Abstract
Background: Hsp90-beta was investigated as prognostic factor because of its apparent association with tumorigenesis. The aim of this study was to investigate the expression of Hsp90-beta in lung cancer patients, to analyze the relationship with respect to the clinicopathological features and to assess whether Hsp90-beta as a potential serum marker for lung cancer. Methods: Expression of Hsp90-beta was examined using immunohistochemistry, in-situ hybridization, western blot and enzyme-linked immunosorbent assay. Sensitivities and specificities for Hsp90-beta serum test were determined using receiver operator characteristic curve and cutoff was defined based on 95% and 85% sensitivities. Results: Lung cancer tissues exhibited higher expression of Hsp90-beta than the normal tissues (P < 0.05) and the serum Hsp90-beta of lung cancer patients also exhibited higher level than control groups (P < 0.05). Moreover, increased serum Hsp90-beta was significantly associated with the pathological grade and clinical stage of lung cancer patients (P < 0.05). Using receiver operator characteristic curve analysis, the cutoffs for distinguishing lung cancer from normal and benign groups were 1.155 and 1.158 ng/ml respectively. The sensitivities of Hsp90-beta for distinguishing lung cancer from normal and benign groups were 98.77% and 95.9%, and specificities were 88.33% and 72.7%. Conclusion: Up-regulation of serum Hsp90-beta was associated with pathological grade and clinical stage of lung cancer patients, which indicated that it could be considered molecular biomarker for diagnosis and prognosis of lung cancer.
Keywords: Lung cancer, serum, Hsp90-beta, biomarker, diagnosis
Introduction
Lung cancer is a major public health problem in china and many other parts of the world. It is well known that the mortality of lung cancer is still very high although there are more achievements pertaining to the molecular mechanism of lung cancer recent years. Some people believe that the most critical reasons are the difficulties in making the early-stage diagnosis of lung cancer and the high recurrence rate after curative treatments. In fact, one of the major challenges in lung cancer research is the identification of stable biomarkers, which can be routinely measured in easily accessible samples and help making early-stage diagnosis. In patients with lung cancer, several serum biomarkers have been proposed to improve clinical diagnosis and treatment of lung cancer [1]. It is commonly understood that an early detection of cancer leads to a better chance for reduced mortality and morbidity. Thus, identification and validation of diagnostic and prognostic biomarkers is tremendously important to improve the clinical outcome of lung cancer treatments [2].
Previously, we has identified the increase of Hsp90-beta expression in the NCI-A549 and NCI-H446 lung cancer cells compared with the 16 HBE human bronchial epithelial cell lines using two-dimensional liquid chromatography-tandem mass spectrometry (2D-LC-MS/MS), and also identified up-regulation of Hsp90-beta in lung cancer tissues was associated with poor post-surgical survival time and lymphatic metastasis of lung cancer patients [3]. However, the origin and nature serum level of Hsp90-beta in lung cancer patients is still unknown. Heat shock protein 90 (Hsp90) is a highly abundant and evolutionarily conserved protein in eukaryotic cells. Five Hsp90 isoforms have been identified to date, which include the two major cytoplasmic isoforms, namely, Hsp90-alpha and Hsp90-beta [4]. Expression of Hsp90-beta has been shown to increase in some cancer tissues such as breast cancer and lung cancer [3,5], but compared with tissues, studying on its serum level and significance in lung cancer patients remains unclearly. In this study, the serum level of Hsp90-beta in lung cancer patients was measured and the clinical value of Hsp90-beta as serum diagnostic tool was assessed.
Material and methods
Patient population
From January 2010 to February 2013, total 268 primary lung cancer patients were enrolled into the study (Gansu Provincial People’s Hospital, Lanzhou, China; Department of oncology, Lanzhou University Second Hospital, Lanzhou, China; Second Affiliated Hospital, Xi’an Jiaotong University, Xi’an, China). The serum samples were collected before therapy. Eighty-two of 268 lung cancer patients underwent surgical resection and matched fresh cancer and adjacent normal tissues were also collected from these patients. All patients were divided according to the TNM classification of the International Association for The Study of Lung Cancer (IASLC, Seventh edition, 2009) [6]. The tumors were histologically subtyped and graded according to the third edition of the World Health Orga-nization guidelines. Male and female patients were included, with an age range of 41 to 84 years (median, 60.9 years). Clinical characteristics of patients were retrieved from the clinical records available and were assessed retrospectively (Table 1). From January 2010 to February 2013, the serum of 256 healthy examined peoples (a healthy physical examination) were collected as normal control, including 143 men and 113 women whose mean (±SD) age was 64±8.21 years. The benign lung disease group comprised 221 patients (65±3.1 years) hospitalized in just mentioned hospital. Those patients had benign lung disease of known etiology (chronic obstructive lung disease, acute infectious diseases, tuberculosis, asthma and diffuse noninfectious interstitial diseases). Written and informed consent was obtained individually from all the participants prior to inclusion and commencement of the study. This study was conducted in accordance with the guidelines the Ethics Committee of just mentioned hospital, by which it was approved.
Table 1.
Clinicopathological features of lung cancer cases (N=268)
| Group | Characteristics | Number (%) |
|---|---|---|
| Sex | ||
| Male | 197 (73.8%) | |
| Female | 71 (26.2%) | |
| Age | ||
| > 60 | 138 (51.8%) | |
| ≥ 60 | 130 (48.2%) | |
| Smoking | ||
| Severe | 130 (48.5%) | |
| Moderate | 4 (1.3%) | |
| Slight | 14 (5.1%) | |
| Never | 120 (45.1%) | |
| Histology | ||
| LAC | 83 (31.2%) | |
| LSCC | 146 (54.6%) | |
| SCLC | 39 (14.2%) | |
| Pathologic grade | ||
| Poorly differentiated | 99 (37.1%) | |
| Moderately differentiated | 84 (31.4%) | |
| Well-differentiated | 53 (19.9%) | |
| Undifferentiated | 32 (11.6%) | |
| Clinical staging | ||
| I-II | 71 (26.5%) | |
| III | 97 (36.5%) | |
| IV | 68 (25.4%) | |
| Unavailable | 32 (11.6%) | |
| Pleural invasion | ||
| absent | 72 (26.4%) | |
| Present | 196 (73.6%) | |
| Lymphatic invasion | ||
| Positive | 159 (59.32%) | |
| Negative | 78 (29.02%) | |
| Unavailable | 31 (11.66%) |
LAC, adenocarcinoma of the lung; LSCC, squamous cell carcinoma of the lung; SCLC, small cell lung cancer.
Immunohistochemistry (IHC)
The expression of Hsp90-beta was determined using an S-P combination of IHC techniques (UltraSensitive S-P Rabbit, Product Code: SP9000, Zhongshan Jinqiao biotech company, Beijing, China). IHC was strictly implemented according to the UltraSensitive S-P Rabbit kit and the first antibody concentration consisted of a rabbit anti-human Hsp90-beta polyclonal antibody was diluted according to 1:100 dilution (Product Code: BA0930, Bostere Biotech Company, Wuhan, China). The kit provided positive slices that served as the positive control sample, and an identical volume of PBS as a replacement to the primary antibody incubated in identical conditions was used as the negative control sample. Immunostaining was blindly evaluated according to a scoring method previously described [3]. At least ten randomly selected high-power fields and > 1,000 cells were counted for each section. Each specimen was scored according to the intensity of staining (intensity) and the area of staining (extent). The intensity was graded according to the following scale: 0, no staining; 1+, mild staining; 2+, moderate staining; 3+, intense staining. The extent was evaluated as follows: 0, no staining of cells in any microscopic fields; 1+, < 30% of tissue stained positive; 2+, between 30% and 60% stained positive; 3+, > 60% stained positive. A combined staining score (intensity + extension) of ≤ 2, between 3 and 4, and between 5 and 6 were considered as low, moderate, and high expression levels, respectively.
In-situ hybridization (ISH)
The mRNA expression of Hsp90-beta was determined by ISH. The probe sequence of Hsp90-beta was 5’-TACCA GTGCT GCTGT AACTG AAGAA ATGCC-3’. The probe was synthesized in a DNA synthesizing instrument (Bostere biotech company, Wuhan, China). ISH was strictly performed according to the ISH kit (Product Code: MK1152, Bostere biotech company, Wuhan, China). The negative control samples included the following: (i) RNase treatment (20 mg/ml) hybridization and (ii) use of neither probes nor anti-Digoxigenin antibody; the controls exhibited no positive signals. The positive controls included the positive slices provided by the kit and the combined use of ISH and IHC. The mRNA level of Hsp90-beta exhibited positive staining in the cytoplasm. A specific scoring method for ISH was performed according to a previously published report [7]. The scoring method was as follows: according to the signal intensity, the signals were divided into 4 groups, namely, absent (0), low (+), moderate (++), and high (+++). For statistical analysis, we grouped the patients as low (0, +), moderate (++), and high (+++).
Western blot analysis (WB)
The harvested cells were washed once with PBS, lysed with 2× sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE) sample buffer (20 mM Tris, pH 8.0, 2% SDS, 2 mM dithiothreitol, 1 mM Na3VO4, 2 mM EDTA, and 20% glycerol), and boiled for 5 min. The protein concentration of each sample was determined using a Micro-BCA protein assay. In all samples, 30 μg of the total cellular protein was loaded on a 10% SDS-PAGE gel and electrophoretically separated. The proteins were transferred to polyvinylidene difluoride membranes. The membranes were blocked for 2 h at 37°C in 20 mM Tris, pH 8.0, 150 mM NaCl, and 0.05% Tween 20 (TBST) containing either 5% BSA or 5% nonfat dried milk. The membranes were incubated with anti-Hsp90-beta antibody (for immunoblotting with anti-Hsp90-beta was 1:200) overnight at 4°C. The primary antibody was detected using horseradish peroxidase-conjugated secondary antibodies, and after three washes with TBST, positive signals were visualized using the enhanced chemiluminescence method. All experiments were performed for three separate times.
Enzyme-linked immunosorbent assay (ELISA)
Serum samples were obtained immediately before therapy start, after having obtained an informed consent. Collected blood was allowed to clot and was centrifuged within 3 days (3000 rpm for 10-15 minutes). Sera were harvested and frozen at -70°C. The numbering of all of the samples was done double blinded. Any serum sample demonstrating hemolysis was considered invalid and excluded from the study. Serum level of Hsp90-beta was measured by sandwich-type ELISA that was originally developed using rabbit anti-human Hsp90-beta antibodies. The assay was performed following the directions given by the manufacturer (Hsp90-beta product Code: CK-E11190H, Xitang biotech company, Shanghai, China). In brief, for detection of Hsp90-beta in serum, 96-well flexible microtiter plates (Xitang biotech company, Shanghai, China) were coated with diluted serum samples in PBS (pH 7.4) containing 1% BSA. The wells were incubated for 1 h with 10 ng/ml of monoclonal anti-Hsp90-beta antibody at 37°C, followed by reaction with avidin-conjugated peroxidase (Dako Cytomation) using a Substrate Reagent (R&D Systems) at 37°C for 15 min. The color reaction was terminated by addition of 50 μl 2 N sulfuric acid and the intensity was determined by a photometer at a wavelength of 450 nm. Standard curve was drawn for each plate using concentration of the standard sample and corresponding OD value of each well.
Statistical analysis
The SPSS 21.0 software package was used to perform the statistical analysis (SPSS Institute, version 21.0, Chicago, USA). The expression of mRNA and protein of Hsp90-beta between normal and cancerous tissues was analyzed using the χ2 and Fisher’s exact. The serum Hsp90-beta was evaluated using the Student’s T-test, One-WAY ANOVA and Kruskal Wallis Test. Receiver operating characteristic (ROC) curves were constructed to evaluate the performance of serum Hsp90-beta for differentiating lung cancer patients. All tests were two-sided, and P-values < 0.05 were considered to be statistically significant.
Results
Increased expression of Hsp90-beta in matched lung cancer tissues than adjacent-cancer normal tissues
The mRNA and protein expression level of Hsp90-beta were determined using ISH and IHC respectively. High expression of Hsp90-beta protein was observed in fifty-five (66.7%) of the 82 lung cancer tissues, whereas were expressed in seven (8.3%) of the 82 normal lung tissues respectively (P < 0.0005). The mRNA of Hsp90-beta was also higher expressed in 82 lung cancer tissues (41.8%) than normal lung tissues (8.3%) respectively (P < 0.0005). Up-regulated mRNA and protein expression of Hsp90-beta were found in the lung cancer tissues (Table 2, Figures 1A-F, 2A and 2C). High mRNA and protein expression of Hsp90-beta were observed in thirty-five (41.8%) and fifty-five (66.7%) of the 82 lung cancer tissues, whereas were lowly expressed in seven (8.3%) of the 82 normal lung tissues respectively (P < 0.0005). The results indicated that mRNA expression of Hsp90-beta was consistent with protein expression (P < 0.0005) (Table 2, Figure 2B and 2D).
Table 2.
Differential mRNA and protein expression of Hsp90-beta between the lung cancer tissues and adjacent-cancer normal tissues (N=82)
| Groups | N | Expression of Hsp90-beta | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| - (%) | + (%) | ++(%) | χ2 value | P value | |||
| mRNA | |||||||
| Normal | 82 | 44 (54.2) | 31 (37.5) | 7 (8.3) | 59.98 | < 0.0005 | |
| Cancerous | 82 | 13 (16.6) | 34 (41.6) | 35 (41.8) | |||
| Protein | |||||||
| Normal | 82 | 24 (29.2) | 51 (62.5) | 7 (8.3) | 39.51 | < 0.0005 | |
| Cancerous | 82 | 7 (8.3) | 20 (25) | 55 (66.7) | |||
|
| |||||||
| Kappa value★ | P value | ||||||
|
|
|||||||
| Normal | |||||||
| mRNA | 82 | 44 (54.2) | 9 (37.5) | 7 (8.3) | 0.895 | < 0.0005 | |
| Protein | 82 | 24 (29.2) | 51 (62.5) | 7 (8.3) | |||
| Cancerous | |||||||
| mRNA | 82 | 13 (16.6) | 34 (41.6) | 35 (41.8) | 1.002 | < 0.0005 | |
| Protein | 82 | 7 (8.3) | 20 (25) | 55 (66.7) | |||
Kappa coefficient.
Figure 1.
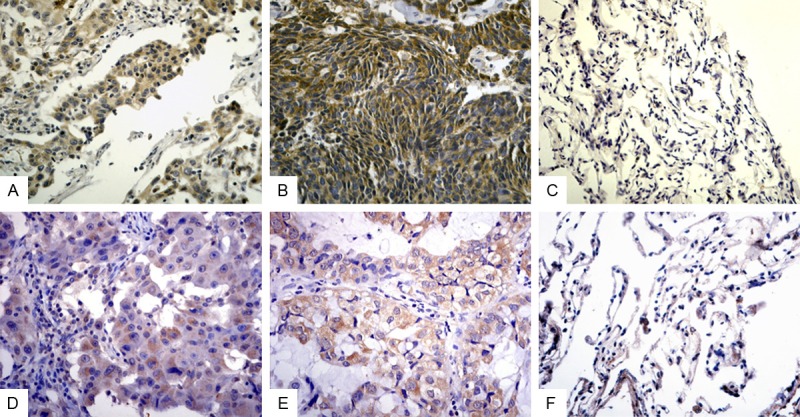
Expression of Hsp90-beta in lung cancer and adjacent-cancer normal tissues (×400). A. High staining of Hsp90-beta in poorly differential LSCC; B. High staining of Hsp90-beta in SCLC; C. Low staining of Hsp90-beta in adjacent normal tissues; D. High staining of Hsp90-beta mRNA in poorly differential LSCC; E. High staining of Hsp90-beta mRNA in poorly differential LAC; F. Low staining of Hsp90-beta mRNA in adjacent normal tissues; LSCC, squamous cell carcinoma of the lung; LAC, adenocarcinoma of the lung; SCLC, small cell lung cancer.
Figure 2.
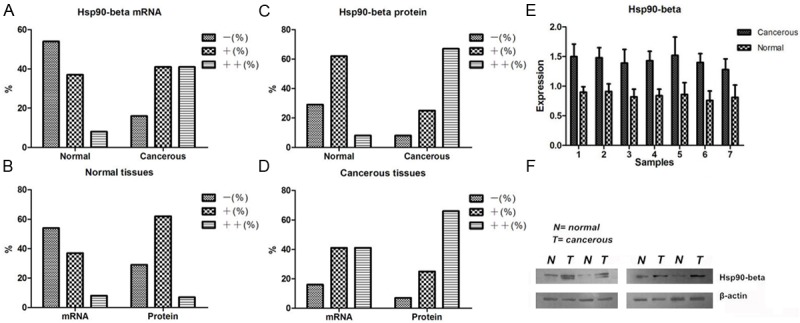
Expression rates of Hsp90-beta in lung cancer and adjacent-cancer normal tissues. A, C. up-regulated mRNA and protein expression of Hsp90-beta were found in the lung cancer tissues; B, D. expression of Hsp90-beta mRNA was consistent with protein expression; E, F. western blotting showed high expression of Hsp90-beta in cancer tissues than adjacent normal tissues (P < 0.05). Normal, adjacent-cancer normal tissues; cancerous, lung cancer tissues; N=normal tissues; T=tumor tissues.
Coincidence rate of mRNA and protein expressions of Hsp90-beta
We performed Western blot to test the expressions of Hsp90-beta in matched lung cancer tissues and adjacent-cancer normal tissues and to verify their differential expressions trend. Equal protein loading was indicated by a parallel β-actin blot experiment. As shown in Figure 2, Hsp90-beta was up-regulated in cancerous tissues compared with normal tissues (P < 0.05) (Figure 2E, 2F). To assess expression trends of three methods (IHC, ISH and Western blot), nonparametric test was performed. The results showed coincidence rates of Hsp90-beta expression using three different methods was 88%, and indicated three methods have a consistent trends.
Increased serum level of Hsp90-beta in lung cancer patients than normal and benign groups
Serum level of Hsp90-beta was detected by enzyme-linked immunosorbent assay in a series of 268 specimens of lung cancer patients, a series of 221 specimens of benign lung diseases and a series of 256 specimens of healthy examined peoples. The results shown serum level of annexin A1 was higher in lung cancer patients (1.34±0.09 pg/ml) than in benign lung diseases group (1.04±0.21 pg/ml) and healthy examined peoples (0.95±0.19 pg/ml) (P < 0.0005) (Table 3, Figure 3A).
Table 3.
Correlation between the serum level of Hsp90-beta and clinicopathologic factors of lung cancer patients
| Groups | N | Level of Hsp90-beta | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| M±SD (pg/ml) | df | F | P | |||
| Resource | ||||||
| Normal | 256 | 0.95±0.19 | 2 | 81.79 | < 0.0005 | |
| Benign | 221 | 1.04±0.21 | ||||
| Cancerous | 268 | 1.34±0.09■ | ||||
| Histology | ||||||
| LAC | 83 | 1.34±0.089 | 2 | 57.65 | < 0.0005 | |
| LSCC | 146 | 1.32±0.092 | ||||
| SCLC | 39 | 1.39±0.069★ | ||||
| Pathologic grade | ||||||
| Undifferentiated | 32 | 1.39±0.069★★ | 3 | 113.13 | < 0.0005 | |
| Poorly | 99 | 1.39±0.055★★ | ||||
| Moderate | 84 | 1.32±0.063 | ||||
| Well | 53 | 1.23±0.084 | ||||
| Lymphatic invasion | ||||||
| N0 | 69 | 1.26±0.10 | 3 | 63.19 | < 0.0005 | |
| N1-N2 | 103 | 1.35±0.058★★★ | ||||
| N3 | 60 | 1.39±0.066★★★ | ||||
| Unavailable | 36 | 1.33±0.23 | ||||
| TNM stage | ||||||
| I-II | 71 | 1.24±0.09 | 2 | |||
| III-IV | 165 | 1.36±0.06▲ | 102.49 | < 0.0005 | ||
| Unavailable | 32 | 1.30±0.11 | ||||
| Pleural invasion | ||||||
| absent | 72 | 1.34±0.089 | 2 | 72.67 | < 0.0005 | |
| Present | 196 | 1.33±0.23 | ||||
LAC, adenocarcinoma of the lung; LSCC, squamous cell carcinoma of the lung; SCLC, small cell lung cancer; LCLC, large cell lung cancer;
cancerous group compared with benign and normal group;
SCLC compared with LAC and LSCC;
undifferentiated and poorly compared with moderate and well;
N1-N3 compared with N0;
III-IV compared with I-II;
M±SD, mean±standard deviation; df, degree of freedom.
Figure 3.
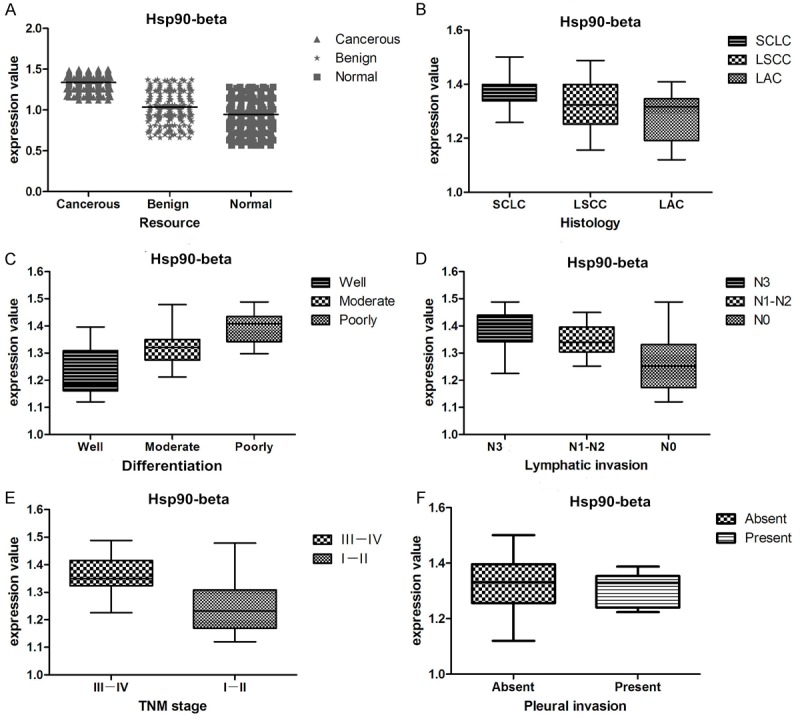
Correlation between serum level of Hsp90-beta and clinicopathologic factors of lung cancer patients. A. Increased serum level of Hsp90-beta in lung cancer patients than benign and normal control groups; B. Increased serum level of Hsp90-beta in SCLC than LSCC and LAC; C. Undifferentiated and poorly undifferentiated patients revealed up-regulated level of Hsp90-beta than moderate and well differentiation; D. Lymphatic invasion patients (N1-N3) revealed increased level of Hsp90-beta than non-lymphatic invasion; E. Patients of III-IV stage had higher Hsp90-beta value than both the I-II stage; F. Serum level of Hsp90-beta was not significant difference about pleural invasion. LAC, adenocarcinoma of the lung; LSCC, squamous cell carcinoma of the lung; SCLC, small cell lung cancer; N, node stage (TNM classification).
Correlation between the serum level of Hsp90-beta and clinicopathologic factors
Mean values of various clinical and biochemical parameters measured in different group are given in Table 3. Different groups showed significant differences with respect to the following parameters: SCLC patients (1.39±0.039 pg/ml) demonstrated a higher level of Hsp90-beta than LSCC (1.32±0.092 pg/ml) and LAC patients (1.34±0.089 pg/ml) (P < 0.0005); undifferentiated (1.39±0.069 pg/ml) and poorly undifferentiated patients (1.39±0.055 pg/ml) revealed up-regulated level of Hsp90-beta than moderate and well differentiation (P < 0.0005); lymphatic invasion patients (N1-N3) revealed increased level of Hsp90-beta than non-lymphatic invasion (1.26±0.10 pg/ml) (P < 0.0005); patients of III-IV stage (1.36±0.06 pg/ml) had higher Hsp90-beta (P < 0.0005) value than both I and II stage (1.24±0.09 pg/ml) (Table 3, Figure 3B-F).
Cut-off of serum Hsp90-beta for differentiating lung cancer patient from benign lung disease patient and normal people
The cut-off for serum value of Hsp90-beta in lung cancer patients were selected based on receiver operating characteristic (ROC) curve analysis [8]. The sensitivity and specificity for the outcome under study were plotted, thus generating an ROC curve. The minimum value that was tested by enzyme-linked immunosorbent assay was 0.57 pg/ml and located in the healthy control group and the maximum was 1.501 pg/ml, distributing in the lung cancer group. It shown that the values of lung cancer and healthy groups intersected near by value of 1.1-1.2 pg/ml as well as lung cancer and benign groups, which indicated that their thresholds must be in the segment of 1.1-1.2 pg/ml, and 95% confidence interval were 0.24 to 0.506 and 0.442 to 1.071 respectively (Figure 4A, 4B, 4D, 4E).
Figure 4.
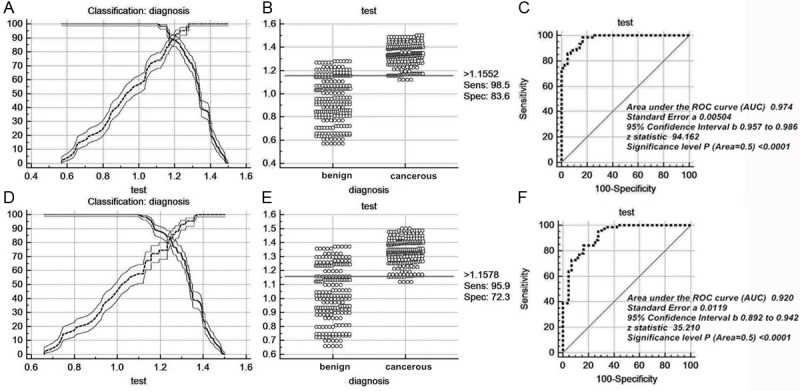
Cut-off selection of serum Hsp90-beta by ROC curve analysis. A-C. selection of cut-off for serum value of Hsp90-beta in distinguishing lung cancer patients from normal group; receiver operating characteristic curves for Hsp90-beta [area under the curve (auc): 0.976]; D-F. selection of cut-off for serum value of Hsp90-beta in distinguishing lung cancer patients from benign group; receiver operating characteristic curves for Hsp90-beta [area under the curve (auc): 0.920]. ROC, receiver operating characteristic curve; Sens, sensitivity; Spec, specificity.
Accuracy of parameters for predicting lung cancer by ROC analysis
When compared lung cancer patients with healthy examined people, the threshold of Hsp90-beta was 1.155 pg/ml. Thus the sensitivity and specificity were 98.5% and 83.6% respectively, which indicated that this threshold could be used to discriminate lung cancer patients from normal people. When compared lung cancer patients with benign lung disease patients, the value of 1.158 pg/ml could be used to discriminate lung cancer patients from benign lung disease patients. We noticed that the sensitivity was still higher (95.9%) but the specificity decreased significantly, which meant that Hsp90-beta may have a better diagnostic ability in discriminating lung cancer from normal group than benign group (Table 5). Figure 4C, 4F) depicts receiver operating characteristic (ROC) curves for Hsp90-beta when cancer group were compared with benign and healthy groups. To discriminate lung cancer from healthy people, the area under the curve (AUC) of Hsp90-beta was 0.974, Standard error was 0.00504, 95% confidence interval was 0.957-0.986, Z value was 94.162 (P < 0.0001) while to discriminate lung cancer from benign lung patients, the area under the curve (AUC) was 0.920, Standard error was 0.0119, 95% confidence interval was 0.892-0.942, Z value was 35.21 (P < 0.0001). The results displayed that serum Hsp90-beta contributes not only to the differentiated diagnosis of lung cancer patients and benign lung patients, but also to the screening of lung cancer, there for promoting early diagnosis of lung cancer as well.
Table 5.
Cut-off score of Hsp90-beta serum level for differentiating lung cancer patients from normal and benign groups
| Selection of cut-off score for serum value of Hsp90-beta in lung cancer patients and healthy examined peoples | ||||
|
| ||||
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI |
|
| ||||
| > 1.1058 | 100.00 | 95.5-100.0 | 73.81 | 63.1-82.8 |
| > 1.1438 | 98.77 | 93.3-100.0 | 78.57 | 68.3-86.8 |
| > 1.1552* | 98.77 | 93.3-100.0 | 83.33 | 73.6-90.6 |
| > 1.173 | 90.12 | 81.5-95.6 | 85.71 | 76.4-92.4 |
| > 1.212 | 87.65 | 78.5-93.9 | 92.86 | 85.1-97.3 |
| > 1.232 | 85.19 | 75.6-92.1 | 95.24 | 88.3-98.7 |
| > 1.2806 | 75.31 | 64.5-84.2 | 100.00 | 95.7-100.0 |
|
| ||||
| Selection of cut-off score for serum value of Hsp90-beta in lung cancer patients and benign lung disease patients | ||||
|
| ||||
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI |
|
| ||||
| > 1.097 | 100.00 | 98.6-100.0 | 57.73 | 50.9-64.3 |
| > 1.12 | 98.51 | 96.2-99.6 | 57.73 | 50.9-64.3 |
| > 1.1331 | 98.51 | 96.2-99.6 | 67.27 | 60.6-73.4 |
| > 1.1578* | 95.90 | 92.8-97.9 | 72.27 | 65.9-78.1 |
| > 1.232 | 84.33 | 79.4-88.5 | 74.55 | 68.3-80.2 |
| > 1.2965 | 72.76 | 67.0-78.0 | 93.18 | 89.0-96.1 |
| > 1.3212 | 63.81 | 57.7-69.6 | 95.45 | 91.8-97.8 |
| > 1.3706 | 38.81 | 32.9-44.9 | 100.00 | 98.3-100.0 |
95% CI, 95% confidence;
threshold of serum annexin A1 for differentiating lung cancer patient from benign lung disease patient and normal people.
Table 4.
NLR and PLR of Hsp90-beta serum level in cancerous, benign and normal groups
| NLR and PLR of Hsp90-beta serum concentration in lung cancer patients and healthy examined peoples | ||||
|
| ||||
| Interval | Positive | Negative | Likelihood ratio | 95% CI |
|
| ||||
| 0.4-0.6 | 0 | 6 | 0.000 | 0.000 to 1.418 |
| 0.6-0.8 | 0 | 56 | 0.000 | 0.000 to 0.137 |
| 0.8-1.0 | 0 | 79 | 0.000 | 0.000 to 0.0970 |
| 1.0-1.2 | 31 | 85 | 0.348 | 0.240 to 0.506 |
| 1.2-1.4 | 169 | 30 | 5.381 | 3.798 to 7.625 |
| 1.4-1.6 | 68 | 0 | ∞ | 8.086 to ∞ |
| Total | 268 | 256 | ||
|
| ||||
| NLR and PLR of Hsp90-beta serum concentration in lung cancer patients and benign lung diseases patients | ||||
|
| ||||
| Interval | Positive | Negative | Likelihood ratio | 95% CI |
|
| ||||
| 0.6-0.7 | 0 | 11 | 0.000 | 0.000 to 0.699 |
| 0.7-0.8 | 0 | 28 | 0.000 | 0.000 to 0.239 |
| 0.8-0.9 | 0 | 20 | 0.000 | 0.000 to 0.338 |
| 0.9-1.0 | 0 | 41 | 0.000 | 0.000 to 0.162 |
| 1.0-1.1 | 0 | 28 | 0.000 | 0.000 to 0.239 |
| 1.1-1.2 | 31 | 37 | 0.688 | 0.442 to 1.071 |
| 1.2-1.3 | 48 | 41 | 0.961 | 0.659 to 1.401 |
| 1.3-1.4 | 121 | 15 | 6.622 | 3.992 to 10.984 |
| 1.4-1.5 | 65 | 0 | ∞ | 6.642 to ∞ |
| 1.5-1.6 | 3 | 0 | ∞ | 0.248 to ∞ |
| Total | 268 | 221 | ||
NLR, negative likelihood ratio; PLR, positive likelihood ratio; 95% CI, 95% confidence interval.
Discussion
Circulating proteins hold great promise as a new class of cancer biomarkers due to their high stability in plasma, association with disease states, and ease of sensitive measurement. Cancer biomarkers are expected to not only predict the predisposed factors but also diagnose cancer patients at early of their stage. Early diagnosis of lung cancer is the most important determinant of survival of patients. Over the past many years, carcinoembryonic antigen (CEA), neuron-specific enolase (NSE), cytokeratin 19 fragment (CYFRA21-1) and squamous cell carcinoma antigen (SCC) have been used as biomarker for the diagnosis and management of patients with lung cancer [9,10]. However, specific marker of lung cancer is extremely absent. One of the reasons with these tumor markers is the lack of lung cancer specificity, thus researchers never stopped exploring new valuable biomarkers for diagnosis and prognostic in lung cancer. There are several distinct types of cancer biomarkers based on different areas: genetics, epigenetics, proteomics and metabolomics. Proteomics techniques include mass spectrometry (MS), ELISA, and immunohistochemistry etc., and utilize these tools to discover novel cancer biomarkers and validate them in clinical trials. Since cancer biomarker discovery has started extensively with the progress of proteomic technology, many protein molecules have been indicated as potential cancer biomarkers [11]. Previously, we has identified the increase of Hsp90-beta expression in the NCI-A549 and NCI-H446 lung cancer cells compared with the 16 HBE human bronchial epithelial cell lines using two-dimensional liquid chromatography-tandem mass spectrometry (2D-LC-MS/MS). Hsp90 over-expression has been related to the prognosis and evolution of neoplasia and is considered the classic chaperone family in cancer. There are two main isoforms of Hsp90, Hsp90α and Hsp90-beta. A study of various tumor cell lines revealed that Hsp90-beta were expressed in HCT116 and HeLa cells. In addition, Hsp90-beta was found in Saos-2 (osteosarcoma), SK-N-SH, HL-60 (acute promyelocytic leukemia) and A375 (malignant melanoma) cell lines [12]. At present the research of Hsp90-beta expression pattern in lung cancer is confine to basic research in vitro, so the serum expression status of lung cancer patients is merely studied. To uncover the epidemiologic features of Hsp90-beta and its clinicopathological significance in lung cancer, Hsp90-beta expression in lung cancer clinical specimens were detected and its relationships with clinicopathological factors were evaluated in our study.
In the histological level, our results showed that Hsp90-beta mRNA and protein exhibited higher expression in all histological types of lung cancer, and in particular in poorly differentiated lung cancer. The high expression of Hsp90-beta was shown to be intimately involved in tumor cell lymph node invasion, larger tumor size and high TNM stage according to our study. Thus, we may infer that higher Hsp90-beta expression is potentially effective in development of lung cancer. These findings are in concordance with previous reports showing that a higher level of Hsp90-beta in cancer is associated with a poor clinical outcome compared with patients who express lower levels of Hsp90-beta [13-16], suggesting that increased expression of Hsp90-beta in the cytoplasm of the tumor cells may contribute to the progression of cancer. When tested coincidence rate of mRNA and protein expressions of Hsp90-beta in matched lung cancer tissues and adjacent-cancer normal tissues, the results indicated that mRNA expression of Hsp90-beta was consistent with protein expression. In order to assess expression trend of three methods (IHC, ISH and Western blot), nonparametric test was performed. The results shown coincidence rate of Hsp90-beta expression using three different methods was 88%, and indicated three methods have a consistent trend. Via the coincidence rate test, the result indicated that the level of transcription and translation of Hsp90-beta is more stable, which is crucial to expression stability of tumor biomarker, and patently strengthen the evidence of high expression of Hsp90-beta in lung cancer cells. It is obvious that the strength of evidence in both of mRNA and protein expression surpasses single expression. Combined detection of both is better than each of them, and is more accurate. For example, amplification or overexpression of HER-2/neu is seen in approximately 20 to 30% of invasive breast cancers and this has been considered to be an adverse prognostic factor in many studies. Immunohistochemistry and fluorescence in situ hybridization have emerged as the most viable assays for evaluation of HER-2/neu in routine clinical practice. However, each of these methods has its advantages and disadvantages [17]. So the combined test of mRNA and protein in cancer tissues has big practical value.
In recent years, a large number of biomarkers for lung cancer have been examined in serum, such as CEA, NSE, CYFRA21-1 and so on. In our study, serum level of Hsp90-beta of lung cancer patients was compared with two control groups without lung cancer. Median level of Hsp90-beta was found to be significantly higher in patients with lung cancer than healthy control and benign lung disease control, thus displaying a significant association between the high serum level and an increased risk for lung cancer. In addition, lung cancer with the high serum level of Hsp90-beta is more likely to show an aggressive phenotype being exemplified by large tumor size and lymphatic metastasis. These results seem to suggest a possibility that the serum level of Hsp90-beta could be risk factor for lung cancer and to provide a new insight into understanding of the association between Hsp90-beta and lung cancer. The up-regulation of Hsp90-beta in serum was observed in SCLC, compared with LSCC and LAC, which suggests that the up-regulation of Hsp90-beta may be particularly related to the malignant invasion of SCLC. Clinically, in SCLC early distant metastasis occurs more frequently than with other histological types. It is well understood that SCLC is more aggressive and often metastasizes widely before the primary tumor mass in the lung reaches a large size, and further research is needed to explore the relationship between SCLC and Hsp90-beta.
Cutoff for Hsp90-beta for the diagnosis of lung cancer at specificity was determined by ROC curve analysis. Logistic regression analysis, using ROC-derived cutoff value, was used to determine the sensitivity of Hsp90-beta. At predefined specificity of 83.3% for distinguishing lung cancer from absence of disease (healthy subjects), the sensitivity was 98.8%. Meanwhile, when distinguishing the lung cancer group from the benign group, Hsp90-beta specificity was 77.8% and 78.9% respectively, which displayed that the ability of Hsp90-beta was higher in discriminating lung cancer from normal group than benign group. We adopted the cut-off levels derived from the ROC analysis, corresponding to 1.155 and 1.158 pg/ml for Hsp90-beta, which showed the best compromise between sensitivity and specificity in predicting lung cancer. When benign group were used as the control, the ROC AUC yielded Hsp90-beta cutoff of 1.158 pg/ml and demonstrating that the value might provide clinically meaningful cutoff in the diagnosis of lung cancer by providing an optimal sensitivity and specificity balance in lung patients. However, this study had several limitations. Firstly, it was conducted at a single center in China, which may limit generalizability of the findings to the wider population. Secondly, the study was not sufficiently powered to assess differences in marker level between early and advanced lung cancer. Therefore, further experimental investigations involving a larger number of samples of lung cancer patients are required to reach a more definitive conclusion. Besides, our preliminary results need to be confirmed by a prospective study including a large number of subjects as well as by the functional analysis of Hsp90-beta through in vitro studies in the future. As lung cancer is a highly malignant respiratory system tumor, a detailed understanding of the function and significance of Hsp90-beta will help to further elucidate the biological mechanisms of lung cancer and aid in the design of preventive treatment.
Conclusion
We have demonstrated that the expression of serum Hsp90-beta was up-regulated in lung cancer patients and these results indicated that higher expression of Hsp90-beta was potentially involved in the aggression and histology of lung cancer. Overall, our findings in this study indicated that serum Hsp90-beta was a useful biomarker for differentiating patients with lung cancer from those with nonmalignant disorders. The results also implied that the choice of a cutoff value for defining elevated Hsp90-beta serum levels has a clinically relevant impact on the sensitivity and specificity, the chief benefit seems to be an improvement in sensitivity with the use of serum Hsp90-beta. However, larger numbers of lung cancer subjects are required for prospective studies as well as for further studies that are warranted to investigate the potential mechanism of increased in lung cancer.
Acknowledgements
This study was supported by grants from the National Natural Scientific Foundation of China (NO.81172234) and the Fundamental Research Funds for the Central Universities of China. We are grateful for the technical advice provided by Dr. Du Mengang (ChaoYing Biotech Company, Xi’an, Shaanxi, China), Li Jun (The fourth Military Medical University, Xi’an, Shaanxi, China).
Disclosure of conflict of interest
The authors have no financial conflicts of interest to declare.
References
- 1.Tufman A, Huber RM. Biological markers in lung cancer: A clinician’s perspective. Cancer Biomark. 2010;6:123–135. doi: 10.3233/CBM-2009-0124. [DOI] [PubMed] [Google Scholar]
- 2.Kim B, Lee HJ, Choi HY, Shin Y, Nam S, Seo G, Son DS, Jo J, Kim J, Lee J, Kim K, Lee S. Clinical validity of the lung cancer biomarkers identified by bioinformatics analysis of public expression data. Cancer Res. 2007;67:7431–7438. doi: 10.1158/0008-5472.CAN-07-0003. [DOI] [PubMed] [Google Scholar]
- 3.Biaoxue R, Xiling J, Shuanying Y, Wei Z, Xiguang C, Jinsui W, Min Z. Upregulation of Hsp90-beta and annexin A1 correlates with poor survival and lymphatic metastasis in lung cancer patients. J Exp Clin Cancer Res. 2012;31:70. doi: 10.1186/1756-9966-31-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sreedhar AS, Kalmar E, Csermely P, Shen YF. Hsp90 isoforms: functions, expression and clinical importance. FEBS Lett. 2004;562:11–15. doi: 10.1016/s0014-5793(04)00229-7. [DOI] [PubMed] [Google Scholar]
- 5.Yan W, Xiao J, Liu T, Huang W, Yang X, Wu Z, Huang Q, Qian M. The effects of Hsp90 expression alteration on spinal metastases of breast carcinoma. Tumour Biol. 2013;34:1391–1397. doi: 10.1007/s13277-012-0584-z. [DOI] [PubMed] [Google Scholar]
- 6.Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, Postmus PE, Rusch V, Sobin L. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol. 2007;2:706–714. doi: 10.1097/JTO.0b013e31812f3c1a. [DOI] [PubMed] [Google Scholar]
- 7.Fiore E, Campani D, Muller I, Belardi V, Giustarini E, Rossi G, Pinchera A, Giani C. IGF-II mRNA expression in breast cancer: predictive value and relationship to other prognostic factors. Int J Biol Markers. 2010;25:150–156. doi: 10.1177/172460081002500305. [DOI] [PubMed] [Google Scholar]
- 8.Hanley JA. Receiver operating characteristic (ROC) methodology: the state of the art. Crit Rev Diagn Imaging. 1989;29:307–335. [PubMed] [Google Scholar]
- 9.Cedres S, Nunez I, Longo M, Martinez P, Checa E, Torrejon D, Felip E. Serum tumor markers CEA, CYFRA21-1, and CA-125 are associated with worse prognosis in advanced non-small-cell lung cancer (NSCLC) Clin Lung Cancer. 2011;12:172–179. doi: 10.1016/j.cllc.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 10.Yu D, Du K, Liu T, Chen G. Prognostic Value of Tumor Markers, NSE, CA125 and SCC, in Operable NSCLC Patients. Int J Mol Sci. 2013;14:11145–11156. doi: 10.3390/ijms140611145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sung HJ, Cho JY. Biomarkers for the lung cancer diagnosis and their advances in proteomics. BMB Rep. 2008;41:615–625. doi: 10.5483/bmbrep.2008.41.9.615. [DOI] [PubMed] [Google Scholar]
- 12.Myung JK, Afjehi-Sadat L, Felizardo-Cabatic M, Slavc I, Lubec G. Expressional patterns of chaperones in ten human tumor cell lines. Proteome science. 2004;2:8. doi: 10.1186/1477-5956-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yano M, Naito Z, Yokoyama M, Shiraki Y, Ishiwata T, Inokuchi M, Asano G. Expression of hsp90 and cyclin D1 in human breast cancer. Cancer letters. 1999;137:45–51. doi: 10.1016/s0304-3835(98)00338-3. [DOI] [PubMed] [Google Scholar]
- 14.McDowell CL, Bryan Sutton R, Obermann WMJ. Expression of Hsp90 chaperome proteins in human tumor tissue. International journal of biological macromolecules. 2009;45:310–314. doi: 10.1016/j.ijbiomac.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Uozaki H, Ishida T, Kakiuchi C, Horiuchi H, Gotoh T, Iijima T, Imamura T, Machinami R. Expression of heat shock proteins in osteosarcoma and its relationship to prognosis. Pathol Res Pract. 2000;196:665–673. doi: 10.1016/S0344-0338(00)80118-1. [DOI] [PubMed] [Google Scholar]
- 16.Jahns F, Wilhelm A, Greulich KO, Mothes H, Radeva M, Wölfert A, Glei M. Impact of butyrate on PKM2 and HSP90β expression in human colon tissues of different transformation stages: a comparison of gene and protein data. Genes Nutr. 2011;7:235–46. doi: 10.1007/s12263-011-0254-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schnitt SJ. Breast cancer in the 21st century: neu opportunities and neu challenges. Mod Pathol. 2001;14:213–218. doi: 10.1038/modpathol.3880288. [DOI] [PubMed] [Google Scholar]


