Abstract
Objectives
This study examines the prevalence of cardiovascular risk factors and chronic disease burden among African Americans compared to Caucasians in a population of higher socioeconomic status.
Design
The current study is a cross-sectional, secondary data analysis of the Cooper Center Longitudinal Study.
Setting
Patients with a medical examination from 1970-2010 at the Cooper Clinic.
Participants
762 African Americans and 40,051 Caucasians who met the criteria.
Outcome Measures
Racial differences in cardiovascular risk factors/burden of disease between African Americans and Caucasians.
Results
African Americans had higher prevalence of evaluated cardiovascular risk factors than did Caucasians after controlling for obesity, tobacco use, and physical fitness. Caucasians had greater likelihood of no risk factors while African Americans were more likely to have all three risk factors. Race was typically predictive of cardiovascular risk factors in African Americans compared to Caucasians.
Conclusions
Findings suggest that health differences persist despite greater socioeconomic status, and further investigations of biopsychosocial causes are warranted. (Ethn Dis. 2013;23[1]:35-42)
Keywords: Socioeconomic Status, Racial/ethnic Minorities, Preventive Medicine, Cardiovascular Risk Factors
Introduction
Despite the increasing life expectancy for the US population, a greater burden of disease continues to exist among African American (AA) men and women compared to their Caucasian counterparts. In 2007, the age-adjusted death rate was 1.3 times greater for African Americans than Caucasians.1 African Americans’ lifespan is 4.8 years (on average) less than Caucasians.1 Cardiovascular disease (CVD) in African Americans accounted for 44.6% and 46.9% of deaths in men and women, respectively, in 2006.2,3 Data from the Centers for Disease Control and Prevention further demonstrate racial/ethnic health disparities by a 32.3% higher mortality rate due to strokes among African Americans compared to Caucasians.3 In addition to CVD, African Americans also have a higher prevalence of cardiovascular risk factors including hypertension, obesity, diabetes mellitus, and physical inactivity.2 For example, 48% of African Americans have multiple cardiovascular risk factors vs 37% of the remainder of the population.4 While race is commonly explored in the health disparities literature, its meaning and relationships to health are routinely discussed for additional clarity in these studies.
The meaning of race has varied over the decades to refer to physical traits or phenotypical features5 or a social political construct that places certain races above or below another race in a so-called hierarchy.6,7 The lack of a conceptual consensus, varied methods to assess, and nebulous operational definitions of race across disciplines has led to a growing methodological literature to further clarify the meaning, influences, and related factors to race. For example, the construct of ethnicity, which is not synonymous with race, could replace race in health disparities research as this term refers to values, customs, behaviors, and/or traditions.8 This construct can be added to a study with an acculturation measure.9 The influence of genes and/or environment on race and health outcomes has advanced with the growth of technology, genetic research, and quantitative methodologies.10 Furthermore, theory-driven constructs that are strongly correlated to race or certain races (eg, discrimination), while not reinforcing stereotypes, can be used to better delineate the relationships between race and various outcomes.11 Unfortunately, race has been confounded by low socioeconomic status (SES) over the past decades where it is not clear if low SES and/or race is contributing to specific poor health outcomes.12
Socioeconomic status pertains to occupation, income, employment, and at times ZIP Code and insurance status.13 While it is optimal to have all of these indicators of SES in health research, survey design, report bias, and privacy of the participant may prevent an actual or valid assessment of all indices. Race as previously defined does not explicitly explain or describe these prior areas of SES. Thus, the relationships are not between race and SES, and their influence on outcomes must be clearly defined in health research. Past research has attempted to do such where racial health inequality may stem predominantly from SES disadvantages in education, income, and employment status (ie, lower SES).14,15 The literature has attempted to address this prior relationship by statistically controlling for SES which has worked for some health outcomes (asthma) compared to others (hypertension).16,17 Thus, other factors can be influencing racial group differences. Discrimination at the personal and health care system level, medical mistrust, limitations in environmental protection, economic development, and limited access to health care also may contribute.18-22 Inadequate health insurance and access to quality health care are critical elements that impact medical care among racial/ethnic minorities.23 Studies demonstrate strong relationships between these sociodemographic and psychosocial factors and greater CVD mortality in African Americans.24,25 There are limited investigations in racial/ethnic minorities with higher SES, comparable to Caucasians, receiving preventive medical services.22,23 Thus it is not clear if racial/ethnic minorities compared to Caucasians, both with high SES levels, have similarly good health outcomes or the racial/ethnic minorities have poorer health similar to findings of minorities with lower SES in the health inequality literature. These issues may prevent a full understanding of the factors contributing to health and disease disparities between racial/ethnic minorities and non-racial/ethnic minorities. Studies assessing higher SES (ie, college educated and/or currently employed) for racial/ethnic minorities are warranted.
Our study compares the prevalence of cardiovascular risk factors and chronic disease burden between African Americans and Caucasians of higher SES and their access to prevennve health care.
Methods
The Cooper Center Longitudinal Study (CCLS) is a large cohort of men and women who underwent a preventive medical examination at the Cooper Clinic in Dallas, Texas from May 1970 to July 2010.26 Reported results are obtained from 762 self-identified African Americans, 61% men, and 40,051 Caucasians, 68% men, with complete cross-sectional data. Cooper Clinic patients are of higher SES and are self-referred or executives referred by their employer for these extensive preventive medicine examinations. Prior CCLS papers have described this database as primarily White, higher SES, and male.27,28 For the purpose of this investigation, high SES was defined as education attainment and ability to obtain said examination. This data set presents a unique opportunity to examine two racial groups (one being a historically defined minority group) from similar, higher SES backgrounds (Table 1). Patients consented and approved the use of their data for research. The study was approved by The Cooper Institute Institutional Review Board.
Table 1.
Demographic and baseline clinical characteristics for African Americans and Caucasians, The Cooper Center Longitudinal Study, 1970-2010
| African American Men (n=463) | Caucasian Men (n=27,238) | P | African American Women (n=299) | Caucasian Women (n=12,813) | P | |
|---|---|---|---|---|---|---|
| Age, years, mean (SD) | 44.1 (8.7) | 46.3 (10.1) | <.0001 | 45.3 (8.9) | 47.2 (11.2) | .003 |
| Education, years, mean (SD) | 16.0 (2.4) | 16.1 (2.4) | .68 | 15.7 (2.6) | 15.2 (2.3) | .003 |
| Employment, yes, n (%) | 348 (75.2) | 19215 (70.5) | .03 | 194 (65) | 5427 (42) | <.0001 |
| Marital history, yes, n (%) | 428 (92.4) | 25667 (94.2) | .10 | 251 (84) | 11838 (92) | <.0001 |
| Overall health, n (%) | ||||||
| Poor/fair | 83 (20.4) | 4393 (19.2) | .54 | 78 (29.0) | 2004 (17.9) | <.0001 |
| Good/excellent | 324 (79.6) | 18491 (80.8) | 191 (71.0) | 9218 (82.1) | ||
| Chronic diseases – Self-reported history – n (%) | ||||||
| Heart attack | 2 (.43) | 325 (1.2) | .13 | 1 (.33) | 49 (.38) | 1.0 |
| Stroke | 1 (.22) | 133 (.49) | .40 | 2 (.67) | 82 (.84) | .72 |
| Hypertension | 127 (27.4) | 4752 (17.5) | <.0001 | 81 (27.1) | 1730 (13.5) | <.0001 |
| High cholesterol | 114 (24.6) | 6852 (25.2) | .79 | 58 (19.4) | 2788 (21.8) | .33 |
| Diabetes | 25 (5.4) | 546 (2.0) | <.0001 | 13 (4.4) | 242 (1.9) | .002 |
| Metabolic syndrome | 74 (16.0) | 5768 (21.1) | .007 | 35 (11.7) | 1127 (8.8) | .08 |
| Cancer | 9 (1.9) | 1800 (6.6) | <.0001 | 11 (3.7) | 1178 (9.2) | .001 |
| Phenotypic parameters – mean (SD) unless otherwise stated | ||||||
| Body mass index, kg/m2 | 29.7 (5.3) | 27.6 (4.3) | <.0001 | 28.2 (6.6) | 24.5 (5.0) | <.0001 |
| BMI ≥30 kg/m2, n (%) | 162 (35.0) | 5469 (20.1) | <.0001 | 87 (29.1) | 1453 (11.3) | <.0001 |
| Waist circumference, cm | 96.0 (11.4) | 95.2 (11.4) | .26 | 82.8 (13.4) | 76.8 (11.9) | <.0001 |
| SBP, mm Hg | 126.2 (14.4) | 123.3 (13.7) | <.0001 | 120.6 (16.4) | 115.7 (16.0) | <.0001 |
| DBP, mm Hg | 85.8 (11.1) | 82.7 (9.7) | <.0001 | 81.4 (10.8) | 77.3 (9.8) | <.0001 |
| Glucose, mg/dL | 102.4 (29.3) | 100.0 (17.5) | .09 | 93.9 (20.1) | 93.6 (13.9) | .77 |
| 100-125, n (%) | 139 (31.5) | 9641 (37.4) | .01 | 50 (17.4) | 2191 (18.3) | .69 |
| >125, n (%) | 31 (7.0) | 903 (3.5) | <.0001 | 7 (2.4) | 198 (1.7) | .31 |
| Total cholesterol, mg/dL | 198.7 (40.2) | 199.6 (38.2) | .65 | 193.8 (36.7) | 197.9 (36.7) | .06 |
| LDL, mg/dL | 128.3 (36.4) | 125.4 (33.5) | .08 | 113.8 (30.7) | 112.8 (32.3) | .58 |
| HDL, mg/dL | 50.0 (11.9) | 47.3 (12.1) | <.0001 | 64.5 (17) | 65.0 (16.5) | .57 |
| TG, median (Q1,Q4), mg/dL | 90.0 (69.0,123.0) | 112.0 (80.0,164.0) | <.0001 | 74 (56.0,102.0) | 86 (64.0,125.0) | <.0001 |
| CES-D (total scale) | 3.9 (4.0) | 4.0 (4.3) | .7 | 4.0 (4.6) | 5.3 (5.2) | .24 |
| Health behaviors - mean (SD) | ||||||
| PA Index | 1.5 (1) | 1.5 (1.1) | .46 | 1.3 (.9) | 1.5 (1.1) | <.0001 |
| CRF (METs) | 10.6 (2.2) | 11.5 (2.4) | <.0001 | 8.5 (1.8) | 9.6 (2.1) | <.0001 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; LDL, low density lipoprotein; HDL, high density lipoprotein; TC, triglycerides; CES-D, Center for Epidemiologic Studies Depression Scale; CRF, Cardiorespiratory fitness; METs, metabolic equivalents, 1 MET = 3.5ml 02 uptake/kg/min.
The medical exam included self-reported personal and family history and demographic information, physical examination by a physician, anthropometric measurements, electrocardiogram, blood chemistry analyses after an overnight fast of 12 hours, blood pressure assessment, and maximal exercise treadmill test. Weight and height were obtained using a standard physician's scale and stadiometer and used to calculate body mass index (BMI) in kilograms per meter squared (kg/m2). Obesity was defined as a BMI of ≥30 kg/m2. Waist circumference was measured on a horizontal plane at the level of the umbilicus with a tape measure. Blood pressures were measured using the auscultatory technique with a mercury sphygmomanometer. Blood chemistry was analyzed using automated methods that corresponded to standards set by the CDC's Lipid Standardization Program. Cardiorespiratory fitness (CRF) was determined by the maximal time on the treadmill during the modified Balke protocol. A correlation of r=.92 was established between V02 max and Balke suess test time in minutes.29 A 5-level self-report physical activity (PA) index was calculated where 0 indicated no regular PA; 1, PA other than walking, jogging, or running; 2, walking, jogging, or running <10 miles per week; 3, 10 to 20 miles per week; and 4, >20 miles per week. This scale has been used as a valid measure of PA within the CCLS population.30,31 The Center for Epidemiologic Studies-Depression scale assessed the presence of depressive symptoms over the previous week. Scores range from 0-30; ≥10 indicates clinically significant depression warranting evaluation.32
The three risk factors for cardiovascular disease are defined below. Dyslipidemia was clinically defined as total cholesterol ≥200mg/dL, and/or high density lipoprotein cholesterol (HDL-C) ≤40mg/dL, and/or low density lipoprotein cholesterol (LDL-C) ≥130mg/dL, and/or triglycerides ≥150mg/dL, and/or a self-reported history of hyperlipidemia. Hypertension and diabetes were based on self-reported history and/or SBP >140 and/or DBP >90 and self-reported history and/or fasting blood glucose >126 mg/dL, respectively.
Statistical Analyses
Descriptive analyses, chi-square, and Student's t tests, when appropriate, were conducted on sociodemographics (eg, age, SES, education and employment, marital status), health behaviors (eg, tobacco use, PA), self-reported chronic diseases, and phenotypic parameters (eg, BMI, glucose, blood pressure). T tests were adjusted using Satterthwaite method to account for unequal sample size and variance when appropriate.33 Race/ethnicity findings were reported by sex. Multivariate logistic regression determined the association of race with three relevant cardiovascular risk factors (hypertension, dyslipidemia, and diabetes mellitus). The models were adjusted for race, age, SES, tobacco, obesity, and/or CRF. The number of cardiovascular risk factors (0-3) was determined for sex and racial strata. P≤.05 was considered significant. Analyses were performed in SAS versiOn 9.1 (SAS Institute, Cary, NC).
Results
Demographic and clinical baseline characteristics (average age = mid-40s) are summarized in Table 1. Among women, there were significant racial differences in age, education, employment, and personal perception of overall health. African American women were younger, more likely to be employed, but less likely ro be married than Caucasian women. African American men were younger, more likely to be employed, and used less tobacco than Caucasian men. Caucasians self-reported fewer chronic diseases, other than cancers, vs African Americans. African Americans had a significancly greater prevalence of self-reported hypertension (27.4% vs. 17.5% for men [X2 = 31.3, P≤.0001] and 27.10/0 vs. 13.5% for women [X2 = 45.3, P≤.000l]) and diabetes (5.4% vs. 2.0% for men [X2 = 26.0, P≤.0001] and 4.4% vs. 1.9% for women [X= 9.27, P=.002]). African Americans had higher prevalence of obesity as well as greater systolic blood pressure and lower CRF than their Caucasian counterparts (Table 1).
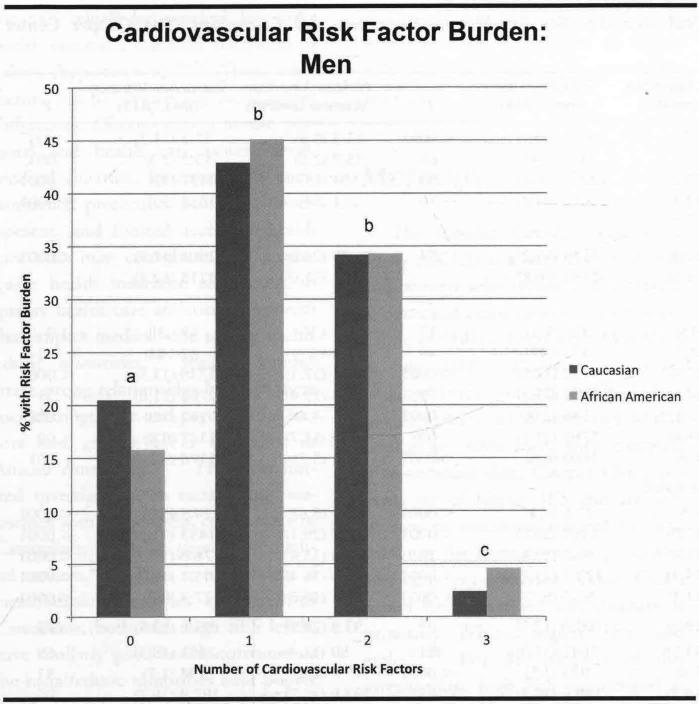
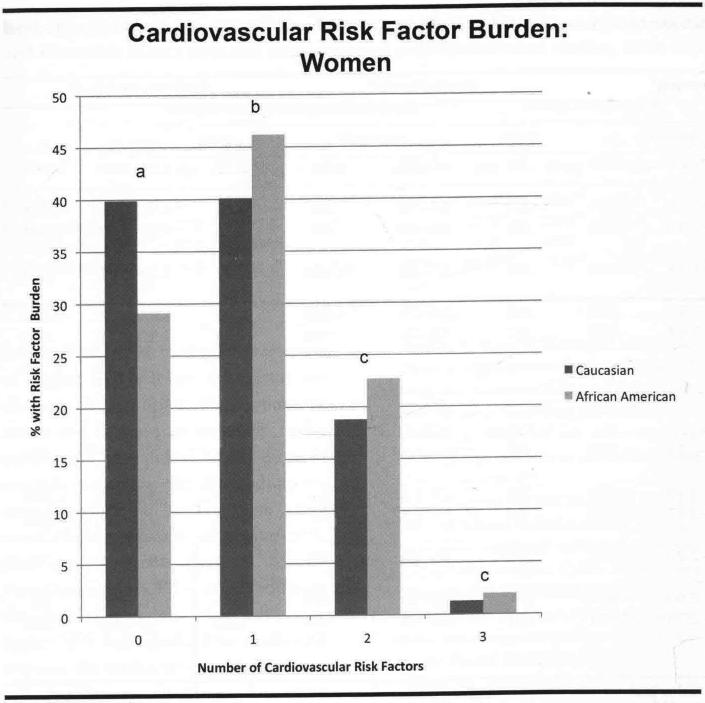
Figures 1a and 1b illustrate the burden of cardiovascular risk factors by absolute numbers, comparing African Americans with Caucasians by sex. A greater proportion of Caucasian men reported none of the identified cardiovascular risk factors (20.5% vs 15.8% in African Americans, P=.012). A similar pattern was identified in women (Caucasian [39.9%] vs. African-American [29.1%], P<.001). A greater proportion of African American men (4.6% vs 2.4%, P=.00l) had all three of the risk factors.
Fig 1a.
Cardiovascular risk factor burden of disease in African American vs Caucasian men, Cooper Center longitudinal Study, 1970-2010. Risk factor burdens adjusted for obesity, and include diabetes, hypertension, and high cholesterol
aP=.012
bnot significant
cP=.001
Fig 1b.
Cardiovascular risk factor burden of disease in African American vs Caucasian women, Cooper Center Longitudinal Study, 1970-2010. Risk factor burdens adjusted for obesity, and include diabetes, hypertension, and high cholesterol
aP<.001
bP=.034
cnot significant(ns)
Adjusted logistic regression models in Table 2 for African American men show greater odds for diabetes (OR= 1.94, 95% CI, 1.37, 2.75, P=.002) and hypertension (OR= 1.35, 95% CI, 1.11, 1.64, P=.002). The odds of prevalent hypertension in African American women in the unadjusted model was higher (OR=2.20, 95% CI, 1.74, 2.78, P<.001) and diabetes (OR=2.19, 95% CI, 1.33, 3.62, P=.002). After adjusting for obesity, however, the odds of diabetes in African American women, while greater than Caucasian, becomes statistically non-significant (OR= 1.58, 95% CI, .094, 2.66, P= .087).
Table 2.
Odds ratios for associations of race on cardiovascular risk factors in men and women, Cooper Center Longitudinal Study, 1970-2010
| Hypertensiona | Dyslipidemiab | Diabetes Mellitusc | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Men | |||||||||
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| Unadjusted (Caucasiane, African American) | 1.53 | 1.28-1.84 | <.001 | .79 | .66-.96 | .02 | 2.15 | 1.54-3.00 | <.001 |
| Adjusted risk for age | 1.73 | 1.43-2.08 | <.001 | .81 | .67-.98 | .03 | 2.69 | 1.92-3.79 | <.001 |
| Adjusted risk for age and tobacco use (noe, yes) | 1.74 | 1.44-2.10 | <.001 | .82 | .68-.99 | .04 | 2.70 | 1.92-3.80 | <.001 |
| Adjusted risk for obesityd (BMI ≤29.9e, BMI ≥30) | 1.32 | 1.09-1.59 | .005 | .69 | .57-.84 | <.001 | 1.72 | 1.22-2.41 | .002 |
| Adjusted for age and fitness | 1.43 | 1.18-1.73 | .002 | .65 | .54-.79 | <.001 | 2.03 | 1.43-2.87 | <.001 |
| Adjusted risk for age, tobacco (noe, yes), obesity (BMI ≤29.9e, BMI ≥30), SES, fitness | 1.35 | 1.11-1.64 | .002 | .62 | .52-.76 | <.001 | 1.94 | 1.37-2.75 | .002 |
| Women | |||||||||
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| Unadjusted (Caucasiane, African American) | 2.20 | 1.74-2.78 | <.001 | .85 | .67-1.07 | .16 | 2.19 | 1.33-3.62 | .002 |
| Adjusted risk for age | 2.87 | 2.24-3.68 | <.001 | .93 | .73-1.17 | .52 | 2.49 | 1.51-4.13 | <.001 |
| Adjusted risk for age and tobacco use (noe, yes) | 2.87 | 2.24-3.67 | <.001 | .93 | .73-1.18 | .56 | 2.50 | 1.51-4.14 | <.001 |
| Adjusted risk for obesityd (BMI ≤29.9e, BMI≥30) | 1.75 | 1.37-2.25 | <.001 | .71 | .56-.90 | .005 | 1.42 | .85-2.38 | .18 |
| Adjusted risk for age and fitness | 2.30 | 1.79-2.96 | <.001 | .74 | .58-.94 | .014 | 1.84 | 1.10-3.07 | .02 |
| Adjusted risk for age, tobacco (noe, yes), obesity (BMI ≤29.9e, BMI≥30), SES, fitness | 2.11 | 1.63-2.73 | <.001 | .70 | .55-.90 | .005 | 1.58 | .94-2.66 | .087 |
Hypertension = self-reported history and/or SBP >140 and/or DBP >90.
Dyslipidemia = self-reported history and/or high density lipoprotein cholesterol <40 mg/dL and/or low density lipoprotein cholesterol >130 mg/dL and/or triglycerides >150mg/dL.
Diabetes mellitus = self-reported history and/or fasting blood glucose >126 mg/dL.
Obesity = BMI ≥30 kg/m2.
Referent group.
Discussion
Our study explored the relationship between sociodemographic factors including race and higher SES on CVD risk burden in African Americans and Caucasians with access ro a preventive medical examination. African Americans presented with a greater prevalence of the self-reported chronic diseases. African Americans had greater odds of prevalent hypertension and diabetes mellitus as compared ro Caucasians. Past research indicated greater morbidity from diabetes and hypertension for African Americans than Caucasians as well.34 In multivariate analyses, obesity strongly influences the risk of diabetes in African American women; in contrast, African Americans had lower risk for the lipid disorders.35 Our srudy found sex-specific health disparities between African Americans and Caucasians, and we examined the impact of additional covariates (obesity, tobacco use, age, SES, and CRF) that can increase cardiovascular risk factor burden. Race as a predictor appeared to be independent, given that our SES was homogenous and should not confound our analyses of other prevalent cardiovascular risk factors in the models. Addressing the overall burden of cardiovascular risk factors as a sum, Caucasians overwhelmingly had greater prevalence of being free of these factors. Despite being socioeconomically similar, African Americans had higher prevalence of multiple risk factors (3 factors). Similar to other health disparities research, our findings demonstrated racial/ethnic differences in chronic disease risk factor burden such as hypertension.14,36,37
Does race, SES, or combination affect health disparities between African Americans and Caucasians?14 Although SES is a complex variable to measure, it is seen as a predictor of racial/ethnic minority health outcomes. Past reports were inconsistent regarding health disparities after controlling for SES.38,39 We conrrolled for SES, but racial health disparities still existed. Greater understanding of these health disparities and correlates is needed. Our study suggests that being African American has unique medical implications, independent of SES, which must be taken into account by health care providers.
Recently, a debate has risen regarding the impact of race and ethnicity on health and disease status, stemming from the lack of clarity of the role of race/ethnicity within the genetic, environmental, psychosocial, and cultural milieu.40,41 Some factors can be linked to theories about the psychosocial and cultural implications of race.42,43 One theory is the “diminishing return hypothesis,” suggesting that higher education or SES attained by African Americans does not lead to similar positive health outcomes comparable to Caucasians due to an incongruent relation between a person's daily experiences and economic status that lead to conflict and stress.42,44 This has rarely been explored in the literature.14 Our findings provide evidence for this theory. This research gap may be attributed to several factors: 1) prevailing focus on the “minority poverty hypothesis,” which suggests disadvantages due to race and lower SES,45,46 2) targeted recruitment of lower SES, and 3) under-recruitment of a range of SES in African-American samples. The current study provides a unique opportunity to stan investigations of the diminishing return hypothesis in a cohort of highly educated African Americans with health care access.
To fully understand this hypothesis, our sample's sociodemographics and relations to chronic disease outcomes must be revisited. Despite comparable SES status, African Americans had more self-reponed chronic disease and cardiovascular risk factors. A plausible interpretation of these findings can come from the diminishing return hypothesis. But, our cohort may have experienced poorer health outcomes because of negative psychosocial factors such as stress, mistreatment/discrimination, less marital support, and/or lower quality of life. Overall health (a proxy for quality of life) is statistically lower for African American vs Caucasian women.47 However, our study found a lack of depressive symptoms (a proxy for stress) based on CES-D in both races.
With higher SES comes greater expectations of certain lifestyles and quality of life.42,43 If these expectations aren't met, an individual may experience a greater level of stress and/or allostatic load. 48,49 Stress has been associated with increased CVD.24 A concept, “John Henryism,” suggests that active coping methods may result in a counterintuitive activation of the sympathetic nervous system in some African Americans.50,51 This may lead to greater negative health outcomes. These theories and hypotheses further support the importance of examining psychosocial factors and health outcomes in racial/ethnic minorities across the SES spectrum. This study provides one of the first epidemiological investigations supporting the diminishing return hypothesis as a plausible explanation of these findings.
There are several strengths of this study. The CCLS provides a large sample of African Americans and Caucasians of both sexes with sociodemo-graphic information, self-reported chronic disease history, and phenotypic data at a preventive medicine visit. This is the first CCLS study examining the effects of race, health behaviors, and SES on chronic burden cardiovascular risk factors. These data on African Americans in the CCLS are comparable to other published data such as the Dallas Heart Study and the National Health and Nutrition Examination Survey (Table 3).52-55 While the absolute disease burden in our sample is lower, the relative burden is consistent with previous literature.52-55 Our data present clinically relevant information for physicians and social scientists. African Americans deserve a careful evaluation of their cardiovascular risk factors and disease even when presenting with higher SES (eg, education). The risk factors reviewed in this study are modifiable through health promotion programs (eg, diet, physical activity, stress management).
Table 3.
Comparisons of absolute prevalence of obesity, hypertension, hyperlipidemia, and diabetes of African American (AA) and Caucasian (Cauc) men and women among population-based studies, 1970-2010, (%)
| Cooper Center Longitudinal Study |
Dallas Heart Study |
National Health and Nutrition Examination Study |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men |
Women |
Men |
Women |
Men |
Women |
|||||||
| AA | Cauc | AA | Cauc | AA | Cauc | AA | Cauc | AA | Cauc | AA | Cauc | |
| Obesity | 35 | 20.1 | 29.0 | 11.3 | 36.052 | 34.052 | 59.052 | 4252 | 37.353 | 31.953 | 49.653 | 33.053 |
| Hypertension | 27.4 | 17.5 | 27.1 | 13.5 | 52.052 | 28.052 | 66.052 | 3352 | 42.458 | 45.858 | 57.658 | 54.258 |
| Dyslipidemia | 24.6 | 25.2 | 19.4 | 21.8 | 2.0 | 7.4 | 1.1 | 2.8 | 45.654 | 55.054 | 47.754 | 58.754 |
| Diabetes Mellitus | 5.4 | 2.0 | 4.4 | 1.9 | 16.052 | 7.052 | 20.052 | 8.052 | 7.055 | 9.055 | 14.055 | 7.055 |
Several limitations must be taken into account. The comparison samples are unbalanced with respect to absolute numbers of African Americans and Caucasians, although this was addressed with statistical methods. The study is cross-sectional which limits causality. The chronic disease history is self-reported although confirmed by the clinic physician. Education and employment were used as proxies to define SES; however, actual income levels were not available. Our study did not include commonly used stress or quality of life measures such as the Perceived Stress Scale and SF-36.56,57
There are three important implications to aid physicians and social scientists working with African Americans. The assumption cannot be made that higher SES levels buffer poorer health outcomes. Health care providers need to proactively address health promotion with African Americans regardless of higher SES. Further research should be directed towards longitudinal epidemiologic evaluation of higher SES African Americans including the complex biopsychosocial needs and the impact on their health outcomes.24 Additional health disparity research examining the diminishing return hypothesis is warranted in other racial/ethnic minorities of higher SES. Our study presents data on African Americans in the CCLS, which addresses the relationship of race with health among higher SES individuals. Our study will improve the understanding of cardiovascular health issues of African Americans withhigher SES who are typically underrepresented in the literature.
Our study compares the prevalence of cardiovascular risk factors and chronic disease burden between African Americans and Caucasians of higher SES and their access to preventive health care.
Despite comparable SES status, African Americans had more self-reported chronic disease and cardiovascular risk factors.
Footnotes
Author Contributions
Design and concept of study: Frierson, DeFina
Data analysis and interpretation: Frierson, DeFina, Powell-Wiley, Willis
Manuscript draft: Frierson, Howard, DeFina, Powell-Wiley, Willis
Statistical expertise: Powell-Wiley, Willis
Administrative: Frierson, Howard, Powell-Wiley, Willis
Supervision: DeFina
References
- 1.Xu J, Kochanek K, Murphy SL, Tejada-Vera B. Division of Viral Statistics. Deaths: Final Data for 2007. National Viral Statistics Reports. 58(19) [PubMed] [Google Scholar]
- 2.Lloyd-Jones D, Adan1s RJ, Brown TM, et al. Heart disease and stroke statistics-2010 update: a report from the American Heart Association. Circulation. 2010. 121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 3.Frieden TR. Forward: CDC Health Disparities and Inequalities Report - United States, 2011. MMWR Surveill Summ. 2011;60(Suppl):l–2. [PubMed] [Google Scholar]
- 4.Haskell WL, Berra K, Arias E. Multifactor cardiovascular disease risk reduction in medically underserved, high-risk patients. Am J Cardiol. 2006;98(11):1472–1479. doi: 10.1016/j.amjcard.2006.06.049. [DOI] [PubMed] [Google Scholar]
- 5.Rowe DC. IQ, birth weight, and number of sexual partners in White, African American, and mixed race adolescents. Popul Environ. 2002;23(6):513–524. [Google Scholar]
- 6.Guidelines on Multicultural Education, Training, Research, Practice, and Organizational Change for Psychologists. Am Psychol. 2003;58(5):377–402. doi: 10.1037/0003-066x.58.5.377. [DOI] [PubMed] [Google Scholar]
- 7.Helms J. The conceprualization of racial identity and other “racial” constructs. In: Trickett E, Warts R, Birman D, editors. Human Diversity: Perspectives on People in Context. The Jossey-Bass Social and Behavioral Science Series. Jossey-Bass; San Francisco: 1994. pp. 285–311. [Google Scholar]
- 8.Phinney J. When we talk about American ethnic groups, what do we mean? Am Psychol. 1996;51(9):918–927. [Google Scholar]
- 9.Zea MC, Asner-Self KK, Birman D, Buki LP. The abbreviated multidimensional acculturation scale: empirical validation with two Latino/Latina samples. Cultur Divers Ethnic Minor Psychol. 2003;9(2):107–126. doi: 10.1037/1099-9809.9.2.107. [DOI] [PubMed] [Google Scholar]
- 10.Whitfield KE, McClearn G. Genes, environment, and race: quantitative generic approaches. Am Psychol. 2005;60(1):104–114. doi: 10.1037/0003-066X.60.1.104. [DOI] [PubMed] [Google Scholar]
- 11.Helms JE, Jernigan M, Mascher J. The meaning of race in psychology and how to change it: a methodological perspective. Am Psychol. 2005;60(1):27–36. doi: 10.1037/0003-066X.60.1.27. [DOI] [PubMed] [Google Scholar]
- 12.Eisenman R. Why psychologists should study race. Am Psychol. 1995;50(1):42–43. [Google Scholar]
- 13.Stronks K, van de MH, van den BJ, Mackenbach JP. The interrelationship between income, health and employment status. Int J Epidemiol. 1997;26(3):592–600. doi: 10.1093/ije/26.3.592. [DOI] [PubMed] [Google Scholar]
- 14.Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60(1):191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 15.Shi L, Srarfield B. The effect of primary care physician supply and income inequality on mortality among Blacks and Whites in US metropolitan areas. Am J Public Health. 2001;91(8):1246–1250. doi: 10.2105/ajph.91.8.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams DR. Race/ethniciry and socioeconomic status: measurement and methodological issues. Int J Health Serv. 1996;26(3):483–505. doi: 10.2190/U9QT-7B7Y-HQ15-JT14. [DOI] [PubMed] [Google Scholar]
- 17.Litonjua AA, Carey VJ, Weiss ST, Gold DR. Race, socioeconomic factors, and area of residence are associated with asthma prevalence. Pediatr Pulmonol. 1999;28(6):394–401. doi: 10.1002/(sici)1099-0496(199912)28:6<394::aid-ppul2>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 18.Whitfield KE, Weidner G, Clark R, Anderson NB. Sociodemographic diversity and behavioral medicine. J Consult Clin Psychol. 2002;70(3):463–481. doi: 10.1037//0022-006x.70.3.463. [DOI] [PubMed] [Google Scholar]
- 19.Durant RW, Legedza AT, Marcantonio ER, Freeman MB, Landon BE. Willingness to participate 111 clinical trials among African Americans and Whites previously exposed to clinical research. J Cult Divers. 2011;18(1):8–19. [PMC free article] [PubMed] [Google Scholar]
- 20.White RM. Misinformarion and misbeliefs in the Tuskegee Study of Untreated Syphilis fuel mistrust in the healthcare system. J Natl Med Assoc. 2005;97(11):1566–1573. [PMC free article] [PubMed] [Google Scholar]
- 21.McLaughlin OK, Stokes CS. Income inequality and mortality in US counties: does minority racial concentration matter? Am J Public Health. 2002;92(1):99–104. doi: 10.2105/ajph.92.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hammond WP, Matthews O, Corbie-Smith G. Psychosocial factors associated with routine health examination scheduling and receipt among African American men. J Natl Med Assoc. 2010;102(4):276–289. doi: 10.1016/s0027-9684(15)30600-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sambamoorthi U, McAlpine DD. Racial, ethnic, socioeconomic, and access disparities in rbe use of preventive services among women. Prev Med. 2003;37(5):475–484. doi: 10.1016/s0091-7435(03)00172-5. [DOI] [PubMed] [Google Scholar]
- 24.Figueredo VM. The rime has come for physicians to take notice: the impact of psychosocial stressors on the heart. Am J Med. 2009;122(8):704–712. doi: 10.1016/j.amjmed.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Yankaskas BC. Epidemiology of breast cancer in young women. Breast Dis. 2005;23:3–8. doi: 10.3233/bd-2006-23102. [DOI] [PubMed] [Google Scholar]
- 26.Blair SN, Kohl HW, III, Paffenbarger RS, Jr., Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality: a prospective study of healthy men and women. JAMA. 1989;262(17):2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 27.Farrell SW, Cortese GM, LaMonte MJ, Blair SN. Cardiorespiratory fitness, different measures of adiposity, and cancer mortality in men. Obesity (Silver Spring) 2007;15(12):3140–3149. doi: 10.1038/oby.2007.374. [DOI] [PubMed] [Google Scholar]
- 28.Farrell SW, FitzGerald SJ, McAuley PA, Barlow CE. Cardiorespiratory fitness, adiposity, and all-cause mortality in women. Med Sci Sports Exerc. 2010;42(11):2006–2012. doi: 10.1249/MSS.0b013e3181df12bf. [DOI] [PubMed] [Google Scholar]
- 29.Pollock ML, Bohannon RL, Cooper KH, et al. A comparative analysis of four protocols for maximal treadmill stress resting. Am Heart J. 1976;92(1):39–46. doi: 10.1016/s0002-8703(76)80401-2. [DOI] [PubMed] [Google Scholar]
- 30.Blair SN, Kannel WB, Kohl HW, Goodyear N, Wilson PWF. Surrogate measures of physical activity and physical fitness: Evidence for sedentary traits of resting tachycardia, obesiry, and low vital capacity. Am J Epidemiol. 1989;129(6):1145–1156. doi: 10.1093/oxfordjournals.aje.a115236. [DOI] [PubMed] [Google Scholar]
- 31.Kohl HW, Blair SN, Paffenbarger RS, Jr., Macera CA, Kronenfeld JJ. A mail survey of physical activity habits as related to measured physical fitness. Am J Epidemiol. 1988;127(6):1228–1239. doi: 10.1093/oxfordjournals.aje.a114915. [DOI] [PubMed] [Google Scholar]
- 32.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 33.Satterthwaite FE. An approximate distribution of estimates of variance components. Biometrics. 1946;2(6):110–114. [PubMed] [Google Scholar]
- 34.Reed W, Darity W, Roberson N. Health and Medical Care of African Americam. Auburn House; Westport, Conn: 1993. [Google Scholar]
- 35.Fryar CD, Hirsch R, Eberhardt MS, Yoon SS, Wright JD. Hypertension, high serum total cholesterol, and diabetes: racial and ethnic prevalence differences in U.S. adults, 1999-2006. NCHS Data Brief. 2010;(36):1–8. [PubMed] [Google Scholar]
- 36.Gillum RF, Mussolino ME, Madans JH. Body fat distribution and hypertension incidence in women and men. The NHANES I Epidemiologic Follow-up Study. Int J Obes Relat Metab Disord. 1998;22(2):127–134. doi: 10.1038/sj.ijo.0800554. [DOI] [PubMed] [Google Scholar]
- 37.Satcher D, Fryer GE, Jr, McCann J, Troutman A, Woolf SH, Rust G. What if we were equal? A comparison of the Black-White mortality gap in 1960 and 2000. Health Aff (Millwood) 2005;24(2):459–464. doi: 10.1377/hlthaff.24.2.459. [DOI] [PubMed] [Google Scholar]
- 38.Hardy D, Xia R, Liu CC, Cormier JN, Nurgalieva Z, Du XL. Racial disparities and survival for nonsmall-cell lung cancer in a large cohort of Black and White elderly patients. Cancer. 2009;115(20):4807–4818. doi: 10.1002/cncr.24521. [DOI] [PubMed] [Google Scholar]
- 39.Signorello LB, Schlundt DG, Cohen SS, et al. Comparing diabetes prevalence between African Americans and Whites of similar socioeconomic status. Am J Public Health. 2007;97(12):2260–2267. doi: 10.2105/AJPH.2006.094482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Howard BV. How do we evaluate and utilize data on ethnic differences? Ann Epidemiol. 1999;9(3):147–148. doi: 10.1016/s1047-2797(99)00002-2. [DOI] [PubMed] [Google Scholar]
- 41.Burchard EG, Ziv E, Coyle N, et al. The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med. 2003;348(12):1170–1175. doi: 10.1056/NEJMsb025007. [DOI] [PubMed] [Google Scholar]
- 42.Geschwender J. Social structure and the Negro Revolt: An examination of some hypotheses. Social Forces. 1964;43(2):248–256. [Google Scholar]
- 43.Dressler WW. Hypertension in the African American community: social, cultural, and psychological factors. Semin Nephrol. 1996;16(2):71–82. [PubMed] [Google Scholar]
- 44.Bowles S, Gintis H. Schooling in Capitalist America: Educational Reform and the Contradictiom of Economic Lift. Basic Books; New York: 1976. [Google Scholar]
- 45.Billingsley A. Climbing jacob's ladder; The Enduring Legacy of African-American Families. Simon & Schuster; New York: 1992. [Google Scholar]
- 46.Willie CV. The Caste and Class Recovery. General Hall, Inc; Dix Hills, NJ: 1979. [Google Scholar]
- 47.Nyman JA, Barleen NA, Dowd BE, Russell OW, Coons SJ, Sullivan PW. Quality-of-life weights for the US population: self-reported health status and priority health conditions, by demographic characteristics. Med Care. 2007;45(7):618–628. doi: 10.1097/MLR.0b013e31803dce05. [DOI] [PubMed] [Google Scholar]
- 48.McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med. 1993;153(18):2093–2101. [PubMed] [Google Scholar]
- 49.McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Horm Behav. 2003;43(1):2–15. doi: 10.1016/s0018-506x(02)00024-7. [DOI] [PubMed] [Google Scholar]
- 50.James SA, Hartnett SA, Kalsbeek WD. John Henryism and blood pressure differences among black men. J Behav Med. 1983;6(3):259–278. doi: 10.1007/BF01315113. [DOI] [PubMed] [Google Scholar]
- 51.Merritt MM, Bennett GG, Williams RB, Sollers JJ, III, Thayer JF. Low educational attainment, John Henryism, and cardiovascular reacovity to and recovery from personally relevant stress. Psychosom Med. 2004;66(1):49–55. doi: 10.1097/01.psy.0000107909.74904.3d. [DOI] [PubMed] [Google Scholar]
- 52.Jain T, Peshock R, McGuire DK, et al. African Americans and Caucasians have a similar prevalence of coronary calcium in the Dallas Heart Study. J Am Colt Cardiol. 2004;44(5):1011–1017. doi: 10.1016/j.jacc.2004.05.069. [DOI] [PubMed] [Google Scholar]
- 53.Ogden C, Carroll MD. Division of Health and Nutrition Examination Surveys. Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults: United States, Trends 1976-1980 Through 2007-2008. CDC; [Google Scholar]
- 54.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140(2):226–235. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 55.McDonald M, Hertz R, Lustik MB, Unger AN. Racial Differences in Diabetes Prevalence, Awareness, and T reatrnent: Findings from the National Health and Nutrition Examination Surveys (NHANES) III and 1999-2000 [Google Scholar]
- 56.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 57.Ware J, Sherbourne C. The MOS 36-Item Short-Form Health Survey (SF-36). Medical Care. 1992;30(6):437. [PubMed] [Google Scholar]
- 58.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch fntem Med. 2005;165(18):2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]