Abstract
The purpose of this study was to determine the presence and prevalence of asymmetry in lower extremity joint moments within and across healthy populations during overground walking. Bilateral gait data from several studies performed at two institutions were pooled from 182 healthy, pain-free subjects. Four distinct populations were identified based on age, activity level and body mass index. Mean peak external joint moments were calculated from three to six trials of level overground walking at self-selected speed for each subject. Right and left limb moments were reclassified as “greater” or “lesser” moment for each subject to prevent obscuring absolute asymmetry due to averaging over positive and negative asymmetries across subjects. A clinically relevant asymmetry measure was calculated from the peak joint moments with an initial chosen cutoff value of 10%. Confidence intervals for the proportion of subjects with greater than 10% asymmetry between limbs were estimated based on the binomial distribution. We found a high amount of asymmetry between the limbs in healthy populations. More than half of our overall population exceeded 10% asymmetry in peak hip and knee flexion and adduction moments. Group medians exceeded 10% asymmetry for all variables in all populations. This may have important implications on gait evaluations, particularly clinical evaluations or research studies where asymmetry is used as an outcome. Additional research is necessary to determine acceptable levels of joint moment asymmetry during gait and to determine whether asymmetrical joint moments influence the development of symptomatic pathology or success of lower extremity rehabilitation.
Keywords: Gait analysis, rehabilitation, joint mechanics
Introduction
Lower limb symmetry is often assumed in healthy individuals, and deviations from this standard are thought to be due to the presence of pathology [1,2]. In a clinical setting, muscle strength and functional symmetry are often used to define goals during rehabilitation [3] and to evaluate treatment efficacy [4].
The use of clinical gait analysis to calculate joint moments is growing and is of particular interest for pathologies such as hip and knee osteoarthritis. At the knee, adduction moments can be used as a surrogate measure of medial-lateral load distribution within the joint [5], while knee flexion moments are related to quadriceps demand [6]. High joint moments have been associated with the severity and progression of osteoarthritis [7,8], and subjects with symptomatic unilateral pathology have been shown to exhibit statistically significant asymmetries in lower extremity moments during walking [9]. However, before we can determine whether symmetry of joint moments during walking would be an appropriate standard for health and rehabilitation for individuals with unilateral pathology, we must first determine whether joint moments are symmetric in healthy individuals.
Although symmetry during walking is generally assumed, previous research has led to mixed conclusions [10]. Some studies have provided support for symmetry in spatiotemporal parameters [11], joint kinematics [12] and ground reaction forces [13] in healthy individuals, while others have reported the presence of asymmetry in these same parameters [14,15]. Previous work in populations of healthy individuals, has investigated joint moment symmetry with conflicting results [9,16–18]. Studies which identified symmetry in peak joint moments grouped data based on limb dominance or by randomly assigned “study” and “non-study” limbs which led to signed (positive and negative) values of calculated asymmetry and may have obscured absolute symmetry when grouped for statistical analysis [9,17].
Additionally, some populations of healthy individuals are known to be at higher risk for developing osteoarthritis than the general population. Obesity, age, and participation in high-intensity athletics such as football have all been associated with increased risk for developing osteoarthritis [19], but joint moment symmetry in such at-risk populations of healthy individuals has not yet been explored. There remains a need to further investigate symmetry in joint moments during walking in healthy individuals, and to do so without the potential for obscuring asymmetry by averaging over positive and negative values of asymmetry that may result from side-dependent grouping. Therefore, the purpose of this research was to determine the presence and prevalence of asymmetry in lower extremity joint moments during walking within and across four distinct populations of healthy subjects that span a range of age, body mass index, and participation in sport.
Methods
Study Population
Data were pooled from several studies performed at The Ohio State University and Stanford University. All studies were approved by their respective university IRB and all subjects provided IRB-approved informed consent prior to data collection. All identifiable information was removed from the data prior to institutional collaboration; only subject age, gender, body mass index (BMI), self-selected walking speed, and joint kinetics were shared between institutions.
All subjects whose data were analyzed were healthy at the time of data collection. Volunteers were excluded from participation if they had a history of previous lower extremity surgery or lower extremity injury, consistent or current lower extremity pain, or previous diagnosis of any orthopaedic or neurological conditions affecting their gait. All subjects were independent community walkers and did not use assistive walking devices. Four distinct populations were identified within the data based on subject age, activity level and BMI. These populations were defined as 1) young healthy: 20–39 years, BMI<30 kg/m2; 2) older healthy: 40–60 years, BMI<30 kg/m2; 3) obese: 20–60 years, BMI>30 kg/m2; and 4) collegiate football linemen: 18–22 years, BMI>30 kg/m2. Physical activity was not controlled for in any population except the collegiate football linemen who were included only if they were active members of a collegiate football team. Additional information for each population can be seen in Table 1.
Table 1.
Population definitions, criteria, data source (The Ohio State University (I1) or Stanford University (I2)), means and standard deviations of subject age, body mass index (BMI) and self-selected walking speed during data collection.
| Criteria | Descriptive Statistics | |||||||
|---|---|---|---|---|---|---|---|---|
| Population | Age | BMI | Total n | Source | Gender | BMI | Age | Speed (m/s) |
| Younger, healthy BMI | 18–39 | < 30 | 93 | 39 I1 54 I2 |
38 Female 55 Male |
23.94±2.96 | 26.78±5.36 | 1.37±0.15 |
| Older, healthy BMI | 40–60 | < 30 | 43 | 1 I1 42 I2 |
21 Female 22 Male |
24.87±3.13 | 50.8±5.66 | 1.36±0.15 |
| Obese | 20–60 | > 30 | 34 | 34 I2 | 20 Female 14 Male |
35.04±3.98 | 34.53±8.40 | 1.35±0.17 |
| Collegiate Linemen | 18–22 | > 30 | 12 | 12 I1 | 12 Male | 36.17±2.84 | 19.75±1.48 | 1.80±0.17 |
| All Subjects | 18–60 | 18–46 | 182 | 52 I1 130 I2 |
79 Female 103 Male |
27.038±5.81 | 33.45±11.92 | 1.39±0.18 |
Data Collection
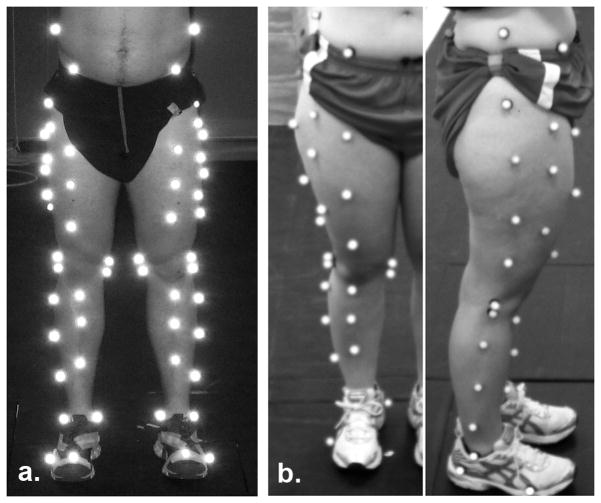
Height, weight and additional anthropometric data were recorded. Reflective markers were placed on each subject according to the point cluster technique (PCT) convention (Figure 1). PCT is a bone pose estimation method and associated marker set for estimating lower extremity kinematics which eliminates excess noise due to soft tissue movement [20] that has been used in healthy and pathological populations over a range of BMI [21,22]. All subjects wore their own shoes during data collection and were instructed to walk at a comfortable pace in a straight line over level ground while marker and force data were collected. Walking paths were approximately 10m long with force plates located in the middle of the path. Both laboratories were equipped with at least eight high-speed motion capture cameras and at least one force plate embedded in the floor. Left and right leg data were collected from consecutive foot strikes on adjacent force plates within the same trial for subjects tested at The Ohio State University; separate walking trials were performed for the left and right legs for subjects whose data were collected at Stanford University. Data from at least three trials with clean footstrikes from each foot were used per subject. Knee joint centers were defined as the midpoint between the markers placed on the femoral condyles. Hip joint centers were calculated with either a Bell’s regression equation [23] (Stanford University) or functionally using the star-arc approach [24] (The Ohio State University). Because each subject acted as his or her own control for comparison between limbs, and within-subject methods were consistent, the differences in data collection and analysis between institutions would have minimal influence on the results of this study.
Figure 1.
Representative subject from data collected at The Ohio State University (a.) and Stanford University (b.) with markers placed according to the Point Cluster Technique (PCT) marker convention
Calculation of Dependent Variables
Inverse dynamics techniques were used to calculate the peak three-dimensional external hip, knee and ankle joint moments that occurred during the stance phase of gait for each trial. Peak moments were calculated for the left and right limb for each trial, and were averaged over three to six trials for each subject. Moments were normalized via division by bodyweight and height for each subject and presented as a percentage of bodyweight times height (%BW*H). The average moments for the right and left sides of each subject were then reclassified as “greater” or “lesser” based on the magnitude of the variable of interest in order to avoid any underrepresentation of absolute asymmetry due to averaging over positive and negative values when calculating group means.
A “clinical asymmetry” measure was calculated for each variable for each subject using the following formula:
This formula, based on a previously defined limb symmetry index [25], indicates the relative difference between limbs for each moment. Using this formula, if the greater moment is twice that of the lesser moment there will be 50% asymmetry between limbs, and if the moments are identical there will be zero asymmetry. Descriptive statistics of the percentage of asymmetry between limbs were calculated for each variable of interest for each group.
A clinically relevant value of asymmetry has not yet been established for joint moments produced during walking. Based on the use of 10% as a cutoff value signifying clinically relevant differences in muscle strength and performance based testing [3,26] we chose 10% as an initial cutoff value for determining symmetric vs. asymmetric joint moments in this study.
Statistical Analysis
The 95% confidence interval for the proportion of subjects in each population exhibiting greater than 10% asymmetry was estimated based on the binomial distribution using the Clopper-Pearson method (MATLAB, Mathworks, Natick, MA) [27]. Differences among the four populations were tested using a Kruskal-Wallis test (non-parametric procedure as ANOVA) for asymmetry, and Chi-square test for the proportion of subjects with >10% asymmetry. Differences between male and female subjects were also tested using a Mann-Whitney test and the association of speed and the magnitude of asymmetry for each moment were examined using a test of the Spearman correlation coefficient.
Results
Population Characteristics
Data from 182 subjects were included in the analysis. Eight subjects were excluded from the original pool of 190; five due to a lack of at least three valid trials, two from the “Collegiate Lineman” group due to BMI below the group criteria threshold, and one due to missing age data. Descriptive statistics from each population can be found in Table 1.
Calculated Joint Moments
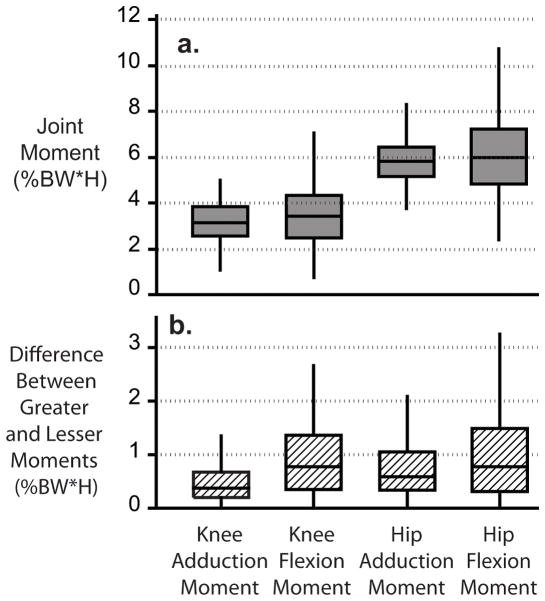
Distributions of the magnitude of external adduction and flexion moments at the knee and hip from all subjects included in this study are shown in Figure 2a. The distribution of the difference between the “greater” and “lesser” moments for all subjects is shown in Figure 2b. Knee adduction moment (KAM), knee flexion moment (KFM), hip adduction moment (HAM) and hip flexion moment (HFM) results are discussed here due to the suggested relationships between these moments and joint degeneration [7,28] (Supplemental Figures 1–3 provide results from additional joint moments).
Figure 2.
Boxplots of the peak joint moments (a.) and the difference between the “greater” and “lesser” moments (b.) for all subjects. Boxes include the interquartile range of the data, medians are indicated by the horizontal line and whiskers represent the upper and lower 25% of the distribution
The greater joint moment was not consistently seen in either right or left limbs throughout any population. In the population of all subjects, the greater knee adduction and flexion moments occurred in the right leg in 48.90% and 38.46% of subjects, respectively, and the greater hip adduction and flexion moments in 57.69% and 52.75%, respectively. No statistical differences were seen between male and female subjects for any joint moments (p value = 0.33 KAM, 0.76 KFM, 0.37 HAM, and 0.10 HFM).
Asymmetry
The median of the calculated percentage of asymmetry between limbs exceeded 10% for all hip and knee joint moments in all groups (Figure 3). More than 50% of our overall population exceeded 10% asymmetry in adduction and flexion moments at the knee and hip (percentage of overall population exceeding 10% asymmetry in each moment: 62.1% KAM, 78.6% KFM, 52.7% HAM, and 61.0% HFM, Figure 4). Subjects were most likely to have asymmetry in the KFM (78.6%); the 95% confidence interval suggests that 72 to 84% of the overall population would exceed 10% asymmetry of the KFM. Asymmetry measures were not statistically different among the four populations based on Kruskal-Wallis tests (p value = 0.67 KAM, 0.30 KFM, 0.32 HAM, and 0.59 HFM). No population has a statistically higher or lower proportion of individuals exhibiting greater than 10% asymmetry based on Chi-square tests (p value = 0.74 KAM, 0.57 KFM, 0.97 HAM, and 0.85 HFM). There was no significant association between walking speed and the magnitude of asymmetry (p value = 0.83 KAM, 0.65 KFM, 0.13 HAM and 0.94 HFM); however, it should be noted that walking speed was significantly faster in the population of collegiate linemen than in the other three populations (p value <0.001).
Figure 3.
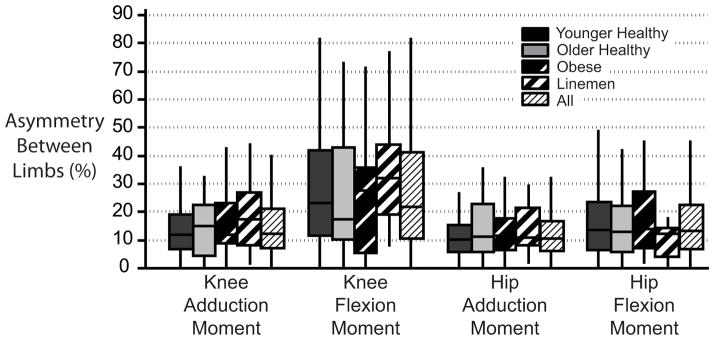
Boxplot for the percentage of asymmetry in knee and hip joint moments between the lower limbs during walking. Boxes include the interquartile range of the data, medians are indicated by the horizontal line and whiskers represent the upper and lower 25% of the distribution.
Figure 4.
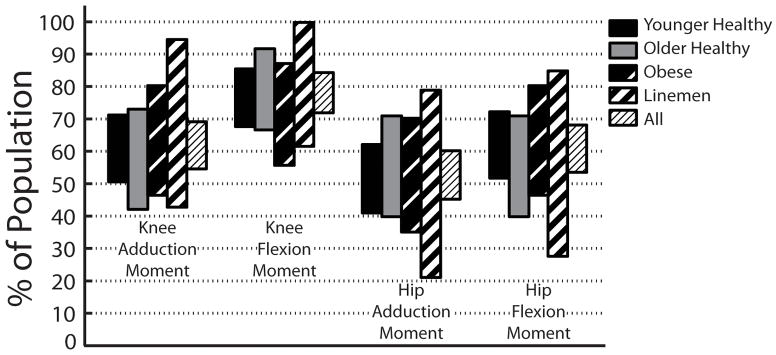
Confidence intervals for the proportion of subjects in each population with greater than 10% asymmetry. From these intervals, we can be 95% certain that the percentage of each population exhibiting greater than 10% asymmetry will fall within the confidence interval shown.
Discussion
The percentage of asymmetry between lower extremity joint moments during walking was greater than expected in all of our populations, for all variables. More than half of our overall population had greater than 10% asymmetry in hip and knee flexion and adduction moments with the greatest likelihood of asymmetry occurring in the KFM (78.6%).
Our results complement previous studies suggesting asymmetry in lower extremity joint moments of healthy populations during gait [16,18], but appear to contradict others which suggest symmetry between limbs [9,17]. Studies by Teichtahl et al. and Creaby et al. found no statistical differences in peak KAMs between the limbs of healthy individuals when data were grouped based on limb dominance [17] or by randomly assigned “study” and “non-study” limbs [9]. In both of these investigations, assignment of limbs dominant/non-dominant or study/non-study prior to the calculation of asymmetry resulted in some subjects having positive and some subjects having negative values of asymmetry within each group, which may have led to an underrepresentation of the magnitude of absolute asymmetry between limbs through averaging within each group. By grouping data based on joint moment magnitude rather than by preassignment, our calculated asymmetries were always greater than or equal to zero, thus giving a clear indication of the absolute asymmetry between limbs without the risk of underrepresenting the magnitude during group analyses.
Relying on predefined assignment of the limbs can potentially underrepresent limb asymmetry. We used a symmetry index similar to that used by Teichtahl and colleagues (SI(%) = 100*[LimbA−LimbB]/[0.5*(LimbA+LimbB)], where SI=0% represents perfect symmetry) to explore the effects of pre-assigning groups on the resulting symmetry. Using this equation, we pre-assigned our data into groups based on limb side (LimbA=right, LimbB=left), and calculated an SI of 0.94% between right and left KAMs. This low SI suggests high symmetry between limbs. However, when we grouped our data by the magnitude of the KAM, we calculated an SI of 17.31% between the “greater” and “lesser” limb moments, demonstrating that a great deal of absolute asymmetry can be obscured if pre-assignment of the limbs to categorical groups results in positive and negative asymmetries within a single group.
One of the strengths of the present investigation is our identification of similar asymmetry in four diverse populations whose data were collected at two institutions with slight differences in data collection and analysis. It is natural to question whether the results of this study may have been influenced by the differences in data collection or analysis between institutions. Our population of younger healthy subjects was comprised of data collected and analyzed at both institutions (42% of subjects at The Ohio State University, 58% of subjects at Stanford University); therefore we can use this population to explore the potential effects of institutional differences with few confounding factors. Within this population, the median asymmetry of KAM, HAM, and HFM differed by less than 4% between institutions with similar interquartile ranges (Supplemental Figure 4). The KFM exhibited greater variability (14% asymmetry difference between institutions); however, asymmetry of the KFM also demonstrated greater variability than the other joint moments within each subject population (Figure 3).
Although a large proportion of subjects included in the present study demonstrated greater than 10% asymmetry, it is important to keep in mind that the clinical relevance of our chosen cutoff value of 10% asymmetry in lower extremity joint moments has not yet been well defined. The value of 10% asymmetry used throughout this paper is based on measures of strength and functional performance [3,26], but clinical significance in joint moments may be different. For instance, high KAMs have been associated with thicker cartilage in a healthy population [29], but have also been associated with progression and severity of osteoarthritis [7,8]. Our results suggest that between 55–69% of individuals in our overall population exhibit greater than 10% asymmetry in KAMs during walking; however, the prevalence of osteoarthritis in the general population is estimated to be only 14%, even in individuals over the age of 60 [30]. Therefore, it would seem that asymmetry exceeding 10% may not be an indicator of pathology or precursor to unilateral osteoarthritis.
This study had several limitations, the greatest of which is that joint moments were calculated from skin-based optical motion capture data. The data, therefore, are dependent upon marker placement and may be influenced by soft-tissue movement, which is expected to be even higher in our high-BMI groups. However, given that these techniques are commonly used within the laboratory setting to examine lower extremity moments and within clinical settings to make treatment decisions, the results are relevant for future research and clinical applications. Moreover, each subject acts as his/her own control because the comparisons performed were all between legs of individuals, so it is assumed that the effects of soft-tissue movement would be similar in both limbs and would minimally affect the results. It should also be noted that between-limb asymmetries were calculated from separate walking trials for the right and left limbs for data collected at Stanford University. However, walking speeds for right and left limb trials for each subject were very similar, differing by an average of only 0.10±0.08 m/s. Data collected at both institutions were also averaged over at least three trials per subject for both the right and left limbs in order to minimize any small differences which may have occurred during individual walking trials. Additionally, differences in asymmetries between institutions were small, as indicated previously.
Differences in the sample size of the populations that were compared may also be a limitation of the present study. Our populations ranged in size from 12 to 93 subjects. Despite these differences in sample size, the distribution of asymmetry of each joint moment was similar across populations (Figure 3); however, including additional subjects in the smaller populations, particularly the population of collegiate linemen may have produced slightly different results. Additionally, we acknowledge that our investigation did not include a population of high-level female athletes. As noted in the results, the effects of gender on joint moment asymmetry were not statistically significant, and within groups (except the linemen), the distributions of male and female subjects were also similar (distributions can be seen in Supplemental Figure 5). However, inclusion of a population of high-level female athletes would have provided additional results and perhaps may have led to different or additional conclusions.
Lastly, it should be noted that limb length discrepancy, strength, mechanical axis alignment and radiographic joint health may also influence joint moment symmetry; however these parameters were not included in our analysis. Although we cannot rule out their influence, we assume that subjects who participated in this study were no more or less likely than other individuals in their greater populations to have asymptomatic limb length discrepancies, strength deficiencies, malalignment or preclinical osteoarthritis.
Conclusions
Clinically, contralateral limb measures are often used for comparison when determining the level of impairment and as a standard for rehabilitation when unilateral limb pathologies are present. In this cross-sectional research study, we found a high amount of asymmetry in hip and knee adduction and flexion moments between the limbs in healthy populations. Knowledge of expected or baseline asymmetry within and across various populations of healthy adults is valuable for interpretation of gait evaluations, particularly if symmetry is to be used as a measure of success for intervention or rehabilitation strategies or for diagnosis of pathology. Longitudinal studies are necessary to determine acceptable levels of asymmetry in healthy individuals and the implications of asymmetrical joint moments on the risk for development of symptomatic pathology.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge Mike McNally and Jay Young for their help with data collection and analysis. Funding for this research was provided by the NFL Charities, OSU Sports Medicine, and VA Merit Review AR6650. This material is based upon work supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE-0822215. Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Science Foundation. Xueliang Pan is also partially supported by Grant 8UL1TR000090-05 from the National Center for Advancing Translational Sciences.
Footnotes
Conflict of Interest Statement
We have no conflicts of interest to report.
References
- 1.Griffin MP, Olney SJ, McBride ID. Role of symmetry in gait performance of stroke subjects with hemiplegia. Gait Posture. 1995;3(3):132–142. [Google Scholar]
- 2.Kaufman KR, Miller LS, Sutherland DH. Gait asymmetry in patients with limb-length inequality. Journal of pediatric orthopedics. 1996;16(2):144–150. doi: 10.1097/00004694-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34(4):269–280. doi: 10.2165/00007256-200434040-00006. [DOI] [PubMed] [Google Scholar]
- 4.Becker HP, Rosenbaum D, Kriese T, Gerngross H, Claes L. Gait asymmetry following successful surgical treatment of ankle fractures in young adults. Clin Orthop Relat Res. 1995;(311):262–269. [PubMed] [Google Scholar]
- 5.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9(1):113–119. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 6.Berchuck M, Andriacchi TP, Bach BR, Reider B. Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am. 1990;72(6):871–877. [PubMed] [Google Scholar]
- 7.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61(7):617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma L, Hurwitz DE, Thonar EJ, et al. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum. 1998;41(7):1233–1240. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 9.Creaby MW, Bennell KL, Hunt MA. Gait differs between unilateral and bilateral knee osteoarthritis. Arch Phys Med Rehabil. 2012;93(5):822–827. doi: 10.1016/j.apmr.2011.11.029. [DOI] [PubMed] [Google Scholar]
- 10.Sadeghi H, Allard P, Prince F, Labelle H. Symmetry and limb dominance in able-bodied gait: a review. Gait Posture. 2000;12(1):34–45. doi: 10.1016/s0966-6362(00)00070-9. [DOI] [PubMed] [Google Scholar]
- 11.Van der Straaten JHM, Scholton PMH. Symmetry and periodicity in gait patterns of normal and hiplegic children. In: Easmussen R, Jorgense R, editors. Biomechanics VI. University Park Press; 1978. pp. 287–292. [Google Scholar]
- 12.Hannah RE, Morrison JB, Chapman AE. Kinematic symmetry of the lower limbs. Arch Phys Med Rehabil. 1984;65(4):155–158. [PubMed] [Google Scholar]
- 13.Hamill J, Bates BT, Knutzen KM. Ground reaction forces symmetry during walking and running. Research Quarterly for Exercise and Sport. 1984;55(3):289–293. [Google Scholar]
- 14.Gundersen LA, Valle DR, Barr AE, Danoff JV, Stanhope SJ, Snyder-Mackler L. Bilateral analysis of the knee and ankle during gait: an examination of the relationship between lateral dominance and symmetry. Phys Ther. 1989;69(8):640–650. doi: 10.1093/ptj/69.8.640. [DOI] [PubMed] [Google Scholar]
- 15.Herzog W, Nigg BM, Read LJ, Olsson E. Asymmetries in ground reaction force patterns in normal human gait. Med Sci Sports Exerc. 1989;21(1):110–114. doi: 10.1249/00005768-198902000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Street BD, Gage W. The effects of an adopted narrow gait on the external adduction moment at the knee joint during level walking: evidence of asymmetry. Hum Mov Sci. 2013;32(2):301–313. doi: 10.1016/j.humov.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Teichtahl AJ, Wluka AE, Morris ME, Davis SR, Cicuttini FM. The associations between the dominant and nondominant peak external knee adductor moments during gait in healthy subjects: evidence for symmetry. Arch Phys Med Rehabil. 2009;90(2):320–324. doi: 10.1016/j.apmr.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 18.Sadeghi H. Local or global asymmetry in gait of people without impairments. Gait Posture. 2003;17(3):197–204. doi: 10.1016/s0966-6362(02)00089-9. [DOI] [PubMed] [Google Scholar]
- 19.Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000;133(8):635–646. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- 20.Andriacchi TP, Alexander EJ, Toney MK, Dyrby C, Sum J. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. J Biomech Eng. 1998;120(6):743–749. doi: 10.1115/1.2834888. [DOI] [PubMed] [Google Scholar]
- 21.Blazek K, Asay JL, Erhart-Hledik J, Andriacchi T. Adduction moment increases with age in healthy obese individuals. J Orthop Res. 2013;31(9):1414–1422. doi: 10.1002/jor.22390. [DOI] [PubMed] [Google Scholar]
- 22.Scanlan SF, Chaudhari AM, Dyrby CO, Andriacchi TP. Differences in tibial rotation during walking in ACL reconstructed and healthy contralateral knees. J Biomech. 2010;43(9):1817–1822. doi: 10.1016/j.jbiomech.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bell AL, Pedersen DR, Brand RA. A comparison of the accuracy of several hip center location prediction methods. J Biomech. 1990;23(6):617–621. doi: 10.1016/0021-9290(90)90054-7. [DOI] [PubMed] [Google Scholar]
- 24.Camomilla V, Cereatti A, Vannozzi G, Cappozzo A. An optimized protocol for hip joint centre determination using the functional method. J Biomech. 2006;39(6):1096–1106. doi: 10.1016/j.jbiomech.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 25.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 26.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson NL, Kemp AW, Kotz S. Univariate Discrete Distributions. Hoboken, NJ: Wiley-Interscience; 1993. [Google Scholar]
- 28.Mundermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52(9):2835–2844. doi: 10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- 29.Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32(3):447–457. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 30.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol. 2006;33(11):2271–2279. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.