Abstract
Background
Human immunodeficiency virus (HIV) epidemic among youth is largely ignored and remains invisible to both young people themselves and to the society as a whole. Thus, the aim of the study was to assess the extent of perception risk of HIV and utilization of voluntary counseling and testing (VCT) service among high school students at Debre-berhan Town, Amhara Regional State, Ethiopia.
Methods
A cross-sectional study was carried out from November 2010 up to January 2011 among secondary school students at Debre-berhan Town. Perception risk and VCT use were considered as dependant variables. A stratified random sampling technique was used to recruit study participants by taking schools as strata. Semi-structured self-administered questionnaire was used to collect the necessary data. Data was entered and analyzed using SPSS version 17.0. P-value < 0.05 was considered as statistically significant.
Results
A total of 339 students were consented to participate in the study and the response rate was 96.3%. The student ages’ were ranged from 15 up to 24 years. Among the study participants, 30 (8.8%) had sexual contact and the mean age of first sexual encounter was 16.4 (SD =2.05) years. Of sexually active students, 12 (40%) had sex with different persons within the last 6 months, 13 (43.3%) had ever used condom and 15 (50%) had used VCT service. There was no statistically significant association between risk perception towards HIV infection and ever use of VCT service (AOR (95% CI) = 1.0(0.30, 4.02).
Conclusions
Some students were engaged in risky sexual behavior even though they had heard about HIV/AIDS. The perception of risk for acquisition of HIV infection and utilization of VCT were low. Thus, education on topic of HIV/AIDS through integrating as part of school curriculum and encouraging the existing health institutions to provide youth-friendly sexual counseling services including VCT for HIV are strongly recommended.
Keywords: Students, Risk perception, VCT use, HIV, Debre-berhan, Ethiopia
Background
Globally, an estimated 35 million people were living with human immunodeficiency virus (HIV) in 2012. At the same time, there were 2.3 million new HIV infections which showed a reduction by 33% as compared from 3.1 million new infections in 2001. Similarly, the number of HIV related deaths was also reduced up to 1.6 million in 2012 as compared from 2.3 million in 2005 [1].
In spite of improved access to antiretroviral treatment and care in many regions of the world, sub Saharan African countries took their greatest share for HIV epidemic [2]. Young people are particularly vulnerable to HIV pandemic and more than half of all new infections worldwide occur between the ages of 15 and 24 [3].
HIV/acquired immunodeficiency syndrome (AIDS) epidemic among youth is largely ignored and remains invisible to both young people themselves and to society as a whole so that the young are more likely to carry the virus for years without knowing that they are infected. Consequently, the epidemic spreads beyond high risk groups to the broader population due to which HIV/AIDS control programs become harder to succeed. Current data indicates that about 20% of young people in Africa, whose age range from 15 up to 19 years (mainly secondary school students), are infected with HIV virus [4].
A study which was done in Nigerian youth in 2007 revealed that about 43% of young people have had sex by the age of 15 and nearly 70% of sexual activity among them was unprotected [5]. In the same study, over one-third of boys and young men had slept with two or more partners in the previous three month. Additionally, the study revealed that about 90% of youth were unable to name all three principal way of avoiding HIV. Only 35% of them who knew that condom is protective used it one last time during sex as compared with 19% of those who did not know. Over one-third of them did not know where to buy condoms. Only 9% of them thought they were at high risk of contracting HIV; however, majority of the youth (86%) did not think they were at significant risk, ether because they explicitly thought they were safe or else they do not know about HIV/AIDS. Out of 70% of youth, who would like to have an HIV test, only 6% have had done the test.
These and other similar studies [3–5] indicated that still more work remain on awareness and behavioral changes among the most vulnerable section of the society, the youth. This was due to the fact that the number of youth who become infected with HIV was significantly increasing which accounts more than 50% of new HIV infection at global level as compared to other segments of risky population groups.
In absence of an effective vaccine and cure, voluntary counseling and testing service has been used as an entry point for behavioral change and access to antiretroviral treatment. Moreover, voluntary counseling and testing (VCT) is helping in the prevention of HIV transmission from mother-to-child with antiretroviral drugs through modification of infant feeding practice [2]. When HIV test was developed, it was intended to be accompanied by HIV counseling service. However, with growing awareness of HIV/AIDS and recent availability of antiretroviral therapy (ART), the scope of and reasons for voluntary counseling and HIV testing services have been broadened. VCT is a process by which an individual undergoes counseling to enable her/him to make an informed decision about being tested for HIV, assess their personal risk for HIV and develop a risk reduction strategy [6]. The service is essential components of HIV prevention and care programs. However, initially many young people were reluctant to be tested even if care and treatment were made available to them [6].
HIV voluntary counseling and testing service (VCT) is now widely accepted as the cornerstone of HIV prevention program in many countries because of its multiple benefits [7]. Unfortunately, many people including the young do not seek the services until they develop symptoms of AIDS [4]. Among the youth, barriers to use VCT service include lack of information, perception of low risk, lack of privacy and confidentiality, costs and laws that require parental consent [4].
In Ethiopia, HIV counseling and testing (HCT) begun few years before with service expanding throughout the country and it was reported that many young people with HIV in Ethiopia did not know that they were infected with the virus [8]. On the other hand, in 2011, Ethiopian Demographic Health Survey (EDHS) revealed that the overall prevalence of HIV in Ethiopia was estimated to be around 1.5% among the population whose age groups in between 15 up to 49 years [9]. Besides, women had a higher HIV prevalence (1.9%) as compared to men (1.0%). At the same time, the survey mentioned that 24% of women and 34% of men, whose age in between 15 up to 24 years, had comprehensive knowledge about HIV/AIDS. Their level of knowledge increased steadily with their educational status, but their main sources of information were believed to be from mass media, health professionals and schools. Similarly, 25% of young women and 28% of men, who had had sexual intercourse, had been tested for HIV. Another study conducted among high school students in Ethiopia showed that 62.2% of them supported the use of condom during sexual intercourse, but only 42.2% of students reported ever to have used condom during their first sexual encounter, while only 27.7% mentioned that they used condom every time [10].
The current study was different from the other studies conducted in Ethiopia, because it was mainly focused on assessing the students’ personal believe of HIV infection and their associated risk factors with comparisons of HIV testing. Hence, the objectives of the study were to identify students’ perception towards their susceptibility of HIV infection as well as their tendency on utilizing VCT and its barriers to the service.
Methods
Study design and area
A cross-sectional survey was conducted among high school students from November 2010 up to January 2011 at Debre-berhan Town, Amhara Regional State, Ethiopia. Ethiopia consisted of 9 regional states and 2 city administrations. Amhara Regional States had a total of 706 high schools [11]. Debre-berhan was one of the oldest towns within the region and located at 130 km towards the North East of Addis Ababa, the capital city of Ethiopia. Size of population in the town, for the year 2007 national census, was about 65,231. Out of which, 31,668 (48.5%) were males and 33,563 (51.5%) females [11]. There were one public high school and preparatory school in the town. High school contained from grade 9 up to grade 10, while preparatory school was from grade 11 up to grade 12.
Study population
Debre-berhan high school students of both sexes from the two schools were used as source population.
Exclusion criteria
Students who were not attending their class during the data collection period, evening students (those who were learning in the evening) and those who were not willing to take part in the study were not included.
Sample size estimation
The required simple size was determined using  where p is prevalence of the intention to get HIV test, Δ is margin of error between the sample estimate and true population value and z is critical value corresponding to a given level of confidence. Assuming 95% confidence level and 4% margin of error [12] and estimated demand of 85% for VCT based on previous Ethiopian study [12], the required minimum sample size was 306. With additional assumption of 15% non-response rate, the overall sample size was 352.
where p is prevalence of the intention to get HIV test, Δ is margin of error between the sample estimate and true population value and z is critical value corresponding to a given level of confidence. Assuming 95% confidence level and 4% margin of error [12] and estimated demand of 85% for VCT based on previous Ethiopian study [12], the required minimum sample size was 306. With additional assumption of 15% non-response rate, the overall sample size was 352.
Sampling techniques
A stratified random sampling technique was used to recruit the required number of students from the two secondary schools in Debre-berhan Town where the strata were grade 9, 10, 11 and 12. Students that correspond to a given grade were selected through simple random sampling technique using the school roster as a sampling frame.
Sampling procedure
High schools consisted of grades 9, 10, 11 and 12. Each of which having several study populations were categorized from source population based on the level of the grade. The numbers of study subjects included in each grade were proportional to their size. Then, sections to be included in each grade were selected based on simple random sampling. The students from the selected sections were assembled in a room and requested to fill out questionnaire in the presence of data collectors. Data collection process was monitored by the two trained data collectors.
Instrument of data collection
Data was collected using semi-structured self-administered questionnaire. The questionnaire was prepared first in English and it was then translated in to Amharic which was the official language of the study area. Amharic version of the questionnaire was pre-tested for clarity, acceptability and flow among non-study subjects before actual data collection and necessary adjustments were made. The questionnaire was adapted from HIV/AIDS behavioral surveillance survey (BSS) of Ethiopia [8]. A total of 44 questions were involved in the questionnaire. Most of questions were linked to demographic characteristics, perception risk including knowledge, attitude, practice of HIV/AIDS and VCT of the students.
Data analysis
The questionnaire which was completed by the study participating students was coded and computerized using SPSS version 17.0 packages. Students were classified as being knowledgeable about HIV transmission if they were able to provide correct response to all four questions describing means of HIV transmission (i.e. mother-to-child, blood transfusion, sexual intercourse and injury with sharp contaminated materials). Data was summarized using frequencies and percentages. Logistic regression was used to adjust for possible confounding factors. Results were reported statistically significant if P-value was less than 0.05.
Dependent variables
Perception risk and VCT use were considered as dependent variables.
Independent variables
Age, sex, marital status, level of education, use of condom, ever practice sex, VCT use were considered as independent variables.
Operational definitions
Youth
Those who are in the age group from 15 up to 24 years.
Perception
A reception and interpretation of sensory input related to HIV preventive method.
Risk
A situation in which an action will result in an outcome that is not known with certainty, but the set of possible outcomes and their associated probabilities are known or can be estimated.
Behavior
Various voluntary movements undertaken by the body in response to motives and decision related to HIV preventive methods.
Perception risk
Students’ attitude towards perceiving themselves as susceptible to HIV infection.
High risk perception
Students were considered to have high perception risk if they had been exposed to at least one of the conditions like having sex without condom, having sex with prostitution, having sex with HIV infected person and having injury with HIV infected sharp materials.
Low risk perception
Students were considered to have low perception risk if they had no sexual contact, if they had used condom during sexual intercourse and being faithful to their sexual partners.
Ethical considerations
Ethical clearance was obtained before data collection from Institutional Review Board of Aklilu Lemma Institute of Pathobiology, AAU. Then, formal letter was written to Debre-berhan Woreda Educational Bureau and the two targeted high schools. Consent was requested from the students prior to the study there by informing them to participate or refuse in the study. No personal identification was recorded on the questionnaire for ethical reason.
Results
Socio-demographic characteristics
A total of 339 students participated in the study and the response rate was 96.3%. Out of the total respondents, 161 (47.5%) were males and the rest were females. The mean age of the study participants was 17.1 (SD = 2.1) years. Three hundred and thirty-four (98.5%) of the respondents were never married. The majority of the respondents 330 (97.3%) were Amhara by ethnicity and 321 (94.7%) were Orthodox Christians followed by Protestants 9 (2.7%). Among the total respondents, 240 (70.8%) were from grade 9 up to grade 10 and the rest were from grade 11 up to grade 12 students (Table 1).
Table 1.
Socio-demographic characteristics of high school students in Debre-berhan Town, January 2010
| Variables | Number | Percent (%) |
|---|---|---|
| Age | ||
| 15-19 | 308 | 90.9 |
| 20-24 | 31 | 9.1 |
| Sex | ||
| Male | 161 | 47.5 |
| Female | 178 | 52.5 |
| Residence | ||
| Urban | 289 | 85.3 |
| Rural | 50 | 14.7 |
| Marital status | ||
| Single | 334 | 98.5 |
| Married | 5 | 1.5 |
| Ethnicity | ||
| Amhara | 330 | 97.3 |
| Oromo | 5 | 1.5 |
| Tigre | 1 | 0.3 |
| Other | 3 | 0.9 |
| Educational status | ||
| 9-10 | 240 | 70.8 |
| 11-12 | 99 | 29.2 |
Knowledge related to HIV/AIDS
All respondents heard about HIV/AIDS, and the most frequently mentioned sources of information for HIV/AIDS were mass media 211 (62.2%) followed by health professionals 177 (52.2%) (Figure 1). Two hundred and seventy-four (80.8%) of students responded that HIV can be transmitted by sexual means whereas 217 (64%) of the respondents reported that it is possible for the virus to be transmitted from mother-to-child. Additionally, 236 (69.6%) and 200 (59%) of students said that the HIV can be transmitted through sharp injury with HIV infected blood materials and blood transfusion, respectively.
Figure 1.
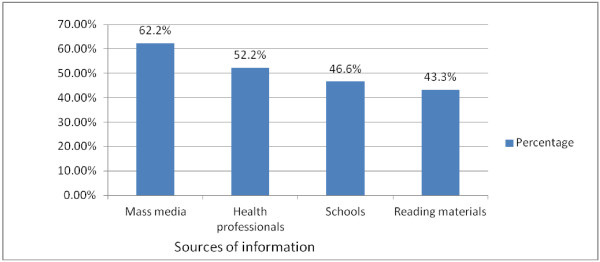
Sources of information for HIV among high school students in Debre-berhan Town, January 2010.
Condom use 295 (87%), abstinence 233 (68.7%), and being faithful to one partner 128 (37.8%) were mentioned as means of best preventing methods for HIV/AIDS. In addition, 299 (88.2%) of students mentioned that virginity should be encouraged as it is one of prevention method for HIV (Table 2). Knowledge on HIV transmission was inversely and significantly associated with educational status (P < 0.05). Students with high school level were less knowledgeable about HIV transmission compared to students who were in preparatory level (AOR (95% CI) =0.3 (0.2, 0.5) (Table 3).
Table 2.
Knowledge of students on modes of HIV transmission and best prevention method in Debre-berhan Town, January 2010
| Variable | M (%) | F (%) | Total (%) |
|---|---|---|---|
| Variable | |||
| Yes | 142 (41.9) | 132 (38.9) | 274 (80.8) |
| No | 19 (5.6) | 46 (13.6) | 65 (19.2) |
| Mother-to-fetus | |||
| Yes | 125 (36.9) | 92 (27.1) | 217 (64) |
| No | 36 (10.6) | 86 (25.4) | 122 (36) |
| Insect bite transmit HIV | |||
| Yes | 50 (14.7) | 87 (25.7) | 137 (40.4) |
| No | 111 (32.7) | 91 (26.8) | 202 (59.6) |
| Kissing transmit HIV | |||
| Yes | 34 (10) | 68 (20.1) | 102 (30.1) |
| No | 127 (37.5) | 110 (32.4) | 237 (69.9) |
| Abstinence protects from HIV | |||
| Yes | 121 (35.7) | 112 (33) | 233 (68.7) |
| No | 40 (11.8) | 66 (19.5) | 106 (31.3) |
| Faithfulness protects from HIV | |||
| Yes | 51 (15.1) | 77 (22.7) | 128 (37.8) |
| No | 110 (32.4) | 101 (29.8) | 211 (62.2) |
| Condom use protects from HIV | |||
| Yes | 147 (43.4) | 148 (43.7) | 295 (87) |
| No | 14 (4.1) | 30 (8.9) | 44 (13) |
NB: Percents will not add up to 100, as multiple responses are possible.
Table 3.
Correlates of knowledge on HIV transmissions with selected variables among high school students in Debre-berhan Town, January 2010
| Variables | Knowledge on HIV | OR (95% CI) | ||
|---|---|---|---|---|
| Yes | No | Crude | Adjusted* | |
| Sex | ||||
| Male | 97 | 64 | 0.5 (0.2, 0.7) | 0.6 (0.4, 1.0) |
| Female | 73 | 105 | 1.0 | 1.0 |
| Age | ||||
| 15-19 | 149 | 159 | 0.3 (0.5, 0.7) | 0.6 (0.3, 1.6) |
| 20-24 | 21 | 10 | 1.0 | 1.0 |
| Educational status | ||||
| 9-10 | 92 | 148 | 0.2 (0.1, 0.4) | 0.3 (0.2, 0.5) ** |
| 11-12 | 78 | 21 | 1.0 | 1.0 |
| Marital status | ||||
| Single | 168 | 166 | 1.5 (0.3, 9.2) | 1.3 (0.2, 11.0) |
| Married | 2 | 3 | 1.0 | 1.0 |
| Ever practiced sex | ||||
| Yes | 10 | 20 | 1.2 (0.6, 2.4) | 1.0 (0.4, 2.5) |
| No | 160 | 149 | 1.0 | 1.0 |
| Risk perception | ||||
| Low | 167 | 156 | 2.0 (0.6, 5.7) | 2.0 (0.5, 7.2) |
| High | 3 | 13 | 1.0 | 1.0 |
| Willingness to VCT | ||||
| Yes | 149 | 141 | 0.9 (0.5, 1.7) | 0.8 (0.4, 1.6) |
| No | 21 | 28 | 1.0 | 1.0 |
NB**=significant (P<0.05).
Adjusted*: for sex, age, educational status, marital status, ever practiced sex, risk perception, willingness to VCT.
Discrepancies had been observed among the respondents’ knowledge and their practices. Only 7 (23.3%) of those respondents who ever had sex believed appropriate use of condom can be protective against HIV and 13 (43.3%) of them did use condom during last sexual intercourse. Eighteen (60%) of those who ever had sex knew that abstaining can protect people from HIV infection. Similarly, 15 (50%) of those who had sex knew that faithfulness can protect people from HIV infection and 12 (40%) of them were not faithful during sexual activity.
Risk perception on HIV/AIDS
Participants’ perception on their susceptible to HIV infection was asked and the result indicated that 323 (95.3%) and 16 (4.7%) believed to have low and high chances of acquiring the virus, respectively. The proportions of students who perceived themselves at risk of contracting HIV were not similar for both sexes. Among those who perceived themselves at risk, 12 (3.5%) reported that they had sex without condom, 2 (0.6%) had injury with contaminated materials, 1 (0.3%) had sex with prostitute, 1 (0.3%) had sex with HIV positive person. The most frequently cited reasons by those who did not perceive themselves at risk were absence of sexual contact 309 (91.2%) followed by using condom 13 (3.8%) and faithful to one partner 12 (3.5%) (Table 4).
Table 4.
Proportion of students by HIV risk perception and reasons for risk perception in Debre-berhan Town, January 2010
| Variable | M (%) | F (%) | Total (%) |
|---|---|---|---|
| Risk perception | |||
| Low | 154 (45.4) | 169 (49.9) | 323 (95.3) |
| High | 7 (2) | 9 (2.7) | 16 (4.7) |
| Reasons for risk | |||
| Had sex without condom | 4 (1.2) | 8 (2.4) | 12 (3.6) |
| Injury with contaminated material | 2 (0.6) | ------ | 2 (0.6) |
| Had sex with prostitution | 1 (0.3) | ------ | 1 (0.3) |
| Had sex with HIV positive person | ----- | 1 (0.3) | 1 (0.3) |
| Reasons for not at risk | |||
| Never had sex | 144 (42.5) | 165 (48.7) | 309 (91.2) |
| Use condom | 11 (3.2) | 2 (0.6) | 13 (3.8) |
| Faithful to partner | 6 (1.8) | 6 (1.8) | 12 (3.6) |
NB: Percents will not add up to 100, as multiple responses are possible.
Risk perception of HIV was significantly associated with those students who had ever practiced sex (AOR (95% CI) =0.02(0.01, 0.1). Those students who ever had practiced sex perceived themselves less frequently at low risk for acquiring HIV as compared those who didn’t practice sex while variables like sex, age, educational status, marital status, knowledge on HIV transmission, and ever used VCT were not significantly associated with risk perception to HIV (P > 0.05) (Table 5).
Table 5.
Correlates of risk perception with selected variables among high school students in Debre-berhan Town, January 2010
| Variables | Risk perception | OR (95% CI) | ||
|---|---|---|---|---|
| Low | High | Crude | Adjusted* | |
| Sex | ||||
| Male | 154 | 7 | 0.6 (0.2. 1.9) | 0.6 (0.1, 2.3) |
| Female | 169 | 9 | 1.0 | 1.0 |
| Age | ||||
| 15-19 | 294 | 14 | 0.7 (0.1, 3.1) | 1.0 (0.2, 6.2) |
| 20-24 | 29 | 2 | 1.0 | 1.0 |
| Educational status | ||||
| 9-10 | 226 | 14 | 1.6 (0.4, 5.7) | 1.7 (0.3, 9.2) |
| 11-12 | 97 | 2 | 1.0 | 1.0 |
| Marital status | ||||
| Single | 320 | 14 | 0.2 (0.02, 1.6) | 1.3 (0.1, 17.8) |
| Married | 3 | 2 | 1.0 | 1.0 |
| Knowledge on HIV transmission | ||||
| Yes | 167 | 3 | 2.0 (0.6, 5.7) | 2.0 (0.5, 7.9) |
| No | 156 | 13 | 1.0 | 1.0 |
| Ever practiced sex | ||||
| Yes | 16 | 17 | 0.02 (0.01, 0.07) | 0.02 (0.01, 0.1)** |
| No | 307 | 2 | 1.0 | 1.0 |
| Ever used VCT | ||||
| Yes | 124 | 6 | 0.9 (0.3, 2.6) | 1.1 (0.3, 4.1) |
| No | 199 | 10 | 1.0 | 1.0 |
NB**=significant (P<0.05).
Adjusted*: for sex, age, educational status, marital status, knowledge of HIV transmission, ever practiced sex, ever used VCT.
Sexual behavior of students
Thirty (8.8%) of the respondents had sexual experience. Out of which, 16 (4.7%) were females and the rest 14 (4.1%) were males. Age at first sexual contact ranged from 15 up to 19 years. The mean age of first sexual contact was being 16.4 (SD = 2.0) in years. With regard to protecting oneself from HIV infection, 309 (91.2%) of the students claimed that they were abstaining from sex, 13 (3.8%) of them were using condoms for HIV protection (Table 6).
Table 6.
Sexual history profile of high school students in Debre-berhan Town, January 2010
| Variables | M (%) | F (%) | Total (%) |
|---|---|---|---|
| Ever practiced sex | |||
| Yes | 17 (5) | 13 (3.8) | 30 (8.8) |
| No | 144 (42.5) | 165 (48.7) | 309 (91.2) |
| Had multiple sexual contact within 6 months | |||
| Yes | 10 (2.9) | 2 (0.6) | 12 (3.5) |
| No | 151 (44.5) | 176 (52.1) | 327 (95.6) |
| Methods of HIV protection | |||
| Abstain | 144 (42.5) | 165 (48.7) | 309 (91.2) |
| Use condom | 11 (3.2) | 2 (0.6) | 13 (3.8) |
| Faithful to partner | 6 (1.8) | 6 (1.8) | 12 (3.6) |
NB: Percents will not add up to 100, as multiple responses are possible.
Two hundred and forty-three (71.7%) of students revealed that they had not regular friend while 96 (28.3%) reported that they had. Out of those who had regular friend, 15 (4.4%) of respondents claimed that they had sex with their friend and the rest 81 (23.9%) of respondents haven’t had sex. The main reasons cited by the students for not having sex with regular friend were decision not to do it before marriage 53 (15.6%), decision not to do it before HIV test 18 (5.3%), to avoid pregnancy 7 (2.1%) and to prevent oneself from sexually transmitted infection (STI) 3 (0.9%).
Out of those who responded to have had previous history of sexual contact, 5 (16.7%) of males and 7 (23.3%) of females had multiple sexual contact during the last six month. Out of those who had multiple sexual contact, 3 (25%) of them said that they had sexual contact with more than four partners during the same period. The main reasons cited by students for having multiple sexual partners include due to sexual desire, 9 (75%); due to cultural reason, 1 (8.3%); and due to seeking to have more children1 (8.3%); and economic reasons 1 (8.3%).
Variables such as sex, age, educational level, knowledge on HIV transmission, and willingness to use VCT did not show significant association (P > 0.05) with ever practiced sex, where as risk perception showed significant association (P < 0.05) with ever practiced sex which was a negative association. Those students who perceived themselves at low risk were less frequently engaged in sexual practice than those students who perceived themselves at high risk (AOR (95% CI) =0.02(0.001, 0.1) (Table 7).
Table 7.
Correlates of sexual behavior with selected variables among high school students in Debre-berhan Town, January 2010
| Variables | Ever practiced sex | OR (95% CI) | ||
|---|---|---|---|---|
| Yes | No | Crude | Adjusted* | |
| Sex | ||||
| Male | 17 | 144 | 0.8 (0.4, 1.6) | 0.9 (0.4, 2.1) |
| Female | 13 | 165 | 1.0 | 1.0 |
| Age | ||||
| 15-19 | 23 | 285 | 0.4 (0.2, 1.1) | 0.4 (0.1, 1.3) |
| 20-24 | 7 | 24 | 1.0 | 1.0 |
| Educational status | ||||
| 9-10 | 22 | 218 | 1.1 (0.5, 2.4) | 1.3 (0.5, 3.9) |
| 11-12 | 8 | 91 | 1.0 | 1.0 |
| Knowledge on HIV transmission | ||||
| Yes | 10 | 160 | 1.2 (0.6, 2.4) | 1.0 (0.4, 2.5) |
| No | 20 | 149 | 1.0 | 1.0 |
| Risk perception | ||||
| Low | 16 | 307 | 0.02 (0.01, 0.1) | 0 .02 (0.01, 0.1)** |
| High | 14 | 2 | 1.0 | 1.0 |
| Willingness to use VCT | ||||
| Yes | 21 | 269 | 2.0 (1.0, 4.5) | 1.2 (0.4, 3.6) |
| No | 9 | 40 | 1.0 | 1.0 |
NB**=significant (P<0.05).
Adjusted*: for sex, age, educational status, marital status, knowledge on HIV transmission, risk perception, willingness to use VCT.
Knowledge, attitude and practice towards VCT service
All of the respondents reported that they had heard about VCT from different sources. Health professionals were the main source of information to access for the majority 226 (66.7%) of the respondents (Figure 2). When asked whether VCT was necessary or not, 327 (96.5%) of the respondents thought it was necessary. Concerning the preference way of receiving HIV test, majority 286 (84.4%) preferred face-to-face followed by secretive letter 44 (13%).
Figure 2.
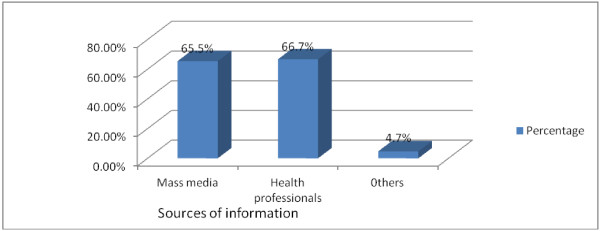
Sources of information for VCT among high school students in Debre-berhan Town, January 2010.
Regarding their history of using VCT, 130 (38.3%) used VCT service, out of whom, male and female accounted for 62 (18.3%) and 68 (20%), respectively (Table 6). Majority of the respondents who had used VCT service responded that their reasons to get tested were for their desire to know their sero-status 124 (36.6%) while 6 (1.8%) did it for marriage purpose. The rest 209(61.7%) of the respondents who do not use VCT claimed that their reasons for not taking part in VCT were never had sex 154 (45.4%), due to fear of having the virus 30 (8.8%) and 2 (0.6%) were due to fear of stigma and discrimination by the society (Figure 3).
Figure 3.
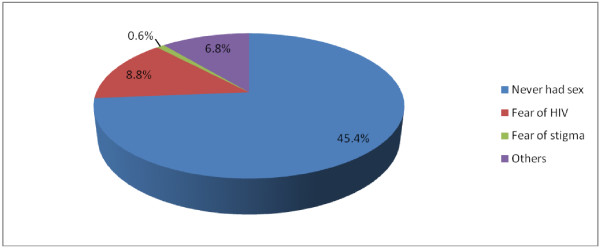
Reasons for not using VCT by percentage among high school students in Debre-berhan Town, January 2010.
Students’ willingness to undertake VCT was assessed. Two hundred-ninety 290 (85.5%) of the respondents responded that they were willing while the rest 49 (14.5%) were not (Table 8). Discrepancies had been observed among the respondents’ knowledge and their practices. Forty-two (12.4%) of those who felt VCT is necessary were not willing to use VCT service. Similarly, of those respondents who believed VCT is necessary, 200 (59%) did not actually use VCT service.
Table 8.
Knowledge, attitude and practice of Debre-berhan high school students towards VCT, January 2010
| Variables | M (%) | F (%) | Total (%) |
|---|---|---|---|
| Heard of VCT | |||
| Yes | 161 (47.5) | 178 (52.5) | 339 (100) |
| No | ------- | ------- | ------- |
| Feel that VCT necessary | |||
| Yes | 155 (45.7) | 172 (50.7) | 327 (96.4) |
| No | 6 (1.8) | 6 (1.8) | 12 (3.6) |
| Willingness to use VCT service | |||
| Yes | 139 (41) | 151 (44.5) | 290 (85.5) |
| No | 22 (6.5) | 27 (7.8) | 49 (14.5) |
| Used VCT service | |||
| Yes | 61 (18) | 69 (20.4) | 130 (38.4) |
| No | 100 (29.4) | 109 (32.2) | 209 (61.6) |
| Availability of VCT service in the vicinity | |||
| Yes | 131 (38.6) | 152 (44.8) | 283 (83.5) |
| No | 30 (8.8) | 26 (7.7) | 56 (16.5) |
NB: Percents will not add up to 100, as eight students failed to answer above variables.
With regard to timing for testing, majority of the students 292 (86.1%) said that one should undergo VCT at any time, 22 (6.5%) agreed just before marriage, 14 (4.1%) thought when an individual having many sex partner, and 7 (2.1%) thought when an individual falls ill. Students’ belief towards provision of safety for other by having HIV test was also assessed. Two hundred seventy-three (80.5%) of respondents agreed that HIV test provide safety for other while 66 (19.5%) of them disagreed. Moreover, 99 (29.2%) of respondents who had used VCT believed that HIV test helps in alleviating anxiety and the rest 31 (9.1%) disagreed.
Availability of VCT service in the vicinity of students’ was also assessed. Two hundred eighty- three (83.5%) of respondents claimed that they could access VCT service in their nearby area where as 56 (16.5%) of them responded that they could not access the service (Table 8). Condom use was strongly correlated and significantly associated with ever used VCT (AOR (95% CI) =4.5 (1.1, 23.3) which was a positive association. Those students who used condom are more likely to be tested for HIV as compared to those who didn’t use (P < 0.05) (Table 9).
Table 9.
Association of socio-demographic variable and practice with ever VCT service use among high school students in Debre-berhan Town, January 2010
| Variables | Ever used VCT | OR (95% CI) | ||
|---|---|---|---|---|
| Yes | No | Crude | Adjusted* | |
| Age | ||||
| 15-19 | 114 | 194 | 0.6 (0.3, 1.3) | 0.6 (0.3, 1.3) |
| 20-24 | 16 | 15 | 1.0 | 1.0 |
| Sex | ||||
| Male | 61 | 100 | 1.1 (0.7, 1.7) | 1.1 (0.7, 1.8) |
| Female | 89 | 109 | 1.0 | 1.0 |
| Marital status | ||||
| Single | 124 | 208 | 0.2 (0.02, 1.5) | 0.1 (0.01, 1.5) |
| Married | 4 | 1 | 1.0 | 1.0 |
| Educational status | ||||
| 9 - 10 | 93 | 147 | 1.1 (0.7, 1.8) | 1.2 (0.7, 2.1) |
| 11-12 | 37 | 62 | 1.0 | 1.0 |
| Ever had sex | ||||
| Yes | 15 | 15 | 0.7 (0.4, 1.5) | 2.2 (0.5, 9.0) |
| No | 115 | 194 | 1.0 | 1.0 |
| Condom use | ||||
| Yes | 6 | 7 | 2.3 (0.8, 6.1) | 4.5 (1.1, 23.3)** |
| No | 134 | 192 | 1.0 | 1.0 |
| Risk perception | ||||
| Low | 124 | 199 | 0.9 (0.3, 2.6) | 1.0 (0.3, 4.02) |
| High | 6 | 10 | 1.0 | 1.0 |
NB** = significant (P<0.05).
Adjusted*: for age, sex, marital status, education, ever practiced sex, condom use and risk perception.
Discussion
All students had heard about HIV/AIDS, its transmission and prevention which was similar to the findings of a study carried out in Nigeria [5, 13]. However, this level of awareness did not necessarily reflect the understanding of how HIV can be transmitted or prevented. Even though students were well informed about HIV, there was knowledge gap on transmission and protective practice. In this study, only 170 (50.1%) could mention all possible ways of HIV transmission and only 30 (8.8%) could identify all possible methods of protecting themselves against HIV infection. This low level of knowledge could predispose these young people to HIV infection.
In this study, 30 (8.8%) of the respondents (14 (4.1%) males and 16 (4.7%) females) had sexual experience which was a bit lower as compared to other study in Ethiopia where 33.3% of students reported that they had sexual intercourse for the first time with the mean age of 15.3 years [14]. Another study conducted on determining perception risk for HIV among adolescent in Uganda showed that 52.2% of boys and 48.8% of girls had sexual experience with the mean age of sexual commencement being 17 years [15]. These might be explained due to the fact that students might not tell the truth because of the sensitivity of the issue in the context of culture of society or might be associated with students’ determination of abstaining from sex as a means of prevention for HIV.
Among students who had sex, 13 (43.3%) were using condoms for HIV protection. This was lower condom use rate as compared to other findings elsewhere, which puts the students at high risk of acquiring sexually transmitted including HIV/AIDS. A study conducted on high risk sexual behavior among youth in Tanzania revealed that 49% of youth reported to have used condom [16]. Another study done among youth in Addis Ababa indicated that condom use rate was found to be up to 48% [6]. But, the finding was comparable to behavioral surveillance survey (BSS) report in Ethiopia [8] which showed that among in-school students who reported to have had sex, 43.1% of them had used condom.
These findings showed that there was still a gap of knowledge in the preventive methods of HIV. This low level of condom usage might indicate that the students might not easily get access to condom due to unavailability of service provider in nearby area or might have embarrassed to go and ask for condom or might be related to the expense of condom.
Majority of students 323 (95.3%) perceived themselves of being at low risk of getting HIV. A similar study in Northwest Ethiopia revealed that only 18.6% of students felt that they could have a high chance for acquiring HIV [17]. Another study which was done in Cape Town revealed that the majority of the youth perceived themselves as being at a little or no risk of HIV infection [18]. The reasons for such low risk perception among students could be that students may underestimate risks in general because of feeling of invulnerability; and that HIV is highly stigmatized by the community so that accepting the risk leads to the possibility of being isolated there by preventing to believe their own personal risk.
All of the study participants (100%) heard the existence of VCT service from different sources. However, only 130 (38.3%) of the study participants (62 (18.2%) males and 68 (20.1%) females) ever used VCT. Although there was apparent discrepancy between awareness and use of VCT service among the study participants, the findings were higher than 9.3% which was reported by BSS in 2005 [8], for VCT use among in-school youth. This showed an increment in the acceptance of VCT as preventive measure. The reason for this improvement could be either positive behavioral changes or expansion of VCT service in the country in the last few years.
The existence of 49 (14.5%) of unwilling students to use VCT service showed the importance of continuing advocacy activities that promote its use. Abstaining from sex, fear of being positive for the test and fear of stigma and discrimination by community were important factors mentioned by the students to refrain them from using VCT service. A study in Botswana also identified fear of the virus, lack of service and stigma associated with HIV/AIDS as key factors in reducing the uptake of VCT services among young students [4].
The study revealed that the perception of being at risk and utilization of VCT were inversely associated. Significant number of students who perceived themselves at low risk for HIV infection had utilized VCT service compared to those who considered themselves to be at higher risk. Similarly, a significant number of those students who did not have sexual contact used HIV test better than those who had sexual experience. This finding was similar to the one obtained on risk perception of HIV infection and VCT utilization among Nigerian youth, which showed that low level of using VCT service was accompanied by high perception risk of infection among adolescents [5]. The result was also true in BSS report [8], which revealed that those students who perceived themselves to be at no or low risk of HIV infection were also more likely to be tested than those who perceive at high risk. This might be due to the fact that they were afraid that their test result could be HIV positive for they could have been engaged in unprotected sexual intercourse.
Conclusions
All students had heard about HIV/AIDS, but misconceptions existed regarding HIV transmission and prevention. Students were engaged in unprotected sexual intercourse which was indicated by low condom use. The perception of majority of the students towards acquisition of HIV was low. Some of students thought that VCT was not necessary even though their knowledge about the benefit of VCT was high. In general, majority of students were willing to use VCT service except for some discouraging factors they mentioned such as fear of stigma, fear of being positive for the test and a misconception that use of VCT is unnecessary if a person is abstaining from sex. It would be advisable to include topics on HIV/AIDS in the school’s curriculum to update the knowledge of students as well as teachers. It is also important to integrate VCT service to anti-AIDS club in schools which assists in making the service to be expanded and easily accessible for students. Information, education and communication program to advocate the benefit of VCT and reduce fear of stigma and discrimination should be strengthened. Improving the existing health institution to provide youth-friendly sexual counseling services including VCT for HIV is also strongly recommended.
Limitations of the study
In the study, the authors used quantitative data for analysis, but it lacked qualitative data which were helpful in substantiating quantitative findings. At the same time, the questionnaire contained culturally sensitive inquiry for the respondents in the study area, for example, about their sexual behavior which might influence the students to provide biased information. Non-respondent rates were not totally avoidable from the study. Moreover, the number of schools which were involved in the study was minimal. Therefore, the findings might be affected in terms of generalizability.
Acknowledgements
We would like to express our deep gratitude and appreciation to staff members of Aklilu Lemma Institute of Pathobiology, AAU and staff members of the two high schools in Debre-berhan Town, who helped in designing and commenting the study. The willingness of the study participants is highly appreciated, as well.
Funding
The research was fully funded by Aklilu Lemma Institute of Pathobiology, Addis Ababa University.
Abbreviations
- AAU
Addis Ababa University
- AIDS
Acquired Immuno Deficiency Syndrome
- AOR
Adjusted Odds Ratio
- ART
Anti Retroviral Treatment
- BSS
Behavioral Surveillance Survey
- CI
Confidence Interval
- EDHS
Ethiopian Demographic Health Survey
- HCT
HIV Counseling and Testing
- HIV
Human Immunodeficiency Virus
- SD
Standard Deviation
- SPSS
Statistical Package for Social Science
- STI
Sexually Transmitted Infection
- VCT
Voluntary Counseling and Testing for HIV.
Footnotes
Competing interests
The authors declare that they have no any competing interests.
Authors’ contribution
SS conceived the idea; GM and SS designed the study; SS collected the data in the field and drafted the manuscript; WE supervised the overall conduct of the study and SS, GM and WE interpreted the results; SS and DW drafted the manuscript for publication. All authors participated in the write up, read and approved the final manuscript.
Contributor Information
Solomon Sisay, Email: solomon.sisay@gmail.com.
Woldaregay Erku, Email: woldaregay_e@yahoo.com.
Girmay Medhin, Email: gtmedhin@yahoo.com.
Desalegn Woldeyohannes, Email: desalegn01@gmail.com.
References
- 1.UNAIDS . Global report on HIV/AIDS epidemic. 2013. [Google Scholar]
- 2.Iliyasu Z, Abubakar IS, Kabir M, Aliyu MH. Knowledge of HIV/AIDS and attitude towards voluntary counseling and testing among adults. J Natl Med Assoc. 2006;98(12):1917–1922. [PMC free article] [PubMed] [Google Scholar]
- 3.Tan X, Pan J, Zhou D, Wang C, Xie C. HIV/AIDS knowledge, attitudes, and behaviors assessment of Chinese students: a questionnaire study. Int J Environ Res Public Health. 2007;3(4):248–253. doi: 10.3390/ijerph2007030009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Majelantle RG, Keetile M, Bainame K, Nkawana P. Knowledge, opinions and attitudes towards HIV and AIDS among Youth in Botswana. J Glob Econ. 2014;2(1):1–7. [Google Scholar]
- 5.Oshi SN, Ezugwu FO, Oshi DC. Does self perception of risk of HIV infection make the youth to reduce risky behavior and seek voluntary counseling and testing services: a case study of Nigerian youth. J Soc Sci. 2007;14(2):195–203. [Google Scholar]
- 6.Gatta AA, Tshweneagae GT: Knowledge of, and attitudes towards voluntary HIV counseling and testing services amongst adolescent high school students in Addis Ababa, Ethiopia.J Demo Nur Org S Afri 2012.,35(1): [DOI] [PubMed]
- 7.Bwambale FM, Ssali SN, Byaruhanga S, Kalyango JN, Karamagi CAS. Voluntary HIV counseling and testing among men in rural Western Uganda: An implication for HIV prevention. BMC Public Health. 2008;8(1):263. doi: 10.1186/1471-2458-8-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.HIV/AIDS Behavioral Surveillance Survey (BSS). Round Two. Ethiopia; 2005. document/BSS/2
- 9.CSA . Ethiopian Demographic Health Survey (EDHS) Ethiopia: Addis Ababa; 2011. [Google Scholar]
- 10.Alemu S, Abseno N, Degu G, Wondmikun Y, Amsalu S. Knowlegde and attitude towards voluntary counseling and testing for HIV: A community based study in North West Ethiopia. Ethiop J Health Dev. 2004;18(2):82–89. [Google Scholar]
- 11.CSA . The 2007 population and housing census result of Ethiopia. Ethiopia: Addis Ababa; 2008. [Google Scholar]
- 12.Abebe A, Mitikie G. Perception of high school students towards voluntary HIV counseling and testing using health belief model in Butajiera (SNNPR) Ethiop J Health Dev. 2009;23(2):148–153. [Google Scholar]
- 13.Wodi BE. HIV/AIDS knowledge, attitudes, and opinions among adolescents in the River States of Nigeria. Int Electron J Health Educ. 2005;8(1):86–94. [Google Scholar]
- 14.Adamu R, Samuel M, Inguidushet S. Pattern and correlate of sexual initiation, sexual risk behavior and condom use among secondary school students in Ethiopia. Ethiop Med J. 2003;41(2):163–177. [PubMed] [Google Scholar]
- 15.Kibombo R, Neema S, Ahmed FH. Perception of risk to HIV infection among adolescents in Uganda: Are they related to sexual behavior? J Afric Repr Health. 2007;11(3):168–181. doi: 10.2307/25549738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lema LA, katapa RS, Musa AS. Knowledge on HIV/AIDS and sexual behavior among youths in Kibaha District, Tanzania. Tanzan J Health Res. 2008;10(2):79–83. doi: 10.4314/thrb.v10i2.14321. [DOI] [PubMed] [Google Scholar]
- 17.Fitaw Y, Worku A. High risk sexual behavior and pattern of condom utilization of Gondar collage of medical sciences students, North West Ethiopia. Ethiop J Health Dev. 2002;16(3):335–338. doi: 10.4314/ejhd.v16i3.9801. [DOI] [Google Scholar]
- 18.Anderson KG, Beutel AM, Brown BM. HIV risk perceptions and first sexual intercourse among youth in Cape Town, South Africa. Int Fam Plan Perspect. 2007;33(3):98–105. doi: 10.1363/3309807. [DOI] [PubMed] [Google Scholar]


