.hyp.33.5.1099. doi:10.1161/01.HYP.33.5.1099. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale. Applied Psychological Measurement. 1977;1:385–401. doi:10.1177/014662167700100306. [Google Scholar]
- Rizzoni D, Muiesan ML, Montani G, Zulli R, Calebich S, Agabiti-Rosei E. Relationship between initial cardiovascular structural changes and daytime and nighttime blood pressure monitoring. American Journal of Hyper-tension. 1992;5:180–186. doi: 10.1093/ajh/5.3.180. doi:10.1093/ajh/5.3.180. [DOI] [PubMed] [Google Scholar]
- Rodriguez CJ, Jin Z, Schwartz JE, Turner-Lloveras D, Sacco RL, Di Tullio MR, Homma S. Socioeconomic status, psychosocial factors, race and nocturnal blood pressure dipping in a Hispanic cohort. American Journal of Hypertension. 2013;26:673–682. doi: 10.1093/ajh/hpt009. doi:10.1093/ajh/hpt009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CE. Walking, exercising, and smoking: Does neighborhood matter? Social Science & Medicine (1982) 2000;51:265–274. doi: 10.1016/s0277-9536(99)00451-7. [DOI] [PubMed] [Google Scholar]
- Scuteri A, Spalletta G, Cangelosi M, Gianni W, Assisi A, Brancati AM, Volpe M. Decreased nocturnal systolic blood pressure fall in older subjects with depression. Aging Clinical and Experimental Research. 2009;21:292–297. doi: 10.1007/BF03324918. [DOI] [PubMed] [Google Scholar]
- Smart Richman L, Pek J, Pascoe E, Bauer DJ. The effects of perceived discrimination on ambulatory blood pressure and affective responses to interpersonal stress modeled over 24 hours. Health Psychology. 2010;29:403–411. doi: 10.1037/a0019045. doi:10.1037/a0019045. [DOI] [PubMed] [Google Scholar]
- Spruill TM, Gerin W, Ogedegbe G, Burg M, Schwartz JE, Pickering TG. Socioeconomic and psychosocial factors mediate race differences in nocturnal blood pressure dipping. American Journal of Hypertension. 2009;22:637–642. doi: 10.1038/ajh.2009.58. doi:10.1038/ajh.2009.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staessen JA, Thijs L, Fagard R, O'Brien ET, Clement D, De Leeuw PW, Webster J. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. JAMA: Journal of the American Medical Association. 1999;282:539–546. doi: 10.1001/jama.282.6.539. doi:10.1001/jama.282.6.539. [DOI] [PubMed] [Google Scholar]
- Stepnowsky CJ, Nelesen RA, DeJardin D, Dimsdale JE. Socioeconomic status is associated with nocturnal blood pressure dipping. Psychosomatic Medicine. 2004;66:651–655. doi: 10.1097/01.psy.0000138124.58216.6c. doi:10.1097/01.psy.0000138124.58216.6c. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23:177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Moses J, Edwards S. Age-related differences in cardiovascular reactions to mental stress tests in women. Health Psychology. 1990;9:18–34. doi: 10.1037//0278-6133.9.1.18. doi:10.1037/0278-6133.9.1.18. [DOI] [PubMed] [Google Scholar]
- Thomas KS, Nelesen RA, Dimsdale JE. Relationships between hostility, anger expression, and blood pressure dipping in an ethnically diverse sample. Psychosomatic Medicine. 2004;66:298–304. doi: 10.1097/01.psy.0000126196.82317.9d. doi: 10.1097/01.psy.0000126196.82317.9d. [DOI] [PubMed] [Google Scholar]
- Thomas KS, Nelesen RA, Ziegler MG, Natarajan L, Dimsdale JE. Influence of education and neighborhood poverty on pressor responses to phenylephrine in African-Americans and Caucasian-Americans. Biological Psychology. 2009;82:18–24. doi: 10.1016/j.biopsycho.2009.04.007. doi:10.1016/j.biopsycho.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomfohr L, Cooper DC, Mills PJ, Nelesen RA, Dimsdale JE. Everyday discrimination and nocturnal blood pressure dipping in Black and White Americans. Psychosomatic Medicine. 2010;72:266–272. doi: 10.1097/PSY.0b013e3181d0d8b2. doi:10.1097/PSY.0b013e3181d0d8b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Wilson DK, Kliewer W, Teasley N, Plybon L, Sica DA. Violence exposure, catecholamine excretion, and blood pressure non-dipping status in African American male versus female adolescents. Psychosomatic Medicine. 2002;64:906–915. doi: 10.1097/01.psy.0000024234.11538.d3. [DOI] [PubMed] [Google Scholar]
- Yano Y, Kario K. Nocturnal blood pressure, morning blood pressure surge, and cerebrovascular events. Current Hypertension Reports. 2012;14:219–27. doi: 10.1007/s11906-012-0261-z. doi:10.1007/s11906-012-0261-z. [DOI] [PubMed] [Google Scholar]
- Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: A systematic review. American Journal of Preventive Medicine. 2009;37:455–63. doi: 10.1016/j.amepre.2009.06.022. doi:10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen IH, Yelin E, Katz P, Eisner MD, Blanc PD. Impact of perceived neighborhood problems on change in asthma-related health outcomes between baseline and follow-up. Health & Place. 2008;14:468–477. doi: 10.1016/j.healthplace.2007.09.003. doi:10.1016/j.healthplace.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]