Abstract
Objectives
The study aims to examine whether a higher proportion of current and former smokers reported having an oral cancer screening (OCS) exam in the past year compared with never smokers in Maryland between 2002 and 2008.
Methods
Secondary analysis of the Maryland Cancer Surveys (conducted in 2002, 2004, 2006, and 2008), population-based, random-digit-dial surveys on cancer screening among adults age 40 years and older. Of 20,197 individuals who responded to the surveys, 19,054 answered questions on OCS and smoking. Results are weighted to the Maryland population.
Results
Self-reported OCS in the past year increased from 33 percent in 2002 to 40 percent in 2008. Screening among never and former smokers increased from about 35 percent to 42 percent and from 35 percent to 43 percent, respectively; screening among current smokers remained between 23 percent and 25 percent. In the adjusted analysis, current smokers had decreased odds of screening compared with never smokers; no significant difference was observed between former and never smokers. When the variable dental visit in the last year was included in the adjusted analysis, it became the strongest predictor of OCS.
Conclusions
Between 2002 and 2008, self-reported OCS in the last year increased among former and never smokers, but remained unchanged for current smokers. A visit to a dental professional attenuated the difference in OCS between current and never smokers. Dental visit in the last year was the strongest predictor of OCS.
Keywords: mouth neoplasms, early detection of cancer, smoking
Introduction
Oral cancer (i.e., cancer of the lip, oral cavity, and/or the oropharynx) accounted for approximately 2.5 percent of cancers in the United States in 2011 (1). It is estimated that 39,400 people were diagnosed with oral cavity and pharynx cancer in 2011 and that 7,900 died of this cancer (2). The 5-year relative survival rate for cancer of the oral cavity and pharynx from 1999 to 2006 was only 61 percent, likely due to its late stage at diagnosis (3–5). Five-year survival was highest among persons with localized disease and lower with regional and distant spread. Males are more likely than females to develop oral cancer (2).
Tobacco use in any form is the major risk factor for oral cancer; it is associated with 90 percent of oral cancers in men and 60 percent in women (6). Data from a population-based case-control study suggest that cigarette smokers have two to five times higher risk of oral cancer than nonsmokers, and the risk increases with the numbers of cigarettes smoked and the years smoked (7). Excessive intake of alcohol is the second major risk factor for developing oral cancer (8). Tobacco and alcohol are independent risk factors for developing oral cancer; together they act synergistically (2,6). While oral cancers occur in an area of the body that can be examined by both dental and medical professionals during routine examinations, only 13 percent of adults 40 years and older in the United States reported having had an oral and pharyngeal cancer exam in 1998 (9). One of the objectives of Healthy People (HP) 2010 was to increase the proportion of adults aged 40 years and older who reported having had an examination to detect oral cancer in the last year to 20 percent (10). Increasing the proportion of adults who receive an oral and pharyngeal cancer screening exam from a dentist or dental hygienist in the last year is a developmental objective for HP 2020, and increasing the proportion of oral cancer detected at the earliest stage and reducing the death rate from oropharyngeal cancer are firm objectives for HP 2020 (11).
While the incidence of oral cancer decreased in Maryland between 2003 and 2007, the decrease in mortality that was seen in the late 1990s and early 2000s has plateaued in recent years (12). Beginning in 2002, the state of Maryland conducted a statewide survey every 2 years through 2008 on cancer screening and risk behaviors, including questions on cigarette smoking and oral cancer screening (OCS). Using the Maryland data from 2002, Ling et al. found that after controlling for demographic and health care characteristics, current and former smokers were no more likely than those who had never smoked cigarettes to report ever having had an OCS exam (13). We used data from four survey years to examine the relationship between self-reported OCS within the past year and smoking status and whether this relationship has changed over time.
Methods
The Maryland Cancer Survey, supported with funds from the Cigarette Restitution Fund Program, was administered biennially from 2002 to 2008 to approximately 5,000 respondents in each year (14). It was a population-based, random-digit-dial, statewide telephone survey, using list-assisted disproportionate stratified sampling by geography. Survey participation was limited to adults age 40 years and older who lived in households in Maryland. Excluded from the survey were individuals who were younger than 40 years of age, who did not speak English (except in 2006 when the survey was offered in Spanish by bilingual interviewers), who were unable to communicate due to physical or mental impairment, and who lived in group homes or institutions.
Genesys-Market Systems Group provided a list of approximately 100,000 telephone numbers each survey year. The sample of telephone numbers was stratified by urban and rural area of residence with oversampling of rural areas. REDA International, Inc., a research firm located in Wheaton, MD, conducted the interviews with Maryland residents. Up to 15 calling attempts were made to each of the selected telephone numbers at various times of day and throughout the week. The telephone interview took about 20 minutes and included questions on demographics, the respondent’s cancer screening behavior, health risk factors, and access to health care. The Council of American Survey Research Organizations response rate (defined as the number of completed interviews/known eligible + presumed eligible), was 38.4 percent (2002), 38.3 percent (2004), 39.7 percent (2006), and 40 percent (2008). Methods for the survey are detailed at: http://fha.dhmh.maryland.gov/cancer/SitePages/surv_data-reports.aspx.
Each of the respondent’s answer was given a final survey weight that could be used to generalize the survey results to the Maryland population age 40 years and older. Pre-stratification weighting was based on the sampling probability by geographic region (urban versus rural), residential telephone sampling between the two density strata of phone numbers, the number of adults age 40 years and older in the respondent’s household, and the inverse of the number of residential telephone numbers in each household. Post-stratification weighting was calculated as the number of adults age 40 years and older in an age-race-gender category in the population of the urban or rural region divided by the sum of the pre-stratification weights for the respondents in that same age-race-gender category. Approval for the surveys was received from the institutional review boards at the Maryland Department of Health and Mental Hygiene and the University of Maryland, Baltimore.
Variables
The questionnaire asked, “Have you ever had a test or exam for oral or mouth cancer in which the doctor or dentist pulls on your tongue, sometimes with gauze wrapped around it, and feels under the tongue and inside the cheeks?” Persons who responded “Yes” or “I think so” were identified as having had an OCS exam. Respondents were then asked when their last OCS exam occurred. Those who said the exam was within the past year were considered to have had a recent OCS. Those who reported the exam was 1 or more years in the past, never had the exam, or did not know the time interval since their last exam were considered to not have had a recent OCS exam.
Smoking status was defined using two questions: “Have you smoked at least 100 cigarettes in your entire life?” and “Do you now smoke cigarettes every day, some days, or not at all?” Respondents who smoked 100 or more cigarettes in their life and were currently smoking every day or some days were identified as current smokers. Former smokers reported they had smoked 100 or more cigarettes in their lifetime but do not currently smoke. Never smokers had never smoked or had smoked fewer than 100 cigarettes in their lifetime.
Alcohol consumption was defined based on the amount of alcohol consumed in the 30-day period before the interview and was categorized as no alcohol use, low-risk drinking, and high-risk drinking. High-risk drinking among men was defined as having more than 14 drinks per week or binge drinking (having at least five drinks on at least one occasion). Among women, high-risk drinking was defined as having more than seven drinks per week or binge drinking. Low-risk drinking was defined as consuming some alcohol in the last 30 days, but less than high-risk drinking.
Race was self-reported and categorized for this analysis as white, black/African American, or other. Marital status was categorized into two groups: married or partnered and not married (divorced, separated, widowed, or never married). Education was categorized into four groups: a) less than high school; b) high school graduate; c) some college, technical school, or college graduate; and d) advanced degree.
Data analysis
The associations between each predictor variable (survey year, sex, age, race, marital status, education, health status, and alcohol consumption) and having had an oral cancer exam in the past year and smoking status were evaluated by the Rao Scott chi-square statistic. None of the predictor variables were found to be potential effect modifiers (Breslow-Day P value < 0.05). Multi-variable logistic regression, including the final survey weights (producing results generalizable to the population of Maryland as described previously), was used to adjust for possible confounders and to find independent predictors of having received an OCS exam in the past year. We present two models, adjusting for the same predictor variables in each, with the addition of the variable, dental visit in the last year (for any reason) in the second model. Data were analyzed with SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). A two-tailed P value <0.05 was used to indicate significance.
Results
There were 20,197 surveys completed during the four survey years. The data from 1,143 people who did not respond to the oral cancer exam question (865) or the smoking questions (294) were excluded from the analysis leaving 19,054 respondents. After applying the survey weights, 16.7 percent of the respondents identified themselves as current smokers and 32.2 percent identified themselves as former smokers.
Table 1 shows the population characteristics as a whole and by smoking status. Compared with never smokers, a statistically significantly higher proportion of current smokers were black, in the youngest age group (40–49 years) and in the high-risk alcohol use category. A lower proportion of current smokers had attained an advanced education degree, reported their general health as excellent, very good, or good, had a routine medical checkup in the past year, or reported having a dental visit in the last year.
Table 1.
Characteristics of the Survey Sample Weighted to the Maryland Population by Smoking Status (Maryland Cancer Survey, 2002–2008)
| Smoking status
|
||||||
|---|---|---|---|---|---|---|
| Total population | Never | Former | Current | |||
|
|
||||||
| Characteristic | n | Weighted* % (95% CI) | Weighted* % (95% CI) | P value | ||
| Sex | ||||||
| Male | 6,782 | 45.9 (45.0–46.8) | 41.0 (39.7–42.2) | 51.8 (50.3–53.3) | 49.8 (47.5–52.1) | <0.0001 |
| Female | 12,272 | 54.1 (53.1–55.0) | 59.0 (57.8–60.3) | 48.2 (46.7–49.7) | 50.2 (47.9–52.5) | |
| Race | ||||||
| White | 14,738 | 70.2 (69.4–71.1) | 69.2 (67.9–70.4) | 75.8 (74.3–77.2) | 62.9 (60.5–65.2) | <0.0001 |
| Black | 3,644 | 25.0 (24.1–25.8) | 24.5 (23.3–25.7) | 21.2 (19.8–22.5) | 33.8 (31.5–36.1) | |
| Other | 672 | 4.8 (4.3–5.2) | 6.3 (5.6–7.1) | 3.1 (2.5–3.7) | 3.3 (2.5–4.2) | |
| Age in years | ||||||
| 40–49 | 5,282 | 36.7 (35.8–37.6) | 38.7 (37.4–40.0) | 26.6 (25.2–28.1) | 49.9 (47.6–52.1) | <0.0001 |
| 50–64 | 7,574 | 37.9 (37.1–38.8) | 36.4 (35.3–37.6) | 40.1 (38.6–41.5) | 38.4 (36.3–40.6) | |
| 65–74 | 3,466 | 14.4 (13.9–15.0) | 13.1 (12.4–13.8) | 19.5 (18.4–20.6) | 8.9 (7.7–10.0) | |
| 75 and older | 2,732 | 10.9 (10.5–11.4) | 11.8 (11.1–12.4) | 13.8 (12.9–14.7) | 2.9 (2.3–3.5) | |
| Marital status | ||||||
| Married/partnered | 11,167 | 67.6 (66.8–68.4) | 70.3 (69.2–71.3) | 70.1 (68.9–71.4) | 54.5 (52.3–56.8) | <0.0001 |
| Not married | 7,825 | 32.4 (31.6–33.2) | 29.7 (28.7–30.8) | 29.9 (28.6–31.1) | 45.5 (43.2–47.7) | |
| Education | ||||||
| Less than high school | 1,640 | 8.2 (7.7–8.7) | 6.1 (5.5–6.6) | 8.0 (7.2–8.8) | 15.3 (13.6–17.0) | <0.0001 |
| High school graduate | 5,436 | 27.0 (26.2–27.7) | 23.7 (22.7–24.7) | 26.0 (24.7–27.3) | 38.8 (36.6–41.1) | |
| Some college or college graduate | 8,573 | 45.8 (44.9–46.7) | 47.2 (46.0–48.5) | 47.2 (45.7–48.7) | 38.9 (36.7–41.1) | |
| Advanced degree | 3,357 | 19.0 (18.3–19.7) | 23.0 (21.9–24.1) | 18.8 (17.6–20.0) | 7.0 (5.9–8.1) | |
| Alcohol use† | ||||||
| None | 9,131 | 45.7 (44.8–46.6) | 49.7 (48.4–50.9) | 40.6 (39.1–42.1) | 43.2 (41.0–45.5) | <0.0001 |
| Low risk | 7,800 | 42.6 (41.8–43.5) | 42.8 (41.6–44.1) | 46.9 (45.4–48.4) | 33.7 (31.6–35.9) | |
| High risk | 1,911 | 11.7 (11.1–12.3) | 7.5 (6.7–8.2) | 12.5 (11.4–13.6) | 23.1 (21.1–25.1) | |
| Health status† | ||||||
| Excellent, very good, or good | 15,708 | 83.8 (83.1–84.4) | 87.5 (86.7–88.3) | 82.4 (81.3–83.5) | 75.0 (73.1–77.0) | <0.0001 |
| Fair or poor | 3,280 | 16.2 (15.6–16.9) | 12.5 (11.7–13.3) | 17.6 (16.5–18.7) | 25.0 (23.0–26.9) | |
| Dental visit in past year† | ||||||
| Yes | 14,132 | 74.5 (73.8–75.3) | 78.4 (77.4–79.5) | 76.1 (74.8–77.4) | 59.5 (57.3–61.8) | <0.0001 |
| No | 4,799 | 25.5 (24.7–26.2) | 21.6 (20.5–22.6) | 23.9 (22.6–25.2) | 40.5 (38.2–42.7) | |
| Routine medical checkup in past year† | ||||||
| Yes | 15,793 | 82.2 (81.5–82.9) | 83.6 (82.7–84.5) | 83.9 (82.8–85.1) | 74.6 (72.6–76.6) | <0.0001 |
| No | 3,125 | 17.8 (17.1–18.5) | 16.4 (15.5–17.3) | 16.1 (14.9–17.2) | 25.4 (23.4–27.4) | |
| Either medical checkup or denta visit in the past year† | ||||||
| Yes | 17,956 | 94.1 (93.7–94.6) | 95.4 (94.9–96.0) | 95.5 (94.8–96.1) | 87.5 (85.9–89.1) | <0.0001 |
| No | 1,028 | 5.9 (5.4–6.3) | 4.6 (4.0–5.1) | 4.5 (3.9–5.2) | 12.5 (10.9–14.1) | |
| Survey year | ||||||
| 2002 | 4,772 | 23.3 (22.6–24.0) | 22.1 (21.1–23.0) | 24.2 (22.9–25.4) | 25.6 (23.7–27.4) | <0.0001 |
| 2004 | 4,686 | 24.4 (23.6–25.1) | 23.8 (22.7–24.8) | 24.9 (23.6–26.2) | 25.2 (23.2–27.2) | |
| 2006 | 4,873 | 25.7 (24.9–26.5) | 25.7 (24.6–26.8) | 25.9 (24.6–27.3) | 25.4 (23.4–27.4) | |
| 2008 | 4,723 | 26.6 (25.8–27.4) | 28.5 (27.3–29.7) | 25.0 (23.7–26.4) | 23.8 (21.8–25.9) | |
Weighted to the Maryland population age 40 years and older.
Not all categories total 19,054 due to missing values.
The proportion of Maryland adults who reported having an OCS exam in the past year increased from 33.2 percent in 2002 to 39.8 percent in 2008 (Table 2). Screening between never and former smokers increased from 35.4 percent to 42.1 percent and from 35.2 percent to 43.8 percent, respectively, while screening among current smokers remained between 23.1 and 24.5 percent (Figure 1).
Table 2.
Characteristics of the Population Having Received versus Not Having Received Oral Cancer Screening within the Past Year (Maryland Cancer Survey, 2002–2008)
| Weighted %*, (95% CI)
|
|||
|---|---|---|---|
| Characteristic | Yes | No | P value |
| Total | 36.1 (35.2–36.9) | 63.9 (63.1–64.8) | |
| Smoking status | |||
| Never | 38.3 (37.1–39.5) | 61.7 (60.5–62.9) | <0.0001 |
| Former | 38.8 (37.4–40.3) | 61.2 (59.7–62.6) | |
| Current | 23.9 (22.0–25.7) | 76.1 (74.3–78.0) | |
| Sex | |||
| Male | 34.0 (32.7–35.4) | 66.0 (64.6–67.3) | <0.0001 |
| Female | 37.8 (36.8–38.8) | 62.2 (61.2–63.2) | |
| Race | |||
| White | 41.7 (40.7–42.6) | 58.3 (57.4–59.3) | <0.0001 |
| Black | 21.7 (20.0–23.3) | 78.3 (76.7–80.0) | |
| Other | 29.1 (24.6–33.7) | 70.9 (66.3–75.4) | |
| Age in years | |||
| 40–49 | 33.2 (31.7–34.8) | 66.8 (65.2–68.3) | <0.0001 |
| 50–64 | 39.2 (37.9–40.5) | 60.8 (59.5–62.1) | |
| 65–74 | 37.4 (35.5–39.3) | 62.6 (60.7–64.5) | |
| 75 and older | 33.1 (31.0–35.1) | 66.9 (64.9–69.0) | |
| Marital status | |||
| Married | 40.0 (38.9–41.1) | 60.0 (58.9–61.1) | <0.0001 |
| Not married | 28.0 (26.8–29.2) | 72.0 (70.8–73.2) | |
| Education | |||
| Less than high school | 14.2 (12.1–16.3) | 85.8 (83.7–87.9) | <0.0001 |
| High school graduate | 27.0 (25.5–28.4) | 73.0 (71.6–74.5) | |
| Some college or college graduate | 39.9 (38.6–41.2) | 60.1 (58.8–61.4) | |
| Advanced degree | 49.5 (47.5–51.6) | 50.5 (48.4–52.5) | |
| Health status | |||
| Excellent, very good, or good | 38.6 (37.7–39.6) | 61.4 (60.4–62.3) | <0.0001 |
| Fair or poor | 23.1 (21.3–24.8) | 76.9 (75.2–78.7) | |
| Routine medical checkup in past year | |||
| Yes | 37.6 (36.7–38.6) | 62.4 (61.4–63.3) | <0.0001 |
| No | 29.2 (27.3–31.1) | 70.8 (68.9–72.7) | |
| Dental visit in past year | |||
| Yes | 47.7 (46.7–48.7) | 52.3 (51.3–53.3) | <0.0001 |
| No | 2.7 (2.1–3.3) | 97.3 (96.7–97.9) | |
| Alcohol use | |||
| None | 30.1 (29.0–31.3) | 69.9 (68.7–71.0) | <0.0001 |
| Low risk | 43.4 (42.0–44.7) | 56.6 (55.3–57.9) | |
| High risk | 33.5 (30.9–36.1) | 66.5 (63.9–69.1) | |
| Survey year | |||
| 2002 | 33.2 (31.7–34.8) | 66.8 (65.2–68.3) | <0.0001 |
| 2004 | 34.1 (32.4–35.7) | 65.9 (64.3–67.6) | |
| 2006 | 36.8 (35.1–38.5) | 63.2 (61.5–64.9) | |
| 2008 | 39.8 (38.0–41.6) | 60.2 (58.4–62.0) | |
Weighted to the Maryland population aged 40 years and older.
Figure 1.
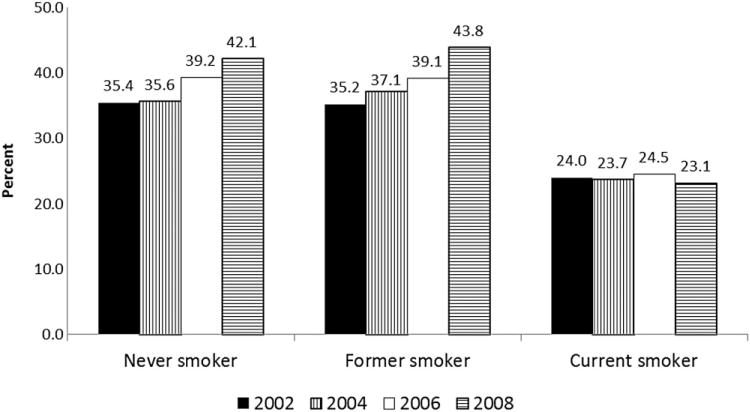
Percentage of Maryland adults, age 40 years and older, indicating they had an oral cancer screening exam within the previous year by smoking status and year of survey (weighted to the Maryland population).
Table 2 shows the unadjusted association of the weighted proportions between ever having an OCS exam within the past year and other characteristics. A significantly higher proportion of Marylanders with the following characteristics reported having an OCS exam within the past year compared with their counterparts: women, whites, those who were married or living with a partner, and those who reported their health status as good to excellent. The proportion of Marylanders reporting an OCS exam in the last year increased with increasing education level. Higher proportions of Marylanders reporting low-risk alcohol consumption in the past 30 days and routine checkups or dental visits within the past year also reported receiving an OCS exam in the past year compared with those reporting high-risk or no alcohol consumption in the past 30 days or those reporting routine checkups or dental visits 1 year or greater than 1 year in the past. Of those who named the type of provider who did the OCS exam, more than 90 percent was done by dental professionals (dentist, dental hygienist, oral surgeon, etc.) in each survey year and the remainder was done by a medical professional (physician or nurse practitioner) (data not shown).
Compared with never smokers, current smokers had 50 percent lower odds of reporting an OCS exam in the past year [unadjusted odds ratio (OR) 0.50, 95 percent confidence interval (CI), 0.45–0.56]. There was no significant difference between never and former smokers (unadjusted OR 1.02, 95 percent CI, 0.94–1.11).
Table 3 shows the adjusted association between having an OCS exam in the past year and smoking status, with and without adjustment for the variable dental visit in the past year. When dental visit in the past year was not included in the model, current smokers exhibited significantly lower odds of having received an OCS exam within the past year (OR 0.72, 95 percent CI, 0.64–0.82) compared with never smokers. There was no difference between former and never smokers (OR 1.05, 95 percent CI 0.96–1.14). Significantly higher odds of having received an OCS exam were noted among women compared with men, those who described their health status as excellent, very good, or good versus fair or poor, and those whose alcohol use was in the low-risk category versus non-drinkers. Higher odds of screening were noted with increasing education level. Blacks and people of other races had lower odds of receiving an oral cancer exam in the past year compared with whites. When compared with the survey year of 2002, those surveyed in 2006 and 2008 had higher odds of reporting an OCS exam in the past year. When the analysis included the variable dental visit in the past year, current smokers remained at decreased odds of reporting an OCS exam compared with never smokers, although the OR was not statistically significant (0.88, 95 percent CI 0.77–1.003). Having a dental visit in the past year was the strongest predictor of reporting an OCS in the past year (OR 26.56, 95 percent CI 21.26–33.18).
Table 3.
Weighted, Adjusted Association between an Oral Cancer Exam in the Past Year and Smoking Status, Adjusted for Other Predictors by Multiple Logistic Regression (Maryland Cancer Survey, 2002–2008)
|
n = 18,683
|
n = 18,571
|
|||
|---|---|---|---|---|
| Characteristic | OR* | 95% CI | OR† | 95% CI |
| Smoking status | ||||
| Never smoker | 1 | (ref) | 1 | (ref) |
| Former smoker | 1.05 | 0.96–1.14 | 1.09 | 1.00–1.19 |
| Current smoker | 0.72 | 0.64–0.82 | 0.88 | 0.77–1.003 |
| Sex | ||||
| Male | 1 | (ref) | 1 | (ref) |
| Female | 1.35 | 1.24–1.47 | 1.25 | 1.14–1.37 |
| Age in years | ||||
| 40–49 | 1 | (ref) | 1 | (ref) |
| 50–64 | 1.28 | 1.16–1.40 | 1.30 | 1.17–1.43 |
| 65–74 | 1.30 | 1.16–1.46 | 1.39 | 1.22–1.57 |
| 75 and older | 1.07 | 0.94–1.22 | 1.11 | 0.96–1.28 |
| Race | ||||
| White | 1 | (ref) | 1 | (ref) |
| Black | 0.48 | 0.43–0.53 | 0.53 | 0.47–0.60 |
| Other | 0.55 | 0.43–0.70 | 0.58 | 0.45–0.75 |
| Marital status | ||||
| Not married | 1 | (ref) | 1 | (ref) |
| Married or partnered | 1.33 | 1.23–1.45 | 1.17 | 1.07–1.28 |
| Education | ||||
| Less than high school | 1 | (ref) | 1 | (ref) |
| High school graduate | 1.75 | 1.44–2.13 | 1.15 | 0.92–1.44 |
| Some college or college graduate | 2.80 | 2.32–3.39 | 1.60 | 1.28–1.99 |
| Advanced degree | 3.70 | 3.02–4.54 | 1.95 | 1.54–2.47 |
| Health status | ||||
| Fair or poor | 1 | (ref) | 1 | (ref) |
| Excellent, very good, or good | 1.50 | 1.34–1.68 | 1.26 | 1.11–1.43 |
| Drinking status | ||||
| None | 1 | (ref) | 1 | (ref) |
| Low risk | 1.27 | 1.17–1.38 | 1.18 | 1.07–1.29 |
| High risk | 1.08 | 0.94–1.24 | 1.04 | 0.89–1.21 |
| Survey year | ||||
| 2002 | 1 | (ref) | 1 | (ref) |
| 2004 | 1.03 | 0.92–1.14 | 1.04 | 0.93–1.17 |
| 2006 | 1.13 | 1.02–1.26 | 1.24 | 1.11–1.39 |
| 2008 | 1.27 | 1.14–1.42 | 1.47 | 1.31–1.65 |
| Dental visit in past year | ||||
| Yes | NA | 26.56 | 21.26–33.18 | |
| No | NA | 1 | (ref) | |
Adjusted for smoking status, sex, race, age, marital status, education, health status, alcohol use, survey year.
Also adjusted for dental exam in the last year.
Discussion
During the period these surveys encompassed, self-reported OCS in the past year increased from 33 percent in 2002 to 40 percent in 2008 among Maryland residents age 40 years and older. During this time period, oral cancer prevention became an important goal for the State of Maryland (15). The Maryland model for oral cancer prevention included education of dental professionals and other health care providers in performing the OCS exam, educational programs for the public on oral cancer, and free OCS. Oral cancer was identified as one of the seven targeted cancers for prevention and screening under the Cigarette Restitution Fund Program and has been included in the Maryland Comprehensive Cancer Control Plans for 2004–2008 and 2011–2015 (16).
While the proportion of never and former smokers who reported receiving an OCS exam in the past year increased during this time period, the proportion of current smokers who reported having the exam remained fairly steady. Those adults at highest risk for developing oral cancer were the least likely to report being screened. Our analysis showed that after adjusting for potential confounders, current smokers had decreased odds of reporting an OCS exam in the past year compared with never smokers. There was no difference between never and former smokers. While other studies have examined self-reported OCS rates, this is the first analysis to show trends over time. Using data from the 1998 National Health Interview Survey (NHIS), Canto et al. found that only 13.8 percent of adults age 40 years or older reported having an OCS exam in the past year (17). Using data from the 2003 Behavioral Risk Factor Surveillance System survey in New York, Oh et al. (18) found that although the majority of adults (80.4 percent) had heard about oral cancer, only 35 percent of New York adults had reported receiving a screening exam in their lifetime. In a 2002 study of North Carolina adults age 18 years or older, Patton et al. showed that 29 percent of respondents reported ever having had an OCS exam and that current smokers were 2.3 times less likely to report having ever had an OCS compared with never/not at all smokers (19). Using data from the 1998 NHIS, Macek et al. (20) demonstrated that current smokers were not more or less likely to have received an OCS exam than never smokers. Reporting on a population-based statewide telephone survey in Florida from 2002, Tomar and Logan (21) found just 19.5 percent of adults reported receiving an oral cancer examination in the previous year, with this percentage being statistically significantly lower among current smokers. Our analysis shows that in Maryland, self-reported OCS exams in the past year have remained stagnant among current smokers since 2002, while the rates among former and never smokers have risen each year to levels above the HP 2010 objective.
Adults who reported having a dental visit in the last year reported higher proportions of OCS exams. When having a dental visit in the last year was included in the model, it became the strongest predictor of having an OCS exam. It is especially important for current and former smokers who are at higher risk for developing the disease to have regular OCS exams. Holmes et al. (22) found that cancers detected by a dental health care provider were of significantly lower stage than those referred by a medical office, especially for those lesions detected by a non-symptom-driven visit. While almost three-quarters of Marylanders age 40 years and older reported having a dental visit in the last year, this percentage was lowest (60 percent) among current smokers. It has been shown that long-term smokers are less likely to report visiting a dentist in the previous year (23).
Groups with other demographic characteristics have been shown to report fewer dental visits in the last year. An analysis of the Household Component of the 2004 Medical Expenditure Panel Survey (MEPS) showed that 63.7 percent of respondents under age 65 years reported no dental visit in the last year (24). In the adjusted analysis, respondents who had highest odds of not having a dental visit in the last year included non-Hispanic blacks and Hispanics (compared with non-Hispanic whites), the uninsured followed by adults with Medicaid insurance (compared with adults with private insurance), and adults with annual incomes of less than $20,000 followed by those with incomes between $20,000 and less than $40,000 (compared with adults with incomes of $40,000 or more). These findings from the MEPS analysis are consistent with what has become known as “the inverse care law,” the finding that people with the greatest health needs are least likely to receive health care. Shi and Stevens reported that low income, lacking health insurance, and not having a regular source of care, either singly or in combination, delayed dental care (25). In our analysis, we found that those with lower health status and lower educational status reported lower prevalence of receiving an OCS exam. As over 90 percent of OCS exams in our population were performed by dental professionals, it is imperative that adults have access to dental services, regardless of their socioeconomic status. It is unlikely all US residents will readily have access to dental care in the near future, as dental services for adults are not included for in the Affordable Care Act (26).
Examples of the inverse care law are not restricted to the United States. In a review published by Dryden et al., lower attendance at general health checks was seen in men with low incomes, lower socioeconomic status, the unemployed, and less educated (27). People who reported risk behaviors (smoking, alcohol consumption, less healthy diet) also had lower participation in health checks. These findings were found in the UK, countries in continental Europe, as well as Canada and the United States. In a study of regular dental checkups and factors associated with oral cancer in the in the UK, only older age was associated with dental checkups (28). After adjusting for education and social class, being male, having higher alcohol intake, smoking at least 20 cigarettes per day, and lower intake of fruits and vegetables were associated with lower odds of regular dental checkups.
It is also important for medical providers to provide OCS when they perform physical exams. While 82 percent in our survey reported having a routine medical checkup in the past year, only 36 percent reported having an OCS exam in the past year. Many adults visit a medical provider more often than a dental provider. Access to dental care is especially lacking for low-income non-elderly adults (29). Physicians, nurse practitioners, and physician assistants should include OCS, as well as counseling about oral cancer risk factors, as part of their routine preventive care. In 2002, Canto et al. (30) reported that only 24 percent of surveyed Maryland family practice physicians provided OCS exams to patients age 40 years and older. In a survey of 389 Maryland nurse practitioners, Siriphant et al. (31) reported in 2002 that while almost 79 percent could identify the procedure involved in conducting an OCS exam, less than one-half knew the early signs of the oral cancer. More education is needed among medical providers. In 2000, the Surgeon General’s report on Oral Health in America highlighted oral health needs in the United States and disparities due to age, race, and socioeconomic status as a major public health problem (32). The National Call to Action to Promote Oral Health under the leadership of the Surgeon General in 2003 promotes opportunities for enhanced educational efforts for both the general public as well as health professionals, including medical providers, to improve oral health (33). For example, the University of Washington recently included an oral health curriculum for their medical students to improve the knowledge and behavior of new practitioners with respect to oral health (34). When performing routine OCS exams, medical and dental health care providers should make additional efforts to inquire about risk factors for oral cancer and make programs available to reduce the effect of well-known risk factors, especially tobacco use.
Limitations and strengths
As with many surveys, this study is limited by its reliance on self-report. Clinical chart review was not done to validate the responses about OCS. While the OCS exam was described in detail during the interview, it is possible that some respondents had received an exam but did not remember having it because the nature of the exam was not emphasized by their health provider. Another limitation of the survey included the use of only landline telephone numbers; households that use only cell phones or have no telephone were excluded. However, as described by Blumberg et al. (35), the percentage of adults without landlines, while increasing, remains relatively small and should have minimal impact on the survey especially among the population age 40 years or older. The survey does not reach people living in group homes, nursing homes, or institutions such as prisons. As the surveys are administered in English, we were not able to reach the non-English speaking residents in Maryland with the exception of 2006 when the survey was offered in Spanish. While the weighting schema adjusts for non- and differential response, underrepresentation of some segments may lead to biased estimates of the screening rates. The Maryland Cancer Survey’s restriction to adults age 40 years and older does not allow us to report on OCS in younger age groups, which have seen a recent increase in oral cancer, most likely due to human papillomavirus (36,37).
The Maryland Cancer Survey has several strengths. It is a population-based, statewide survey with a large sample size for each survey year. Four years of survey data have been included in this analysis. Recall bias is reduced by the wording used to ask the specific questions related to OCS that may help the respondent to recall whether they have had the procedure performed. The results found in this study add to the growing body of literature regarding the importance of OCS by health practitioners.
Conclusion
Current and former smokers are high-risk groups who need to be targeted for oral cancer exams by dental professionals and primary care providers. While the proportion of adults reporting an OCS exam increased each survey year, the increase was seen exclusively among never and former smokers. There was no change in self-reported OCS in current smokers between 2002 and 2008. Annual dental visits should be encouraged for all persons, especially current and former smokers who may be at higher risk for developing oral cancers. Dental health providers should also avail themselves of the opportunity to screen for oral cancer at any office visit and discuss the nature of the exam with their patients, especially for their clients who may be at high risk for disease. OCS should become a part of each routine physical exam given by a primary care provider. Thus, schools that train medical providers such as doctors, nurses, and physician’s assistants must include OCS in their curriculum. Routine dental care needs to be made available to low-income and uninsured adults. In addition to OCS during routine office visits, dental and medical offices should offer assistance in the reduction of risk factors for oral cancer, particularly in referral to tobacco-use cessation programs.
Footnotes
Conflict of interest
None.
References
- 1.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics. CA Cancer J Clin. 2011;61:212–36. doi: 10.3322/caac.20121. [cited 2012 Mar 12]. Available from: http://onlinelibrary.wiley.com/doi/10.3322/caac.20121/pdf. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer facts & figures 2011. Atlanta: American Cancer Society; 2011. [cited 2012 Mar 12]. Available from: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-029771.pdf. [Google Scholar]
- 3.Surgeon general’s report 2004. [cited 2012 Mar 12]. Available from: http://www.cdc.gov/tobacco/data_statistics/sgr/2004/pdfs/chapter2.pdf.
- 4.Lambert R, Sauvaget C, de Carmargo Cancela M, Sankaranarayanan R. Epidemiology of cancer from the oral cavity and oropharynx. Eur J Gastroenterol Hepatol. 2011;23(8):633–41. doi: 10.1097/MEG.0b013e3283484795. [DOI] [PubMed] [Google Scholar]
- 5.Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Chen HS, Feuer EJ, Cronin KA, Edwards BK, editors. Seer cancer statistics review, 1975–2008. Bethesda, MD: National Cancer Institute; 2010. [cited 2012 Mar 12]. Available from: http://seer.cancer.gov/csr/1975_2008/, based on November SEER data submission, posted to the SEER web site, 2011. [Google Scholar]
- 6.Blot WJ, McLaughlin JK, Winn DM, Austin DF, Greenberg RS, Preston-Martin S, Bernstein L, Schoenberg JB, Stemhagen A, Fraumeni JF., Jr Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48:3282–7. [PubMed] [Google Scholar]
- 7.Winn DM. Tobacco use and oral disease. J Dent Educ. 2001;65(4):306–12. [PubMed] [Google Scholar]
- 8.Tramacere I, Negri E, Bagnardi V, Garavello W, Rota M, Scotti L, Islami F, Corrao G, Boffetta P, La Vecchia C. A meta-analysis of alcohol drinking and oral and pharyngeal cancers. Part 1: overall results and dose-risk relation. Oral Oncol. 2010;46(7):497–503. doi: 10.1016/j.oraloncology.2010.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Truman BI, Gooch BF, Sulemana I, Gift HC, Horowitz AM, Evans CA, Griffin SO, Carande-Kulis VG, Task Force on Community Preventive Services Reviews of evidence on interventions to porevent dental caries, oral and pharyngeal cancers, and sports-related craniofacial injuries. Am J Prev Med. 2002;23(1S):21–54. doi: 10.1016/s0749-3797(02)00449-x. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services. Healthy People 2010, with understanding and improving health and objectives for improving health. Vol. 2. Washington, DC: U.S. Government Printing Office; 2000. [cited 2012 Feb 22]. Available from: http://www.healthypeople.gov/2010/Publications/ [Google Scholar]
- 11.U.S. Department of Health and Human Services. Healthy People 2020. Oral health topics and objectives. [cited 2012 Feb 22]. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=32.
- 12.Maryland Department of Health and Mental Hygiene. Cigarette restitution fund program cancer report 2008. Baltimore MD: Dec, 2010. Updated March 2011 [cited 2012 Sep 5]. Available from: http://fha.dhmh.maryland.gov/cancer/Documents/CRF_Cancer_Report_2010.pdf. [Google Scholar]
- 13.Ling H, Gadalla S, Israel E, Langenberg P, Zhan M, Dwyer DM, Groves C, Hopkins A, Steinberger EK. Oral cancer exams among cigarette smokers in Maryland. Cancer Detect Prev. 2003;30:499–506. doi: 10.1016/j.cdp.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Maryland Department of Health and Mental Hygiene. Maryland cancer survey reports, 2002–2008. [cited 2012 Mar 12]. Available from: http://fha.dhmh.maryland.gov/cancer/SitePages/surv_data-reports.aspx#anch3.
- 15.Maybury C, Horowitz AM, Goodman HS. Outcomes of oral cancer early detection and prevention statewide model in Maryland. J Public Health Dent. 2012;72(1):S34–S38. doi: 10.1111/j.1752-7325.2012.00320.x. [DOI] [PubMed] [Google Scholar]
- 16.Maryland Department of Health and Mental Hygiene. Maryland comprehensive cancer control plan. [cited 2012 Mar 12]. Available from: http://fha.dhmh.maryland.gov/cancer/cancerplan/SitePages/Home.aspx.
- 17.Canto MT, Drury TF, Horowitz AM. Use of skin and oral cancer examinations in the United States, 1998. Prev Med. 2003;37:278–82. doi: 10.1016/s0091-7435(03)00124-5. [DOI] [PubMed] [Google Scholar]
- 18.Oh J, Kumar J, Cruz G. Racial and ethnic disparity in oral cancer awareness and examination: 2003 New York state BRFSS. J Public Health Dent. 2008;68(1):30–8. doi: 10.1111/j.1752-7325.2007.00075.x. [DOI] [PubMed] [Google Scholar]
- 19.Patton LL, Agans R, Elter JR. Oral cancer knowledge and examination experience among North Carolina adults. J Public Health Dent. 2004;64(3):173–80. doi: 10.1111/j.1752-7325.2004.tb02748.x. [DOI] [PubMed] [Google Scholar]
- 20.Macek MD, Reid BC, Yellowitz JA. Oral cancer examinations among adults at high risk: findings from the 1998 National Health Interview Survey. J Public Health Dent. 2003;63(2):119–25. doi: 10.1111/j.1752-7325.2003.tb03485.x. [DOI] [PubMed] [Google Scholar]
- 21.Tomar SL, Logan HL. Florida adults’ oral cancer knowledge and examination experiences. J Public Health Dent. 2005;65(4):221–30. doi: 10.1111/j.1752-7325.2005.tb03022.x. [DOI] [PubMed] [Google Scholar]
- 22.Holmes JD, Dierks EJ, Homer LD, Potter BE. Is detection of oral and oropharyngeal squamous cancer by a dental health care provider associated with a lower stage at diagnosis? J Oral Maxillofac Surg. 2003;61(3):285–91. doi: 10.1053/joms.2003.50056. [DOI] [PubMed] [Google Scholar]
- 23.Mucci LA, Brooks DR. Lower use of dental services among long term cigarette smokers. J Epidemiol Community Health. 2001;55:389–93. doi: 10.1136/jech.55.6.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shi L, Lebrun LA, Tsai J. Access to medical care, dental care, and prescription drugs: the roles of race/ethnicity, health insurance, and income. South Med J. 2010;103(6):509–16. doi: 10.1097/SMJ.0b013e3181d9c2d8. [DOI] [PubMed] [Google Scholar]
- 25.Shi L, Stevens GD. Vulnerable populations in the United States. San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- 26.American Dental Association. Potential effects of the affordable care act on dentistry. [cited 2012 Dec 27]. Available from: http://www.ada.org/sections/newsAndEvents/pdfs/PotentialEffectsoftheACAonDentistry_NewsStory_Final.pdf.
- 27.Dryden R, Williams B, McCowan C, Themessl-Huber M. What do we know about who does and does not attend general health checks? Findings from a narrative scoping review. BMC Public Health. 2012;12:723. doi: 10.1186/1471-2458-12-723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Netuveli G, Sheiham A, Watt RG. Does the “inverse screening law” apply to oral cancer screening and regular dental check-ups? J Med Screen. 2006;13(1):47–50. doi: 10.1258/096914106776179836. [DOI] [PubMed] [Google Scholar]
- 29.Licata R, Paradise J. Kaiser commission on medicaid and the uninsured. Oral health and low-income nonelderly adults. [cited 2013 Jan 4]. Available from: http://www.kff.org/medicaid/upload/7798-02.pdf.
- 30.Canto MT, Horowitz AM, Drury TF, Goodman HS. Maryland family physicians’ knowledge, opinions, and practices about oral cancer. Oral Oncol. 2002;38:416–24. doi: 10.1016/s1368-8375(01)00080-x. [DOI] [PubMed] [Google Scholar]
- 31.Siriphant P, Drury TF, Horowitz AM, Harris RM. Oral cancer knowledge and opinions among Maryland nurse practitioners. J Public Health Dent. 2001;61(3):138–44. doi: 10.1111/j.1752-7325.2001.tb03380.x. [DOI] [PubMed] [Google Scholar]
- 32.U.S. Department of Health and Human Services. Oral health in America: a report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [cited 2012 Mar 7]. Available from: http://www.surgeongeneral.gov/library/reports/oralhealth/ [Google Scholar]
- 33.U.S. Department of Health and Human Services. National call to action to promote oral health. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Dental and Craniofacial Research; Spring. 2003. (NIH Publication No. 03-5303). [cited 2012 Mar 7]. Available from: http://www.surgeongeneral.gov/topics/oralhealth/nationalcalltoaction.html. [PubMed] [Google Scholar]
- 34.Mouradian WE, Reeves A, Kim S, Evans R, Schaad D, Marshall SG, Slayton R. An oral health curriculum for medical students at the University of Washington. Acad Med. 2005;80(5):434–42. doi: 10.1097/00001888-200505000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Blumberg SJ, Luke JV, Cynamon ML. Telephone coverage and health survey estimates: evaluating the need for concern about wireless substitution. Am J Public Health. 2006;96(5):926–31. doi: 10.2105/AJPH.2004.057885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaminagakura E, Villa LL, Andreoli MA, Sobrinho JS, Vartanian JG, Soares FA, Nishimoto IN, Rocha R, Kowalski LP. High-risk human papillomavirus in oral squamous cell carcinoma of young adults. Int J Cancer. 2012;130(8):1726–32. doi: 10.1002/ijc.26185. [DOI] [PubMed] [Google Scholar]
- 37.Bleyer A. Cancer of the oral cavity and pharynx in young females: increasing incidence, role of human papilloma virus, and lack of survival improvement. Semin Oncol. 2009;36(5):451–9. doi: 10.1053/j.seminoncol.2009.07.005. [DOI] [PubMed] [Google Scholar]


