Abstract
Objective: Results following anterior cervical discectomy (ACD) without fusion are not well reported because of skepticism that the disturbed cervical spine anatomy after ACD might compromise clinical outcome. The purpose of this study was to determine whether ACD without fusion prompts the degenerative process significantly, and whether it is necessary to preserve disc height and cervical alignment for the sake of better clinical outcome following cervical spine surgery. Background data: Out of 56 consecutive patients, 37 patients who replied and consequently underwent postoperative MRI from April to June 2009 were included in this study. Material and methods: A total of 37 consecutive patients diagnosed as having cervical monoradiculopathy and treated with percutaneous endoscopic cervical discectomy (PECD) were investigated. Angle of cervical lordosis, change in cervical range of motion, disc height change, and degree of degenerative changes at the corresponding level were evaluated. The visual analogue scale (VAS) score for neck and arm pain and the neck disability index (NDI) were compared preoperatively and at the final follow-up. The mean follow-up period was 45.5 months. Results: Despite prompted radiological deterioration such as loss of disc height (the posterior disc heights and central disc height ratio were significantly decreased from 3.6 to 2.6 mm, from 30.3% to 24.5%, respectively, p<0.05) or degenerative progression (from average grade of 2.8 to 4.1, p<0.05), the patients achieved significant improvement in clinical outcomes (VAS for neck and arm dropped from mean 6.3 and 7.5 to 2.7 and 2.6, respectively, and NDI score improved from 46.8% to 17.2%, p<0.05) after PECD. Conclusions: Neither loss of disc height nor progression of degeneration at disc space compromised clinical outcome after PECD without fusion on long-term follow-up.
Introduction
Anterior cervical discectomy techniques are commonly used in the treatment of cervical spondylotic radiculopathy, and the majority of spine surgeons advocate the use of an autogenous allograft, or even an artificial disc, upon the completion of decompression. This reconstruction of the cervical spine would be based on the theory that the disrupted ventral cervical anatomy combined with empty disc space after decompression would naturally collapse in a kyphotic manner when left alone, leading to a postoperative axial neck pain associated with distorted cervical alignment or delayed radicular pain with the compromise of the neural foramen.1 Over the past decade, there was a lack of controversy about this procedure, and a majority of surgeons did not hesitate to insert a graft or spacer into this surgically disturbed cervical spine based on this vague theory.
There has been little research on the outcome after ACD without fusion, because of skepticism about the disturbance of the cervical spine anatomy after surgery, which was thought to compromise the clinical outcome. Therefore, there has been a consequent paucity of previous literature.2–6
However, after careful selection of the patients with isolated cervical soft disc herniation or focal osteophyte formation without instability, subluxation, malalignment, or loss of normal cervical lordosis, the number of the patients who were required to undergo a delayed fusion procedure could be reduced to less than<1.5%.7 With these promising results from the literatures and the evolution of endoscopic and instrumental technology, we have pursued direct removal of disc pathology through percutaneous endoscopic cervical discectomy (PECD) for patients who have met the inclusion criteria, leaving the majority of the anterior and central disc, anterior longitudinal ligament, and both upper and lower vertebral end plates intact. Our theory would be that this selective evacuation of the intervertebral disc space without fusion might maximize the possibility to reduce of reducing the damage to the surrounding tissue and to dispense dispensing with bony or ligament resection, deterring the development of subsequent instability or malalignment while minimizing e fusion surgery-related complications.86
However, despite these delicate and selective removals of cervical pathology in nonfusion style for the sake of maintenance of the original cervical spine construction, the progression of degenerative changes would be inevitable, as noted by the fact that most experimental degenerative animal models involve only needle puncture, and from the frustrating results from human series that there is a threefold increase in risk of developing adjacent level disc degeneration in incorrectly needle-marked discs after anterior cervical discectomy and fusion (ACDF) at short-term follow-up.9
Based on regarding the effects of disturbed cervical anatomy on the clinical outcome, the purpose of this study was to identify if PECD without fusion would significantly accelerate the degenerative process, and if disc height and cervical alignment should be preserved, in terms of the clinical outcome after surgery.
Materials and Methods
A total of 37 consecutive patients who had monoradiculopathy caused by soft cervical disc herniations, and who had been treated with PECD using a WSH endoscope system (Karl-Storz, Tuttlingen, Germany) from September 2003 to February 2007, were included in this study. the inclusion criteria was summarized as follows: (1) intractable neck pain or cervical radiculopathy unresponsive to conservative management over 12 weeks, (2) localized monosegmental contained or noncontained soft disc herniation demonstrated on computed tomography (CT) scan or magnetic resonance image (MRI), (3) the problem occurring from C3-4 to C6-7 levels, (4) preservation of at least 4 mm of posterior disc height, and (5) no past history of cervical surgery.8 Those patients who had calcified disc; sequestered fragments; evidence of myelopathic features; central canal stenosis with broad-based bulging; foraminal stenosis without disc herniation, segmental instability, or deformity; or previous neck surgery history were excluded. PECD without fusion was performed on 1 patient at C3-4, on 8 at C4-5, on 19 at C5-6, and on 9 at C6-7 levels.
The changes in clinical outcomes measured by visual analogue scale (VAS) score for neck and arm pain, and the neck disability index (NDI) were compared preoperatively and at the final follow-up visit.
The radiographic evaluation was performed using PiView medical imaging software (Mediface, Seoul, Korea). The change in posterior disc heights was measured by absolute value at the midvertebral level on T2-weighted MRI. The disc height index, which is the ratio of the disc height to the sagittal diameter of the overlying vertebral body from anterior to the posterior body margin, was also calculated from the midvertebral level by Inoue method.14 The changes of MR grades of disc degeneration10 (Table 1) were assessed using grading system by Miyazaki et al.10 on the midsagittal T2-weighted MRI. The overall sagittal alignment and regional Cobb's angle were determined by measuring the angle formed by the tangential lines drawn parallel to the lower end plates between C2-7 and adjacent vertebral bodies at the treated level, respectively. The regional range of motion was measured by angle formed from the line drawn along the one edge of the overlying image of extension on the underlying image of flexion. A serial exact superimposition of the two cervical vertebral bodies and spinous processes adjacent to the level under investigation from the two images representing the cervical spine in the end positions of the flexion/extension was required to follow the Penning method.11 For comparison, all 37 patients had their final follow-up radiograph and MRI examination between April and June 2009. The sex ratio was 20:17 (M:F) and the mean follow-up period was 45.5 months.
Table 1.
Grading System for Cervical Intervertebral Disc Degeneration
| Grade | Nucleus signal intensity | Nucleus structure | Distinction of nucleus and annulus | Disc height |
|---|---|---|---|---|
| I | Hyperintense | Homogenous, white | Clear | Normal |
| II | Hyperintense | Inhomogenous with horizontal band, white | Clear | Normal |
| III | Intermediate | Inhomogenous, gray to black | Unclear | Normal to decreased |
| IV | Hypointense | Inhomogenous, gray to black | Lost | Normal to decreased |
| V | Hypointense | Inhomogenous, gray to black | Lost | Collapsed |
Surgical procedure
The patient is placed in a supine position with the neck mildly extended on a radiolucent table. A plastic hood over the face enables communication with the anesthesiologist. The C-arm of the fluoroscope is put in front and then in profile, and the level of the operation is carefully marked on the skin with a felt pen using a metallic instrument. The operation is typically conducted with the patient under local anesthesia and analgesia by neuroleptics, so that the surgeons can be immediately aware of any changes in the patient's symptoms and signs. General anesthesia may be used in a few patients who want it or who cannot tolerate the position, but with general anesthesia, the urgent need for conversion to open surgery may not be detected early. A solution of 1% lidocaine is usually used to infiltrate the skin and subcutaneous tissue.
Usually, a paramedian approach (2–5 mm from the anterior midline) from the contralateral side is chosen. The surgeon gently pushes the trachea or larynx toward the opposite side with the index and middle finger, then applies a firm pressure in the space between the sternocleidomastoid muscle and trachea and points toward the vertebral surface until the prominence of the anterior edge of the disc can be palpated (Fig. 1). The trachea and larynx are displaced medially and the carotid pulsation is palpated on the lateral side. The 18-gauge puncture needle is then inserted through the space between the tracheoesophagus and the carotid artery. After the surgeon confirms the midline position of this 18-gauge needle on the center of the anterior annulus by intraoperative fluoroscopy, the needle is advanced close to the posterior body line of the posterior disc space (Fig. 2). Then a discography with 10 mL Telebrix (Guerbert, France) and indigo carmine (Korean United Pharma, Seoul, Korea) is performed to confirm the presence of soft disc herniation and also to stain the nucleus into blue in contrast with the neural tissue (Fig. 3). Up to 0.5 mL of contrast media is injected to specify the posterior part of the disc. Then a guide wire is inserted to replace the puncture needle, and a 3–5 mm skin incision is made to allow the passage of serial progressive dilator (2–5 mm) along the guide wire to stretch the soft tissues. Finally, the tip of the working cannula is hammered to reach the posterior part of the disc (Fig. 4), and the forceps should reach to the end of the posterior margin to remove the herniated mass effectively, without injuring the spinal cord.
FIG. 1.
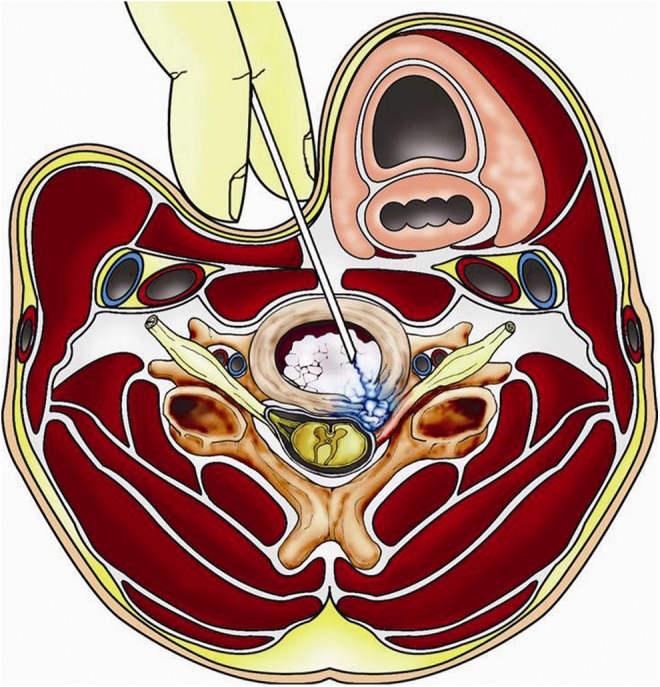
Safe needle insertion into the created space during percutaneous endoscopic cervical discectomy (PECD). The surgeon gently pushes the trachea or larynx toward the opposite side with the index and middle finger, then applies firm pressure in the space between the sternocleidomastoid muscle and trachea and points toward the vertebral surface until the prominence of the anterior edge of the disc can be palpated.
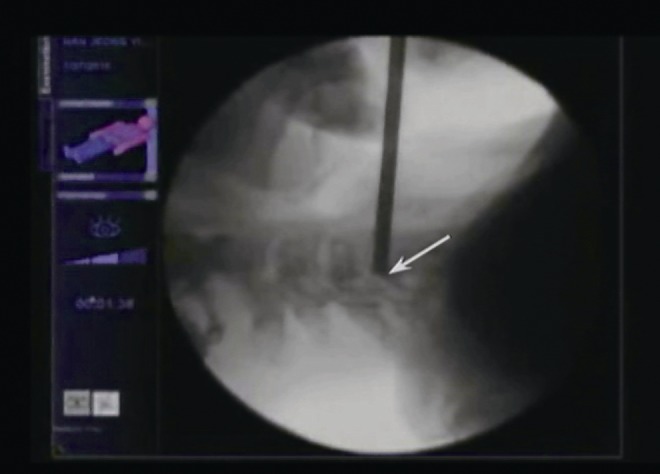
FIG. 2.
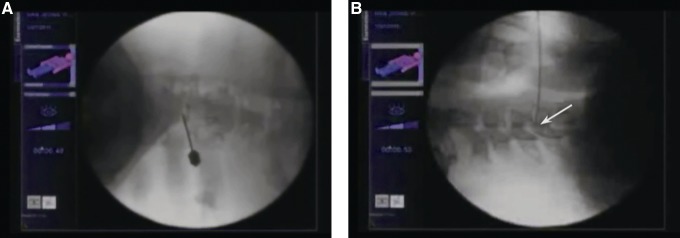
An intraoperative C-arm fluoroscopic (A) anteroposterior (AP) and (B) lateral view after the needle insertion. After confirming the midline position of this 18-gauge needle in the center of the anterior annulus, the needle is advanced close to posterior body line of the posterior disc space.
FIG. 3.
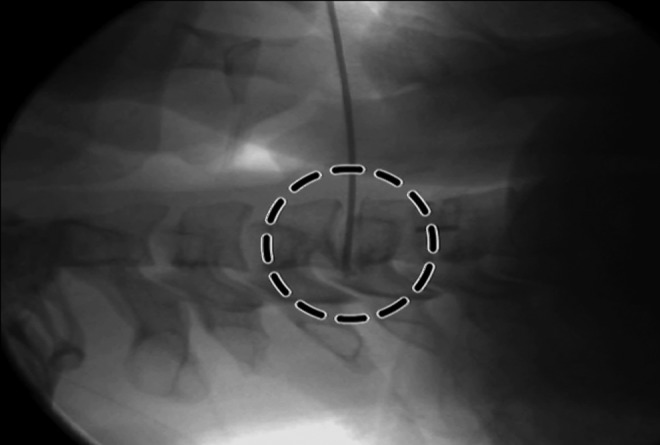
A lateral intraoperative fluoroscopic view after discography using indigo carmine. Advancement of the needle close to the posterior body line is important to properly stain the actual herniated disc fragment (dotted circle).
FIG. 4.
An intraoperative C-arm fluoroscopic lateral view after the working sheath insertion.
The initial discographic images indicate the depth required for the small disc forceps to remove the herniated fragments close to the posterior longitudinal ligament. With the surgeon closely monitoring with the fluoroscopy and direct endoscopic vision, the annular anchorage is loosened with a side firing laser and small forceps. Extraction of the tail of the herniated mass, which is usually more fibrotic and collagenous, is attempted. The intradiscal space is rinsed continuously with cefazolin-mixed saline through an irrigation channel.
Endoscopic vision helps in confirming the adequacy of decompression of the dural sac or the exiting nerve root (Figs. 5 and 6). A single stitch with moderate localized pressure to control the bleeding completes the procedure. The patients are observed for 3–24 h in the hospital, and then discharged with the cervical region braced with a Miami-Jackson collar for 3–14 days postoperatively. Rehabilitation exercises are usually started 4–6 weeks after the surgery.
FIG. 5.
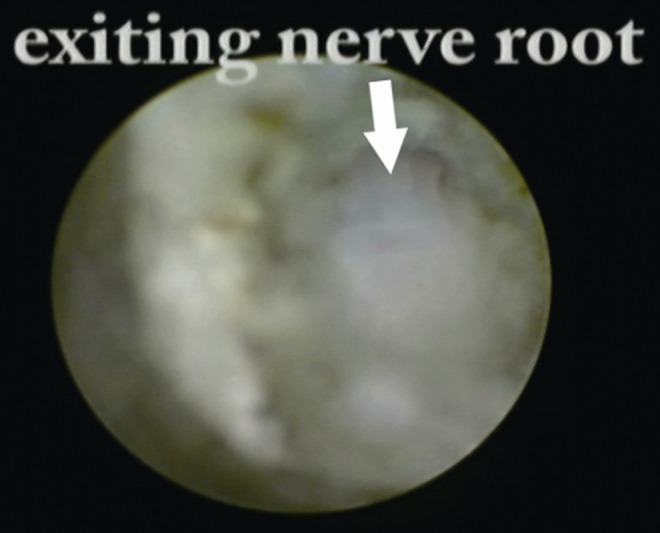
An intraoperative endoscopic view of the final phase of procedure during percutaneous endoscopic cervical discectomy (PECD). The lateral margin of dura and its exiting nerve root is well exposed after full decompression.
FIG. 6.
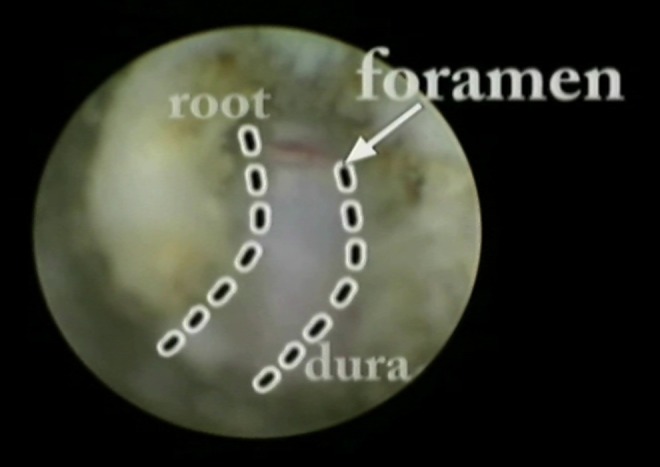
An intraoperative endoscopic view of the final phase of procedure during percutaneous endoscopic cervical discectomy (PECD). Well decompressed ventral dura from midline to the start of the foramen is exposed.
Statistical analysis
An independent two sample t test and a Wilcoxon rank sum test were performed to evaluate the amount of changes that had occurred from index point to the final follow-up.
Results
PECD without fusion promoted the degenerative process at the operated cervical disc level, as shown in the radiological results. The posterior disc heights and central disc height ratio were significantly decreased (3.6–2.6 mm, 30.3–24.5%, respectively, p<0.05) and the degenerative grades were significantly aggravated (average grade of 2.8–4.1, p<0.05) (Fig. 7). However, the overall sagittal alignment was significantly improved (8.5o–11.7o, p<0.05) and the regional Cobb's angle or range of motion was well maintained (1.9°–2.3°, 6.0°–5.0°, respectively, p>0.05).
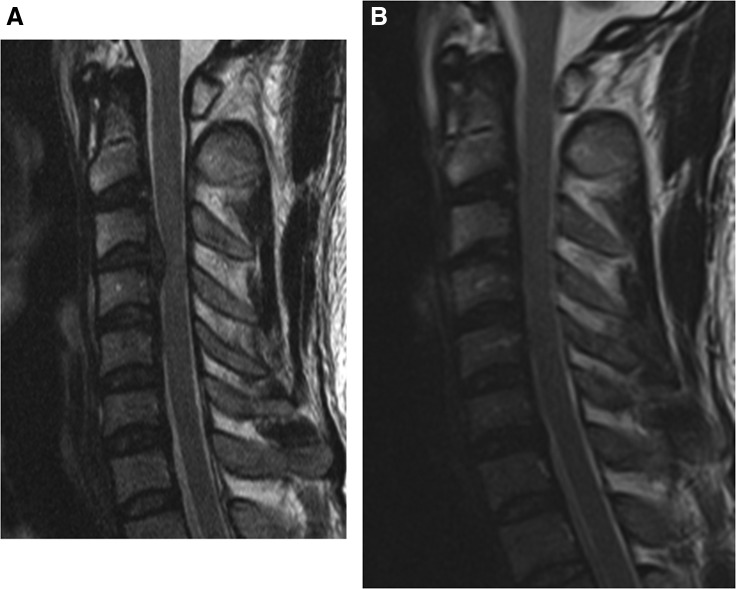
FIG. 7.
Radiographic changes as demonstrated by T2-weighted sagittal MRI comparison between preoperative (A) and postoperative 57 months (B). Note that the degenerative process within C3-4 disc level has aggravated from Miyazaki grade II to grade IV upon final follow-up after the performance of percutaneous endoscopic cervical discectomy (PECD).
There were no radiological changes with any deleterious effect on the clinical outcomes, as the VAS for neck and arm dropped from mean 6.3 and 7.5 to 2.7 and 2.6, respectively, and NDI score improved from 46.8% to 17.2% after PECD (p<0.05). There were four patients with recurrence or development of progressive kyphosis, who underwent ACDF consequently. There was no intraoperative complication such as iatrogenic neurological deficit or cerebrospinal fluid (CSF) leakage caused by dural tear.
Discussion
Most spinal surgeons skilled with ACD introduce a bone graft or cage into the empty disc space after decompression procedure is completed, and over the past decades, it has been difficult to argue against such success of ACDF as one of the gold standards. As most surgeons have good theoretical reasons to believe that the disturbed cervical spine anatomy or alignment may compromise the clinical outcome, there have been extravagant hardware usages in most of the ACD procedures.
A well-designed prospective randomized study comparing ACD without graft or artificial disc with ACD with graft or spacer could be a best answer to this issue of the correlation between the preservation of cervical spine anatomy and the clinical outcome after surgery. Although this series involves the longest clinical and radiological results regarding ACD without fusion based on the average 4-year follow-up, there is still a limitation that it is designed in retrospective fashion, which means downgrading levels of evidence.
There have been four prospective randomized studies that have addressed this issue.2,3,5,6 However, these studies are all compromised by important methodological flaws, which seriously limit their value. None of the trials were empowered to determine a proper sample size, and none of the end-points and outcome measures had been validated. The follow-up period was too short to allow any conclusions to be drawn about the long-term effects of the two procedures. Despite their shortcomings, these four randomized studies provided the best evidence to date about the relative merits of introducing a bone graft or spacer following cervical discectomy. None of the studies found any statistically significant difference in clinical outcome between the ACD alone group and ACDF group and also reported minor advantages in outcome in favor of ACD group. Haden et al.1 provided prospective, objective, and validated clinical data in which they investigated the relationships among loss of disc height, cervical spine alignment, and clinical outcome in 140 patients undergoing ACD without interbody graft or cage during the 1-year follow-up period. Half of their series demonstrated that loss of disc height or disturbance of alignment could lead to a segmental kyphosis and prominently, subjects with good preservation of disc height or cervical alignment could eventually experience loss of disc height and disturbance of cervical alignment.1,4 However, they have not found any correlation between loss of disc height and clinical outcome.
Most recently, several reports using larger retrospective series based on longer follow-up period have been noted. Yang et al.12 compared the therapeutic effectiveness of PECD, percutaneous cervical disc nucleoplasty, and a combination of the two performed on their series of 171 patients with the average of 4.1 years of follow-up. The portion of each group that was rated as clinically successful was>80%, without significant difference among the groups. Notably, there was no impact on the stability of the cervical column in any of the patients, nor was there any difference between the pre- and postoperative stability in each group during follow-up. Deukmedjian et al.13 also recently reported about successful use of Deuk Laser Disc Repair® for 66 consecutive subjects with symptomatic single or two level cervical disc disease. At an average of 3 months of follow-up, their overall clinical success rate was 94.6%.
Although sophisticated surgical treatments for cervical disc herniation have evolved throughout the twentieth century, this evolution is mostly related to the evolution of the nature of the implants that are being inserted into the empty disc space, lacking the evolution related to clarifying the surgical opinions that have existed since the introduction of ACD; including whether or not ACD without fusion prompts the degenerative process and cervical malalignment significantly, and whether or not it is important to preserve disc height and cervical alignment for the sake of clinical outcome following cervical spine surgery.
Because of the paucity in the literature that would answer this question, the authors are not fully empowered with scientific evidence about the relative merits of simple cervical partial discectomy without inserting a bone graft or spacer. Moreover, there has been a recent report of a threefold increase in the risk of developing adjacent level disc degeneration in incorrectly needle-marked discs after ACDF at short-term follow-up, indicating that even minor needle-related trauma contributes to accelerated segmental degeneration.9 These are all discouraging facts for the authors, refraining from justifying or emphasizing the minimal nature of the anterior cervical structures and disc violation using small endoscope for the sake of preserving the cervical stability or alignment even without implant. However, as Hadley and Sonntag suggested,7 after careful selection of the patients with isolated cervical soft disc herniation or focal osteophyte formation without instability, subluxation, malalignment, or loss of normal cervical lordosis, the number of the patients requiring a delayed fusion procedure could be reduced to<1.5%. Every one of the 37 patients in the authors' series demonstrated the promoted degenerative process inside the operated disc level while relatively preserving alignments over an average of a 4-year follow-up span with more improved clinical outcomes. This result is coincides with the most recent assertion from Haden1 that this lack of correlation runs counter to the widely held belief that preservation of disc height is an important surgical objective justifying donor site morbidity or expenditure on spinal implants. It is actually unknown whether preservation of disc height and cervical spine alignment is important to treat cervical disc disorders or not. Presumably, most surgeons are introducing bone graft or spacers into the emptied disc space for a variety of different reasons. However, our series depicts the contrary results; showing the lack of importance of maintaining (or preserving) cervical anatomy with regard to enhancing the consequent clinical outcomes. Moreover, there is a very low morbidity associated with a rapid recovery resulting in a significant savings on expenditure after PECD alone. However, longer follow-up studies based on a large number of series are required to assess the corresponding segment degeneration and stability as feared by most surgeons favoring the conventional fusion surgeries. A better designed comparative study between ACD alone and ACDF could finalize the controversies regarding this issue.
Acknowledgments
This study was supported by a grant from the Wooridul Spine Foundation. This article is approved by Institutional Review Board of Seoul Wooridul Spine Hospital (IRB No: WRDIRB-2013-04-006). The contents and results contained in this article were produced from the work in the Seoul Wooridul Spine Hospital research laboratory.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Haden N., Latimer M., Seeley H.M., and Laing R.J. (2005). Loss of inter-vertebral disc height after anterior cervical discectomy. Br. J. Neurosurg. 19, 469–474 [DOI] [PubMed] [Google Scholar]
- 2.Dowd G.C., and Wirth F.P. (1999). Anterior cervical discectomy: is fusion necessary? J. Neurosurg. 90, 8–12 [DOI] [PubMed] [Google Scholar]
- 3.Martins A. (1976). Anterior cervical discectomy with and without interbody bone graft. J. Neurosurg. 44, 290–295 [DOI] [PubMed] [Google Scholar]
- 4.Pointillart V., Cernier A., Vital J.M., and Senegas J. (1995). Anterior discectomy without interbody fusion for cervical disc herniation. Eur. Spine J. 4, 45–51 [DOI] [PubMed] [Google Scholar]
- 5.Rosenorn J., Hansen E.B., and Rosenorn M.A. (1983). Anterior cervical discectomy with and without fusion. A prospective study. J. Neurosurg. 59, 252–255 [DOI] [PubMed] [Google Scholar]
- 6.Savolainen S., Rinne J., and Hernesniemi J. (1998). A prospective randomized study of anterior single level cervical disc operations with long-term follow-up: surgical fusion is unnecessary. Neurosurgery 43, 51–55 [DOI] [PubMed] [Google Scholar]
- 7.Hadley M.N., and Sonntag V.K. (1993). Cervical disc herniations. The anterior approach to symptomatic interspace pathology. Neurosurg. Clin. N. Am. 4, 45–52 [PubMed] [Google Scholar]
- 8.Lee S.H., Lee J.H., Choi W.C., Jung B., and Mehta R. (2007). Anterior minimally invasive approaches for the cervical spine. Orthop. Clin. North Am. 38, 327–337 [DOI] [PubMed] [Google Scholar]
- 9.Nassr A., Lee J.Y., Bashir R.S., Rihn J.A., Eck J.C., Kang J.D., and Lim M.R. (2009). Does incorrect level needle localization during anterior cervical discectomy and fusion lead to accelerated disc degeneration? Spine 15, 189–192 [DOI] [PubMed] [Google Scholar]
- 10.Miyazaki M., Hong S.W., Yoon S.H., Morishita Y., and Wang J. (2008). Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J. Spinal Disord. Tech. 21, 288–293 [DOI] [PubMed] [Google Scholar]
- 11.Penning L. (1978). Normal movements of the cervical spine. Am. J. Roentgenol. 130, 317–326 [DOI] [PubMed] [Google Scholar]
- 12.Yang B., Xie J., Yin B., Wang L., Fang S., and Wan S. (2014). Treatment of cervical disc herniation through percutaneous minimally invasive techniques. Eur. Spine J. 23, 382–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deukmedjian A.J., Jason Cutright S.T., Augusto Cianciabella P.C., and Deukmedjian A. (2013). Deuk Laser Disc Repair(®) is a safe and effective treatment for symptomatic cervical disc disease. Surg. Neurol. Int. 4, 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inoue H., Ohmori K., Miyasaka K., and Hosoe H. (1999). Radiographic evaluation of the lumbosacral disc height. Skeletal Radiol. 28, 638–643 [DOI] [PubMed] [Google Scholar]