Abstract
Purpose
To assess the impact of obesity and population attributes on the circadian pattern of cardiac autonomic modulation (CAM) in a population-based sample of adolescents.
Methods
We used data from 421 adolescents who completed the follow-up exam in the Penn State Children Cohort (PSCC) study. CAM was assessed by heart rate variability (HRV) analysis of beat-to-beat normal R-R intervals from a 24-hour ECG, on a 30-minute basis. The HRV indices included frequency domain (HF, LF, and LF/HF ratio), and time domain (SDNN, RMSSD, and HR) variables. Nonlinear mixed-effects models were used to calculate a cosine periodical curve, each has three parameters that quantify its circadian: M (mean levels of the HRV variables), Â (amplitude of the oscillation), and θ (the timing of the highest oscillation).
Results
The mean(SD) age was 16.9(2.2)yrs, with 54% male and 77% white. The mean BMI percentile is 66; with 16% obese (BMI percentile ≥95). Overall, HF (a marker of parasympathetic modulation) gradually increases from late afternoon reaching the peak amplitude around 3:00AM, and then decreasing throughout the daytime until late afternoon. In contrast, obesity had adverse effects on all circadian parameters. The age, sex and race showed varying differences on the CAM circadian parameters. The adjusted means (95%Cls) of M, Â, and θ for HF where 5.99(5.79–6.19), 0.77(0.66–0.89), 3:15(2:15–4:15)AM, and 6.21(6.13–6.29), 0.66(0.61–0.70), 2:45(2:30–3:15)AM for obese and non-obese, respectively.
Conclusion
Circadian pattern of CAM can be quantified by the three cosine parameters. Obesity is associated with lower HRV even in young individuals like children/adolescents.
Keywords: Adolescents, obesity, cardiac autonomic modulation, heart rate variability, circadian
Introduction
Cardiovascular diseases (CVD) in children are becoming more prevalent in conjunction with the rise in childhood obesity [1]. Obese children are more likely to become obese adults, enhancing their risk of developing CVD. In fact, by the year of 2035 the number of additional cardiovascular events attributable to obesity in adolescence is expected to be >100,000 [2]. In addition, childhood obesity is often accompanied by cardiovascular abnormalities, suggesting immediate attention to prevent cardiovascular damage at young age [3].
Heart rate variability (HRV) is used as a noninvasive measurement of cardiac autonomic modulation (CAM) [4]. The balance of sympathetic and parasympathetic modulation regulates HRV. Lower HRV has been associated with CVD morbidity and mortality [5]. In recent years, several epidemiological studies have reported evidence of impaired CAM in obese children, finding a reduction of parasympathetic activity of HRV in the obese as compared to non-obese [6–10]. Nevertheless, previous findings from our group also demonstrated an impaired CAM towards a sympathetic overflow and reduced parasympathetic modulation in obese children [9]. However, these studies examined the effect of obesity on the overall mean levels of HRV without studying its impact on the circadian pattern of HRV.
The circadian pattern of HRV has been described in adults [11–15] and children [16–22]. It can be quantified using a cosine periodic regression model consisting of three cosine function parameters: mean (M), mean levels of a HRV index; amplitude (Â), amplitude of oscillation; and acrophase (θ), the clock time of the highest oscillation. Lack of circadian variation of HRV has been associated with increased risk to cardiovascular events in adults [13]. Previous studies have reported the cosine pattern of HRV in children and young adults at the group-level time-specific average of HRV index [15–16]. However, they did not account for between-subjects variability, or provide reference ranges, e.g. 95%(CIs), of the cosine parameters. To our knowledge, there is no study examining the effect of obesity on the circadian pattern of HRV, using the cosine function parameters M, Â and θ, in adolescents from the general population.
Thus, this study has three objectives: to obtain the quantitative measures of the HRV circadian pattern and their normative ranges of the three cosine parameters, to evaluate the influence of population attributes on the circadian pattern of HRV, and to examine the effect of obesity on the circadian pattern of HRV in a population-based sample of adolescents.
Methods
Study population
We used available data from 421 adolescents who completed the follow-up examination of the Penn State Children Cohort (PSCC) study. The recruitment and examination procedures for the baseline study have been published elsewhere [18]. During 2010–2013, a follow-up examination for 700 participants from phase II of PSCC was conducted. Among these subjects, 421 of them completed the follow-up with a response rate of 60% and a mean follow-up time of 7.7-year. The loss to follow-up was mainly due to subjects moving out of central Pennsylvania. However, no major difference in baseline characteristics was observed between subjects who did or did not participate. During the study period, participants were evaluated overnight in the Clinical Research Center at the Pennsylvania State University College of Medicine (COM) for the following: a complete physical examination; a whole body dual-energy x-ray absorptiometry; a high-fidelity Holter ECG monitor to measure beat-to-beat ECG for 39-hour; a 9-hour fixed-time PSG recording, and overnight fasting, blood, saliva, and urine samples. After released from the overnight stay, they were given the following: 8-day actigraph; a set of questionnaires about habitual behavior; and an activity log. The study protocol was approved by Pennsylvania State University COM IRB. Written informed consents were obtained from participants and their parents if participant was a minor (<18 years old).
Classification of obesity
Participants were weighted with a standard weight scale during their visit. Standing height without shoes was measured with a standard height scale. Body mass index (BMI) was calculated by dividing weight (kg) by height (m2); and age and sex adjusted BMI percentile was calculated based on the 2000 CDC Growth Charts. For this particular analysis, obesity was defined as a binary variable (non-obese= BMI percentile <95th, and obese=BMI percentile≥95th).
Continuous ECG recording
A high-fidelity (sampling frequency 1,000 Hz) 12-lead HScribe Holter System (Mortara Instrument, Inc., Milwaukee, WI) was used for 39-hour beat-to-beat ECG data collection. All recordings started between 5:00PM and 7:00PM. The standardized operation procedures for the PSCC study were followed in the data collection, offline processes, HRV analysis, and interpretation processes. We followed the Holter ECG Data Collection and Analysis Procedures previously described [19], but using 39-hour recording instead of 24-hour.
CAM measures
Out of the 39-hour Holter beat-to-beat ECG data, the first 24-hour (7:00PM of Day-1 to 7:00PM of Day-2) were used for analysis. The normal beat-to-beat RR interval data were divided into 30-minute segments of RR data. Thus, each individual provided 48 segments of 30-minute RR data. The RR data for HRV analysis were processed according to current recommendations [19]. The time and frequency-domain HRV analysis were performed on the normal RR interval data if their total length was >22.5-minute (75% of original data), using the HRV Analysis Software v1.1 [20]. For the frequency-domain HRV analysis we used Fast Fourier Transformation (FFT) previously described [14]. The following HRV indices were calculated as measures of CAM: high frequency range (0.15–0.40Hz, HF), low frequency range (0.04–0.15Hz, LF), the ratio of LF to HF (LF/HF), standard deviation of all RR intervals (SDNN, ms), and the square root of the mean of the sum of the squares of differences between adjacent RR intervals (RMSSD, ms). For statistical analysis, HF and LF were logarithmic transformed.
Covariables
A standardized questionnaire was used for the following individual-level information: demographic variables; medication uses; physician diagnosed chronic disease history. For the purpose of this paper, age was used as a continuous variable; gender (female=0 and male=1) and race (non-Hispanic white=1 and non-white=0) were used as binary variables.
Statistical analysis
Mean (SD) and proportions where used to describe the study population. After excluding individuals who did not have sufficient ECG data, 388 individuals contributed up to 48 segments of 30-minute RR interval data, thus we analyzed 18624 segments total A two-stage analysis was performed to assess the relationship of obesity and population attributes on the circadian pattern of HRV. At stage-1, for each individual we fit the HRV data based on all 48 segments to a cosine periodic regression model [21] using nonlinear least squares:
HRVi(t)=Mi+Ai•cos[2π•(t−θi)/T]+εi(i=1,…,388),
where Mi=average of HRV of the ith subject, Ai=amplitude of HRV of the ith subject around Mi, t=time-specific segment order number (one unit of t=30-minute, with t=1 indicating 7:00PM to7:30PM, 2 indicating 7:30PM to 8:00PM, etc.), T=48 segments, θi=lag from the reference time point (7:00PM) to the time of the zenith of the cosine curve fit to the data of the ith subject, and εi=error term of the ith subject. Thus, from the above cosine model, we obtained the estimated individual-level cosine periodic regression parameters (M, Â, and θ) to quantify the periodicity of the HRV variables. At stage-2, we used random-effects meta-analyses to obtain overall estimates of the 3 parameters and 95%(CIs) to test the associations [22]. To visualize the impact of obesity on these three parameters, we plotted the circadian pattern predicted HF of the entire sample, and stratified by obesity. For the analysis on the effect of obesity on each cosine parameters of HRV, 6 adolescents with type 2 diabetes were excluded. All analyses were performed using SAS version 9.3 software (SAS Institute Inc., Cary, N.C. USA).
Results
Characteristics of study population
From the PSCC study follow-up, 390 participants completed the Holter recording for 39-hour, 2 were excluded due to insufficient ECG data for the HRV analysis. The effective sample size for this study was 388 children (92% of the original 421 children). The characteristics of the study population as well as stratified by gender are presented in Table 1. The prevalence of obesity was 16%. The mean(SD) BMI percentile was 66(28). All HRV indices, with the exception of HR, were lower in females than males.
Table 1.
The study population characteristics and summaries of HRV indices
| Demographics | All (N=388) |
Male (N=206; 54%) |
Female (N=182; 46%) |
|---|---|---|---|
| Age (years) | 16.95 (2.16) | 16.86 (2.15) | 17.05 (2.15) |
| Non-Hispanic White (%) | 76.39 | 78.05 | 74.50 |
| BMI Percentile | 66.34 (28.0) | 64.45 (26.67) | 68.48 (25.73) |
| Obesity (%) | 15.80 | 15.89 | 15.70 |
| HRV Indices*: | |||
| Frequency-domain Variables | |||
| Log of HF (ms2) | 6.17 (1.14) | 6.22 (1.10) | 6.13 (1.19) |
| Log of LF (ms2) | 6.65 (0.78) | 6.74 (0.76) | 6.54 (0.80) |
| LF/HF Ratio | 1.10 (0.20) | 1.11 (0.21) | 1.09 (0.17) |
| Time-domain Variables | |||
| SDNN (ms) | 92.72 (35.05) | 97.03 (36.07) | 87.81 (33.34) |
| RMSSD (ms) | 58.88 (33.68) | 59.96 (32.97) | 57.83 (34.62) |
| Heart Rate (BPM) | 76.56 (16.67) | 75.35 (16.60) | 77.95 (16.63) |
Abbreviations: HRV, heart rate variability; HF, high frequency powers; LF, low frequency powers; RMSSD, the square root of the mean of the sum of the squared differences of the adjacent RR intervals; SDNN, standard deviation of RR intervals.
Continuous variables reported as mean ± SD; binary variables reported as %.
: Overall average of the intra-subject means.
Circadian pattern of HRV variables
The overall means of the three cosine parameters and their 95%(CIs) for each of the HRV indices from the entire sample are presented in Table 2. The acrophases of HF and RMSSD were similar (around 3 AM), and that of LF and SDNN were similar (around 6:00 AM). The acrophase of LF/HF and HR were similar (around 1:00 PM). The tests of the amplitude (Hu: Â=0) were highly significant for each HRV variable, suggesting a significant circadian variation.
Table 2.
The means and their 95% CI of the cosine periodic regression parameters for each HRV index
| Cosine Periodic Parameters | |||
|---|---|---|---|
| HRV Indices | Mean (95% CI) | Amplitude (95% CI) | Acrophase (95%CI)† |
| Frequency-domain Variables | |||
| Log HF (ms2) | 6.16 (6.08–6.24) | 0.68 (0.64–0.73)* | 2:45 (2:30–3:15) AM |
| Log LF (ms2) | 6.65 (6.59–6.70) | 0.33 (0.31–0.35)* | 6:15 (5:45–7:00) AM |
| LF/HF Ratio | 1.10 (1.11–1.09) | 0.10 (0.09–0.11)* | 12:45 (12:15–1:00) PM |
| Time-domain Variables | |||
| SDNN (ms) | 91.9 (89.5–94.2) | 16.8 (15.8–17.9)* | 6:00 (5:30–6:30) AM |
| RMSSD (ms) | 57.8 (55.5–60.1) | 19.9 (18.4–21.3)* | 3:00 (2:30–3:15) AM |
| Heart Rate (BPM) | 77.2 (76.2–78.1) | 14.0 (13.3–14.6)* | 1:30 (1:15–1:45) PM |
Abbreviations: BPM, beats per minute; CIs, confidence intervals; HF, high frequency power; HRV, heart rate variability; LF, low frequency power; Log, logarithm; RMSSD, square root of the mean of the sum of the squares of differences between adjacent RR intervals; SDNN, standard deviation of all RR intervals.
: P value <0.0001 for non-zero amplitude test of the HRV variables.
: Calculated as the unit to peak ± 2 standard errors, and translated into clock time.
Population attributes and HRV circadian pattern
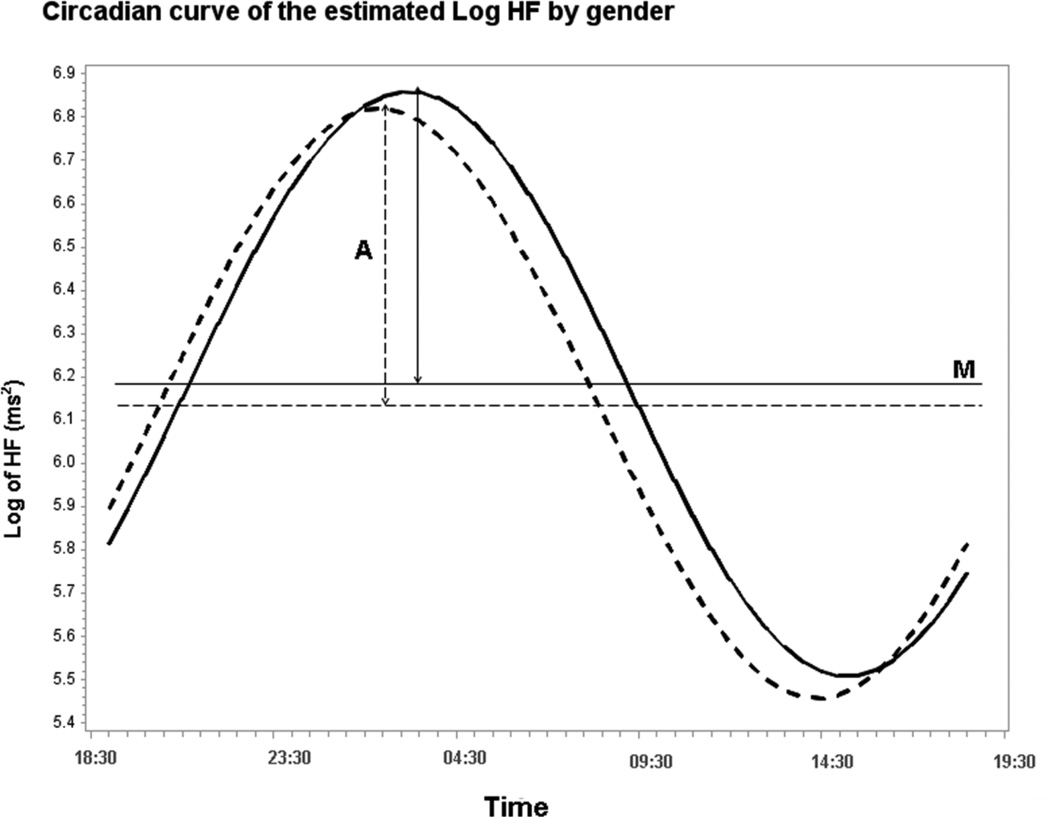
The association between each cosine parameter and population attributes are presented in Table 3. Older age was significantly associated with higher M for LF/HF and lower M for HR; with higher Âs of HF, LF/HF, RMSSD; and higher θ for LF/HF and HR The between gender comparison of the Ms indicated no significant gender difference, except for LF, SDNN and HR. The M was significantly higher in males than in females for LF and SDNN, and lower for HR. For between gender comparisons of the Âs, males showed higher fluctuation amplitude of LF and SDNN. The between gender comparison of the θs indicated no significant gender difference, except for HF. To visualize the gender influence on HRV circadian pattern, we presented a circadian curve of HF by gender in Figure 1, which clearly illustrated that for both gender HF gradually increasing from late afternoon throughout the evening reaching the highest oscillation and gradually decreasing throughout most of the daytime until late afternoon. However, males had later θ of HF, about 1-hour later than females. Non-Hispanic whites had significantly higher M for LF, and higher θ of SDNN suggesting that their θ of SDNN was significantly delayed by over 1-hour, when compared to non-whites. No significant ethnicity difference in the Âs of any HRV variable was found.
Table 3.
The regression coefficient (β) estimates and SE of major population attributes on mean, amplitude and acrophase of the circadian periodic curves of HRV from random-effects meta-analysis
| HRV Indices | |||||||
|---|---|---|---|---|---|---|---|
| Frequency-domain variables | Time-domain variables | ||||||
| Population Attributesa |
Log HF (ms2) | Log LF (ms2) | LF/HF ratio | SDNN (ms) | RMSSD (ms) |
HR (BPM) | |
| β(SE) | β(SE) | β(SE) | β(SE) | β(SE) | β(SE) | ||
| Ageb | Mc | −0.01(0.02) | 0.02(0.01) | 0.006(0.002)** | 0.95(0.54) | 0.26(0.54) | 0.91(0.21)** |
| Âc | 0.03(0.01)** | 0.004(0.005) | 0.004(0.001)** | 0.42(0.25) | 0.93(0.33)** | 0.22(0.15) | |
| θc | 0.04(0.18) | −0.48(0.28) | 0.41(0.16)** | −0.14(0.21) | −0.17(0.18) | 0.23(0.08)** | |
| Male | Mc | 0.04(0.08) | 0.18(0.05)** | 0.02(0.009) | 8.07(2.37)** | 1.08(2.35) | 2.24(0.91)** |
| Âc | −0.004(0.004) | 0.05(0.02)* | −0.009(0.006) | 4.97(1.08)** | 1.38(1.46) | 1.05(0.64) | |
| θc | 1.61(0.81)* | 0.52(1.22) | 0.38(0.72) | −0.65(0.89) | 1.05(0.80) | 0.49(0.36) | |
| Non-Hispanic white | Mc | 0.03(0.09) | 0.12(0.06)** | 0.01(0.01) | 4.45(2.80) | 0.58(2.79) | −1.39(1.08) |
| Âc | −0.05(0.05) | 0.02(0.03) | −0.01(0.01) | 1.13(1.27) | −0.02(1.72) | 0.19(0.75) | |
| θc | 0.59(0.96) | 1.80(1.44) | −0.34(0.85) | 2.23(1.05)* | 0.52(0.95) | −0.60(0.43) | |
Abbreviations: Â, amplitude, BPM, beats per minute; CIs, confidence intervals; HF, high frequency power; HRV, heart rate variability; LF, low frequency power; Log, logarithm; M, mean; RMSSD, square root of the mean of the sum of the squares of differences between adjacent RR intervals; SDNN, standard deviation of all RR intervals; θ, acrophrase time.
All variables were added into the same model.
Age was analyzed as a continuous variable; thus the regression coefficient correspond to the changes for every 1-year increase in age
M, Â, and θ : parameters of the cosine periodic curve mean, amplitude, and acrophase; 1 unit of θ corresponds to 30-minute, with a positive θ of 2 unit indicating 1-hour later.
p-value :
p<0.05;
p<0.01
Figure 1.
Circadian curve of the estimated Log HF by gender. By Gender: Male: β(M)=6.18; β(A)=0.67; β(θ)=03:25. Female: β(M)=6.13; β(A)=0.68; β(θ)=02:25. p-value for the difference: P_M=0.56; P_A= 0.89; P_θ=0.04
Obesity and HRV circadian pattern
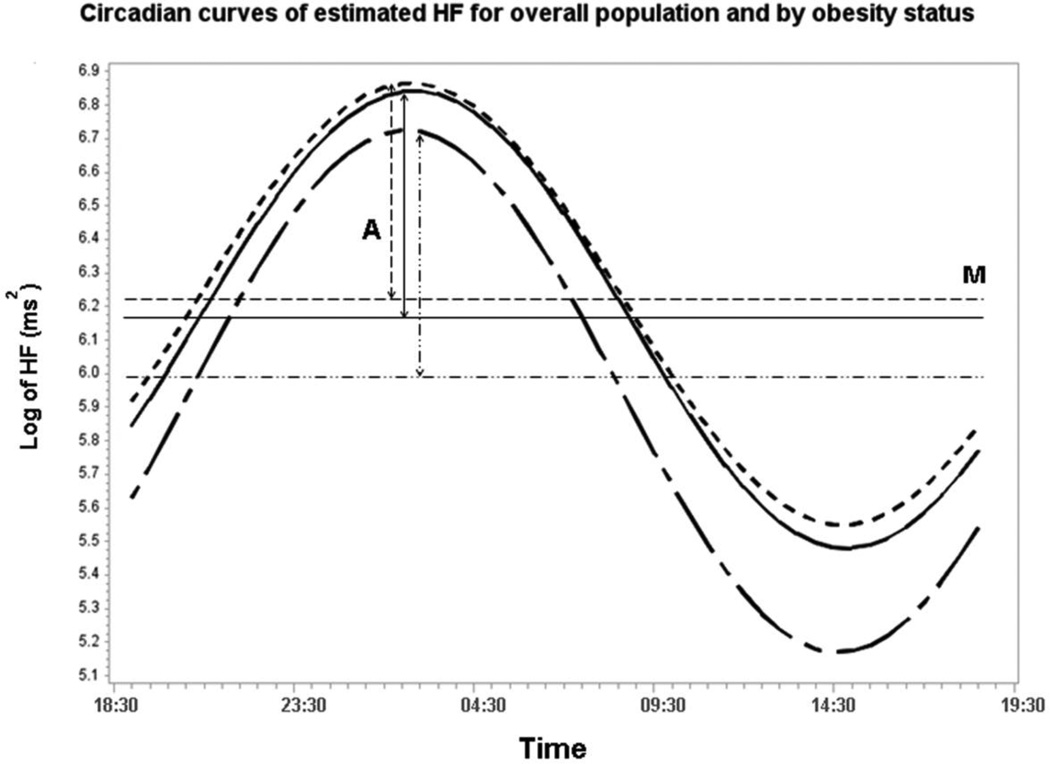
The adjusted means of the cosine parameters and their 95%(CIs) for each HRV index from the entire sample as well as stratified by obesity status are presented in Table 4. In general, obesity was significantly associated with lower M of HF, LF, SDNN, and higher HR; and marginally related to higher LF/HF. No significant association was found on RMSSD. Obesity was significantly associated with higher  of LF and marginally associated with higher  of HF; and with lower θ of HR, suggesting that θ was 30-minute earlier in obese than non-obese adolescents.
Table 4.
Adjusted means of the cosine periodic regression parameters and their 95% CIs for each HRV index from the entire population as well as stratified by obesity status.
| HRV Indices | Overall | Non-Obese | Obese | P value§ |
|
|---|---|---|---|---|---|
| Frequency-domain Variables | |||||
| Log HF (ms2) | M | 6.17 (6.10–6.25) | 6.21 (6.13–6.29) | 5.99 (5.79–6.19) | 0.020 |
| Â | 0.67 (0.63–0.72)* | 0.66 (0.61–0.70)* | 0.77 (0.66–0.89)* | 0.058 | |
| θ† | 3:00 (2:30–3:15) AM | 2:45 (2:30–3:15) AM | 3:15 (2:15–4:15) AM | 0.365 | |
| Log LF (ms2) | M | 6.65 (6.60–6.71) | 6.68 (6.62–6.73) | 6.53 (6.39–6.66) | 0.046 |
| Â | 0.33 (0.31–0.35)* | 0.32 (0.29–0.34)* | 0.41 (0.35–0.46)* | 0.003 | |
| θ† | 6:15 (5:45–6:45) AM | 6:15 (5:45–7:00) AM | 5:45 (4:15–7:15) AM | 0.453 | |
| LF/HF Ratio | M | 1.10 (1.09–1.11) | 1.10 (1.09–1.10) | 1.12 (1.10–1.14) | 0.059 |
| Â | 0.10 (0.09–0.11)* | 0.10 (0.09–0.11)* | 0.11 (0.09–0.12)* | 0.372 | |
| θ† | 12:45 (12:15–1:00) PM | 12:45 (12:15–1:00) PM | 12:45 (11:45–1:30) PM | 0.955 | |
| Time-domain Variables | |||||
| SDNN (ms) | M | 92.33 (90.04–94.62) | 93.42 (90.94–95.90) | 86.90 (80.99–92.82) | 0.047 |
| Â | 16.79 (15.79–17.80)* | 16.67 (15.58–17.77)* | 17.76 (15.15–20.37)* | 0.453 | |
| θ† | 6:00 (5:30–6:15) AM | 6:00 (5:30–6:30) AM | 5:45 (4:45–7:00) AM | 0.878 | |
| RMSSD (ms) | M | 58.34 (56.02–60.65) | 59.10 (56.59–61.62) | 54.05 (48.06–60.05) | 0.128 |
| Â | 19.92 (18.53–21.31)* | 19.64 (18.14–21.15)* | 21.65 (18.04–25.26)* | 0.316 | |
| θ† | 3:00 (2:30–3:30) AM | 3:00 (2:30–3:15) AM | 3:30 (2:30–4:30) AM | 0.215 | |
| Heart Rate (BPM) | M | 77.03 (76.16–77.90) | 76.39 (75.41–77.28) | 80.48 (78.25–82.70) | 0.001 |
| Â | 13.86 (13.27–14.46)* | 14.02 (13.38–14.68)* | 13.01 (11.47–14.56)* | 0.234 | |
| θ† | 1:30 (1:30–1:45) PM | 1:45 (1:30–1:45) PM | 1:15 (12:45–1:30) PM | 0.048 |
Abbreviations: Â, amplitude, BPM, beats per minute; CIs, confidence intervals; HF, high frequency power; HRV, heart rate variability; LF, low frequency power; Log, logarithm; M, mean; RMSSD, square root of the mean of the sum of the squares of differences between adjacent RR intervals; SDNN, standard deviation of all RR intervals; θ, acrophrase time.
All models were adjusted for age, gender, and race.
: p value compering the difference between obese and non-obese.
: p<0.0001 for zero amplitude test of the HRV variables.
: Calculated as the unit to peak ± 2 standard errors, and translated into clock time.
Figure 2 presents the circadian patterns of HF from the entire population as well as stratified by obesity status and adjusted by major covariables. The predicted circadian pattern of HF in the entire sample showed the parasympathetic modulation gradually increasing from late afternoon throughout the evening reaching θ at 3:00AM, and gradually decreasing throughout most of the daytime until late afternoon. For obesity status it shows the same patterns on the parasympathetic modulation as the entire sample. Obese adolescents had later θ in HF, about 30-minute later than non-obese, even after adjusting for major covariables.
Figure 2.
Circadian curves of estimated HF for overall population and by obesity status. Overall (adjusted for age, race, and sex): β(M)=6.17; β(A)=0.67; β(θ)=03:00, all p < 0.05. By Obesity (adjusted for age, race, and sex): No: β(M)=6.21; β(A)=0.66; β(θ)=02:45. Yes: β(M)=5.99; β(A)=0.78; β(θ)=03:15. p-value for the difference: P_M=0.02; P_A= 0.06; P_θ=0.36
Discussion
This is the first study to define the circadian pattern of HRV and provide its normative ranges in a population-based sample of adolescents. Furthermore, we demonstrated that male and older adolescents have delayed circadian pattern of HRV, while ethnicity appears to play a less relevant role. Importantly, we show that adolescent obesity is associated with an overall impairment of HRV as well as with a shift in its circadian pattern. These findings support the need to address obesity in earlier stages of life to prevent CVD.
We first quantitatively describe the HRV circadian pattern by using a cosine periodic regression model, and obtain the normative range of the three cosine parameters. Our results shown in Table 2 demonstrated that the circadian patterns of adolescents can be captured by these cosine parameters. In our population, HF, LF, SDNN, and RMSSD variables follow similar circadian pattern (Figure 2)—increasing in the evening, reaching the acrophase highest level early morning, and then decreasing during the morning until reaching the lowest levels in the afternoon. On the other hand, LF/HF and HR variables showed an opposite diurnal pattern—decreasing during the evening, reaching the lowest levels after midnight, then increasing in the morning until reaching the acrophase in the afternoon, to then turning downwards again. In addition, the tests of non-zero amplitude, suggesting a significant day–night circadian variation, were highly significant for every HRV variable.
The circadian patter of CAM in healthy adults has been previously quantitatively described using the 3 cosine parameters [14–15]. To our knowledge, there is one previous study in children that examined the circadian pattern of HRV as a cosine function [16]. They identified a significant circadian variation in HRV from late infancy; characterized by a rise during sleep. However, they used time-specific averages from the sample, and estimated the cosine parameters from there. In contrast, we used a two-stage analysis allowing us to capture the individual variation of HRV over time per participant and the between individual differences in the circadian variation at any time point, and provide 95%(CIs) for each cosine parameters. Compared to adults [14], adolescents have higher M levels of HRV indices, except for LF/HF, indicative of a healthier CAM profile, approximately 30-minute earlier θ on parasympathetic HRV indices, and around 1-hour delay of the θ on the sympathetic HRV indices. Our findings can be used to pursue studies on the CAM effects of various CVD risk factors (e.g., obesity).
We examine the influences of the population attributes on the cosine parameters of HRV. Our findings suggest that males have significantly higher Ms of LF, SDNN, and lower Ms of HR, higher  of HF and SDNN, and delayed θ (1-hour) in HF than female. Available reports in adolescents on gender differences on HRV are controversial, reporting females with significantly lower [23–24], or greater [25–26] values of HRV than males. These inconsistences in the findings from different studies could be due to confounding factors such as data collection, HRV recording time, hormonal differences between genders, and menstrual cycle in females. However, similar to our findings, a study in adolescents found that males have higher SDNN than females [24]. To our knowledge, we are the first group examining the influence of gender on  and θ in adolescents. These findings are similar to previous report from our group showing that middle-age males have higher  of HRV than females, and that the θ for LF/HF is significantly delayed by about 3-hour in males [14]. Furthermore, in our population the impact of older age on higher LF/HF and lower HF Ms, are consistent with previous studies in children [24,26] and adults [14]. With increased age we found higher  for HF and RMSSD, and higher θ for LF/HF and HR. No data in adolescent is available on the effect of age on Â, and θ. We did not find significant ethnic effects on the cosine parameters; however, θ for SDNN was significantly delayed by 1-hour in non-Hispanic whites as compared to non-whites. The influence of ethnicity on HRV in children have been inconsistent [23,24,26], with studies reporting that African American youth have lower HRV [23], Asian have higher LF/HF [26], or that there are no significant ethnic differences [27]. Although we weren’t able to find any significant ethnic differences on  and θ, we are the first group analyzing the ethnicity and these parameters on adolescents.
Based on recent reports that childhood obesity increases the risk of CVD, we further examined the effect of obesity on the 3 cosine parameters. After adjustment for major covariables, obesity was significantly associated with lower Ms for HF, LF, SDNN, and higher Ms for LF/HF and HR. Our results are consistent with previous reports studying CAM in obese children, indicating a significant reduction in HRV [7–9]. In terms of the circadian pattern of HRV, obesity was significantly associated with higher  of LF, and the θ of HR in obese adolescents was 30-minute earlier than in non-obese. Furthermore, Figure 2 demonstrates that obese adolescents have later θ than non-obese. To our knowledge, the effects of obesity in healthy adolescents on the circadian  and θ of HRV have not been reported in the literature, making this the first study examining the effects of childhood obesity on these parameters of HRV. This is of importance since we know that impaired CAM is a predictor of CVD morbidity and mortality in adults [28–30]. Thus, evaluating these parameters of CAM could help in the early identification of children/adolescent at risk of CVD.
To obtain normal circadian pattern of HRV in our sample of adolescents, we excluded individuals with/or at risk for diabetes from the obesity and cosine parameters analysis. Therefore, the generalizability of our data to individuals with diabetes may be limited. Other limitation is that from our data we cannot establish a temporal relationship. Thus, a longitudinal study is needed to investigate the effect of obesity on the circadian parameters of CAM. Also, we did not account for the influence of hormones on gender differences. In addition, for this particular analysis we did not account for central obesity measurements like waist circumference, and waist-to-hip ratio. However, several strengths are worth mentioning. The 24-hour ECG data was acquired at daytime and nighttime. In humans, the autonomic activity shows a circadian rhythm towards a parasympathetic activity during the night and a prevalence of sympathetic activity during the day. Therefore, the HRV indices collected are representative of day-night-time HRV. Distinguished from previous publication, which primarily analyzed short-time HRV variables in children [19], we utilized cosine parameters to fit individual-level models to 24-hour of HRV data to get individual-level M, Â and θ, of each HRV variable. We were able to collect long duration of continuous ECG recording, and successfully acquired HRV analysis on 92% of the follow-up PSCC sample.
In this population-based sample of healthy adolescents, the HRV can be quantified not only by the mean HRV values, but also by the circadian of HRV through cosine periodic parameters like— Â, and θ. The HRV variables, exhibit a distinct circadian rhythm over a 24-hour period. Furthermore, population attributes, are associated with the HRV cosine circadian parameters. Finally, our data showed that general obesity is associated with lower HRV even in young individuals like children/adolescents; demonstrating that obesity associated alterations in the cardiovascular autonomic activity are already occurring in healthy young adolescents.
Acknowledgments
The authors gratefully acknowledge the adolescents and their parents who participated in this study. This project was supported by National Institutes of Health (NIH) grants: 1 R01 HL 097165, R01 HL63772, R21HL087858, and the Penn State CTSI Grant UL Tr000127. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of interest
The authors declare that they have no conflict of interest.
Reference
- 1.Crowley DI, Khoury PR, Urbina EM, Ippisch HM, Kimball TR. Cardiovascular impact of the pediatric obesity epidemic: higher left ventricular mass is related to higher body mass index. J Pediatr. 2011;158:709–714. e1. doi: 10.1016/j.jpeds.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 2.Bibbins-Domingo K, Coxson P, Pletcher MJ, Lightwood J, Goldman L. Adolescent overweight and future adult coronary heart disease. N Engl J Med. 2007;357:2371–2379. doi: 10.1056/NEJMsa073166. [DOI] [PubMed] [Google Scholar]
- 3.Koopman LP, McCrindle BW, Slorach C, et al. Interaction between myocardial and vascular changes in obese children: a pilot study. J Am Soc Echocardiogr. 2012;25:401–410. e1. doi: 10.1016/j.echo.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 4.Kleiger RE, Stein PK, Bigger JT. Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol. 2005;10:88–101. doi: 10.1111/j.1542-474X.2005.10101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liao D, Barnes RW, Chambless LE, Simpson RJ, Jr, Sorlie P, Heiss G. Population based study of heart rate variability and prevalent myocardial infarction – The ARIC Study. J Electrocardiol. 1996;29:189–198. doi: 10.1016/s0022-0736(96)80082-3. [DOI] [PubMed] [Google Scholar]
- 6.Cote AT, Harris KC, Panagiotopoulos C, Sandor GG, Devlin AM. Childhood obesity and cardiovascular dysfunction. J Am Coll Cardiol. 2013;62/15:1309–1319. doi: 10.1016/j.jacc.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 7.Tonhajzerova I, Javorka M, Trunkvalterova Z, et al. Cardio-respiratory interaction and autonomic dysfunction in obesity. J Physiol Pharmacol. 2008;59/6:709–718. [PubMed] [Google Scholar]
- 8.Vanderlei LC, Pastre CM, Freitas IF, Jr, Godoy MF. Analysis of cardiac autonomic modulation in obese and eutrophic children. Clinics. 2010;65:789–792. doi: 10.1590/S1807-5932201000080009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodriguez-Colon SM, Bixler EO, Li X, Vgontzas AN, Liao D. Obesity is associated with impaired cardiac autonomic modulation in children. Int J Pediatr Obes. 2011;6:128–134. doi: 10.3109/17477166.2010.490265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lazarova Z, Tonhajzerova I, Trunkvalterova Z, et al. Baroreflex sensitivity is reduced in obese normotensive children and adolescents. Can J Physiol Pharmacol. 2009;87:565–571. doi: 10.1139/y09-041. [DOI] [PubMed] [Google Scholar]
- 11.Li X, Shaffer ML, Rodríguez-Colón SM, et al. Systemic inflammation and circadian rhythm of cardiac autonomic modulation. Auton Neurosci. 2011;162:72–76. doi: 10.1016/j.autneu.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rodríguez-Colón SM, Li X, Shaffer ML, et al. Insulin resistance and circadian rhythm of cardiac autonomic modulation. Cardiovasc Diabetol. 2010;9:85. doi: 10.1186/1475-2840-9-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kardelen F, Akcurin G, Ertug H, Akcurin S, Bircan I. Heart rate variability and circadian variations in type 1 diabetes mellitus. Pediatr Diabetes. 2006;7:45–50. doi: 10.1111/j.1399-543X.2006.00141.x. [DOI] [PubMed] [Google Scholar]
- 14.Li X, Shaffer ML, Rodriguez-Colon S, et al. The circadian pattern of cardiac autonomic modulation in a middle-aged population. Clin Auton Res. 2011;21/3:143–150. doi: 10.1007/s10286-010-0112-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakagawa M, Iwao T, Ishida S, et al. Circadian rhythm of the signal averaged electrocardiogram and its relation to heart rate variability in healthy subjects. Heart. 1998;79:493–496. doi: 10.1136/hrt.79.5.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Massin MM, Maeyns K, Withofs N, Ravet F, Gerard P. Circadian rhythm of heart rate and heart rate variability. Arch Dis Child. 2000;83:179–182. doi: 10.1136/adc.83.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bilan A, Witczak A, Palusiński R, Myśliński W, Hanzlik J. Circadian rhythm of spectral indices of heart rate variability in healthy subjects. J Electrocardiol. 2005;38/3:239–243. doi: 10.1016/j.jelectrocard.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 18.Bixler EO, Vgontzas AN, Lin HM, et al. Blood pressure associated with sleep-disordered breathing in a population sample of children. Hypertension. 2008;52/5:841–846. doi: 10.1161/HYPERTENSIONAHA.108.116756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93:1043–1065. [PubMed] [Google Scholar]
- 20.Niskanen JP, Tarvainen MP, Ranta-Aho PO, Karjalainen PA. Software for advanced HRV analysis. Comput Methods Programs Biomed. 2004;76/1:73–81. doi: 10.1016/j.cmpb.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 21.D’Negri CE, Marelich L, Vigo D, et al. Circadian periodicity of heart rate variability in hospitalized angor patients. Clin Auton Res. 2005;15:223–232. doi: 10.1007/s10286-005-0280-9. [DOI] [PubMed] [Google Scholar]
- 22.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 23.Faulkner MS, Hathaway D, Tolley B. Cardiovascular autonomic function in healthy adolescents. Heart Lung. 2003;32/1:10–22. doi: 10.1067/mhl.2003.6. [DOI] [PubMed] [Google Scholar]
- 24.Wang X, Thayer JF, Treiber F, Snieder H. Ethnic differences and heritability of heart rate variability in African- and European American youth. Am J Cardiol. 2005;96/8:1166–1172. doi: 10.1016/j.amjcard.2005.06.050. [DOI] [PubMed] [Google Scholar]
- 25.Antelmi I, de Paula RS, Shinzato AR, Peres CA, Mansur AJ, Grupi CJ. Influence of age, gender, body mass index, and functional capacity on heart rate variability in a cohort of subjects without heart disease. Am J Cardiol. 2004;93:381–385. doi: 10.1016/j.amjcard.2003.09.065. [DOI] [PubMed] [Google Scholar]
- 26.Reed KE, Warburton DE, Whitney CL, McKay HA. Differences in heart rate variability between Asian and Caucasian children living in the same Canadian community. Appl Physiol Nutr Metab. 2006;31/3:277–282. doi: 10.1139/h05-015. [DOI] [PubMed] [Google Scholar]
- 27.Franke WD, Lee K, Buchanan DB, Hernandez JP. Blacks and whites differ in responses, but not tolerance, to orthostatic stress. Clin Auton Res. 2004;14:19–25. doi: 10.1007/s10286-004-0155-5. [DOI] [PubMed] [Google Scholar]
- 28.Liao D, Sloan RP, Cascio WE, et al. The multiple metabolic syndrome is associated with lower heart rate variability -- The ARIC Study. Diabetes Care. 1998;21:2116–2222. doi: 10.2337/diacare.21.12.2116. [DOI] [PubMed] [Google Scholar]
- 29.Dekker JM, Crow RS, Folsom AR, et al. Low heart rate variability in a two minute rhythm strip predicts risk of coronary heart disease and mortality from several causes -- The ARIC Study. Circulation. 2000;102:1239–1244. doi: 10.1161/01.cir.102.11.1239. [DOI] [PubMed] [Google Scholar]
- 30.Liao D, Carnethon MR, Evans GW, Cascio WE, Heiss G. Lower Heart Rate Variability Is Associated with the Development of Coronary Heart Disease in Individuals with Diabetes - The ARIC Study. Diabetes. 2002;51:3524–3531. doi: 10.2337/diabetes.51.12.3524. [DOI] [PubMed] [Google Scholar]