Abstract
Objective
To assess how exposures to community activities in residency impact anticipated future involvement in community child health settings.
Methods
Prospective cohort study of pediatric residents from 10 programs (12 sites) who completed training between 2003 and 2009. Residents reported annual participation for ≥8 days in each of 7 community activities (eg, community settings, child health advocacy) in the prior year. At the start and end of residency, residents reported anticipated involvement in 10 years in 8 community settings (eg, school, shelter). Anticipated involvement was dichotomized: moderate/substantial (“high”) versus none/limited (“low”). Logistic regression modeled whether residency exposures independently influenced anticipated future involvement at the end of residency.
Results
A total of 683 residents completed surveys at the start and end of residency (66.8% participation). More than half of trainees reported ≥8 days’ of involvement in community settings (65.6%) or child health advocacy (53.6%) in residency. Fewer anticipated high involvement in at least 1 community setting at the end of residency than at the start (65.5% vs 85.6%, P < .001). Participation in each community activity mediated but did not moderate relations between anticipated involvement at the start and end of residency. In multivariate models, exposure to community settings in residency was associated with anticipated involvement at end of residency (adjusted odds ratio 1.5; 95% confidence interval 1.2, 2.0). No other residency exposures were associated.
Conclusions
Residents who anticipate high involvement in community pediatrics at the start of residency participate in related opportunities in training. Exposure to community settings during residency may encourage community involvement after training.
Keywords: community health services, education, medical, graduate, graduate medical education, pediatrics/education
Pediatricians have defined their role to include promoting and advocating for children’s health at a population level and recognize the importance of training to prepare for these roles.1 Since 1997, the Pediatric Residency Review Committee has required that programs provide “structured educational experiences, with planned didactic and experiential opportunities for learning…. that prepare [residents] for the role of advocate for the health of children within the community.”2 In turn, residency programs have responded by investing curricular time and other resources to teach community pediatrics.3 The current Program Requirements for Residency Education in Pediatrics mandate that the 5 ambulatory units include elements of community pediatrics and child advocacy, and 6 educational units be individualized on the basis of residents’ learning needs and career plans.4
The Dyson Community Pediatrics Training Initiative (CPTI) provided 5 years of support to 10 residency training programs at 12 sites beginning in July 2000 to enhance community pediatrics training. These programs exposed trainees to different facets of community child health with the goal of developing pediatricians with “greater knowledge, skills, and interest in community-based medicine and advocacy to build capacity that results in child health improvement in their communities.”5 Through a combination of community-based and didactic experiences, residents acquired skills in community pediatrics with the hope they will engage in these types of activities and promote population child health throughout their careers.6 Each Dyson CPTI program adhered to a set of principles identified by the funder and tailored the program in collaboration with community partners and in ways that recognized the strengths of their communities and training programs. Thus, a single intervention common to all programs was not implemented. An independent evaluation, the Dyson Initiative National Evaluation (DINE) was conducted. Other residency initiatives including UCLA’s Community Health and Advocacy Training Program and Stanford’s Child Advocacy Curriculum also have supported innovative community pediatrics curricula.7,8
Despite increased national attention on community pediatrics training, there has been an overall decline in related activities among pediatricians in the United States. Forty percent of pediatricians reported involvement in any community activity in the previous 12 months in 2013 relative to 56.6% in 1989.9,10 In 2004, although the youngest pediatricians (≤34 years) reported the most training in community pediatrics before or during residency, they were least likely to engage in community activities to promote child health in the previous 12 months.11 In addition, younger pediatricians were less satisfied with their current level of participation. This discordance between actual and desired participation may reflect a disconnect between intent to participate in community pediatrics and conflicting work and personal demands. Yet, we know little about expectations for involvement at the end of residency and the impact of training. Given declining pediatrician involvement in community child health and the new Accreditation Council for Graduate Medical Education requirement to develop individualized curricula tailored to residents’ needs and career goals, it is important to understand residents’ expectations for community involvement.
Many factors may influence anticipated involvement in community activities when assessed at the end of residency including demographic characteristics,10,12,13 prior participation in community activities,14 predisposition to engage in community pediatrics at the end of medical school, and exposure to community activities during residency.1,15 Although personal upbringing and exposures before residency influence propensity for civic engagement,14 the role of exposures to community settings during residency on expectations for involvement after residency is largely unknown.
The objectives of this study were to examine how anticipated involvement in community child health activities changed from the start to end of residency, and whether exposure to community activities during residency mediated and/or moderated changes in anticipated involvement (Figure). This study recognized that anticipated involvement in community activities could change during residency and could be influenced by demographic characteristics, community involvement before residency, perceived importance of community involvement, and community involvement and source of guidance about community pediatrics during residency.
Figure.
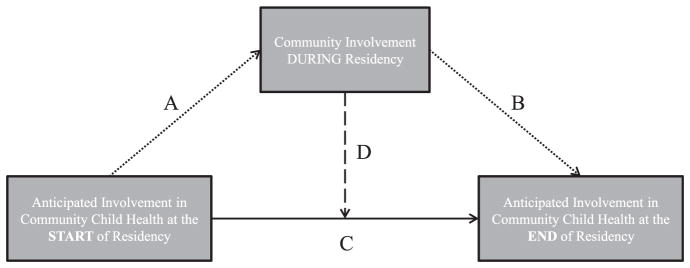
Paths A and B indicate the association between anticipated involvement in community child health at the start (independent variable) and end (dependent variable) of residency and the potential mediator, community involvement during residency. Path C indicates the unadjusted association between the independent and dependent variables. Path D denotes a moderation model in which the association between the independent and dependent variables change as a function of the community involvement during residency.
Methods
Sample
The data used in this study were from the DINE. Eligible participants included physicians who completed residency training at 1 of 10 CPTI-funded programs (12 sites) in the years 2003 to 2009, who responded to surveys at the beginning and end of residency, and who provided information at the end of residency regarding anticipated future involvement in community child health settings. Six CPTI programs were funded for 5 years beginning in 2000, and an additional 4 programs were funded for 5 years beginning in 2002. Sites included Columbia University in partnership with Harlem Hospital Center; Children’s Hospital of Philadelphia; Children’s Hospital of Wisconsin/Medical College of Wisconsin; University of California, San Diego, in partnership with San Diego Naval Medical Center; University of Hawaii; University of Rochester; University of California, Davis; University of Florida, Jacksonville; Indiana University; and University of Miami. Human subjects approval was obtained from the Johns Hopkins institutional review board.
Survey Instruments
Five surveys informed these analyses: 2 surveys completed at the start of residency (brief demographic and baseline surveys), and 3 annual surveys completed at the conclusion of each year of residency. The 8-question demographic survey included gender, race/ethnicity, and date of birth. The 12-question, multi-item survey of residents fielded at the beginning of residency assessed perceived importance of and involvement in community activities from the start of medical school until the start of residency and anticipated involvement in community activities 10 years from the time of survey completion. An 11-question multi-item annual survey included information on exposure to community activities during the past 12 months and anticipated involvement in community activities 10 years from the time of survey completion. Respondents reported marital and parental status and undergraduate and medical school debt at the end of residency. Paper-based surveys were used at the start of residency; subsequent surveys included web and paper-based, depending on preferences of CPTI program leaders. Survey content was informed by literature reviews, related AAP periodic surveys, and input from the DINE advisory committee.
Outcome Measure
The main outcome was anticipated future involvement in 1 or more of 8 community settings (eg, school, community health center) 10 years after completion of residency (Appendix online at http://www.academicpedsjnl.net). For each setting, residents used a 4-point Likert scale to indicate anticipated future involvement (1 = not at all, 4 = substantial). The responses for each setting were dichotomized into low involvement (not at all/limited) versus high involvement (moderate/substantial), and a dichotomous aggregate measure for high participation (moderate/substantial) in 1 or more community settings was generated.
Independent Variables
Independent variables included demographic characteristics (gender, race), personal characteristics at the end of residency (marital status, children, educational debt, contact with person who provides guidance and advice about community pediatrics), participation in and perceived importance of community activities from the beginning of medical school to the beginning of residency, exposures to community activities during residency training, and anticipated future involvement assessed at the start of residency. Age at the start of residency was calculated using date of birth.
Community Involvement Before Residency
Respondents indicated perceived importance of participation in 11 community settings and 4 additional community activities at the start of residency training (Appendix online at http://www.academicpedsjnl.net). Perceived importance during medical school in each of the 11 community settings and 4 additional activities was measured on a 4-point Likert scale (1 = none, 2 = limited, 3 = moderate, 4 = very). A dichotomous variable was created to indicate low (none/limited/moderate) versus high perceived importance (very). The cutoff used for variable dichotomization was based on variable distribution and our interest in those particularly motivated to engage in community child health during medical school. Likert responses to perceived importance in each of 11 community settings was combined into one dichotomous measure of low versus high perceived importance in 1 or more of the 11 community settings during medical school to capture importance of exposure to community settings. Perceived importance of each of 4 additional community activities was considered individually as a result of the distinct nature of these pursuits.
Extent of participation in each of the same 11 community settings and 5 additional activities in medical school (including tutoring) was reported. Participation was measured on a 4-point ordinal scale (1 = no participation, 2 = 1–7 days of participation, 3 = 8–30 days of participation, 4 = >30 days of participation). A dichotomous variable indicated ≤30 days versus >30 days of involvement. The cutoff used for variable dichotomization was based on variable distribution and our interest in those with especially high participation in community child health during medical school. Likert responses to extent of participation in each of the 11 community settings were combined into one dichotomous measure of ≤30 versus >30 days of involvement in 1 or more of the 11 community settings. Extent of participation in each of the 5 community activities was considered individually.
Community Involvement During Residency
At the end of each year, residents reported extent of involvement within the past 12 months in the same 11 community settings and additional community activities. Respondents provided their participation on a similar 4-point Likert scale in the same community activities captured at baseline and 2 additional activities: grand rounds related to community and other lectures/seminars focused on community. Resident reports of community experiences have been shown to be strongly correlated with reports by CPTI program leaders (data available upon request). To dichotomize exposures into low and high groups, residency participation data were converted to a binary measure (0 = no or 1–7 days of exposure, 1 = 8–30 or >30 days of exposure). The 8-day cutoff used for variable dichotomization was based on variable distribution and our interest in those with high participation given the time constraints of residency training. Dichotomized variables for each exposure in each year of residency were created and summed over all 3 years. The range of exposures for each of the 6 community activities is 0 to 3, where 0 is equal to no exposure of ≥8 days in any given year and 3 equals ≥8 days of exposure to at least 1 of the 6 activities in all 3 years of residency. For the 11 settings, we created a variable for each participant for each year in which 0 represented those participants with 0 to 7 days of participation in any setting in a given year and 1 represented ≥8 days of participation in at least 1 setting in a given year. These 3 annual values were summed to create an overall participation variable with a range 0 to 3, indicating the number of years with ≥8 days of participation in at least 1 setting.
Data Analysis
Chi-square statistics were used to compare respondents with high versus low anticipated future involvement in community activities at the start of residency on key demographic characteristics, perceived importance at the start of residency, and community involvement in medical school. Variables significant at the bivariate level (P < .05) or of known importance in the literature were entered into a multivariable logistic regression model to identify independent factors associated with anticipated future involvement in 1 or more community settings assessed at the end of residency. We used the Baron and Kenny16 approach to determine whether exposures during residency are independently associated with anticipated involvement at the end of training (moderator); we also assessed whether medical students predisposed to engage in community child health activities are more likely to engage in similar experiences as residents and thereby more likely to anticipate high involvement in the beginning of their careers (mediator).
Mediation was assessed using logistic regression to examine the association between the independent variable and the potential mediator, the independent variable and the dependent variable, and the multivariable model in which the independent and potential mediator were regressed on the dependent variable. Moderation was assessed using an interaction term between the potential moderator and the independent variable. Residency experiences were considered mediators if associations between the independent variable and the mediator and the independent variable and dependent variable were significant and if there was a 5% decrease in odds ratio after adding the mediator.
There were <1% missing data for demographic and anticipated future involvement; there were 9% to 15% missing data for exposure variables collected during residency, due largely to partial survey completion. We performed multiple imputation17 using CPTI site, graduation year, and gender to complete residency exposure data. There were no significant differences between the imputed and unimputed distributions. Analyses were conducted by Stata 11.0 software (StataCorp, College Station, Tex). Study participants received disclosure statements before each survey. CPTI sites annually received a small amount of funds to purchase lunch or gift cards for the residents in appreciation of their participation in the national evaluation.
Results
A total of 683 residents participated in DINE and reported anticipated involvement at the start and end of residency (66.8% participation). Respondents compared to nonrespondents were similar with regard to educational debt (73.8% vs 79.6%, P = .08). However, participants were more likely to be women (76.7% vs 63.4%) and underrepresented in medicine (13.6% vs 9.1%; both P <.05). Participants also were slightly younger than non-participants (median age 27.2 vs 27.7 years; P <.001).
Among respondents, 26.5% had at least 1 child, and 61.2% were married at the end of residency. At the start of residency, many trainees reported high perceived importance of participation in at least 1 community setting (60.3%) and advocacy for child health (45.7%, Table 1). Participants less commonly reported high perceived importance of committee membership (17.2%), community-based research (17.1%), and longitudinal community-based projects (17.3%). Forty-six percent of participants reported >30 days of participation in 1 or more community settings during medical school.
Table 1.
Participant Characteristics by Level of Anticipated Future Involvement in One or More Community Settings at Start of Residency* (n = 683)
| Characteristic | Total n (%) | Anticipated Future Involvement Reported at Start of Residency, n (%)
|
P Value† | |
|---|---|---|---|---|
| Low (n = 98)
|
High (n = 585)
|
|||
| n (%) | n (%) | |||
| Demographic characteristic | ||||
| Female | 496 (72.7) | 62 (12.5) | 434 (87.5) | .025 |
| Median age, y | 27.9 | 28.6 | 27.8 | .002 |
| Underrepresented in medicine‡ | 93 (13.6) | 12 (12.9) | 81 (87.1) | .756 |
| High perceived importance from time started medical school until beginning of residency | ||||
| In 1 or more setting§ | 412 (60.3) | 33 (8.0) | 379 (92.0) | <.0001 |
| Committee member for a medical school, local or national organization | 100 (17.2) | 6 (6.0) | 94 (94.0) | .009 |
| Community-based research | 95 (17.1) | 4 (4.2) | 91 (95.8) | NA |
| Longitudinal community-based project | 95 (17.3) | 2 (2.1) | 93 (97.9) | NA |
| Advocacy related to child health | 258 (45.7) | 16 (6.2) | 242 (93.8) | <.0001 |
| ≥30 d of participation from time started medical school until beginning of residency | ||||
| In 1 or more setting§ | 309 (45.5) | 34 (11.0) | 275 (89.0) | .025 |
| Committee member for a medical school, local or national organization | 175 (30.5) | 14 (8.0) | 387 (92.0) | .006 |
| Community-based research | 93 (16.9) | 11 (11.8) | 82 (88.2) | .552 |
| Longitudinal community-based project | 45 (8.3) | 3 (6.7) | 42 (93.3) | NA |
| Advocacy related to child health | 59 (10.6) | 2 (3.4) | 57 (96.6) | NA |
| Tutoring/mentoring individuals | 95 (16.4) | 5 (5.3) | 90 (94.7) | .007 |
NA = unable to calculate as a result of small cell sizes.
Includes school, day care center, Head Start program, juvenile justice detention center, shelter, community health center, local or state health department, camp for children with special needs.
P values indicates t test (continuous variables) and chi-squared (dichotomous variables) results for comparison between low and high anticipated future involvement reported at start of residency.
Includes Black/African American, Native Hawaiian/Other Pacific Islander, American Indian/Alaska Native, and Hispanic/Latino.
Includes settings above plus home visiting, Indian Health Service, and international health.
Participants reported anticipated future involvement in community settings at both the start and end of residency allowing us to identify factors associated with changing anticipated involvement. Sixty participants (8.7%) reported low involvement at both the beginning and end of residency, 38 participants (5.6%) reported low involvement at the start of residency and high involvement at the end of residency, 176 participants (25.8%) reported high involvement at the beginning and low involvement at the end of residency, and 409 (59.9%) reported high involvement at both time points. Those who reported high perceived importance and >30 days of participation in at least 1 community setting during medical school were also more likely to report higher anticipated involvement at the beginning of residency. Also, high perceived importance and participation in each additional activity at the beginning of residency were associated with high anticipated future involvement in community pediatrics reported at the beginning of training.
Over 65% of participants had ≥8 days of exposure to a community setting during at least 1 year of residency (Table 2). Thirty-four percent had 1 year of ≥8 days, 20.5% had 2 years of ≥8 days, and 10.7% had 3 years with ≥8 days. About half of all respondents reported at least 8 days of exposure in any given year to grand rounds related to community. There was substantial participation as a committee member, with over 20% of the sample having ≥8 days of participation in any year. Thirty-one percent of participants reported having ≥8 days of exposure to community-based research in at least 1 year during residency, while more than half of respondents had ≥8 days of exposure in 1 or more years of residency to advocacy related to child health.
Table 2.
Exposures to Community Pediatrics During Residency
| Characteristic | No. of Years With 8+ Days of Exposure
|
|||||
|---|---|---|---|---|---|---|
| 0
|
1
|
2
|
3
|
Median | SD | |
| n (%) | n (%) | n (%) | n (%) | |||
| In 1 or more setting* | 235 (34.4) | 235 (34.4) | 140 (20.5) | 73 (10.7) | 1 | 0.99 |
| Grand rounds related to community | 343 (50.2) | 190 (27.8) | 100 (14.6) | 50 (7.3) | 0 | 0.95 |
| Other lectures/seminars focused on community | 268 (39.2) | 206 (30.2) | 134 (19.6) | 75 (11.0) | 1 | 1.01 |
| Committee member for a medical school, local or national organization | 546 (79.9) | 81 (11.9) | 35 (5.1) | 21 (3.1) | 0 | 0.71 |
| Community-based research | 469 (68.7) | 123 (18.0) | 63 (9.2) | 28 (4.1) | 0 | 0.83 |
| Longitudinal community-based project | 401 (58.7) | 146 (21.4) | 92 (13.5) | 44 (6.4) | 0 | 0.93 |
| Advocacy related to child health | 317 (46.4) | 187 (27.4) | 122 (17.9) | 57 (8.4) | 1 | 0.98 |
SD = standard deviation.
Includes school, day care center, Head Start program, juvenile detention program, shelter, camp for children with special needs, community health center, local or state health department, home visiting, Indian Health Service, and international health.
In bivariate analyses, anticipated future involvement at the end of residency in 1 or more community settings was associated with anticipated involvement at the start of residency and high perceived importance at the start of residency in all 5 community activities (all P < .05, Table 3). Anticipated future involvement in 1 or more community settings at the end of residency also was associated with 30 days or more of participation in medical school in at least 1 community setting community-based research, and tutoring or mentoring (P < .05). Participants with at least 8 days of involvement in each of the 7 types of community related experiences were more likely to anticipate high involvement in at least 1 community setting (all P < .05). Moreover, participants who were in contact with a person who provided guidance and advice about community pediatrics more likely to have high anticipated involvement in 1 or more community settings at the end of residency as those who were not (odds ratio 1.8, 95% confidence interval 1.1, 2.7). In multivariate models adjusting for age and gender, ≥8 days of involvement in at least 1 community setting during residency remained associated with anticipated involvement at the end of residency (odds ratio 1.5, 95% confidence interval 1.2, 2.0). Each of the 7 community exposures in residency mediated but did not moderate relations between anticipated future involvement in community settings at the beginning and at the end of residency.
Table 3.
Factors Associated With Anticipated Future Involvement in One or More Community Settings Assessed at End of Residency
| Characteristic | Anticipated Involvement in 1+ Community Settings
|
|
|---|---|---|
| Bivariate Odds Ratio (95% CI) | Multivariate Odds Ratio* (95% CI) | |
| Anticipated involvement in 1 or more community settings at the start of residency | 3.7 (2.4, 5.7) | 1.1 (0.6, 2.2) |
| Demographic characteristics | ||
| Female sex | 1.3 (0.9, 1.9) | 1.3 (0.8, 2.2) |
| Underrepresented in medicine† | 1.0 (0.6, 1.6) | 0.7 (0.4, 1.4) |
| Has children at the end of residency | 0.8 (0.5, 1.1) | 0.8 (0.4, 1.3) |
| Educational debt (any) at the end of residency | 1.0 (0.7, 1.6) | 1.3 (0.7, 2.6) |
| High perceived importance at the start of residency | ||
| In 1 or more setting‡ | 1.6 (1.2, 2.2) | 1.1 (0.6, 1.9) |
| Committee member for a medical school, local or national organization | 1.9 (1.1, 3.1) | 1.0 (0.5, 2.2) |
| Community-based research | 3.0 (1.7, 5.4) | 0.7 (0.3, 2.0) |
| Longitudinal community-based project | 3.7 (2.0, 6.6) | 2.9 (1.0, 7.9) |
| Advocacy related to child health | 1.9 (1.3, 2.7) | 1.6 (1.0, 2.9) |
| >30 d of participation during medical school | ||
| In 1 or more setting‡ | 1.6 (1.2, 2.2) | 0.8 (0.5, 1.3) |
| Committee member for a medical school, local or national organization | 1.5 (1.0, 2.3) | 0.8 (0.4, 1.5) |
| Community-based research | 1.8 (1.1, 3.1) | 2.3 (1.0, 5.3) |
| Longitudinal community-based project | 1.9 (0.9, 4.0) | 0.6 (0.2, 2.1) |
| Advocacy related to child health | 1.8 (0.9, 3.4) | 1.4 (0.5, 4.0) |
| Tutoring/mentoring individuals | 3.6 (1.6, 4.9) | 2.2 (1.0, 5.0) |
| ≥8 d of community involvement during residency | ||
| In 1 or more setting‡ | 1.6 (1.3, 1.9) | 1.5 (1.2, 2.0) |
| Grand rounds related to community | 1.4 (1.1, 1.6) | 1.0 (0.7, 1.4) |
| Other lectures/seminars focused on community | 1.6 (1.4, 1.9) | 1.3 (1.0, 1.9) |
| Committee member for a medical school, local or national organization | 1.6 (1.2, 2.1) | 1.3 (0.8, 2.0) |
| Community-based research | 1.6 (1.3, 2.1) | 1.1 (0.8, 1.7) |
| Longitudinal community-based project | 1.4 (1.2, 1.7) | 0.9 (0.6, 1.2) |
| Advocacy related to child health | 1.3 (1.1, 1.6) | 1.1 (0.8, 1.4) |
| Contact with person who provides guidance and advice about community pediatrics | 1.8 (1.1, 2.7) | 1.7 (0.9, 3.2) |
CI = confidence interval.
Adjusted for site and age.
Includes Black/African American, Native Hawaiian/Other Pacific Islander, American Indian/Alaska Native, and Hispanic/Latino.
Includes school, day care center, Head Start program, juvenile justice detention center, shelter, community health center, local or state health department, camp for children with special needs, home visiting, Indian Health Service, and international health.
Discussion
This study demonstrated that residents with high anticipated involvement in 1 or more community settings at the start of residency were more likely at the end of residency to anticipate substantial future participation in community settings; this association was mediated by exposure to community settings in residency. Thus, residents who anticipated high involvement in community pediatrics at the start of residency appeared to participate in related opportunities in training. In addition, trainees who spent a significant amount of time in community settings in residency were more likely to anticipate higher involvement in the future, regardless of intent to engage in community pediatrics when assessed at the beginning of residency. These findings suggest that although exposures to community pediatrics may strengthen some residents’ predisposition to engage with their communities, these experiences also may enhance career participation for residents who were initially less interested in community involvement. These results are consistent with the study of Nader et al demonstrating that residents who participated in 1 specific community setting, schools, were more likely to be involved in this setting after training.15 Individualized curricula in residency may provide opportunities to modify training experiences to meet the evolving interests and learning needs of trainees.
Our findings suggest that exposures to community activities contribute to changing expectations for community involvement. Although predisposition to engage in community child health decreases over the course of residency, the results shed light into the potential for substantial exposure to community child health settings during residency to mitigate this decline. To our knowledge, this is the first study to formally evaluate how anticipated involvement in a broad array of community child health activities change from the start to the end of residency, and to evaluate whether exposures to community child health activities during residency influence these perspectives.
Although it is important to understand how exposures during residency impact actual involvement in community settings after training,6 theories of behavior change highlight that intentions strongly influence future decision making.18 The identification of specific experiences that are associated with plans for future participation in community child health at the end of residency reinforces the opportunity for program directors to include these targeted experiences in residency training. These findings support the value of placing trainees in community child health settings to either strengthen their interest in community child health or provide exposures that may influence future participation. The association between participation in a community child health setting during training and anticipated involvement in community child health at the end of residency is likely the result of 3 features common to many of these community settings: well-established partnerships between the community agencies and the residency program, the relationship building that occurs in these settings, and the acquisition of specific skills that occurs while working in these contexts.19
Although activities such as attendance at grand rounds related to community promote knowledge and skills, the contacts and relationships that are developed when residents work in partnership with community organizations may allow for greater understanding of the operations of organizations focused on improving population child health and the process of establishing and nurturing community partnerships. Developing community relationships and contacts may be critically important when attempting to reengage after time is spent establishing a career and family immediately after training. Moreover, the specific skills and strategies that are developed and utilized during on-site experiences in community agencies are often transferrable between settings. The lack of findings related to exposures to longitudinal projects and anticipated future involvement in 1 or more community settings likely reflects the high degree of variability of these projects across and within training programs.
We also observed no association between educational debt and anticipated future involvement. This may be due to other factors playing a more central role or limited variability in the sample, with nearly three-quarters reporting debt. Further efforts are needed to understand the interplay of family and personal obligations with employment choices as more graduates seek positions as salaried employees with organizations that prioritize clinical productivity over community involvement. Such an understanding may lead to additional residency interventions such as informing trainees about loan repayment programs.
Several limitations of this study should be noted. First, although theories of behavior change support the association between anticipated and actual involvement, we did not assess actual participation in community child health but rather used anticipated involvement as a proxy measure. Second, we used self-reported involvement before and during residency and were not able to verify the quality of the exposures; however, variability in exposures suggests respondents’ willingness to report low levels of involvement. Third, only 66.8% of those who started the evaluation process returned surveys at the end of residency; however, we observed few differences between those who did and those who did not return surveys.
Conclusions
Residents who anticipated high involvement in community settings at the start of residency participated in related opportunities in training. More specifically, exposure to community settings in residency was associated with anticipated future involvement and mediated the association between anticipation at the beginning and end of residency. Longitudinal follow-up of these trainees will help us understand how expectations translate into specific behaviors once pediatricians become established in their careers.
Supplementary Material
What’s New.
Pediatrics residents anticipating extensive community involvement at the start of residency are more likely to anticipate substantial future participation in community settings at the end of residency; this association is mediated by exposure to community settings in residency.
Acknowledgments
Supported in part by the Dyson Foundation (PIs Cynthia Minkovitz, Holly Grason, Bernard Guyer) and the Hopkins Population Center (R24-HD042854).
Footnotes
Supplementary data related to this article can be found online at http://dx.doi.org/10.1016/j.acap.2014.02.011.
The authors declare that they have no conflict of interest.
References
- 1.American Academy of Pediatrics Council on Community Pediatrics. Community pediatrics: navigating the intersection of medicine, public health, and social determinants of children’s health. Pediatrics. 2013;131:623–628. [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. [Accessed July 23, 2013];Program requirements for residency education in pediatrics. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/320_pediatrics_07012007.pdf.
- 3.Solomon BS, Minkovitz CS, Grason HA, Carraccio C. Community pediatrics: a consistent focus in residency training from 2002 to 2005. Ambul Pediatr. 2007;7:321–324. doi: 10.1016/j.ambp.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Accreditation Council for Graduate Medical Education. [Accessed July 23, 2013];Program requirements for residency education in pediatrics. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/320_pediatrics_07012013.pdf.
- 5.Palfrey JS, Hametz P, Grason H, et al. Educating the next generation of pediatricians in urban health care: the Anne E. Dyson community pediatrics training initiative. Acad Med. 2004;79:1184–1191. doi: 10.1097/00001888-200412000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Solomon BS, Grason HA, Swigonski N, et al. Residency training and use of strategies to promote community child health one year after graduation. Acad Pediatr. 2012;12:344–346. doi: 10.1016/j.acap.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 7.Kuo AA, Shetgiri R, Guerrero AD, et al. A public health approach to pediatric residency education: responding to social determinants of health. J Grad Med Educ. 2011;3:217–223. doi: 10.4300/JGME-D-10-00150.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chamberlain LJ, Sanders LM, Takayama JI. Child advocacy training: curriculum outcomes and resident satisfaction. Arch Pediatr Adolesc Med. 2005;159:842–847. doi: 10.1001/archpedi.159.9.842. [DOI] [PubMed] [Google Scholar]
- 9.Minkovitz CS, Grason H, Solomon BS, et al. Pediatricians’ involvement in community child health from 2004 to 2010. Pediatrics. 2013;132:997–1005. doi: 10.1542/peds.2013-1917. [DOI] [PubMed] [Google Scholar]
- 10.Minkovitz CS, O’Connor KG, Grason H, et al. Pediatricians’ involvement in community child health from 1989 to 2004. Arch Pediatr Adolesc Med. 2008;162:658–664. doi: 10.1001/archpedi.162.7.658. [DOI] [PubMed] [Google Scholar]
- 11.Minkovitz CS, O’Connor KG, Grason H, et al. Pediatricians’ perspectives regarding community child health: training, involvement, and expectations by age. Pediatrics. 2007;120:1036–1043. doi: 10.1542/peds.2007-0842. [DOI] [PubMed] [Google Scholar]
- 12.Minkovitz CS, Chandra A, Solomon BS, et al. Community pediatrics: gender differences in perspectives of residents. Ambul Pediatr. 2006;6:326–331. doi: 10.1016/j.ambp.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Gruen RL, Campbell EG, Blumenthal D. Public roles of US physicians: community participation, political involvement and collective advocacy. JAMA. 2006;296:2467–2475. doi: 10.1001/jama.296.20.2467. [DOI] [PubMed] [Google Scholar]
- 14.Minkovitz C, Grason H, Aliza B, et al. Evaluation of the community access to child health program. Pediatrics. 1999;103(6 pt 3):1384–1393. [PubMed] [Google Scholar]
- 15.Nader PR, Broyles SL, Brennan J, Taras H. Two national surveys on pediatric training and activities in school health: 1991 and 2001. Pediatrics. 2003;111(4 pt 1):730–734. doi: 10.1542/peds.111.4.730. [DOI] [PubMed] [Google Scholar]
- 16.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psych. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 17.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: J. Wiley; 2009. [Google Scholar]
- 18.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 19.Shipley LJ, Stelzner SM, Zenni EA, et al. Teaching community pediatrics to pediatric residents: strategic approaches and successful models for education in community health and child advocacy. Pediatrics. 2005;115(suppl 3):1150–1157. doi: 10.1542/peds.2004-2825J. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


