Abstract
Smokers who inhabit social contexts with a greater number of smokers may be exposed to more positive norms towards smoking and more cues to smoke. This study examines the relation between number of smoking friends and changes in number of smoking friends, and smoking cessation outcomes. Data were drawn from Wave 1 (2002) and Wave 2 (2003) of the International Tobacco Control (ITC) Project Four Country Survey, a longitudinal cohort survey of nationally representative samples of adult smokers in Australia, Canada, United Kingdom, and United States (N=6,321). Smokers with fewer smoking friends at Wave 1 were more likely to intend to quit at Wave 1 and were more likely to succeed in their attempts to quit at Wave 2. Compared to smokers who experienced no change in their number of smoking friends, smokers who lost smoking friends were more likely to intend to quit at Wave 2, attempt to quit between Wave 1 and Wave 2, and succeed in their quit attempts at Wave 2. Smokers who inhabit social contexts with a greater number of smokers may be less likely to successfully quit. Quitting may be particularly unlikely among smokers who do not experience a loss in the number of smokers in their social context.
Keywords: smoking cessation, tobacco, social context, social network
Introduction
Smoking remains the leading preventable cause of morbidity and mortality in high-income countries (World Health Organization, 2009). The vast majority of smokers regret ever starting to smoke (Fong et al., 2004). Most smokers want to quit, however quitting smoking remains difficult (Centers for Disease Control and Prevention, 2011; Hughes & Keely, 2004). In 2010 in the United States, 52.4% of smokers attempted to quit, and 6.2% successfully quit (Centers for Disease Control and Prevention, 2011). There is nearly universal agreement that the primary reason that quitting is difficult is because of the addictiveness of nicotine in cigarettes, and nicotine dependence is the most consistent predictor of failure in quit attempts (Benowitz, 2010; Jarvis, 2004; US Surgeon General, 2010; Vangeli, Stapleton, Smit, Borland, & West, 2011).
Although nicotine addiction maintains smoking behavior, there is evidence that the social context also plays a role. Differences in smoking prevalence and cessation rates by country (Lopez, Collishaw, & Piha, 1994; World Health Organization, 2011), and within countries by gender (Hitchman & Fong, 2011) and by socioeconomic status suggest that the social context may exert powerful effects (Cavelaars, Kunst, Geurts, & Crialesi, 2000; Cummings, Fong, & Borland, 2009; Jarvis & Wardle, 2006). Individual smoking behavior and intensity of smoking also vary across social situations (Farkas, Gilpin, Distefan, & Pierce, 1999; Shiffman & Rathbun, 2011; Shiffman et al., 2002). Moreover, the presence of others’ smoking often precedes lapse/relapse to smoking following a quit attempt (O’Connell, Shiffman, & Decarlo, 2011; Shiffman et al., 2002; Shiffman, Paty, Gnys, Kassel, & Hickcox, 1996). To be sure, nicotine addiction and the social context, including cues to smoke, work together and affect smoking behavior in complex ways; research on nicotine addiction suggests that if people smoke around other smokers and smoking-related objects that these contextual features can become associated with the addiction, and act as cues for continued smoking (Benowitz, 2010).
Despite the apparent impact of the social context on smoking, there is only some research on how smokers in a person’s social context (particularly number of smoking friends) may be related to quit success, and even less research on how changes in smoking friends may be related to smoking cessation outcomes. Biener, Hamilton, Siegel, & Sullivan, (2010) commented that “although it seems an important socio-cultural factor, there is surprisingly little information about the role of smoking among one’s friends as a factor in adult cessation” (p.547). Interpersonal relationships are critical to daily life, and the desire to maintain these relationships is regarded as fundamental to human motivation; hence, the role of this socio-cultural factor in smoking cessation needs to be better understood (Baumeister, 1995).
Smokers who inhabit a social context with a greater number of smokers could be less likely to quit for several reasons. Smokers with more smoking friends may be exposed to more smoking cues during quit attempts, increasing the potential for relapse (Shiffman, 2005). Smokers with more smoking friends may also be exposed to more positive norms towards smoking, and may be less motivated to attempt to quit (Borland et al., 2010; Christakis & Fowler, 2009; Levine & Moreland, 2006). They may also have less social support to quit, including less access to information through their social networks about effective cessation strategies (Valente, 2011; Westmaas, Bontemps-Jones, & Bauer, 2010). Indeed, number of smoking friends may provide the social context for one or more of the above factors to operate.
Population studies using longitudinal data suggest that smokers with more smoking friends are less likely to quit (Biener et al., 2010; Herd, Borland, & Hyland, 2009; Levy, Biener, & Rigotti, 2009; Osler & Prescott, 1998). Other longitudinal studies also show that smokers who live with other smokers are less likely to quit (Chandola, Head, & Bartley, 2004; Hyland et al., 2004; Hymowitz et al., 1997), and one study found that smokers who were often in the presence of other smokers were less likely to succeed in their quit attempts (Zhou et al., 2009).
Although the relation between smokers’ number of smoking friends at baseline and some smoking cessation outcomes has been considered, less attention has been paid to how changes in a smokers’ number of smoking friends over time may be related to smoking cessation. A study of smoking in a large social network found that over a 32-year period, people who continued to smoke remained connected to social contacts who also smoked, and that connections between smokers and non-smokers diminished as people quit (Christakis & Fowler, 2008). Additionally, theories that can be applied to behavior change, such as PRIME, which stands for plans, responses, impulses, inhibitions, motives, and evaluations (West, 2006, 2009), emphasize the importance of transitions in motivation in the smoking cessation process (e.g., from wanting to quit to not wanting to quit), and how changes in the environment can trigger a quit attempt, or a lapse back to smoking. Population interventions to encourage quitting also focus on the need to change the environment (e.g., increase cigarette prices). Therefore it seems natural to consider whether a change in the number of smokers in a person’s social context is related to smoking cessation. Additionally, most previous studies have not considered the impact of smoking friends on the full range of smoking cessation outcomes, including quit intentions (longitudinal and cross-sectional), quit attempts, and quit attempt success.
The current study examines how both (a) smokers’ number of smoking friends at baseline, and (b) changes in smokers’ number of smoking friends over time, are related to smoking cessation outcomes, including: (a) quit intentions, (b) quit attempts, and (c) quit attempt success; this study used nationally representative longitudinal cohort samples of adult smokers from Australia, Canada, United Kingdom (UK), and United States (US). All analyses controlled for demographics and other predictors of smoking cessation.
Differences in the relation between both number of smoking friends and changes in number of smoking friends, and the smoking cessation outcomes across countries and by level of education and income (socioeconomic status; SES), and ethnicity (majority vs. minority group) were also considered. The relation between having more smoking friends and smoking cessation outcomes may be stronger for low SES and minority (non-white) populations because research suggests that they are more likely to deeply construe themselves into their social networks (be interdependent; Markus & Kitayama, 1991; Stephens, Markus, & Townsend, 2007).
Methods
Survey
The International Tobacco Control (ITC) Four Country Survey is a nationally representative longitudinal cohort survey of current adult smokers (at recruitment) in Australia, Canada, UK, and US, who were recruited using random digit dialing methods starting in 2002. Current smoking was defined as having smoked at least 100 lifetime cigarettes and having smoked at least once in the last 30 days. Further details of the methodology are available elsewhere (Fong et al., 2006; ITC Project, 2004, 2011; Thompson et al., 2006). The ITC Four Country Survey is part of the International Tobacco Control Policy Evaluation Project that consists of parallel cohort surveys of smokers and non-smokers in 22 countries.
Respondents
Respondents were drawn from Wave 1 and Wave 2 of the ITC Four Country Survey. Data collection involved Computer Assisted Telephone Interviewing, with Wave 1 data collected between October and December of 2002, and Wave 2 between May and September of 2003. A mean of 6.7 months separated the surveys. The current study used the Wave 1 – Wave 2 longitudinal sample (N=6,682) of respondents who completed both waves. The Wave 1 – Wave 2 follow-up rates were 81% in Australia, 76% in Canada, 78% in the UK, and 63% in the US. Respondents with missing or “don’t know” responses on key variables were deleted. The final sample size was (N=6,321).
Measures
The key independent variables were number of smoking friends at Wave 1, and change in number of smoking friends between Wave 1 and Wave 2 (friend change). To measure number of smoking friends, respondents were asked, “Of the five closest friends or acquaintances that you spend time with on a regular basis, how many of them are smokers (0, 1, 2, 3, 4, or 5)?” Friend change was measured as the difference between number of smoking friends at Wave 1 and number of smoking friends at Wave 2, creating an 11 category variable that ranged from a loss of five friends (−5), to no change (0), to a gain of five friends (5). From the eleven category variable, a three category variable was derived: loss vs. no change vs. gain in number of smoking friends.
Demographic Characteristics at Wave 1
Demographic measures included country (Australia, Canada, UK, and US), sex, age group (18–24, 25–39, 40–54, or 55+), education (low=high school or less; medium=technical, trade school, or community college (some or completed), or some university; and high=at least a university degree), employment outside the home (yes/no), ethnicity, and annual household income. Ethnicity was defined as white (majority group) vs. non-white (minority group) in Canada, the UK, and the US, and as English spoken in the home (majority group) vs. language other than English (minority group) in Australia. For UK, income was categorized as: low = under £30,000, moderate = £30,000–£44,999, and high = £45,000 or higher. Because there were a large number of ‘don’t know’/refusals for income, a fourth category was coded for these responses (‘no answer’).
Smoking cessation predictor variables at Wave 1
Smoking cessation predictor variables included smoking status (daily vs. non-daily), heaviness of smoking index (HSI, a measure of nicotine dependence), quit attempt in last year (yes vs. no), intentions to quit, longest quit attempt (never, one week or less, more than one week but less than six months, or six months or more), outcome expectancy of quitting, and worry that smoking will damage health. HSI is a composite measure of cigarettes per day (0–10, 11–20, 21–30, or >30), and minutes to first cigarette after waking (<5, 6–30, 31–60, or >60), with higher scores (range of 0 – 6) signifying greater nicotine dependence (Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989). To measure intentions to quit, smokers were asked if they were planning to quit smoking, and answers were coded as indicating: intention to quit (in next month, in next six months) vs. no intention (intention to quit beyond six months, not planning to quit, or don’t know). To assess positive outcome expectancies of quitting, respondents were asked: how much do you think you would benefit from health and other gains if you were to quit smoking permanently in the next six months…not at all, slightly, moderately, very much, or extremely? For worry that smoking would damage their health, respondents were asked: How worried are you, if at all, that smoking will damage your health in the future…not at all worried, a little worried, moderately worried, or very worried?
Smoking Cessation Outcomes
Smoking cessation outcomes included: intentions to quit smoking at Wave 1 and 2, quit attempt between Wave 1 and Wave 2, and quit attempt success. The same measure for intentions to quit that is described above for Wave 1 was used again at Wave 2. For quit attempts, respondents were asked if they had made any attempts to stop smoking since Wave 1 (attempt vs. no attempt to quit). Among smokers who attempted to quit between Wave 1 and Wave 2, quit attempt success was defined as having been quit for at least one month at the Wave 2 interview date.
Analyses
All measures were treated as categorical variables. The exceptions were (1) Heaviness of Smoking Index (HSI), (2) outcome expectancy of quitting, and (3) worried smoking will damage health, which were treated as continuous variables.
Analyses were conducted using SAS 9.2. Survey weights were computed using estimated population values from national benchmark surveys. The longitudinal Wave 1 – Wave 2 survey weights used in the current analysis were adjusted for Wave 1-Wave 2 attrition. Further details on weight construction are available elsewhere (Fong et al., 2006; ITC Project, 2004, 2011; Thompson et al., 2006).
Logistic regression analyses were used to examine the relation between the smoking cessation outcomes and both number of smoking friends at Wave 1, and changes in number of smoking friends between Wave 1 and Wave 2. Note that the relation between intentions to quit at Wave 1 and changes in smoking friends between Wave 1 and Wave 2 was not examined, and is being explored in a forthcoming publication.
For models predicting each smoking cessation outcome, a different analytic sample was used: intentions to quit at Wave 1 and quit attempts at Wave 2 included all respondents (N=6,321); intentions to quit at Wave 2 included respondents who were still smoking at Wave 2 (N=5,739); and quit attempt success at Wave 2 included only respondents who made a quit attempt between Wave 1 and Wave 2 (N=2,308). Interactions were tested using the method described by Jaccard (2001) to determine whether the relation between both number of smoking friends and changes in number of smoking friends and the smoking cessation outcomes differed across countries and by SES (education and income).
All analyses used logistic regression, and controlled for demographics and smoking cessation predictor variables. Because number of smoking friends at Wave 1 was predictive of number of smoking friends at Wave 2, all analyses that included friend change, included number of smoking friends at Wave 1 as a covariate.
Results
Key sample characteristics
Key sample characteristics are presented in Table 1. Although the three category friend change variable was used in all analyses (loss vs. no change vs. gain), the frequencies for the eleven category variable are presented to illustrate the variable’s distribution. Differences between respondents in this study (Wave 1 – Wave 2 sample) and those lost to follow-up at Wave 2 were examined for the characteristics in Table 1, and intentions to quit. Respondents with the following characteristics were more likely to be lost to follow-up: from the US, younger, minority group (except UK), low education (Canada and US), males (US), and respondents with more smoking friends. There were no significant differences in follow-up for intentions to quit or smoking status.
Table 1.
Key Characteristics of Wave 1 – Wave 2 Longitudinal Sample (N=6,321, unweighted)
| Variable | Country | |||||||
|---|---|---|---|---|---|---|---|---|
| Australia (N=1,748) |
Canada (N=1,595) |
United Kingdom (N=1,714) |
United States (N=1,264) |
|||||
| n | % | n | % | n | % | n | % | |
| Sex | ||||||||
| Female | 942 | 53.9% | 885 | 55.5% | 982 | 57.3% | 740 | 58.5% |
| Male | 806 | 46.1% | 710 | 44.5% | 732 | 42.7% | 524 | 41.5% |
| Age group** | ||||||||
| 18–24 | 252 | 14.4% | 201 | 12.6% | 113 | 6.6% | 149 | 11.8% |
| 25–39 | 639 | 36.6% | 513 | 32.2% | 509 | 29.7% | 342 | 27.1% |
| 40–54 | 621 | 35.5% | 583 | 36.6% | 622 | 36.3% | 480 | 38.0% |
| 55-max | 236 | 13.5% | 298 | 18.7% | 470 | 27.4% | 293 | 23.2% |
| Education** | ||||||||
| Low | 1169 | 66.9% | 717 | 45.0% | 1109 | 64.7% | 516 | 40.8% |
| Moderate | 355 | 20.3% | 657 | 41.2% | 394 | 23.0% | 573 | 45.3% |
| High | 224 | 12.8% | 221 | 13.9% | 211 | 12.3% | 175 | 13.8% |
| Ethnicity** | ||||||||
| Non-white, other Language | 211 | 12.1% | 169 | 10.6% | 74 | 4.3% | 259 | 20.5% |
| White, English only | 1537 | 87.9% | 1426 | 89.4% | 1640 | 95.7% | 1005 | 79.5% |
| Smoking status* | ||||||||
| Daily | 1577 | 90.2% | 1461 | 91.6% | 1599 | 93.3% | 1155 | 91.4% |
| Weekly/Monthly | 171 | 9.8% | 134 | 8.4% | 115 | 6.7% | 109 | 8.6% |
| Number of smoking friends at Wave 1 | ||||||||
| 0 | 228 | 13.0% | 201 | 12.6% | 227 | 13.2% | 174 | 13.8% |
| 1 | 236 | 13.5% | 208 | 13.0% | 230 | 13.4% | 166 | 13.1% |
| 2 | 341 | 19.5% | 316 | 19.8% | 331 | 19.3% | 240 | 19.0% |
| 3 | 376 | 21.5% | 328 | 20.6% | 319 | 18.6% | 247 | 19.5% |
| 4 | 221 | 12.6% | 213 | 13.4% | 234 | 13.7% | 152 | 12.0% |
| 5 | 346 | 19.8% | 329 | 20.6% | 373 | 21.8% | 285 | 22.5% |
| Friend change between Wave 1 and Wave 2* | ||||||||
| −5 | 5 | 0.3% | 1 | 0.1% | 12 | 0.7% | 9 | 0.7% |
| −4 | 14 | 0.8% | 23 | 1.4% | 18 | 1.1% | 15 | 1.2% |
| −3 | 57 | 3.3% | 61 | 3.8% | 58 | 3.4% | 54 | 4.3% |
| −2 | 137 | 7.8% | 125 | 7.8% | 149 | 8.7% | 118 | 9.3% |
| −1 | 291 | 16.6% | 313 | 19.6% | 307 | 17.9% | 237 | 18.8% |
| No change | 713 | 40.8% | 628 | 39.4% | 689 | 40.2% | 471 | 37.3% |
| 1 | 330 | 18.9% | 260 | 16.3% | 287 | 16.7% | 207 | 16.4% |
| 2 | 128 | 7.3% | 128 | 8.0% | 120 | 7.0% | 100 | 7.9% |
| 3 | 49 | 2.8% | 39 | 2.4% | 50 | 2.9% | 30 | 2.4% |
| 4 | 11 | 0.6% | 8 | 0.5% | 16 | 0.9% | 18 | 1.4% |
| 5 | 13 | 0.7% | 9 | 0.6% | 8 | 0.5% | 5 | 0.4% |
Pearson χ2 test significantly different across countries at p<.0001
Pearson χ2 test significantly different across countries at p<.05
Number of smoking friends at Wave 1 and intentions to quit at Wave 1, intentions to quit at Wave 2, quit attempts, and quit attempt success at Wave 2
Number of smoking friends at Wave 1 was significantly related to intentions to quit at Wave 1, and quit attempt success at Wave 2 (see Table 2). Smokers with 5 vs. 0 smoking friends at Wave 1 were less likely to intend to quit at Wave 1 (OR = 0.76; p =.02). Smokers with 5 vs. 0 smoking friends at Wave 1 were also less likely to be successful in their attempts to quit smoking at Wave 2 (OR = 0.60; p = .03). No other statistically significant associations were found between number of smoking friends at Wave 1 and these or other smoking cessation outcomes.
Table 2.
Number of Smoking Friends at Wave 1, and Intentions to Quit Smoking at Wave 1 and Wave 2, Attempts to Quit Smoking at Wave 2, and Successful Quit Attempts at Wave 2a
| Smoking Cessation Outcome |
Intentions to Quit at Wave 1 (N=6,321) | Intentions to Quit at Wave 2 (N=5,739) | Attempts to Quit at Wave 2 (N=6,321) | Successful Quit Attempts at Wave 2 (N=2,308) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | n and (%) Intend to Quit at W1 |
ORb | 95% CIc | p | n and (%) Intend to Quit at W2 |
ORb | 95% CIc | p | n and (%) Attempted to Quit |
ORb | 95% CIc | p | n and (%) Successful Quit Attempts |
ORb | 95% CIc | p |
| Number of smoking friends at Wave 1 | ||||||||||||||||
| 0 | 830(38.5) | 1.00 | 1.00 | refd | 741(32.9) | 1.00 | 1.00 | refd | 830(38.7) | 1.00 | 1.00 | refd | 320(21.1) | 1.00 | 1.00 | refd |
| 1 | 840(42.9) | 1.21 | 0.94,1.55 | 0.15 | 747(34.5) | 1.06 | 0.81,1.39 | 0.67 | 840(37.7) | 0.92 | 0.72,1.18 | 0.53 | 316(23.4) | 1.20 | 0.76,1.89 | 0.44 |
| 2 | 1228(36.8) | 0.89 | 0.70,1.12 | 0.32 | 1092(33.7) | 1.09 | 0.84,1.41 | 0.52 | 1228(36.4) | 0.91 | 0.72,1.14 | 0.42 | 445(22.0) | 1.04 | 0.68,1.59 | 0.85 |
| 3 | 1270(38.6) | 0.95 | 0.75,1.21 | 0.70 | 1159(30.7) | 0.86 | 0.66,1.12 | 0.27 | 1270(38.2) | 0.97 | 0.77,1.22 | 0.77 | 466(18.8) | 0.89 | 0.58,1.36 | 0.59 |
| 4 | 820(33.5) | 0.80 | 0.62,1.04 | 0.09 | 757(27.6) | 0.81 | 0.61,1.08 | 0.15 | 820(35.4) | 0.87 | 0.67,1.12 | 0.28 | 291(16.3) | 0.71 | 0.43,1.17 | 0.18 |
| 5 | 1333(31.5) | 0.76 | 0.59,0.96 | 0.02 | 1243(27.1) | 0.86 | 0.66,1.12 | 0.25 | 1333(36.3) | 0.97 | 0.77,1.23 | 0.83 | 470(12.6) | 0.60 | 0.38,0.95 | 0.03 |
adjusting for demographics, and smoking cessation predictor variables
OR=adjusted odds ratio
95% confidence interval
ref=reference group
Tests of interactions by country, education, and ethnicity were not significant, suggesting that the relation between number of smoking friends and the smoking cessation outcomes did not differ across countries, or by education or ethnicity. Tests of interactions by income for intentions to quit, and quit attempt success were not statistically significant, suggesting that the relation between number of smoking friends and smoking cessation outcomes did not differ by income. However the interaction for income by number of smoking friends for quit attempts was significant, Wald χ2(15, N = 6321) = 27.35, p = . 03. Examination of the interaction showed no meaningful pattern of results, and the possibility that this interaction was driven by the ‘no answer’ income category.
Changes in number of smoking friends between Wave 1 and Wave 2, and intentions to quit, quit attempts, and quit attempt success at Wave 2
Change in number of smoking friends was significantly related to intentions to quit at Wave 2, quit attempts at Wave 2, and quit attempt success at Wave 2 (see Table 3). Compared to smokers who experienced no change in their number of smoking friends, smokers who gained smoking friends were less likely to intend to quit at Wave 2 (OR = 0.82; p = .04).
Table 3.
Changes in Number of Smoking Friends Between Wave 1 and Wave 2, and Intentions to Quit Smoking at Wave 2, Attempts to Quit Smoking at Wave 2, and Successful Quit Attemptsa
| Smoking Cessation Outcome |
Intentions to Quit at Wave 2 (N=5,739) | Attempts to Quit at Wave 2 (N=6,321) | Successful Quit Attempts at Wave (N=2,308) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | n and (%) Intend to Quit |
ORb | 95%CIc | p | n and (%) Attempted to Quit |
ORb | 95%CIc | p | n and (%) Successful Quit Attempt |
ORb | 95%CIc | p |
| Change in number of smoking friends between Wave 1 and Wave 2 | ||||||||||||
| No change | 2290(30.2) | 1.00 | 1.00 | refd | 2501(34.5) | 1.00 | 1.00 | refd | 860(17.1) | 1.00 | 1.00 | refd |
| Loss | 1761(32.6) | 1.18 | 0.98,1.41 | 0.08 | 2004(42.1) | 1.50 | 1.27,1.76 | <0.0001 | 632(21.9) | 1.62 | 1.20,2.19 | <.01 |
| Gain | 1688(28.97) | 0.82 | 0.68,0.99 | 0.04 | 1816(34.6) | 0.97 | 0.82,1.15 | 0.76 | 816(15.5) | 0.73 | 0.52,1.04 | 0.08 |
adjusting for demographics, smoking cessation predictor variables, and number of smoking friends at Wave 1
OR=odds ratio,
95% confidence interval
ref=reference group
Although this analysis showed that smokers who lost smoking friends were not significantly more likely to intend to quit compared to those who experienced no change, see Table 3, analyses not shown here using the 11-category friend change variable (−5 to 0 to 5), found that some comparisons were significant, e.g., smokers who lost 4 smoking friends were 2.22 times more likely to intend to quit than smokers who experienced no change, (OR = 2.22, 95% CI = 1.09–4.55; p = .03).
Smokers who lost smoking friends were significantly more likely to have attempted to quit than smokers who experienced no change in their smoking friends (OR = 1.50; p<.0001). However, smokers who gained smoking friends were no more or less likely to have attempted to quit than smokers who experienced no change.
Smokers who lost smoking friends were more likely to have been successful in their attempt to quit compared to those who experienced no change in their smoking friends (OR = 1.62; p <.01). However, again, smokers who gained smoking friends were no more or less likely to have successfully quit than smokers who experienced no change. Tests of interactions by country, education, and ethnicity were not significant, suggesting that the relation between change in number of smoking friends and the smoking cessation outcomes did not differ across countries, education, or ethnicity.
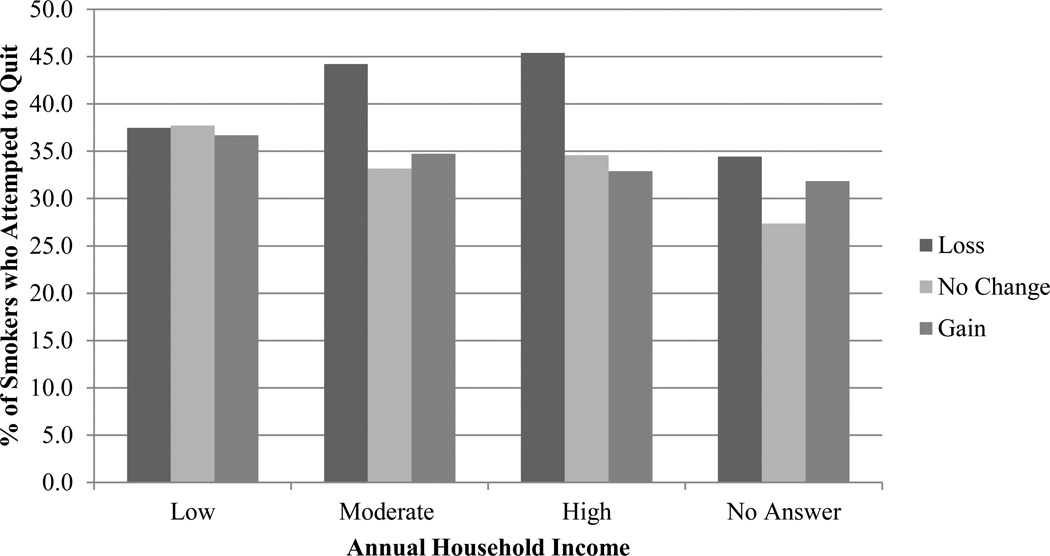
The friend change by income interactions for intentions to quit, and quit attempt success were not statistically significant, however the friend change by income interaction for quit attempts was, Wald χ2 (6, N=6321) =14.06, p = .03. See Figure 1. For low income respondents there was no significant relation between friend change and quit attempts; low income respondents who lost smoking friends, and low income respondents who gained smoking friends were no more, (OR = 1.01, 95% CI = 0.75–1.36; p = .93) or less likely, (OR = 0.91, 95% CI = 0.69–1.55; p = .55), to attempt to quit than those who experienced no change. In contrast, moderate and high income respondents who lost smoking friends were significantly more likely to attempt to quit compared to respondents who experienced no change (OR = 1.75, 95% CI = 1.34–2.29; p<.0001), and (OR = 1.82, 95% CI = 1.38–2.41; p<.0001), respectively. Further analyses showed that the results for respondents who gave no answer for income was similar to low income respondents.
Figure 1.
Income x Change in Number of Smoking Friends (loss, no change, gain) Interaction and Attempts to Quit Smoking at Wave 2
Discussion
This study found that across nationally representative samples of smokers in four countries changes in smokers’ number of smoking friends were related to their intentions to quit (at Wave 2), making quit attempts, and quit attempt success. Smokers who lost smoking friends were more likely to intend to quit at Wave 2, and smokers who gained smoking friends were less likely to intend to quit (additional analyses using the 11 category friend change variable). Smokers who lost smoking friends were also more likely to attempt to quit, and be successful in their attempts. However, smokers who gained smoking friends were no more or less likely to attempt to quit, or to succeed in their attempts to quit. This contrast in findings suggests that changes in a smoker’s social context contrary to their current behavior (i.e., loss in smoking friends) are related to behavioral change, whereas changes in the social context in line with current behavior (i.e., gain in smoking friends) are not. Additionally, although not explicitly discussed, this study found a surprising lack of constancy in people’s number of smoking friends, with 60% reporting a change over an average span of 6.7 months.
Unexpectedly, there was no relation between change in number of smoking friends and quit attempts among low income respondents. However, moderate and high income respondents who lost smoking friends were more likely to attempt to quit than respondents who experienced no change in their smoking friends. It is possible that losing smoking friends may not affect low income respondents’ motivation to quit because a loss in smoking friends may exert less influence or be overshadowed by other factors such as overall positive norms toward smoking in their social context, more stressful circumstances, higher prevalence of comorbid disorders, or other features associated with low SES that could impede quit behavior (Hiscock, Bauld, Amos, Fidler, & Munafò, 2012). Similar to the current study, Christakis and Fowler (2008) concluded that smokers with more education were both more likely to be influenced by their friends’ cessation behavior, and more likely to influence their friends’ cessation behavior (Christakis & Fowler, 2008).
Overall, the relation between changes in smoking friends and the smoking cessation outcomes suggests that further insights into the cessation process may be gained by considering the impact of change in the social context on smoking behavior. Others have similarly emphasized the need to study quitting as a ‘dynamic’ process that is influenced by changing factors (Larabie, 2005; Shiffman, 2005; West & Sohal, 2006).
Seemingly in line with the results for changes in smoking friends, smokers’ number of smoking friends at baseline was positively associated with both quit intentions at Wave 1 and with successfully quitting at Wave 2. A previous study similarly found that smokers who were more likely to report being in the presence of other smokers were less likely to be successful in their attempts to quit (Zhou et al., 2009). Another study also that found that smokers with more smoking friends (assessed when quit) were more likely to relapse (Herd et al., 2009). This study differs from the previous because it focused on current smokers at baseline, and considered the effect of changes in smoking friends.
This study has implications for future research, and cessation interventions. Future studies could examine the barriers that smokers encounter when trying to avoid other smokers when quitting, and how changes in smoking friends may be related to long-term abstinence. Interventions could help smokers avoid other smokers during quit attempts, keeping in mind that changing the current social context to minimize or even end contact with smoking friends may be difficult. Low SES smokers, who have been hypothesized to have difficulty succeeding in their quit attempts because of the high number of smokers in their social context (Hiscock et al., 2012; Jarvis, 2004; Kotz & West, 2009; Rose, Chassin, & Presson, 1996; Wiltshire, Bancroft, Parry, & Amos, 2003), may benefit the most from these interventions. Other strategies could also be encouraged, including eliciting social support for quitting, asking others not to smoke around them, and possibly helping them build connections with other smokers who want to quit or ex-smokers from their community through smoking cessation clinics. Unfortunately, the effectiveness of these interventions may depend on the ability of former smokers to avoid other smokers in the long-term (Hawkins, Hollingworth, & Campbell, 2010; Macy, Seo, Chassin, Presson, & Sherman, 2007; Wiltshire et al., 2003).
The main limitation of this study is that the design does not allow determination of the nature of the temporal sequencing between changing the number of smoking friends and the smoking cessation outcomes. Thus, although there was a relation between losing smoking friends and intentions, attempts, and quit success, it is uncertain whether the loss occurred prior to and/or after the smoking cessation outcome. Additionally, it is uncertain whether the relation between changes in smoking friends and smoking cessation outcomes is due to endogeneous, contextual, and/or correlated effects (for a full discussion see; Manski, 1993, 1995). For example, the relation would be contextual if the respondent and their friend were both exposed to the same tobacco control policies which led them to quit, whereas it would be endogeneous if the friend quit smoking because the respondent quit or had recently attempted to quit. Another limitation is the use of self-report. For instance, respondents may have forgotten about a quit attempt (Berg et al., 2010; Gilpin & Pierce, 1994). Another limitation is differential attrition among some groups, and greater attrition in the US which may have led to some attrition bias. For example, because smokers with more smoking friends were more likely to be lost to follow-up, the findings may underrepresent this group. It is also possible that time-related changes in respondents’ number of smoking friends may be quite different amongst populations that were not followed-up, because they may have been more likely to have moved and to have established new social networks.
The measure of number of smoking friends also has limitations. For example, because it asked about close friends and acquaintances, it is possible that respondents thought about different people when they responded. Indeed, cognitive testing by Thrasher et al., (2011) suggests that some respondents considered family members; however, there was no evidence of systematic bias in understanding the question across smokers from Anglophone countries. It is nonetheless possible that the measure included random error if some respondents thought about different friends at each wave. Although reliability of measurement may have been lower than desired, this cannot, in and of itself, explain the results whose direction and magnitude fit with prior research and associated hypotheses. It is also uncertain why respondents experienced changes in their smoking friends (friend quit smoking, de-selected smoking friend, etc.).
Despite limitations, the study had important strengths. The use of the nationally representative longitudinal cohort samples allowed the relation between number of smoking friends and smoking cessation outcomes to be examined prospectively across four countries. The consistency of the results across the four countries strengthens the confidence in our conclusions. The breadth of smoking cessation outcomes examined was an additional strength, particularly as it is increasingly clear that the predictors of quit attempts and successful quitting differ (Borland et al., 2010; Fidler & West, 2011; Kotz & West, 2009; Vangeli et al., 2011).
Acknowledgments
Grant support provided by Canadian Institutes for Health Research (57897, 79551, and 115016), Robert Wood Johnson Foundation (045734), Cancer Research UK (C312/A3726, C312/A6465, C312/A11039, and C312/A11943), Commonwealth Department of Health and Aging, Canadian Tobacco Control Research Initiative (014578), National Health and Medical Research Council of Australia (265903 and 450110), U.S. National Cancer Institute (P50 CA111236 and RO1 CA100362). Support was also provided by Ontario Institute for Cancer Research (Senior Investigator Award to the second author), Canadian Cancer Society Research Institute (Prevention Scientist Award to the second author), and a Canadian Institutes of Health Research Doctoral Research Award to the first author.
Footnotes
We have no conflicts of interest to declare.
References
- Baumeister RF. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin. 1995;117(3):497–529. Retrieved from http://psycnet.apa.org/psycinfo/1995-29052-001. [PubMed] [Google Scholar]
- Benowitz NL. Nicotine addiction. New England Journal of Medicine. 2010;362(24):2295–2303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CJ, An LC, Kirch M, Guo H, Thomas JL, Patten Ca, West R. Failure to report attempts to quit smoking. Addictive Behaviors. 2010;35(10):900–904. doi: 10.1016/j.addbeh.2010.06.009. [DOI] [PubMed] [Google Scholar]
- Biener L, Hamilton WL, Siegel M, Sullivan EM. Individual, social-normative, and policy predictors of smoking cessation: a multilevel longitudinal analysis. American Journal of Public Health. 2010;100(3):547–554. doi: 10.2105/AJPH.2008.150078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R, Yong H-H, Balmford J, Cooper J, Cummings KM, O’Connor RJ, Fong GT. Motivational factors predict quit attempts but not maintenance of smoking cessation: findings from the International Tobacco Control Four country project. Nicotine & Tobacco Research. 2010;12(Suppl):S4–S11. doi: 10.1093/ntr/ntq050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavelaars AEJM, Kunst AE, Geurts JJM, Crialesi R. Educational differences in smoking: international comparison. BMJ. 2000;320(7242):1102. doi: 10.1136/bmj.320.7242.1102. Retrieved from http://www.bmj.com/content/320/7242/1102.short. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Quitting Smoking Among Adults — United States, 2001 – 2010. Morbidity and Mortality Weekly Report. 2011;60(44):1514–1545. [PubMed] [Google Scholar]
- Chandola T, Head J, Bartley M. Socio-demographic predictors of quitting smoking: how important are household factors? Addiction. 2004;99(6):770–777. doi: 10.1111/j.1360-0443.2004.00756.x. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. The New England Journal of Medicine. 2008;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. Connected: The surprising power of social networks and how they shape our lives. 1st ed. New York, New York, USA: Hachette Book Group; 2009. [Google Scholar]
- Cummings KM, Fong GT, Borland R. Environmental influences on tobacco use: evidence from societal and community influences on tobacco use and dependence. Annual Review of Clinical Psychology. 2009;5:433–458. doi: 10.1146/annurev.clinpsy.032408.153607. [DOI] [PubMed] [Google Scholar]
- Farkas AJ, Gilpin EA, Distefan JM, Pierce JP. The effects of household and workplace smoking restrictions on quitting behaviours. Tobacco Control. 1999;8(3):261–265. doi: 10.1136/tc.8.3.261. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1763963&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidler JA, West R. Enjoyment of smoking and urges to smoke as predictors of attempts and success of attempts to stop smoking: a longitudinal study. Drug and Alcohol Dependence. 2011;115(1–2):30–34. doi: 10.1016/j.drugalcdep.2010.10.009. [DOI] [PubMed] [Google Scholar]
- Fong GT, Cummings KM, Borland R, Hastings G, Hyland A, Giovino GA, Thompson ME. The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tobacco control. 2006;15(Suppl 3):iii3–iii11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong GT, Hammond D, Laux F, Zanna M, Cummings KM, Borland R, Ross H. The near-universal experience of regret among smokers in four countries: Findings from the International Tobacco Control Policy Evaluation Survey. Nicotine & Tobacco Research. 2004;6(6):341–351. doi: 10.1080/14622200412331320743. [DOI] [PubMed] [Google Scholar]
- Gilpin EA, Pierce JP. Measuring smoking cessation: problems with recall in the 1990 California Tobacco Survey. Cancer Epidemiology, Biomarkers & Prevention. 1994;3(7):613–617. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7827593. [PubMed] [Google Scholar]
- Hawkins J, Hollingworth W, Campbell R. Long-term smoking relapse: a study using the british household panel survey. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2010;12(12):1228–1235. doi: 10.1093/ntr/ntq175. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. British Journal of Addiction. 1989;84(7):791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2758152. [DOI] [PubMed] [Google Scholar]
- Herd N, Borland R, Hyland A. Predictors of smoking relapse by duration of abstinence: findings from the International Tobacco Control (ITC) Four Country Survey. Addiction. 2009;104(12):2088–2099. doi: 10.1111/j.1360-0443.2009.02732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: a review. Annals of the New York Academy of Sciences. 2012;1248:107–123. doi: 10.1111/j.1749-6632.2011.06202.x. [DOI] [PubMed] [Google Scholar]
- Hitchman SC, Fong GT. Gender empowerment and female-to-male smoking prevalence ratios. Bulletin of the World Health Organization. 2011;89(3):195–202. doi: 10.2471/BLT.10.079905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Keely J. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38. doi: 10.1111/j.1360-0443.2004.00540.x. Retrieved from http://onlinelibrary.wiley.com/doi/10.1111/j.1360-0443.2004.00540.x/full. [DOI] [PubMed] [Google Scholar]
- Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine & Tobacco Research. 2004 Dec;6(Suppl 3):S363–S369. doi: 10.1080/14622200412331320761. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15799599. [DOI] [PubMed] [Google Scholar]
- Hymowitz N, Cummings KM, Hyland A, Lynn W, Pechacek TF, Hartwell T. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tobacco Control. 1997;6(Suppl 2):S57–S62. doi: 10.1136/tc.6.suppl_2.s57. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1766209/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- ITC Project. International Tobacco Control Policy Evaluation Survey (ITC 4-Country Survey): Wave 1 Technical Report. [Retrieved March 08, 2012];2004 from http://www.itcproject.org/documents/keyfindings/technicalreports/itcw1techreportfinalpdf. [Google Scholar]
- ITC Project. International Tobacco Control Policy Evaluation Survey (ITC): Four Country Project Waves 2–8 Technical Report. [Retrieved March 08, 2012];2011 from http://www.itcproject.org/documents/keyfindings/4cw28techreportmay2011_2_pdf. [Google Scholar]
- Jaccard J. Interaction Effects in Logistic Regression: Sage University Papers Series on Quantitative Applications in the Social Sciences. Thousand Oaks, California: SAGE Publications; 2001. [Google Scholar]
- Jarvis MJ. Why people smoke. BMJ. 2004;328(7434):277–279. doi: 10.1136/bmj.328.7434.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarvis MJ, Wardle J. Social patterning of individual health behaviours: the case of cigarette smoking. In: Marmot M, Wilkinson RG, editors. Social Determinants of Health. New York: Oxford University Press; 2006. pp. 224–237. Second. [Google Scholar]
- Kotz D, West R. Explaining the social gradient in smoking cessation: it’s not in the trying, but in the succeeding. Tobacco Control. 2009;18(1):43–46. doi: 10.1136/tc.2008.025981. [DOI] [PubMed] [Google Scholar]
- Larabie LC. To what extent do smokers plan quit attempts? Tobacco Control. 2005;14(6):425–428. doi: 10.1136/tc.2005.013615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine JM, Moreland RL. Group Composition. In: Levine J, Moreland R, editors. Small Groups: Readings in Social Psychology. New York, New York, USA: Psychology Press; 2006. pp. 11–19. [Google Scholar]
- Levy DE, Biener L, Rigotti NA. The natural history of light smokers: a population-based cohort study. Nicotine & Tobacco Research. 2009;11(2):156–163. doi: 10.1093/ntr/ntp011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez AD, Collishaw NE, Piha T. A descriptive model of the cigarette epidemic in developed countries. Tobacco Control. 1994;3(3):242. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1759359/ [Google Scholar]
- Macy JT, Seo D-C, Chassin L, Presson CC, Sherman SJ. Prospective predictors of long-term abstinence versus relapse among smokers who quit as young adults. American journal of public health. 2007;97(8):1470–1475. doi: 10.2105/AJPH.2006.101386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manski C. Identification of endogenous social effects: The reflection problem. The Review of Economic Studies. 1993;60(3):531–542. Retrieved from http://restud.oxfordjournals.org/content/60/3/531.short. [Google Scholar]
- Manski C. Identification Problems in the Social Sciences. Cambridge, Massachusetts: Harvard University Press; 1995. [Google Scholar]
- Markus H, Kitayama S. Culture and the self: Implications for cognition, emotion, and motivation. Psychological review. 1991;98(2):224–253. Retrieved from http://psycnet.apa.org/journals/rev/98/2/224/ [Google Scholar]
- O’Connell KA, Shiffman S, Decarlo LT. Does extinction of responses to cigarette cues occur during smoking cessation? Addiction. 2011;106(2):410–417. doi: 10.1111/j.1360-0443.2010.03172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osler M, Prescott E. Psychosocial, behavioural, and health determinants of successful smoking cessation: a longitudinal study of Danish adults. Tobacco Control. 1998;7(3):262–267. doi: 10.1136/tc.7.3.262. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1763896&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose JS, Chassin L, Presson CC. Demographic factors in adult smoking status: Mediating and moderating influences. Psychology of Addictive Behaviors. 1996;10(1):28–37. Retrieved from http://psycnet.apa.org/journals/adb/10/1/28/ [Google Scholar]
- Shiffman S. Dynamic influences on smoking relapse process. Journal of Personality. 2005;73(6):1715–1748. doi: 10.1111/j.0022-3506.2005.00364.x. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Gwaltney CJ, Balabanis MH, Liu KS, Paty JA, Kassel JD, Gnys M. Immediate antecedents of cigarette smoking: An analysis from ecological momentary assessment. Journal of Abnormal Psychology. 2002;111(4):531–545. doi: 10.1037//0021-843x.111.4.531. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty Ja, Gnys M, Kassel Ja, Hickcox M. First lapses to smoking: within-subjects analysis of real-time reports. Journal of consulting and clinical psychology. 1996;64(2):366–379. doi: 10.1037//0022-006x.64.2.366. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8871421. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Rathbun SL. Point process analyses of variations in smoking rate by setting, mood, gender, and dependence. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2011;25(3):501–510. doi: 10.1037/a0022178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens NM, Markus HR, Townsend SSM. Choice as an act of meaning: the case of social class. Journal of Personality and Social Psychology. 2007;93(5):814–830. doi: 10.1037/0022-3514.93.5.814. [DOI] [PubMed] [Google Scholar]
- Thompson ME, Fong GT, Hammond D, Boudreau C, Driezen P, Hyland A, Laux FL. Methods of the International Tobacco Control (ITC) Four Country Survey. Tobacco control. 2006;15(Suppl 3):iii12–iii18. doi: 10.1136/tc.2005.013870. (Suppl 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher JF, Quah ACK, Borland R, Driezen P, Omar M, Hosking W, Boado M. Using Cognitive Interviewing and Behavioral Coding to Determine Measurement Equivalence across Linguistic and Cultural Groups: An Example from the International Tobacco Control Policy Evaluation Project. Field Methods. 2011;23(4):439–460. doi: 10.1177/1525822X11418176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Surgeon General. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Rockville, MD: 2010. Retrieved from http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:How+Tobacco+Smoke+Causes+Disease+:+The+Biology+and+Behavioral+Basis+for+Smoking-Attributable+Disease+A+Report+of+the+Surgeon+General#0. [PubMed] [Google Scholar]
- Valente TW. Social Networks and Health Communication. In: Thompson TL, Parrott R, Nussbaum J, editors. The Routledge Handbook of Health Communication. New York, New York, USA: Taylor and Francis; 2011. pp. 519–531. **(Second. [Google Scholar]
- Vangeli E, Stapleton J, Smit ES, Borland R, West R. Predictors of attempts to stop smoking and their success in adult general population samples: a systematic review. Addiction. 2011;106(12):2110–2121. doi: 10.1111/j.1360-0443.2011.03565.x. [DOI] [PubMed] [Google Scholar]
- West R. Theory of Addiction. London: Blackwell Publishing; 2006. [Google Scholar]
- West R. The multiple facets of cigarette addiction and what they mean for encouraging and helping smokers to stop. COPD: Journal of Chronic Obstructive Pulmonary Disease. 2009;6(4):277–283. doi: 10.1080/15412550903049181. [DOI] [PubMed] [Google Scholar]
- West R, Sohal T. Catastrophic pathways to smoking cessation: findings from national survey. BMJ. 2006;332(7539):458–460. doi: 10.1136/bmj.38723.573866.AE. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1382539&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westmaas JL, Bontemps-Jones J, Bauer JE. Social support in smoking cessation: reconciling theory and evidence. Nicotine & Tobacco Research. 2010;12(7):695–707. doi: 10.1093/ntr/ntq077. [DOI] [PubMed] [Google Scholar]
- Wiltshire S, Bancroft A, Parry O, Amos A. “I came back here and started smoking again”: perceptions and experiences of quitting among disadvantaged smokers. Health Education Research. 2003;18(3):292–303. doi: 10.1093/her/cyf031. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global health risks: Mortality and burden of disease attributable to selected major risks. Bulletin of the World Health Organization. Vol. 87. Geneva: 2009. [Google Scholar]
- World Health Organization. WHO report on the Global Tobacco Epidemic, 2011: Warning about the Dangers of Tobacco. Most. Geneva: 2011. [Google Scholar]
- Zhou X, Nonnemaker J, Sherrill B, Gilsenan AW, Coste F, West R. Attempts to quit smoking and relapse: factors associated with success or failure from the ATTEMPT cohort study. Addictive Behaviors. 2009;34(4):365–373. doi: 10.1016/j.addbeh.2008.11.013. [DOI] [PubMed] [Google Scholar]