Abstract
AIM: To determine the incidence of appendiceal Crohn’s disease (CD) and to summarize the characteristic histologic features of appendiceal CD.
METHODS: We reviewed the pathology files of 2179 appendectomy specimens from January 2007 to May 2013. The computer-assisted retrieval search facility was utilized to collect specimens. We selected those cases that were diagnosed as CD or chronic granulomatous inflammation and defined the final diagnosis according to the histologic findings of CD, including transmural lymphocytic inflammation, non-caseating epithelioid granulomas, thickening of the appendiceal wall secondary to hypertrophy of muscularis mucosa, mucosal ulceration with crypt abscesses, mucosal fissures, and fistula formation.
RESULTS: We found 12 cases (7 male and 5 female patients, with an average age of 29.8 years) of appendiceal CD. The incidence of appendiceal CD was 0.55%. The chief complaints were right lower quadrant pain, abdominal pain, lower abdominal pain, and diarrhea. The duration of symptom varied from 2 d to 5 mo. The histologic review revealed appendiceal wall thickening in 11 cases (92%), transmural inflammation in all cases (100%), lymphoid aggregates in all cases (100%), epithelioid granulomas in all cases (100%), mucosal ulceration in 11 cases (92%), crypt abscesses in 5 cases (42%), perforation in 2 cases (17%), muscular hypertrophy in 1 case (8%), neural hyperplasia in 5 cases (42%), and perpendicular serosal fibrosis in 8 cases (67%).
CONCLUSION: A typical and protracted clinical course, unusual gross features of the appendix and the characteristic histologic features are a clue in the diagnosis of appendiceal CD.
Keywords: Appendix, Appendectomy, Acute appendicitis, Crohn’s disease, Prognosis
Core tip: Appendiceal Crohn’s disease (CD) is relatively rare and is indistinguishable from acute appendicitis. Appendiceal CD shows a favorable clinical outcome with a low recurrence rate. The differential diagnosis includes intestinal tuberculosis, foreign body reaction, diverticulitis of the appendix, sarcoidosis, actinomycosis, and Yersinia infection. Atypical and protracted clinical course, unusual gross features of the appendix and the characteristic histologic features are a clue in the diagnosis of appendiceal CD.
INTRODUCTION
Crohn’s disease (CD) is a chronic inflammatory bowel disorder characterized by a transmural inflammatory reaction and non-caseating small granulomas and may involve all parts of the gastrointestinal (GI) tract from the mouth to the anus[1-7]. The most common sites of involvement are the ileum and colon[8]. Appendiceal CD is a rare disease but has been well summarized in the various reports[9-14]. The incidence of appendicitis with granulomatous reaction varies from 0.1% to 2.0%[15]. Since Meyerding et al[16] had reported an interesting case of appendiceal CD without demonstrable involvement of the adjacent GI tract in 1953, many additional cases of appendiceal CD have been demonstrated in the literature to date .
The purpose of this retrospective review study was to determine the exact incidence of appendiceal CD in patients who underwent appendectomy and to summarize the common characteristic histologic findings along with a review of the literature.
MATERIALS AND METHODS
Ethics
The materials used in our study are human appendix tissue samples, which are products of surgical procedures. Our study contains no private information relating to the patients, and so ensures their anonymity. Therefore, our study has no problems in causing any ethical issue or encroachment of human rights.
Patient tissue
A retrospective review of 2179 appendectomy specimens from January 2007 to May 2013 was conducted. All patients underwent appendectomy at the Hanyang University Hospital (Seoul, South Korea). The computer-assisted retrieval search facility was utilized to collect appendectomy specimens. Appendices resected for acute appendicitis and those removed as a part of right hemicolectomy and gynecology procedures were collected and reviewed. We selected those cases that were diagnosed as CD or chronic granulomatous inflammation and defined the final diagnosis according to the common histologic findings of CD, including transmural lymphocytic inflammation, non-caseating small epithelioid granulomas, thickening of the appendiceal wall secondary to hypertrophy of muscularis mucosa, mucosal ulceration with crypt abscesses, mucosal fissures, and fistula formation. No evidence of parasitic, fungal and mycobacterial disease, foreign body, or systemic sarcoidosis was found in any patient. The clinical information including age, gender, clinical data, and data about the surgical procedure for each case as well as follow-up data including colonoscopic evaluation was collected. The special staining technique such as Ziehl-Neelsen staining and special molecular technique such as tuberculosis polymerase chain reaction (Tb-PCR) were performed to rule out Mycobacterium tuberculosis.
RESULTS
Out of these 2179 appendectomy specimens, 12 cases (0.55%) were classified as appendiceal CD. The clinicopathologic characteristics of the appendiceal CD patients are summarized in Tables 1 and 2. Out of these 12 patients, there were 7 male and 5 female patients. The age of patients ranged from 11 to 51 years (average age of 29.8 years). The chief complaints of patients were right lower quadrant (RLQ) pain, abdominal pain, lower abdominal pain, and diarrhea. The duration of symptom with which patients presented varied from 2 d to 5 mo. There was no systemic clinical manifestation such as arthralgia, uveitis, or arthritis. No history of tuberculosis of any organ was found in these patients. There was also no clinical evidence of systemic sarcoidosis. The initial clinical impression was acute appendicitis in all of these 12 patients along with perforation in 2 among these 12 patients. All patients underwent appendectomy. The final pathologic report was CD in all of these 12 cases. All cases showed a negative result for Mycobacterium tuberculosis in Ziehl-Neelsen staining and Tb-PCR. The histologic review of these 12 cases revealed appendiceal wall thickening in 11 cases (92%), transmural inflammation in all cases (100%), lymphoid aggregates in all cases (100%), epithelioid granulomas in all cases (100%), mucosal ulceration in 11 cases (92%), crypt abscesses in 5 cases (42%), perforation with abscess formation in 2 cases (17%), muscular hypertrophy in 1 case (8%), neural hyperplasia in 5 cases (42%), and perpendicular serosal fibrosis in 8 cases (67%). The representative microphotographs are shown in Figure 1. There is no evidence of disease recurrence in these 12 patients to date.
Table 1.
Summary of the patients with appendiceal Crohn’s disease
| Case No. | Sex | Age (yr) | c/c | SD | Clinical impressions | AFB | Tb-PCR |
| 1 | F | 30 | RLQ pain | None | Acute appendicitis | Negative | Negative |
| 2 | M | 38 | RLQ pain | 14 d | Acute appendicitis | Negative | Negative |
| 3 | M | 26 | RLQ pain | None | Acute appendicitis | Negative | Negative |
| 4 | M | 28 | RLQ pain | 7 d | Acute appendicitis | Negative | Negative |
| 5 | F | 25 | RLQ pain | 14 d | Acute appendicitis | Negative | Negative |
| 6 | F | 29 | RLQ pain | 7 d | Acute appendicitis | Negative | Negative |
| 7 | M | 51 | RLQ pain | 5 mo | Acute appendicitis, perforation | Negative | Negative |
| 8 | F | 49 | RLQ pain | 8 d | Acute appendicitis | Negative | Negative |
| 9 | M | 30 | Abdominal pain | 10 d | Acute appendicitis, perforation | Negative | Negative |
| 10 | M | 23 | Lower abdominal pain | 2 d | Acute appendicitis | Negative | Negative |
| 11 | M | 18 | Lower abdominal pain, diarrhea | 3 d | Acute appendicitis | Negative | Negative |
| 12 | F | 11 | RLQ pain | 7 d | Acute appendicitis | Negative | Negative |
F: Female; M: Male; c/c: Chief complaint; RLQ: Right lower quadrant; SD: Symptom duration; AFB: Acid-fast bacillus; Tb-PCR: Tuberculosis polymerase chain reaction.
Table 2.
Summary of histologic features of appendiceal Crohn’s disease
| Histologic features | Number of cases | % |
| Wall thickening | 11/12 | 92 |
| Transmural inflammation | 12/12 | 100 |
| Lymphoid aggregates | 12/12 | 100 |
| Epithelioid granuolmas | 12/12 | 100 |
| Mucosal ulceration | 11/12 | 92 |
| Crypt abscess | 5/12 | 42 |
| Perforation | 2/12 | 17 |
| Muscular hypertrophy | 1/12 | 8 |
| Neural hyperplasia | 5/12 | 42 |
| Perpendicular serosal fibrosis | 8/12 | 67 |
Figure 1.
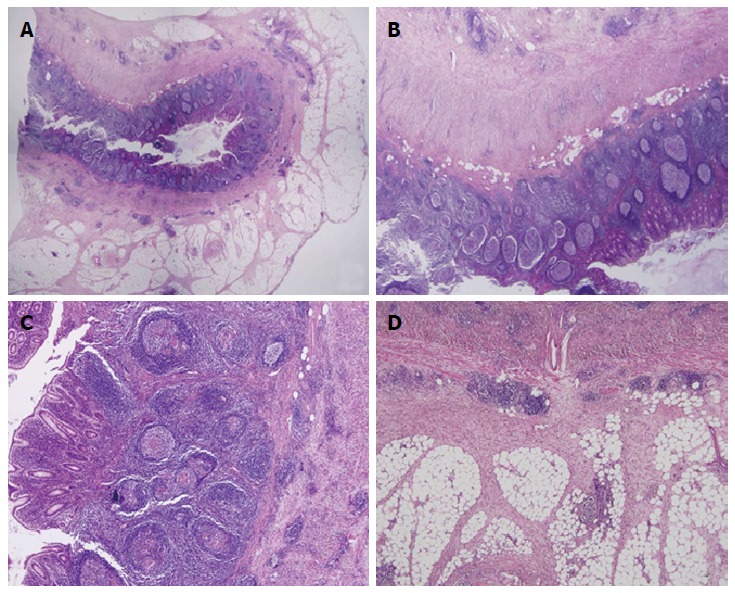
Appendiceal Crohn’s disease. A: The appendix with Crohn’s disease shows transmural inflammation with markedly thickened wall; B: There is a prominent lymphoid hyperplasia in the mucosa and serosa; C: The mucosa shows many small non-caseating granulomas; D: The serosa shows creeping fat with perpendicular thick fibrous bands.
DISCUSSION
Crohn first described that CD stops at the ileocecal valve with sparing of the colon and appendix. However, this theory was disproved as patients with CD often have involvement of the colon and appendix[5]. The first isolated appendiceal CD was reported by Meyerding et al[16] in 1953. Since Meyerding et al[16] had reported a case of CD arising in the appendix, many case reports and some collective reviews have been reported in the literature. The incidence of appendiceal CD is variable[17-21]. Prieto-Nieto et al[4] described that approximately 0.2% of patients (10 out of 4468 appendectomies performed during 20 years) had appendiceal CD. In our review, 12 cases (0.55%) out of 2179 appendectomy specimens were revealed as appendiceal CD.
Appendiceal CD is usually found among young patients, however, it can occur at any age[3,12]. Yang et al[14] described the age with onset of disease in 14 patients with appendiceal CD, ranged from 10 to 45 years (average age of 21.1 years). Prieto-Nieto et al[4] reported the disease onset-age in 10 patients with appendiceal CD, ranged from 10 to 33 years (average age of 29 years). The difference in incidence of disease in males and females has been reported, with male predominance[4,14]. In our study, the age ranged from 11 to 51 years, with an average age of 29.8 years. Among 12 patients, 7 were male, reflecting more male patients with the disease described previously.
The clinical presentation of appendiceal CD is variable. The most common presenting symptom is acute lower abdominal pain especially in the RLQ, which is very similar to the lower abdominal pain presented in patients with acute appendicitis[4,13,22]. Approximately 25% of appendiceal CD patients show chronic abdominal pain in the right lower abdomen[13]. The symptoms may be more protracted or recurrent than in the usual case of acute suppurative appendicitis. Appendiceal CD should be suspected when the patients show atypical or protracted unusual clinical course[2,13]. In our study, most patients presented with the pain in the RLQ. The initial clinical impression was acute appendicitis in all 12 patients. Most patients had symptoms for two or more days, and 8 patients (67%) presented with these symptoms for over a week.
Appendiceal CD usually shows an enlarged appendix with marked thickening of the appendiceal wall and fibrous adhesion to the periappendiceal soft tissue[2,22,23]. Microscopically, the histologic features are characterized by transmural chronic inflammation with marked fibrous thickening of the wall, lymphoid aggregates, small non-caseating granulomas, ulcerative mucosal change, crypt abscesses, muscular hypertrophy, and neural hyperplasia[13,24-26]. In our study, the features were similar to the previously described histologic characteristics. Interestingly, we found that appendiceal CD had the characteristic perpendicular serosal fibrous band formation in 8 out of 12 cases.
The differential diagnosis includes intestinal tuberculosis, foreign body reaction, diverticulitis of the appendix, sarcoidosis, actinomycosis, and Yersinia infection[10,13,22,24,25]. Appendiceal tuberculosis results in the formation of epithelioid granulomas, however, the granulomas in tuberculosis are larger with a central caseous necrosis and less discrete than those in Crohn’s disease[10,27-29]. If a foreign body is present, histologic examination should reveal the offending material and diverticular disease may be excluded via careful examination[14,27]. Intestinal sarcoidosis is extremely rare and does not occur as an isolated finding[13,30]. Actinomycosis also results in a vague granulomatous tissue reaction, however, actinomycosis shows neutrophilic abscess formation with floating bacterial colonies (sulphur granules)[31-34]. Yersinia infection results in necrotizing granulomatous reaction in the appendiceal mucosa or submucosa and shows microabscess formation[35,36].
The treatment of choice for appendiceal CD is appendectomy[30]. Appendiceal CD shows lower recurrence rate compared with CD arising in other parts of the intestine[25]. The prognosis of appendiceal CD seems to be much better than that of CD arising in the small or large bowel[14].
In conclusion, we described the incidence of appendiceal CD in patients who underwent appendectomy and summarized the common characteristic histologic findings along with a review of the literature. Atypical and protracted clinical course, unusual gross features of the appendix and the characteristic features are a clue in the diagnosis of appendiceal CD.
COMMENTS
Background
Appendiceal Crohn’s disease (CD) is a rare disease. Since Meyerding et al had reported an interesting case of appendiceal CD without demonstrable involvement of the adjacent gastrointestinal tract in 1953, many additional cases of appendiceal CD have been demonstrated in the literature to date.
Research frontiers
The incidence of appendicitis with granulomatous reaction varies from 0.1% to 2.0%. The incidence of appendiceal CD is variable. The purpose of this study was to determine the exact incidence of appendiceal CD in patients who underwent appendectomy and to summarize the common characteristic histologic findings along with a review of the literature.
Innovations and breakthroughs
The histologic features are characterized by transmural chronic inflammation with marked fibrous thickening of the wall, lymphoid aggregates, small non-caseating granulomas, ulcerative mucosal change, crypt abscesses, muscular hypertrophy, and neural hyperplasia. In this study, the features were similar to the previously described histologic characteristics. However, the authors found that appendiceal CD had the characteristic perpendicular serosal fibrous band formation in 8 out of 12 cases.
Applications
With the characteristic clinical presentation and the typical pathologic findings, the clinicians and pathologists can consider the possibility of appendiceal CD. Atypical and protracted clinical course, unusual gross features of the appendix and the characteristic histologic features are a clue in the diagnosis of appendiceal CD.
Terminology
CD is a chronic inflammatory bowel disorder characterized by a transmural inflammatory reaction and non-caseating small granulomas and may involve all parts of the gastrointestinal tract from the mouth to the anus.
Peer review
The authors described appendiceal CD clinically presenting as acute appendicitis. This is an interesting review and CD in appendix is a rare condition. Whenever it is encountered, the surgeon must know what to do and be aware of its prognosis. This paper will lead surgeons to this condition.
Footnotes
P- Reviewer: Cetinkunar S, Matsumoto S, Sartelli M S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
References
- 1.Stangl PC, Herbst F, Birner P, Oberhuber G. Crohn’s disease of the appendix. Virchows Arch. 2002;440:397–403. doi: 10.1007/s004280100532. [DOI] [PubMed] [Google Scholar]
- 2.Vanek VW, Spirtos G, Awad M, Badjatia N, Bernat D. Isolated Crohn’s disease of the appendix. Two case reports and a review of the literature. Arch Surg. 1988;123:85–87. doi: 10.1001/archsurg.1988.01400250095017. [DOI] [PubMed] [Google Scholar]
- 3.Haddad M, Azim F, Koren A, Stelman E, Mor C, Zelikovski A. Crohn’s disease of the appendix. Eur J Surg. 1993;159:191–192. [PubMed] [Google Scholar]
- 4.Prieto-Nieto I, Perez-Robledo JP, Hardisson D, Rodriguez-Montes JA, Larrauri-Martinez J, Garcia-Sancho-Martin L. Crohn’s disease limited to the appendix. Am J Surg. 2001;182:531–533. doi: 10.1016/s0002-9610(01)00811-x. [DOI] [PubMed] [Google Scholar]
- 5.Crohn BB, Ginzburg L, Oppenheimer GD. Regional ileitis: a pathologic and clinical entity. 1932. Mt Sinai J Med. 2000;67:263–268. [PubMed] [Google Scholar]
- 6.Kahn E, Markowitz J, Daum F. The appendix in inflammatory bowel disease in children. Mod Pathol. 1992;5:380–383. [PubMed] [Google Scholar]
- 7.Kovalcik P, Simstein L, Weiss M, Mullen J. The dilemma of Crohn’s disease: Crohn’s disease and appendectomy. Dis Colon Rectum. 1977;20:377–380. doi: 10.1007/BF02587363. [DOI] [PubMed] [Google Scholar]
- 8.Nivatvongs S. Crohn’s disease of the appendix: report of a case and review of the literature. Dis Colon Rectum. 1978;21:361–363. doi: 10.1007/BF02586668. [DOI] [PubMed] [Google Scholar]
- 9.Zager JS, Gusani NJ, Derubertis BG, Shaw JP, Kaufman JP, DeNoto G. Laparoscopic appendectomy for Crohn’s disease of the appendix presenting as acute appendicitis. J Laparoendosc Adv Surg Tech A. 2001;11:255–258. doi: 10.1089/109264201750539808. [DOI] [PubMed] [Google Scholar]
- 10.Lindhagen T, Ekelund G, Leandoer L, Hildell J, Lindström C, Wenckert A. Crohn’s disease confined to the appendix. Dis Colon Rectum. 1982;25:805–808. doi: 10.1007/BF02553319. [DOI] [PubMed] [Google Scholar]
- 11.Agha FP, Ghahremani GG, Panella JS, Kaufman MW. Appendicitis as the initial manifestation of Crohn’s disease: radiologic features and prognosis. AJR Am J Roentgenol. 1987;149:515–518. doi: 10.2214/ajr.149.3.515. [DOI] [PubMed] [Google Scholar]
- 12.Ruiz V, Unger SW, Morgan J, Wallack MK. Crohn’s disease of the appendix. Surgery. 1990;107:113–117. [PubMed] [Google Scholar]
- 13.McCue J, Coppen MJ, Rasbridge SA, Lock MR. Crohn’s disease of the appendix. Ann R Coll Surg Engl. 1988;70:300–303. [PMC free article] [PubMed] [Google Scholar]
- 14.Yang SS, Gibson P, McCaughey RS, Arcari FA, Bernstein J. Primary Crohn’s disease of the appendix: report of 14 cases and review of the literature. Ann Surg. 1979;189:334–339. doi: 10.1097/00000658-197903000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.AbdullGaffar B. Granulomatous diseases and granulomas of the appendix. Int J Surg Pathol. 2010;18:14–20. doi: 10.1177/1066896909349246. [DOI] [PubMed] [Google Scholar]
- 16.Meyerding EV, Bertram HF. Nonspecific granulomatous inflammation (Crohn’s disease) of the appendix; a case report. Surgery. 1953;34:891–894. [PubMed] [Google Scholar]
- 17.Larsen E, Axelsson C, Johansen A. The pathology of the appendix in morbus Crohn and ulcerative colitis. Acta Pathol Microbiol Scand Suppl. 1970;212:Suppl 212: 161+. [PubMed] [Google Scholar]
- 18.Lennard-Jones JE, Morson BC. Changing concepts in Crohn’s disease. Dis Mon. 1969;Aug:1–37. [PubMed] [Google Scholar]
- 19.Lockhart-mummery HE, Morson BC. Crohn’s disease of the large intestine. Gut. 1964;5:493–509. doi: 10.1136/gut.5.6.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rappaport H, Burgoyne FH, Smetana HF. The pathology of regional enteritis. Mil Surg. 1951;109:463–502. [PubMed] [Google Scholar]
- 21.Warren S, Sommers SC. Cicatrizing enteritis as a pathologic entity; analysis of 120 cases. Am J Pathol. 1948;24:475–501. [PMC free article] [PubMed] [Google Scholar]
- 22.Cerdán FJ, Balsa T, Torres-Melero J, García MC, Remezal M, Balibrea JL. Appendiceal Crohn’s disease. Rev Esp Enferm Dig. 1995;87:331–334. [PubMed] [Google Scholar]
- 23.Wettergren A, Munkholm P, Larsen LG, Meinecke B, Langholz E, Jess P, Binder V. Granulomas of the appendix: is it Crohn’s disease? Scand J Gastroenterol. 1991;26:961–964. doi: 10.3109/00365529108996249. [DOI] [PubMed] [Google Scholar]
- 24.Kosakowski C, Thompson JE, Feinberg MJ. Coexistence of primary Crohn’s disease and carcinoid tumor isolated to the appendix. A case report. Acta Chir Scand. 1986;152:233–236. [PubMed] [Google Scholar]
- 25.Ariel I, Vinograd I, Hershlag A, Olsha O, Argov S, Klausner JM, Rabau MY, Freund U, Rosenmann E. Crohn’s disease isolated to the appendix: truths and fallacies. Hum Pathol. 1986;17:1116–1121. doi: 10.1016/s0046-8177(86)80416-6. [DOI] [PubMed] [Google Scholar]
- 26.Early CK, Kouri S. Granulomatous disease of the appendix manifesting as a cecal mass: report of a case. Dis Colon Rectum. 1980;23:421–422. doi: 10.1007/BF02586793. [DOI] [PubMed] [Google Scholar]
- 27.Allen DC, Biggart JD. Granulomatous disease in the vermiform appendix. J Clin Pathol. 1983;36:632–638. doi: 10.1136/jcp.36.6.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang TK, Tolnai G, Campbell JS, Sirois J, Liepa E. Crohn’s disease of the appendix. Can Med Assoc J. 1972;106:233–236. [PMC free article] [PubMed] [Google Scholar]
- 29.Weiss Y, Durst AL. Crohn’s disease of the appendix. Presentation of a case with review of the literature. Am J Gastroenterol. 1975;63:333–339. [PubMed] [Google Scholar]
- 30.Bak M, Andersen JC. Crohn’s disease limited to the vermiform appendix. Acta Chir Scand. 1987;153:441–446. [PubMed] [Google Scholar]
- 31.Liu V, Val S, Kang K, Velcek F. Case report: actinomycosis of the appendix--an unusual cause of acute appendicitis in children. J Pediatr Surg. 2010;45:2050–2052. doi: 10.1016/j.jpedsurg.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 32.Lee SY, Kwon HJ, Cho JH, Oh JY, Nam KJ, Lee JH, Yoon SK, Kang MJ, Jeong JS. Actinomycosis of the appendix mimicking appendiceal tumor: a case report. World J Gastroenterol. 2010;16:395–397. doi: 10.3748/wjg.v16.i3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Altanis E. Actinomycosis of the appendix and pelvis. J Reprod Med. 2009;54:411–412; author reply 412. [PubMed] [Google Scholar]
- 34.Yiğiter M, Kiyici H, Arda IS, Hiçsönmez A. Actinomycosis: a differential diagnosis for appendicitis. A case report and review of the literature. J Pediatr Surg. 2007;42:E23–E26. doi: 10.1016/j.jpedsurg.2007.03.057. [DOI] [PubMed] [Google Scholar]
- 35.Kojima M, Morita Y, Shimizu K, Yoshida T, Yamada I, Togo T, Johshita T. Immunohistological findings of suppurative granulomas of Yersinia enterocolitica appendicitis: a report of two cases. Pathol Res Pract. 2007;203:115–119. doi: 10.1016/j.prp.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 36.Bronner MP. Granulomatous appendicitis and the appendix in idiopathic inflammatory bowel disease. Semin Diagn Pathol. 2004;21:98–107. doi: 10.1053/j.semdp.2004.12.001. [DOI] [PubMed] [Google Scholar]


