Abstract
The prevalence of obesity in adolescents and children has risen to alarming levels globally, and this has serious public health consequences. Sedentary lifestyle and consumption of calorie-dense foods of low nutritional value are speculated to be two of the most important etiological factors responsible for escalating rate of childhood overweight in developing nations. To tackle the childhood obesity epidemic we require comprehensive multidisciplinary evidence-based interventions. Some suggested strategies for childhood obesity prevention and management include increasing physical activity, reducing sedentary time including television viewing, personalized nutrition plans for very obese kids, co-curriculum health education which should be implemented in schools and counseling for children and their parents. In developing countries like India we will need practical and cost-effective community-based strategies with appropriate policy changes in order to curb the escalating epidemic of childhood obesity.
Keywords: Childhood, consequences and prevention strategies, determinants, obesity, overweight
INTRODUCTION
Obesity is the main determinant of preventable burden of diseases.[1] It results from excess consumption of calories/energy compared to expenditure thus impacting health. Globally, children in particular are gaining weight, which tracks into adulthood thus increasing the risk of adult diseases such as type 2 diabetes, cardiovascular disease (CVD), hypertension and polycystic ovarian syndrome (PCOS) later in life.[2,3]
Developing countries more often contain children with diseases at both ends of the spectrum viz. under and over nutrition.[4] Despite various public health and advocacy programs under-nutrition still persists in India however in the recent years over-nutrition has also emerged as an important public health problem. Also maybe, with increasing awareness the obese children are getting identified earlier. This underscores the importance of screening children for obesity regularly in schools and the role of pediatricians, teachers and parents in identifying these overweight children to take appropriate timely action.[5]
The aim of this narrative review is to present an overview of the various determinants/risk factors and consequences of childhood obesity and discuss prevention/intervention strategies from an Asian Indian context.
DETERMINANTS OF CHILDOOD OBESITY-THE ASIAN INDIAN CONTEXT
In the young, psychological and behavioral factors manifesting as unhealthy dietary habits and sedentary behavior are probably the most important determinants of obesity. The potential role of genetic programming in the rising prevalence of childhood obesity epidemic is also being increasingly accepted.
Dietary habits
Childhood obesity is largely influenced by the increased intake of energy-dense foods that are high in fat and sugars but low in proteins, vitamins, minerals and other healthy micronutrients.[6] Aggarwal et al. showed that among obese adolescents in Punjab a significant percentage (82.3%) were non-vegetarians.[7] They also found that obesity/overweight was found to be significantly higher in those adolescents who regularly ate out and among those who replaced snacks for meals. The variety of convenience foods available in the market and the role of media in sensitizing the parents and children to these changes could have also undoubtedly contributed to childhood obesity.[8] One of the factors that could significantly affect children's energy intake is the increasing availability of energy-dense, high-calorie foods/snacks and drinks in school canteens. Working mothers or single-parent families may also increase the demand for take away foods or increase the frequency of eating out and cause reliance on pre-prepared foods. The higher per capita income also increases the family's economic capacity and thus the affordability to buy high calorie foods from restaurants. Goyal et al.[9] reporting on adolescents from Gujarat did not find a difference in the prevalence of overweight and obesity among vegetarians and non-vegetarians but did find a correlation with frequency of eating out as well as with junk food consumption.
A report from America suggested a strong link between sugar-sweetened beverages and prevalence of childhood obesity.[10] Sugar-sweetened beverages are high in calories but nutrient-poor and this is often coupled with consumption of salty and high fat food choices.[11] With changing dietary trends due to westernization and globalization there is more frequent consumption of these sweetened beverages even at young ages. This link needs to be further investigated among Indian children and adolescents.
Physical inactivity/sedentary activity
Physical inactivity trends have been increasing, not just in adults but also among children and adolescents mainly due to the switch to sedentary activities such as watching television and playing computer games.[12] Studies on prevention of childhood obesity focus primarily on this important issue as these sedentary activities are seen to have a direct correlation to increased body weight.[8,13,14] The Central Board of Secondary Education (CBSE) 2007 fact sheet[15] reported that only 30% of adolescents played regularly for at least 1 hour a day. Aggarwal et al.[7] reported that more than half of the adolescents’ spent 1-4 hours per day viewing TV or sitting at the computer. Kotian and co-workers[16] found the prevalence of overweight was higher among adolescents of high socioeconomic strata those who had physical activity of less than 1 hour per day, watched television for 4 hours/day, and ate chocolates daily. Goyal et al.[9] also reported that physical inactivity influenced the children's body mass index (BMI) with overweight and obese children being less likely to participate in sports and other outdoor activities. In addition, changing modes of transportation, that is, people prefer driving to cycling or walking even for short distances, and increasing mechanization and use of labor-saving devices at home are also contributing factors.[6] Finally, the latest influence on childhood obesity has been that of mass media with deliberate, and sometimes unethical, marketing strategies targeted at children. We need to be able to document how this marketing affects our children and what safeguards need to be introduced and at what age.[17]
Built environment (Home and school)
The dietary and physical activity behaviors of children and adolescents are influenced by many sections of society, including the family, school, peers, child care setting, medical care provider, faith-based institutions, government agencies, the media, the food and beverage market and the entertainment industry.[18] All these together form the built environment. Changes in the built environment over the past three decades have upset the energy balance equation. Urbanization and industrialization have immensely contributed to increasing children's energy intake and decreasing their energy expenditure thus promoting obesity. The challenge thus lies in formulating policies that address how best to change this built environment in a positive manner in order to maintain children's energy balance and prevent excessive weight gain.[8,13,14]
The reluctance of policy makers to regulate the food environment is a direct consequence of the belief that people's food choices reflect their true desires. The reality is that food choices are often automatic and in children they are driven by the effects of mass media, family habits and more by peer pressure. Cohen and Babey in a recent editorial show a clear example of this influence by quoting the example of placement of candy/chocolates at the cash register at any supermarket.[19] This is widely acknowledged to be a promotional strategy called “impulse marketing.” Impulse marketing encourages “spur-of-the-moment,” emotion-related purchases that are triggered by seeing a product or a related message. Impulse marketing works by placing goods at prominent locations in the supermarket (Ex: end-of-aisle or at the cash counter). These are seen to account for about 30% of all supermarket sales. The common belief is that those who respond to impulse marketing simply lack self-control and should learn how to resist such marketing strategies. However, anyone who has visited a supermarket will know that most last minute purchasing decisions are made very quickly and automatically without substantial cognitive input. Unfortunately, these decisions are generally more with regards to foods high in fat and sugar rather than choices of healthy foods such as fruits and vegetables or whole grains and pulses that require more thought. Policy makers need to understand the effect of these marketing strategies employed to increase sales, in relation to public health and limit the types of foods that can be displayed in prominent end-of-aisle locations and move foods which could promote chronic diseases, to locations that require some effort to find.
Socio-economic status
In developed countries, children from the low socio-economic strata are more obese than their affluent counterparts, whereas the opposite is observed in developing countries where children from the upper socio-economic strata are more likely to be obese than children from the lower socio-economic strata.[20] Marwaha et al.[21] classified children as normal, overweight and obese as per the IOTF guidelines and showed that among the upper socio-economic status (USES) children, prevalence of overweight and obesity was 17% and 5.6% in boys and 19% and 5.7% in girls, respectively, whereas in the lower socio-economic status (LSES) it was 2.7% and 0.4% in boys and 2.1% and 0.5% in girls, respectively. Kaneria et al.[22] made a comparative assessment of overweight and obesity in two different socioeconomic groups of school-age children from Udaipur city (Rajasthan), on the basis of 85th and 95th percentile for BMI. Obesity in the affluent group was 3.7%, but no case of obesity (0%) was observed in the non-affluent group. Unnithan and Syamakumari[23] have shown that obesity and overweight were more common in boys, while underweight and severe underweight were seen in girls. Not unexpectedly, they also showed that the prevalence of overweight and obesity were higher among urban children, while the percentage of underweight and severe underweight was higher among rural children. However, recent studies have shown that in the government schools, though the prevalence of underweight is higher, overweight is also present in 3-5% of children.[9,24] This shows that slowly, but steadily, the epidemic of childhood obesity is now spreading to the lower socio-economic groups as well.
Genetic, antenatal and postnatal factors
The Avon Longitudinal Study showed that the odds of children aged 7 becoming obese if the father, mother or both had obesity were 2.93, 4.66 and 11.75, respectively, showing clearly the dominant influence of parental obesity.[25] Parental obesity is considered to be a stronger predictor of obesity in adulthood than the child's weight status at less than 3 years of age.[26] Genetic factors influence the susceptibility of a given child to an obesity-conducive environment. Few cases of childhood obesity have been reported due to leptin deficiency or medical causes such as hypothyroidism and growth hormone deficiency or due to the side effects of drugs such as steroids.[13] However, personal lifestyle choices and the environment influence childhood and adult obesity much more than the above-mentioned conditions. The common antenatal factors and postnatal factors thought to play a role in childhood and adulthood obesity are gestational diabetes mellitus, maternal weight gain during pregnancy, intrauterine growth retardation (IUGR), babies small or large for gestational age, early bottle feeding, infant overnutrition and early adiposity rebound at 5-6 years of age. However, a study from Delhi reported that only 6% of overweight children had low birth weight and found a positive correlation between children with a birth weight of ≥ 3 kg and obesity in their adolescent years.[27] Systematic reviews have concluded that breastfeeding seems to have a small but consistent, protective effect against obesity in children.[14] Von Kries et al.[28] showed that the prevalence of obesity in children who were never breastfed was 4.5%, compared to 2.8% in breastfed children. Early menarche has been shown to be associated with a two-fold increase in rate of obesity.[29]
Although genes are familial, so are environmental patterns, hence it may be difficult to tease out the difference between the two. The “Fetal Origins Hypothesis,” commonly known as the “Barker Hypothesis,” suggests that antenatal stress or placental insufficiency can “program” metabolic alterations in beta cell function. This increased insulin sensitivity then persists into adult life and promotes the development of metabolic abnormalities including obesity.[30,31] Intrauterine growth patterns play a significant role in the evolution of obesity by modifying fat and lean body mass, neuroendocrine appetite control mechanisms, and pancreatic functional capacities. Longitudinal studies have identified a strong relationship between birth weight and BMI attained in later life.[25] Low birth weight babies show a dramatic transition to central adiposity and insulin resistance very early in life.[32] The combination of lower birth weight and higher BMI during childhood is dangerous as it is associated with an increased risk of CVD in later life.[26,31] Catch up growth and early adiposity rebound significantly increases the odds of children becoming obese.[33] The age of adiposity rebound, the point at which body fatness begins to increase usually occurring between 5 and 6 years of age is also an important predictor of adult obesity. Children with an early adiposity rebound have a fivefold greater chance of becoming obese as adults, compared to those with late adiposity rebound.[34]
CONSEQUENCES OF CHILDHOOD OBESITY
There are several well-documented consequences of childhood obesity [Figure 1] and prominent among them are listed below:
Figure 1.
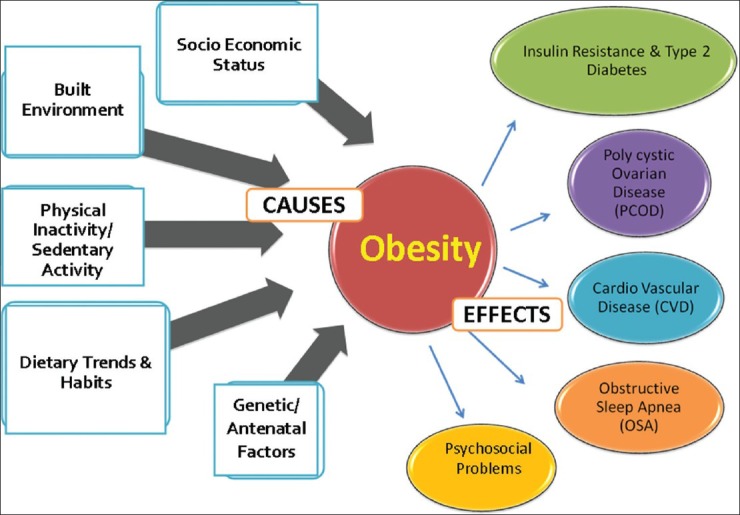
Childhood obesity-complex condition with multiple causes and consequences
Insulin resistance and type 2 diabetes
Obesity and body fat patterning are important determinants of insulin resistance in children. In the natural history of diabetes, obesity and insulin resistance precede abnormal glucose. Studies have shown that the effect of obesity on insulin action is likely to be mediated by a progressive decline in muscle glycogen synthase activity and glycogenesis.[35,36] Obesity-induced insulin resistance plays an important role in increasing lipid concentrations in insulin-responsive tissues.[37] The mechanism by which free fatty acids (FFA) can cause insulin resistance include generation of lipid metabolites (diacylglycerol), proinflammatory cytokines such as TNF-α, IL1β, IL6, MCP1 and cellular stress including oxidative and endoplasmic reticulum stress.[38] Such individuals are thus prone to develop diabetes.[39]
The Bogalusa Heart Study has shown that hyperinsulinemia, once established in childhood, tracks through to adulthood, with adverse consequences.[40] About one-third of overweight or obese urban Asian Indian children have insulin resistance.[41] Yajnik et al.[42] have shown that Asian Indian neonates and children have higher level of hyperinsulinemia and related metabolic derangements as compared to white Caucasian neonates. Vikram et al.[43] have reported an overall prevalence of fasting hyperinsulinemia in 29% and 64% of normal weight and overweight adolescents, respectively. In postpubertal Asian Indian children, the overall prevalence of fasting hyperinsulinemia was high (27%).[42] Obesity and insulin resistance lead to the development of type 2 diabetes.[44,45] Indians are susceptible to diabetes at younger ages and at relatively lower BMIs compared to the white Caucasians.[46] Data from the New Delhi Birth Cohort[47] has shown that the pattern of weight gain, particularly rapid weight gain after the age of 2 years, has been shown to be significantly associated with a higher prevalence of the metabolic derangements in young Asian Indians.
There is growing evidence that the prevalence of glucose intolerance in childhood and adolescents is increasing globally.[48,49] In a recent population-based study conducted in South India, the overall prevalence of glucose intolerance (prediabetes and/or diabetes) was 3.7%, and higher in girls compared to boys (4.2% vs. 3.2%) which increased to 12.7% in girls with abdominal obesity.[50]
Polycystic ovary syndrome (PCOS)
Obese adolescent girls are more likely to suffer from PCOS-a syndrome of variable combinations of menstrual irregularity, hirsutism or acne, with obesity and insulin resistance.[51] Obesity may play a pathogenic role in the development of PCOS in susceptible individuals. Early adiposity promotes hyperandrogenemia, and conversely androgen excess may lead to central adiposity and PCOS-related metabolic aberrations.[52] Other factors such as increased estrogen production rate, increased activity of the opioid system and of the hypothalamic-pituitary-adrenal axis, decreased sex hormone binding globulin synthesis and, possibly, high dietary lipid intake, may be additional mechanisms by which obesity favors the development of hyperandrogenism in PCOS.[53] A higher prevalence of PCOS has been reported in obese south Asian women residing in the United Kingdom when compared to their obese white Caucasian women counterparts. The south Asian women also present and seek treatment for PCOS at a younger age, have more severe symptoms, and higher fasting insulin concentrations with lower insulin sensitivity than white Caucasian women.[54]
Cardiovascular disease (CVD)
Obesity significantly contributes to morbidity and mortality from CVD. Earlier studies have shown that CVD processes begin early in childhood and are influenced by genetic factors as well as other potentially modifiable risk factors including obesity.[55] Obesity plays a major role in the pathogenesis of various CV diseases. Obesity is associated with hemodynamic overload by increasing total blood volume, cardiac output, and cardiac workload.[56] Childhood and adolescent adiposity have strong influences on the structure and function of the heart, predominantly of the left ventricle (LV).[49] LV afterload is elevated in obese individuals due to both increased peripheral resistance and greater conduit artery stiffness. Right ventricular afterload may be increased, presumably due to associated sleep disordered breathing and LV changes.[56] In addition, increased levels of leptin, an adipocyte-derivedhormone that controls food intake and energymetabolism, may also be related to CV disease. Studies have reported that obesity in childhood and adolescence is a determinant of a number of cardiovascular risk factors in adulthood.[57,58,59] Obesity may affect the heart through its influence on risk factors such as dyslipidemia, hypertension, glucose intolerance, inflammatory markers, obstructive sleep apnea/hypoventilation, and the prothrombotic state. A report on rural and urban students from Punjab showed that in those with a normal BMI, the prevalence of hypertension was 4.5%, while in those who were overweight it was 15.3% and in the obese it was 43.1%. In rural areas, 6.8% of the overweight students had sustained hypertension while in obese group it was 61.7%.[22] Another recent study from our group[24] showed that the prevalence of hypertension was 20.4% among obese/overweight and 5.2% among non-obese children (Odds Ratio 4.7, 95% CI: 4.2-5.3, P < 0.001).
Obstructive sleep apnea (OSA)
There is evidence to demonstrate that obstructive sleep apnea (OSA) is associated with obesity and is highly prevalent in children and adolescents. It is well established that obesity can result or worsen OSA, via several potential mechanisms. Several studies have reported decreasedupper airway muscle protectiveforce or altered muscle structure due tofatty deposits within the muscle[60] resulting in increasedcollapsible velopharynx during wakefulnessin obese individuals. This may lead to upper airway obstructionduring sleep. On the other hand, OSA may itself predispose individuals to worsening obesitybecause of sleep deprivation, daytime somnolence, and disrupted metabolism.[61] The pathophysiologic change of cardiovascular importance in OSA among children includes altered sympathovagal balance, increased oxidative stress, production of inflammatory cytokines, vascular remodeling, and endothelial cell dysfunction.[62] However, data from Indian children and adolescents is lacking.
Psychosocial problems
Numerous psychosocial problems have been shown to be strongly associated with obesity in children and adolescents. These include depression, poor self-image, and adjustment difficulties in both the home and social environment (including school). Psychosocial factors work against the child with a weight problem and thus hamper his/her overall growth and development. Overweight and obese adolescents tend to have poor body image and low self-esteem. Among obese children, appearance related teasing is more frequent and is associated with higher weight concerns, more loneliness, poor self-perception of physical appearance, higher preference for sedentary or isolated activities and lower preference for social activities.[63] Social isolation and stress could interfere with their learning and lead to depression, anxiety, and/or emotional instability.
Childhood obesity and adult mortality
It is well known that obesity, glucose intolerance, hypertension, and hypercholesterolemia in adult adulthood increase mortality rates. However, not many studies have been conducted to determine whether the presence of these risk factors in childhood predicts premature death. Franks et al.[64] studied a cohort of 4857 American Indian children without diabetes, who were born between 1945 and 1984 and followed them up for an average of 24 years. After standardizing the risk factors according to sex and age, it was seen that 559 individuals (11.5%) died before the age of 55 and there were 166 deaths from endogenous causes (3.4% of the cohort) during a median follow-up period of 23.9 years. The most common causes of death were alcohol-related liver disease and CVD. In this study, childhood obesity turned out to be the strongest predictor of premature death.
PREVENTION AND INTERVENTION STRATEGIES IN INDIA TO COMBAT CHILDHOOD OBESITY
There are numerous childhood obesity intervention programs that have been reported from the west[65,66,67,68] but there are very few from India.[69,70,71,72,73] Most of these interventions are primarily school based, involving diet, exercise and health education with a few integrating the family or community. The few Indian interventions[69,70,71,72,73] have been further described here and summarized in Table 1.
Table 1.
Intervention strategies from India to prevent/combat childhood obesity childhood obesity in India.[69,70,71,72,73]
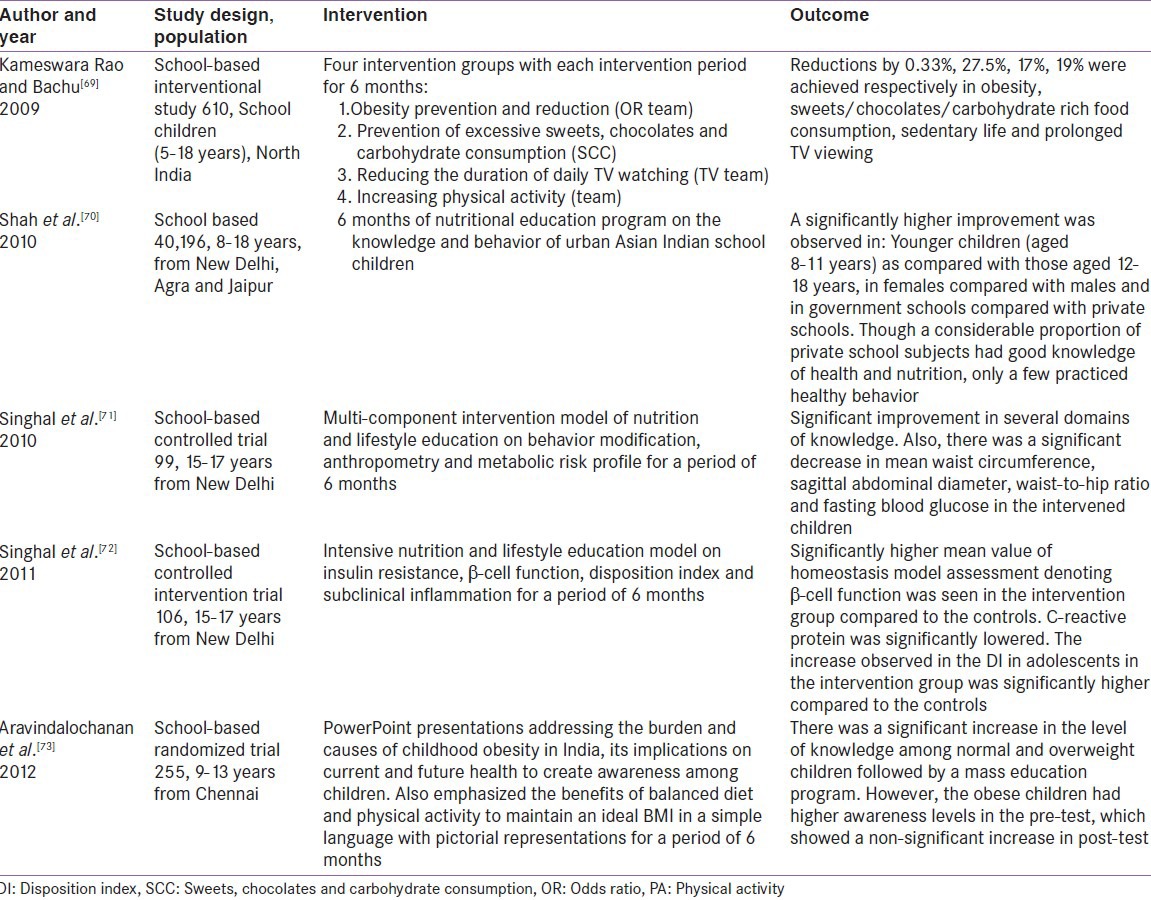
Kameswararao et al.[69] studied a school-based intervention in North India which consisted of four groups focusing on: Obesity prevention and reduction; prevention of excessive sweet, chocolate and carbohydrate consumption; reducing daily TV watching; and increasing physical activity. School aged children aged 5-18 years (n = 610) participated in weekly 2-hour sessions for 6 months. The intervention reported 0.33% reduction in obesity, 27.5% reduction in sweets, chocolates, and carbohydrate-rich food consumption, 17%, reduction in sedentary activities, and 19% reduction in prolonged TV watching. Shah et al.[70] aimed to evaluate the impact of a school-based health and nutritioneducation program on knowledge and behavior on 3128 school children (8-18 years), 2241 parents and 841 teachers from three different cities representing North India. Low baseline knowledge and behavior scores were reported in 75-94% of the government and 48-78% of the private school children, across all age groups. A significant improvement was observed in younger children (aged 8-11 years) compared with those aged 12-18 years; in females compared to males and in government schools compared to private schools (P < 0.05 for all). The same group[71] also reported the effectiveness of a more focused multi-component intervention model of nutrition and lifestyle education on behavior modification, anthropometry and metabolic risk profile in urban Indian adolescents. Two schools matched for student strength and socioeconomic strata were randomly allocated as intervention and control group. Changes in nutrition-related knowledge, attitude, lifestyle practices, food frequency and body image of eleventh-grade students (15-17 years) were tested in both schools. At 6 months follow-up, significant improvement in several domains of knowledge and lower consumption of aerated drinks and energy-dense unhealthy foods was observed in the intervention school children (n = 99) as compared to the control school children (n = 102). Another significant observation was that higher proportion of intervened children brought packed lunch and carried fruit to school compared to the control group. Additional measurements in relation to insulin resistance, β-cell function, disposition index, and subclinical inflammation were reported in another paper on the same cohort of adolescents which predictably showed marked improvements in these measures among the intervened children compared to the control group.[72] A recent study from southern India revealed that a significant increase in the level of knowledge among normal and overweight children can be achieved by a mass education program.[73]
Since, India is only waking up to this epidemic of childhood obesity, existing gaps in knowledge regarding prevention strategies for this age group should be addressed by conducting qualitative research in order to understand perceptions and barriers about childhood obesity among various stakeholders. This should be followed by implementing evidence-based interventions that can be successful and sustainable in the Indian setting.
CONCLUSIONS
Recent reviews on childhood obesity prevalence in India[74,75] clearly show that this trend is increasing in India thus making childhood overweight and obesity a significant public health problem. Effective prevention strategies are available for reversing this trend and India should initiate appropriate steps in this regard to put an early stop to the eventual consequences of childhood obesity. Public health interventions that can force implementation of strong policies especially targeting the built environment need to be instigated at the earliest, to effectively tackle this problem in the country. Childhood obesity is indeed a reality in India and the time for action is now!
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Popkin BM. Global nutrition dynamics: The world is shifting rapidly toward a diet linked with non-communicable diseases. Am J Clin Nutr. 2006;84:289–98. doi: 10.1093/ajcn/84.1.289. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation (WHO) 2005. Preventing chronic diseases: A vital investement, WHO Global report. [Last accessed on 2013 Oct 31]. Available from: http://www.who.int/chp/chronic disease report .
- 3.Singh AS, Mulder C, Twisk JW, Mechelen VW, Chinapaw MJ. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes Rev. 2008;9:474–88. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 4.Caballero B. A nutrition paradox-underweight and obesity in developing countries. N Engl J Med. 2005;325:1514–6. doi: 10.1056/NEJMp048310. [DOI] [PubMed] [Google Scholar]
- 5.Wright CM. Which threshold should india use to define childhood obesity and how much does it matter? Indian Pediatr. 2011;48:103–4. doi: 10.1007/s13312-011-0030-0. [DOI] [PubMed] [Google Scholar]
- 6.Global Strategy on Diet, Physical Activity and Health. [Last accessed on 2013 Nov 22]. Available from: http://www.who.int/dietphysicalactivity/childhood_why/en/index.html .
- 7.Aggarwal T, Bhatia RC, Singh D, Sobti PC. Prevalence of obesity and overweight in affluent adolescents from Ludhiana, Punjab. Indian Pediatr. 2008;45:500–2. [PubMed] [Google Scholar]
- 8.Sreevatsava M, Narayan KM, Cunningham SA. Evidence for interventions to prevent and control obesity among children and adolescents: Its applicability to India. Indian J Pediatr. 2013;80(Suppl 1):S115–22. doi: 10.1007/s12098-012-0881-y. [DOI] [PubMed] [Google Scholar]
- 9.Goyal RK, Shah VN, Saboo BD, Phatak SR, Shah NN, Gohel MC, et al. Prevalence of Overweight and Obesity in Indian Adolescent School Going Children: Its Relationship with Socioeconomic Status and Associated Lifestyle Factors. JAPI. 2010;58:151–8. [PubMed] [Google Scholar]
- 10.Malik VS, Popkin BM, Bray GA, Després JP, Hu FB. Sugar sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356–64. doi: 10.1161/CIRCULATIONAHA.109.876185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caprio S. Calories from Soft Drinks - Do They Matter? N Engl J Med. 2012;367:1462–3. doi: 10.1056/NEJMe1209884. [DOI] [PubMed] [Google Scholar]
- 12.Popkin BM. The nutrition transition and obesity in the developing world. J Nutr. 2001;131:871S–3. doi: 10.1093/jn/131.3.871S. [DOI] [PubMed] [Google Scholar]
- 13.Dehghan M, Danesh NA, Merchant AT. Childhood obesity, prevalence and prevention. Nutr J. 2005;4:24. doi: 10.1186/1475-2891-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raj M, Krishna Kumar R. Obesity in children and adolescents. Indian J Med Res. 2010;132:598–607. [PMC free article] [PubMed] [Google Scholar]
- 15.Global School based health survey. [Last accessed on 2013 Dec 08]. Available from: http://www.who.int/chp/gshs/2007_India_CBSE_fact_sheet.pdf .
- 16.Kotian MS, Kumar GS, Kotian SS. Prevalence and Determinants of Overweight and Obesity among Adolescent School Children of South Karnataka, India. Indian J Community Med. 2010;35:176–8. doi: 10.4103/0970-0218.62587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.James WP. The challenge of childhood obesity. Int J Pediatr Obes. 2006;1:7–10. doi: 10.1080/17477160600630404. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 19.Cohen D, Babey S. Candy at the Cash Register - A Risk Factor for Obesity and Chronic Disease. N Engl J Med. 2012;15:1381–3. doi: 10.1056/NEJMp1209443. [DOI] [PubMed] [Google Scholar]
- 20.Raj M, Sundaram KR, Paul M, Deepa AS, Kumar RK. Obesity in Indian children: Time trends and relationship with hypertension. Natl Med J India. 2007;20:288–93. [PubMed] [Google Scholar]
- 21.Marwaha RK, Tandon N, Singh Y, Aggarwal R, Grewal K, Mani K. A Study of Growth Parameters and Prevalence of Overweight and Obesity in School Children from Delhi. Indian Pediatr. 2006;43:943–52. [PubMed] [Google Scholar]
- 22.Kaneria Y, Singh P, Sharma DC. Prevalence of Overweight and Obesity in Relation to Socio-economic Conditions in Two Different Groups of School-age Children of Udaipur City (Rajasthan) Indian Acad Clin Med J. 2006;7:133–5. [Google Scholar]
- 23.Unnithan AG, Syamakumari S. Prevalence of Overweight, Obesity and Underweight among School Going Children in Rural and Urban areas of Thiruvananthapuram Educational District, Kerala State (India) Internet J Nutr Wellness. 2008. [Last accessed on 2013 Nov 12]. p. 6. Available from http://ispub.com/IJNW/6/2/7073 .
- 24.Sonya J, Ranjani H, Priya M, Anjana RM, Mohan V. Prevalence of over-weight and obesity among school going children and adolescents in Chennai using a national and international cut point (ORANGE-3) Indian Pediatr. 2014;51:544–9. doi: 10.1007/s13312-014-0444-6. [DOI] [PubMed] [Google Scholar]
- 25.Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Avon Longitudinal Study of Parents and Children Study Team. Early life risk factors for obesity in childhood: Cohort study. BMJ. 2005;330:1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 27.Sharma A, Sharma K, Mathur KP. Growth pattern and prevalence of obesity in affluent schoolchildren of Delhi. Public Health Nutr. 2007;10:485–91. doi: 10.1017/S1368980007223894. [DOI] [PubMed] [Google Scholar]
- 28.Kries VR, Koletzko B, Sauerwald T, Mutius VE, Barnert D, Grunert V, et al. Breast feeding and obesity: Cross sectional study. BMJ. 1999;319:147–50. doi: 10.1136/bmj.319.7203.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, et al. Overweight in children and adolescents: Pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 30.Barker DJ, Eriksson JG, Forsen T, Osmond C. Fetal origins of adult disease: Strength of effects and biological basis. Int J Epidemiol. 2002;31:1235–9. doi: 10.1093/ije/31.6.1235. [DOI] [PubMed] [Google Scholar]
- 31.Dietz WH. Overweight in childhood and adolescence. N Engl J Med. 2004;350:855–7. doi: 10.1056/NEJMp048008. [DOI] [PubMed] [Google Scholar]
- 32.Ibáñez L, Ong K, Dunger DB, de Zegher F. Early development of adiposity and insulin resistance after catch-up weight gain in small-for-gestational-age children. J Clin Endocrinol Metab. 2006;91:2153–8. doi: 10.1210/jc.2005-2778. [DOI] [PubMed] [Google Scholar]
- 33.Whitaker RC, Pepe MS, Wright JA, Seidel KD, Dietz WH. Early adiposity rebound and the risk of adult obesity. Pediatrics. 1998;101:E5. doi: 10.1542/peds.101.3.e5. [DOI] [PubMed] [Google Scholar]
- 34.Velasquez-Mieyer P, Perez-Faustinelli S, Cowan PA. Identifying Children at Risk for Obesity, Type 2 Diabetes, and Cardiovascular Disease. Diabetes Spectr. 2005;18:213–20. [Google Scholar]
- 35.Lillioja S, Mott DM, Zawadzki JK, Young AA, Abbott WG, Bogardus C. Glucose storage is a major determinant of in vivo “insulin resistance” in subjects with normal glucose tolerance. J Clin Endocrinol Metab. 1986;62:922–7. doi: 10.1210/jcem-62-5-922. [DOI] [PubMed] [Google Scholar]
- 36.Tataranni PA. Pathophysiology of obesity-induced insulin resistance and type 2 diabetes mellitus. Eur Rev Med Pharmacol Sci. 2002;6:27–32. [PubMed] [Google Scholar]
- 37.Greco AV, Mingrone G, Giancaterini A, Manco M, Morroni M, Cinti S, et al. Insulin resistance in morbid obesity: Reversal with intramyocellular fat depletion. Diabetes. 2002;51:144–51. doi: 10.2337/diabetes.51.1.144. [DOI] [PubMed] [Google Scholar]
- 38.Boden G. Obesity, insulin resistance and free fatty acids. Curr Opin Endocrinol Diabetes Obes. 2011;18:139–43. doi: 10.1097/MED.0b013e3283444b09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garg A. Lipodystrophies. Am J Med. 2000;108:143–52. doi: 10.1016/s0002-9343(99)00414-3. [DOI] [PubMed] [Google Scholar]
- 40.Bao W, Srinivasan SR, Wattigney WA, Berenson GS. Persistence of multiple cardiovascular risk clustering related to syndrome X from childhood to young adulthood. The Bogalusa Heart Study. Arch Intern Med. 1994;154:1842–7. [PubMed] [Google Scholar]
- 41.Misra A, Vikram NK, Arya S, Pandey RM, Dhingra V, Chatterjee A, et al. High prevalence of insulin resistance in postpubertal Asian Indian children is associated with adverse truncal body fat patterning, abdominal adiposity and excess body fat. Int J Obes Relat Metab Disord. 2004;28:1217–26. doi: 10.1038/sj.ijo.0802704. [DOI] [PubMed] [Google Scholar]
- 42.Yajnik CS, Lubree HG, Rege SS, Naik SS, Deshpande JA, Deshpande SS, et al. Adiposity and hyperinsulinemia in Indians are present at birth. J Clin Endocrinol Metab. 2002;87:5575–80. doi: 10.1210/jc.2002-020434. [DOI] [PubMed] [Google Scholar]
- 43.Vikram NK, Misra A, Pandey RM, Luthra K, Wasir JS, Dhingra V. Heterogeneous phenotypes of insulin resistance and its implications for defining metabolic syndrome in Asian Indian adolescents. Atherosclerosis. 2006;186:193–9. doi: 10.1016/j.atherosclerosis.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 44.Li C, Ford ES, McGuire LC, Mokdad AH, Little RR, Reaven GM. Trends in hyperinsulinemia among nondiabetic adults in the U.S. Diabetes Care. 2006;29:2396–402. doi: 10.2337/dc06-0289. [DOI] [PubMed] [Google Scholar]
- 45.Fajans SS. Maturity-onset diabetes of the young (MODY) Diabetes Metab Rev. 1989;5:579–606. doi: 10.1002/dmr.5610050705. [DOI] [PubMed] [Google Scholar]
- 46.Yajnik CS, Ganpule-Rao AV. The obesity-diabetes association: What is different in Indians? Int J Low Extrem Wounds. 2010;9:113–5. doi: 10.1177/1534734610380028. [DOI] [PubMed] [Google Scholar]
- 47.Fall CH, Sachdev HS, Osmond C, Lakshmy R, Biswas SD, Prabhakaran D, et al. Adult metabolic syndrome and impaired glucose tolerance are associated with different patterns of BMI gain during infancy: Data from the New Delhi Birth Cohort. Diabetes Care. 2008;31:2349–56. doi: 10.2337/dc08-0911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pinhas-Hamiel O, Zeitler P. The global spread of type 2 diabetes mellitus in children and adolescents. J Pediatr. 2005;146:693–700. doi: 10.1016/j.jpeds.2004.12.042. [DOI] [PubMed] [Google Scholar]
- 49.Raj M. Obesity and cardiovascular risk in children and adolescents. Indian J Endocrinol Metab. 2012;16:13–9. doi: 10.4103/2230-8210.91176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ranjani H, Sonya J, Anjana RM, Mohan V. Prevalence of Glucose Intolerance Among Children and Adolescents in Urban South India (ORANGE-2) Diabetes Technol Ther. 2013;15:13–9. doi: 10.1089/dia.2012.0236. [DOI] [PubMed] [Google Scholar]
- 51.Littlejohn EE, Weiss RE, Deplewski D, Edidin DV, Rosenfield R. Intractable early childhood obesity as the initial sign of insulin resistant hyperinsulinism and precursor of polycystic ovary syndrome. J Pediatr Endocrinol Metab. 2007;20:41–51. doi: 10.1515/jpem.2007.20.1.41. [DOI] [PubMed] [Google Scholar]
- 52.Diamanti-Kandarakis E, Christakou CD, Kandaraki E, Alexandraki KI. Early onset adiposity: A pathway to polycystic ovary syndrome in adolescents? Hormones (Athens) 2007;6:210–7. [PubMed] [Google Scholar]
- 53.Gambineri A, Pelusi C, Vicennati V, Pagotto U, Pasquali R. Obesity and the polycystic ovary syndrome. Int J Obes Relat Metab Disord. 2002;26:883–96. doi: 10.1038/sj.ijo.0801994. [DOI] [PubMed] [Google Scholar]
- 54.Wijeyaratne CN, Balen AH, Barth JH, Belchetz PE. Clinical manifestations and insulin resistance (IR) in polycystic ovary syndrome (PCOS) among South Asians and Caucasians: Is there a difference? Clin Endocrinol. 2002;57:343–50. doi: 10.1046/j.1365-2265.2002.01603.x. [DOI] [PubMed] [Google Scholar]
- 55.Hayman LL, Meininger JC, Daniels SR, McCrindle BW, Helden L, Ross J, et al. Primary prevention of cardiovascular disease in nursing practice: Focus on children and youth: A scientific statement from the American Heart Association Committee on Atherosclerosis, Hypertension, and Obesity in Youth of the Council on Cardiovascular Disease in the Young, Council on Cardiovascular Nursing, Council on Epidemiology and Prevention, and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116:344–57. doi: 10.1161/CIRCULATIONAHA.107.184595. [DOI] [PubMed] [Google Scholar]
- 56.Alpert MA. Obesity cardiomyopathy: Pathophysiology and evolution of the clinical syndrome. Am J Med Sci. 2001;321:225–36. doi: 10.1097/00000441-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 57.Haji SA, Ulusoy RE, Patel DA, Srinivasan SR, Chen W, Delafontaine P, et al. Predictors of left ventricular dilatation in young adults (from the Bogalusa Heart Study) Am J Cardiol. 2006;98:1234–7. doi: 10.1016/j.amjcard.2006.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lauer RM, Lee J, Clarke WR. Factors affecting the relationship between childhood and adult cholesterol levels: The Muscatine Study. Pediatrics. 1988;82:309–18. [PubMed] [Google Scholar]
- 59.Raitakari OT, Juonala M, Viikari JS. Obesity in childhood and vascular changes in adulthood: Insights into the Cardiovascular Risk in Young Finns Study. Int J Obes (Lond) 2005;29(Suppl 2):S101–4. doi: 10.1038/sj.ijo.0803085. [DOI] [PubMed] [Google Scholar]
- 60.Carrera M, Barbe F, Sauleda J, Tomas M, Gomez C, Santos C, et al. Effects of obesity upon genioglossus structure and function in obstructive sleep apnoea. Eur Respir J. 2004;23:425–9. doi: 10.1183/09031936.04.00099404. [DOI] [PubMed] [Google Scholar]
- 61.Pillar G, Shehadeh N. Abdominal fat and sleep apnea: The chicken or the egg? Diabetes Care. 2008;31(Suppl 2):S303–9. doi: 10.2337/dc08-0715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Katz ES, D’Ambrosio CM. Pediatric obstructive sleep apnea syndrome. Clin Chest Med. 2010;31:221–34. doi: 10.1016/j.ccm.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 63.Hayden-Wade HA, Stein RI, Ghaderi A, Saelens BE, Zabinski MF, Wilfley DE. Prevalence, characteristics, and correlates of teasing experiences among overweight children vs. non-overweight peers. Obes Res. 2005;13:1381–92. doi: 10.1038/oby.2005.167. [DOI] [PubMed] [Google Scholar]
- 64.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood Obesity, Other Cardiovascular Risk Factors, and Premature Death. N Engl J Med. 2010;362:485–93. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vandongen R, Jenner DA, Thompson C, Taggart AC, Spickett EE, Burke V, et al. A controlled evaluation of a fitness and nutrition intervention program on cardiovascular health in 10- to 12-year-old children. Prev Med. 1995;24:9–22. doi: 10.1006/pmed.1995.1003. [DOI] [PubMed] [Google Scholar]
- 66.Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, et al. Outcomes of a field trial to improve children's dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health. CATCH collaborative group. JAMA. 1996;275:768–76. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- 67.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, Hovell ME. The Effects of a 2-Year Physical Education Program (SPARK) on Physical Activity and Fitness in Elementary School Students. Am J Public Health. 1997;87:1328–34. doi: 10.2105/ajph.87.8.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Muller MJ, Asbeck I, Mast M, Langnase K, Grund A. Prevention of obesity - more than an intention. Concept and first results of the Kiel Obesity Prevention Study (KOPS) Int J Obes Relat Metab Disord. 2001;25:S66–74. doi: 10.1038/sj.ijo.0801703. [DOI] [PubMed] [Google Scholar]
- 69.Kameswararao AA, Bachu A. Survey of childhood diabetes and impact of school level educational interventions in rural schools in Karimnagar district. Int J Diabetes Dev Ctries. 2009;29:73. doi: 10.4103/0973-3930.53123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shah P, Misra A, Gupta N, Hazra DK, Gupta R, Seth P, et al. Improvement in nutrition related knowledge and behaviour of urban Asian Indian school children: Findings from the ’Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing’ (MARG) intervention study. Br J Nutr. 2010;104:427–36. doi: 10.1017/S0007114510000681. [DOI] [PubMed] [Google Scholar]
- 71.Singhal N, Misra A, Shah P, Gulati S. Effects of controlled school-based multi-component model of nutrition and lifestyle interventions on behavior modification, anthropometry and metabolic risk profile of urban Asian Indian adolescents in North India. Eur J Clin Nutr. 2010;64:364–73. doi: 10.1038/ejcn.2009.150. [DOI] [PubMed] [Google Scholar]
- 72.Singhal N, Misra A, Shah P, Gulati S, Bhatt S, Sharma S, et al. Impact of intensive school-based nutrition education and lifestyle interventions on insulin resistance, β-cell function, disposition index, and subclinical inflammation among Asian Indian adolescents: A controlled intervention study. Metab Syndr Relat Disord. 2011;9:143–50. doi: 10.1089/met.2010.0094. [DOI] [PubMed] [Google Scholar]
- 73.Aravindalochanan V, Rengarajan M, Kumpatla S, Rajan R, Viswanathan V. Impact of Awareness Program on Prevention of Childhood Obesity among School Children in a Metropolitan City – Chennai Slim and Fit Programme. J Educ Pract. 2012;3:88–95. [Google Scholar]
- 74.Gupta N, Shah P, Nayyar S, Misra A. Childhood Obesity and the Metabolic Syndrome in Developing Countries. Indian J Pediatr. 2013;80:S28–37. doi: 10.1007/s12098-012-0923-5. [DOI] [PubMed] [Google Scholar]
- 75.Ranjani H, Mehreen TS, Pradeepa R, Anjana RM, Garg R, Anand K, et al. Epidemiology of childhood overweight and obesity in India - Current Scenario. A World Health Organization (WHO) working document 2013-APW PO NO. 200637279 NCD/SEARO WHO India [Google Scholar]


