Abstract
Background
A recent proposed modification in surgical technique in total knee arthroplasty (TKA) has been the introduction of the “kinematically aligned” TKA, in which the angle and level of the posterior joint line of the femoral component and joint line of the tibial component are aligned to those of the “normal,” pre-arthritic knee. The purpose of this study was to establish the relationship of the posterior femoral axis of the “kinematically aligned” total knee arthroplasty (TKA) to the traditional axes used to set femoral component rotation.
Methods
114 consecutive, unselected patients with preoperative MRI images undergoing TKA were retrospectively reviewed. The transepicondylar axis (TEA), posterior condylar axis (PCA), antero-posterior axis (APA) of the trochlear groove, and posterior femoral axis of the kinematically aligned TKA (KAA) were templated on axial MRI images by two, independent observers. The relationships between the KAA, TEA, APA, and PCA were determined, with a negative value indicating relative internal rotation of the axis.
Results
On average, the KAA was 0.5° externally rotated relative to the PCA (minimum of -3.6°, maximum of 5.8°), -4.0° internally rotated relative to the TEA (minimum of -10.5°, maximum of 2.3°), and -96.4° internally rotated relative to the APA (minimum of -104.5°, maximum of -88.5°). Each of these relationships exhibited a wide range of potential values.
Conclusions
Using a kinematically aligned surgical technique internally rotates the posterior femoral axis relative to the transepicondylar axis, which significantly differs from current alignment instrument targets.
Keywords: kinematic alignment, total knee arthroplasty, femoral rotation, transepicondylar axis, flexion-extension axis
Introduction
Total knee arthroplasty (TKA) has been highly successful in relieving pain and restoring function in patients with degenerative joint disease, with numerous studies demonstrating implant survivorship of greater than 90% at 10 years and beyond (1-3). However, as the volume of TKAs performed in the United States continues to increase, especially in the younger population, concerns remain regarding the expectations and functional demands placed on these prostheses (4-7). Recent studies focusing on patient satisfaction as the primary outcome measure have shown the percentage of patients who remain “unsatisfied” following a TKA to be as high as 15% to 30%, with higher rates of dissatisfaction seen in younger patients (less than 65 years old) (7-10). Parvizi et al. demonstrated a high prevalence of residual symptoms in young, active patients, as only 66% of patients stated their knee to feel “normal,” with persistent pain in 33%, stiffness in 41%, and grinding or other noise in 33% (10).
The long-held tenet in TKA is that a successful outcome is dependent on achievement of a neutral mechanical axis of the lower extremity with the tibial and femoral components aligned perpendicular to the mechanical axis in the coronal plane. However, the significance of a neutral, mechanical alignment both on overall component survivorship and on clinical function has recently been questioned (11-13). Furthermore, the introduction of the concept of “constitutional varus” has hypothesized that restoration of a neutral, mechanical alignment may in fact be “unnatural” for a substantial proportion of the population, thus in part contributing to residual symptoms and dissatisfaction (12, 14, 15). A recent modification in surgical technique has been to attempt to align the angle and level of the femoral component, posterior joint line of the femoral component, and joint line of the tibial component to those of the “normal,” pre-arthritic knee (14). This modification has been introduced as the “kinematically aligned” TKA, and preliminary results have been encouraging (16-18). Internal-external rotation of the femoral component in the axial plane is focused on restoration of the pre-arthritic, posterior femoral joint line based on the defined thickness of the femoral component to be used. This is in contrast to the classical, mechanically aligned TKA, in which axial rotation of the femoral component is set by aligning the posterior joint line relative to one of three axes: 1) perpendicular to the anteroposterior axis of the trochlear groove (Whiteside's line) (19), 2) parallel to the transepicondylar axis (20, 21), or 3) 3° externally rotated to the posterior condylar axis (22).
Femoral component malrotation continues to be a concern in TKA, and reproducible and accurate positioning in the axial plane remains elusive due to the anatomic variability of these traditional landmarks, and the associated difficulty in identifying them intraoperatively (23-26). Furthermore, whether these traditional landmarks should even be targeted in TKA has been questioned, as Eckhoff et al. has demonstrated that they do not accurately reproduce the true flexion-extension axis of the knee (25, 27). To our knowledge, the effect of “kinematically aligning” a TKA on rotation of the femoral component compared to these traditional axes has not yet been reported and warrants investigation.
The purpose of this study was to establish the relationship of the posterior femoral axis of the kinematically aligned TKA to the traditional axes used to determine femoral component rotation. Our hypothesis is that use of a kinematically aligned surgical technique will lead to a posterior femoral axis that is significantly different than current alignment instrument targets.
Materials and Methods
This study is an IRB-approved, retrospective review of a prospectively collected registry of patients undergoing total knee arthroplasty at a single institution. Inclusion criteria for the study were patients over the age of 18 years old, with a primary diagnosis of osteoarthritis or inflammatory arthritis, undergoing a unilateral TKA with preoperative magnetic resonance imaging (MRI) scans as part of the preparation for use of patient specific cutting guides (Signature™, Biomet Inc., Warsaw, IN, USA). From November 2007 to October 2012, a consecutive series of 114 patients who met the inclusion criteria were identified (50 males, 64 females; mean age 64 years, range 46 to 90 years).
All MRIs were obtained using a 1.5 Tesla, high resolution, lower extremityimaging coil, and axial, T2 weighted, fast-spin, fat saturation images with slice thicknesses of 6mm were analyzed (General Electric Medical Systems, Milwaukee, Wisconsin, USA). The axial image most prominently demonstrating the medial and lateral epicondyles was selected for digital landmarking of the posterior condylar axis (PCA), the transepicondylar axis (TEA), and the anteroposterior axis (APA) of the distal femur. A line drawn tangent to the most prominent cartilaginous surfaces of the medial and lateral posterior femoral condyles was used to define the PCA (22). For the TEA, a line was drawn through the two most prominent points on the femoral epicondyles, correlating with the previously defined clinical transepicondylar axis (28). For the APA of the trochlear groove, a line was drawn through the deepest point on the trochlear groove and the center of the intercondylar notch (19) (Figure 1).
Figure 1.

Axial MRI image demonstrating landmarking of the anteroposterior axis (APA), transepicondylar axis (TEA), posterior femoral axis of the kinematically aligned TKA (KAA), and the posterior condylar axis (PCA).
For each MRI, templating of the femoral resections for a kinematically aligned TKA, using a femoral implant with a symmetric thickness of 9mm, was performed as described by Howell et al (18, 29). In a kinematically aligned TKA, alignment of the femoral component with the “normal” distal and posterior joint lines is confirmed when the thicknesses of the distal and posterior femoral resections, after correcting for cartilage loss, bone wear, and kerf of the saw blade, equal the thicknesses of the distal and posterior condyles of the femoral implant (14, 17, 18). As this study focused on alignment of the posterior femoral axis in the axial plane, a brief description of templating the depth of resection of the posterior condyles is described, however a similar method can be used for assessing the resection depths required for the distal femoral condyles (29).
For each MRI, the presence of cartilage loss or bone wear of the posterior condyles was assessed. The relative presence of posterior cartilage wear between the medial and lateral compartments was determined by drawing a best-fit circle on the cartilaginous surface of the nonaffected compartment, and propagating this circle to the affected compartment on sagittal MRI images (Figure 2). If cartilage loss was present, a bony resection of 6mm was proposed for that respective condyle. Thus, the depth of resection (6mm), amount of cartilage wear (approximately 2mm), and kerf of the saw blade (approximately 1mm), would sum to equal the 9mm thickness of the implant's femoral condyle (29). The native, cartilage thickness of the posterior condyles was presumed to be 2mm based on prior MRI assessments (14). In contrast, in the nonaffected compartment with wellpreserved cartilage, an 8mm resection was proposed, accounting only for the kerf of the saw blade (1mm). Two points were then marked on the axial MRI image, signifying the proposed depths of resection for both the medial and lateral, posterior condyles. A line connecting these two points represented the posterior femoral axis of the kinematically aligned TKA (KAA), which was landmarked on the same axial image as the TEA, PCA, and APA (Figure 1).
Figure 2.
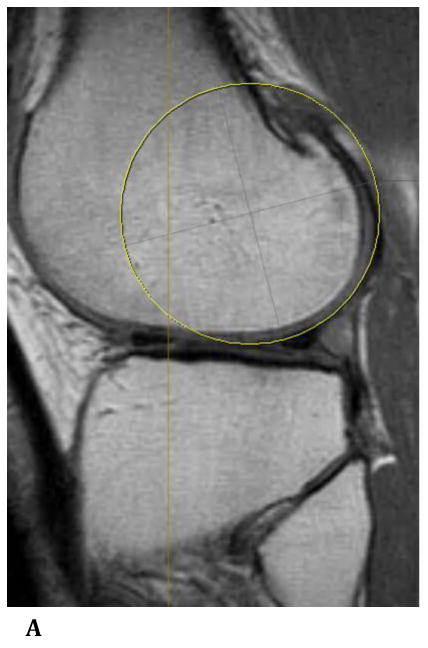

Sagittal plane, T1 weighted MRI images demonstrating a best-fit circle around the cartilaginous surface of the nonaffected lateral femoral condyle (a), and propagation of this circle to the affected medial femoral condyle (b). Cartilage wear is appreciated at the posterior aspect of the medial femoral condyle.
A single observer selected the axial MRI on which all rotational axes were to be landmarked, templated all MRIs for placement of a kinematically aligned TKA, and proposed the surgical plan for the KAA. All measurements were then performed by two, independent observers, who landmarked the TEA, PCA, APA, and followed the proposed surgical plan for the KAA. Using the angle measurement tool, the relationships between the KAA, TEA, APA, and PCA were determined. For convention, a negative value indicated relative internal rotation of the axis, while a positive number indicated relative external rotation.
Statistical Analysis
All data was collected and analyzed utilizing Microsoft Excel software (Microsoft Corporation, Redmond, WA). Interobserver correlation coefficients were graded using previously described semi-quantitative criteria: excellent for 0.9≤r≤1.0, good for 0.7≤r≤0.89, fair/moderate for 0.5≤r≤0.69, low for 0.25≤r≤0.49, and poor for 0.0≤r≤0.24 (30).
Results
A wide range of variability was appreciated in the relationships between the PCA, TEA, and APA. On average, the TEA was 4.5° externally rotated relative to the PCA, with a standard deviation of 2.4°. The range of values was 11.7° (minimum of -1.3°, maximum of 10.4°). Similarly, on average, the APA was 96.9° externally rotated relative to the PCA, with a standard deviation of 3.2°. The range of values was 15.6° (minimum of 90°, maximum of 105.6°). Lastly, on average, the APA was 92.4° externally rotated relative to the TEA, with a standard deviation of 3.5°. The range of values was 18.8° (minimum of 84.1°, maximum of 102.9°).
On average, the KAA was 0.5° externally rotated relative to the PCA, with a standard deviation of 1.8°. The range of values was 9.4° (minimum of -3.6°, maximum of 5.8°). The KAA was, on average, -4.0° internally rotated relative to the TEA, with a standard deviation of 2.5°. The range of values was 12.8° (minimum of -10.5°, maximum of 2.3°). Lastly, the KAA was on average -96.4° internally rotated relative to the APA, with a standard deviation of 3.3° (minimum of -104.5°, maximum of -88.5°). The significant variability of these relationships in this consecutive series of unselected patients is appreciated in Figure 3. A summary of the relationship of the KAA to the PCA, TEA, and APA is presented in Table 1. Using semi-quantitative criteria, interobserver correlation coefficients were fair/moderate (r=058 to 0.65) for measurement of the relationships between the KAA, PCA, TEA, and APA.
Figure 3.
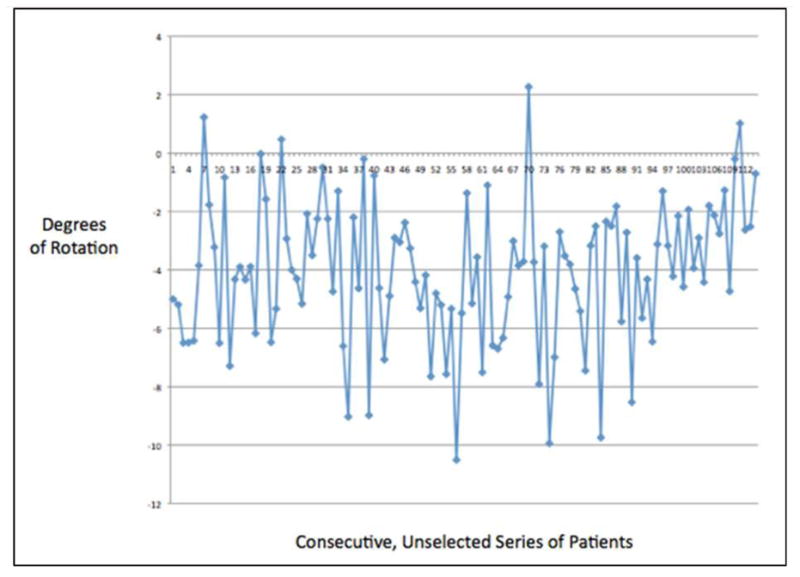
Line graph demonstrating the variability in the relationship between the KAA and the TEA in a consecutive series of unselected patients undergoing TKA. KAA = posterior femoral axis of the kinematically aligned TKA, TEA = transepicondylar axis.
Table 1.
Summary of the relationship between the posterior femoral axis of the kinematically aligned TKA, to the traditional distal femoral axes used to set femoral component rotation. KAA = posterior femoral axis of the kinematically aligned TKA, PCA = posterior condylar axis, TEA = transepicondylar axis, APA = anteroposterior axis.
| Mean | Standard Deviation | Minimum Value | Maximum Value | |
|---|---|---|---|---|
| KAA relative to PCA | 0.5° | 1.8° | -3.6° | 5.8° |
| KAA relative to TEA | -4.0° | 2.5° | -10.5° | 2.3° |
| KAA relative to APA | -96.4° | 3.3° | -104.5° | -88.5° |
Discussion
This study demonstrates that on average, the KAA is only 0.5° externally rotated relative to the PCA, -4.0° internally rotated relative to the TEA, and -96.4° internally rotated relative to the APA, with each of these relationships exhibiting a wide range of potential values. Therefore, our results support our hypothesis and demonstrate the posterior femoral axis of the kinematically aligned TKA to be internally rotated relative to the traditional axes used to set femoral component rotation in the mechanically aligned TKA.
There were several limitations to this study, which should be discussed prior to interpretation of our results. First, one technique of setting femoral component rotation not accounted for in this study is the gap balancing method (31), which relies on initially balancing the extension gap, then setting femoral component rotation to create a balanced flexion gap relative to the tibial resection. However, the purpose of this study was to compare the use of traditional anatomic landmarks for a mechanically aligned TKA versus the kinematically aligned TKA. Second, this study presents a relatively small series of patients. However, our sample size was limited by inclusion of a consecutive, unselected series of patients who had MRI examinations prior to their total knee arthroplasties. A third limitation is that this study presents the theoretical, proposed resections of a kinematically aligned TKA, and is not a clinical representation of the actual alignment achieved intraoperatively using this technique. However, as this specific aspect of the technique had not yet been assessed, we believed it was prudent to assess these proposed resections on preoperative imaging to determine its potential effect on rotational alignment of the femoral component. Furthermore, only one observer templated the proposed femoral resections for a kinematically aligned TKA, and thus there may be some variability in the proposed resections depths. However, this technique has previously been well described in the literature (14, 16), and we felt that greater interobserver reliability would potentially be seen in the actual measurements of the relationships between each, respective axis.
The concept of the kinematically aligned TKA has recently received attention, as it contrasts the long-held tenet of the mechanically aligned TKA, in which the goal is to create distal femoral and proximal tibial resections perpendicular to each, respective mechanical axis. The concept of an anatomic restoration of the joint line was initially introduced by Hungerford and Krackow, with the Porous-Coated Anatomical (PCA) Knee, often resulting in an anatomic, proximal tibial resection of 3° of varus (32). The goal of the kinematically aligned TKA is to restore the prearthritic, orthogonal 3-D orientation of the 3 axes that describe normal knee kinematics: 1) the transverse axis about which the patella flexes and extends, 2) the transverse axis about which the tibia flexes and extends, and 3) the longitudinal axis about which the tibia and femur internally and externally rotate (17). The impetus for the development of this technique was in part due to recognition of the substantial proportion of patients who remain unsatisfied following TKA (8). Preliminary results with the use of this surgical technique have been encouraging (14, 17, 18, 29). Dossett et al., in a randomized controlled trial comparing 41 kinematically aligned and 41 mechanically aligned TKAs, demonstrated significant improvements in the Western Ontario and McMaster Universities Osteoarthritis Index Score, Oxford Knee Score, Knee Society Score, and overall knee flexion in the kinematically aligned cohort at 6 months follow-up (17). However, several questions remain regarding this technique, including its impact on long-term component survivorship and on rotational alignment of the femoral component and subsequent patellofemoral tracking.
This study focused on the transverse axis about which the tibia flexes and extends, or the posterior femoral axis, and showed that the flexion-extension axis (FEA) of the kinematically aligned TKA is approximately 4° internally rotated relative to the transepicondylar axis: a commonly used target for the mechanically aligned TKA. Traditionally, the TEA has been used as a surrogate for the instant center of knee flexion and extension, which has been incorporated into surgical techniques and modern implant designs (20, 33, 34). However, much of the rationale of using the TEA as a surrogate for the flexion-extension axis was based off of 2-dimensional studies assessing only the coronal and transverse planes, which determined that the difference between the TEA and the FEA was minimal (35, 36). However, Eckhoff et al., in an analysis of 23 cadaveric knees using computed tomography and reconstructions in 3-D virtual space, demonstrated the true FEA to be approximately 4.6° internally rotated relative to the TEA (25), which has been further supported by several kinematic studies (36-38). Thus, use of the kinematically aligned surgical technique closely approximates the true FEA of the knee, thus potentially improving knee kinematics following TKA.
Furthermore, Eckhoff et al. found a wide range of variability in the relationship between the FEA and the TEA, with values in their difference ranging from 1.8° to 11.3° (25). This range of values was similar to that seen in our study (12.8°). Given the wide range of variability between the traditional axes used to set femoral component rotation, and with respect to the posterior femoral axis of the kinematically aligned knee, it appears that a technique that sets resection depths of the posterior condyles based on cartilage wear (rather than rotation based off a traditional axis) most reliably approximates a patient's native FEA.
However, while this study suggests the kinematically aligned TKA to more closely approximate the native flexion-extension axis of the knee, questions still remain. Given that the majority of implant designs have used the transepicondylar line as the reference axis, the effect of relative internal rotation of the femoral component and its relationship to anterior knee pain and patella maltracking must still be assessed. Furthermore, how to precisely determine the amount of cartilage and bone wear of both the medial and lateral femoral condyles, and thus the amount of resection necessary to restore a patient's native axis, must continue to be studied. Lastly, whether this technique will consistently improve knee kinematics and functional results, without compromising long-term implant survivorship, remains to be seen. This study is the first to assess the relationship of the posterior femoral axis of the kinematically aligned TKA relative to the traditional axes used to set femoral component rotation. Using a kinematically aligned surgical technique internally rotates the posterior femoral axis relative to the transepicondylar axis, which significantly differs from current alignment instrument targets. The longterm effect on clinical outcomes, survivorship, and implant design must still be determined.
Highlights.
We determine the relationship of the posterior femoral axis of the kinematically aligned total knee arthroplasty to traditional axes used to set femoral component rotation
Use of the kinematically aligned surgical technique internally rotates the femoral component relative to traditional axes used in the mechanically aligned total knee arthroplasty
Use of the kinematically aligned surgical technique may better approximate the true flexion-extension axis of the knee
Footnotes
This study has been approved by the Institutional Review Board at Washington University School of Medicine (St. Louis, MO).
Conflict of Interest Statement: The authors have no financial conflicts of interested related to this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lutzner J, Hubel U, Kirschner S, Gunther KP, Krummenauer F. Long-term results in total knee arthroplasty. A meta-analysis of revision rates and functional outcome. Chirurg. 2011 Jul;82(7):618–24. doi: 10.1007/s00104-010-2001-8. [DOI] [PubMed] [Google Scholar]
- 2.Meding JB, Meding LK, Ritter MA, Keating EM. Pain relief and functional improvement remain 20 years after knee arthroplasty. Clin Orthop Relat Res. 2012 Jan;470(1):144–9. doi: 10.1007/s11999-011-2123-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wegener JT, van Ooij B, van Dijk CN, Karayeva SA, Hollmann MW, Preckel B, et al. Longterm pain and functional disability after total knee arthroplasty with and without single-injection or continuous sciatic nerve block in addition to continuous femoral nerve block: A prospective, 1-year follow-up of a randomized controlled trial. Reg Anesth Pain Med. 2013 Jan-Feb;38(1):58–63. doi: 10.1097/AAP.0b013e318272523c. [DOI] [PubMed] [Google Scholar]
- 4.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the united states from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 5.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: National projections from 2010 to 2030. Clin Orthop Relat Res. 2009 Oct;467(10):2606–12. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Price AJ, Longino D, Rees J, Rout R, Pandit H, Javaid K, et al. Are pain and function better measures of outcome than revision rates after TKR in the younger patient? Knee. 2010 Jun;17(3):196–9. doi: 10.1016/j.knee.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Wainwright C, Theis JC, Garneti N, Melloh M. Age at hip or knee joint replacement surgery predicts likelihood of revision surgery. J Bone Joint Surg Br. 2011 Oct;93(10):1411–5. doi: 10.1302/0301-620X.93B10.27100. [DOI] [PubMed] [Google Scholar]
- 8.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res. 2010 Jan;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noble PC, Conditt MA, Cook KF, Mathis KB. The john insall award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006 Nov;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 10.Parvizi J, Nunley RM, Berend KR, Lombardi AV, Ruh EL, Clohisy JC, et al. High level of residual symptoms in young patients with total knee arthroplasty. Open Meeting of the Knee Society. 2013 doi: 10.1007/s11999-013-3229-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010 Sep 15;92(12):2143–9. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 12.Bellemans J, Colyn W, Vandenneucker H, Victor J. The chitranjan ranawat award: Is neutral mechanical alignment normal for all patients? the concept of constitutional varus. Clin Orthop Relat Res. 2012 Jan;470(1):45–53. doi: 10.1007/s11999-011-1936-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bellemans J. Neutral mechanical alignment: A requirement for successful TKA: Opposes. Orthopedics. 2011 Sep 9;34(9):e507–9. doi: 10.3928/01477447-20110714-41. [DOI] [PubMed] [Google Scholar]
- 14.Howell SM, Hodapp EE, Vernace JV, Hull ML, Meade TD. Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? an intersurgeon analysis of consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2012 Oct 2; doi: 10.1007/s00167-012-2220-2. [DOI] [PubMed] [Google Scholar]
- 15.Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc. 2013 Apr 4; doi: 10.1007/s00167-013-2481-4. [DOI] [PubMed] [Google Scholar]
- 16.Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008 Sep;31(9):857–63. doi: 10.3928/01477447-20080901-15. [DOI] [PubMed] [Google Scholar]
- 17.Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics. 2012 Feb 17;35(2):e160–9. doi: 10.3928/01477447-20120123-04. [DOI] [PubMed] [Google Scholar]
- 18.Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013 Mar;471(3):1000–7. doi: 10.1007/s11999-012-2613-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whiteside LA, Arima J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res. 1995 Dec;(321):168–72. [PubMed] [Google Scholar]
- 20.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993 Jan;(286):40–7. [PubMed] [Google Scholar]
- 21.Katz MA, Beck TD, Silber JS, Seldes RM, Lotke PA. Determining femoral rotational alignment in total knee arthroplasty: Reliability of techniques. J Arthroplasty. 2001 Apr;16(3):301–5. doi: 10.1054/arth.2001.21456. [DOI] [PubMed] [Google Scholar]
- 22.Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am. 2005 Oct;87(10):2276–80. doi: 10.2106/JBJS.D.02945. [DOI] [PubMed] [Google Scholar]
- 23.Jerosch J, Peuker E, Philipps B, Filler T. Interindividual reproducibility in perioperative rotational alignment of femoral components in knee prosthetic surgery using the transepicondylar axis. Knee Surg Sports Traumatol Arthrosc. 2002 May;10(3):194–7. doi: 10.1007/s00167-001-0271-x. [DOI] [PubMed] [Google Scholar]
- 24.Yan CH, Yau WP, Ng TP, Lie WH, Chiu KY, Tang WM. Inter- and intra-observer errors in identifying the transepicondylar axis and whiteside's line. J Orthop Surg (Hong Kong) 2008 Dec;16(3):316–20. doi: 10.1177/230949900801600310. [DOI] [PubMed] [Google Scholar]
- 25.Eckhoff D, Hogan C, DiMatteo L, Robinson M, Bach J. Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res. 2007 Aug;461:238–44. doi: 10.1097/BLO.0b013e318112416b. [DOI] [PubMed] [Google Scholar]
- 26.Fehring TK. Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res. 2000 Nov;(380):72–9. doi: 10.1097/00003086-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Eckhoff DG, Dwyer TF, Bach JM, Spitzer VM, Reinig KD. Three-dimensional morphology of the distal part of the femur viewed in virtual reality. J Bone Joint Surg Am. 2001;(83-A Suppl 2)(Pt 1):43–50. doi: 10.2106/00004623-200100021-00010. [DOI] [PubMed] [Google Scholar]
- 28.Victor J, Van Doninck D, Labey L, Innocenti B, Parizel PM, Bellemans J. How precise can bony landmarks be determined on a CT scan of the knee? Knee. 2009 Oct;16(5):358–65. doi: 10.1016/j.knee.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 29.Howell SM, Papadopoulos S, Kuznik KT, Hull ML. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc. 2013 Aug 15; doi: 10.1007/s00167-013-2621-x. [DOI] [PubMed] [Google Scholar]
- 30.Munro BH. Correlation In: Statistical Methods for Healthcare Research. 3rd. Lippincott-Raven; 1997. pp. 224–245. [Google Scholar]
- 31.Dennis DA, Komistek RD, Kim RH, Sharma A. Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res. 2010 Jan;468(1):102–7. doi: 10.1007/s11999-009-1112-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hungerford DS, Kenna RV, Krackow KA. The porous-coated anatomic total knee. Orthop Clin North Am. 1982 Jan;13(1):103–22. [PubMed] [Google Scholar]
- 33.Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur. J Bone Joint Surg Am. 1987 Jul;69(6):873–80. [PubMed] [Google Scholar]
- 34.Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res. 2001 Nov;(392):38–45. doi: 10.1097/00003086-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 35.Asano T, Akagi M, Nakamura T. The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: In vivo analysis using a biplanar image-matching technique. J Arthroplasty. 2005 Dec;20(8):1060–7. doi: 10.1016/j.arth.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 36.Churchill DL, Incavo SJ, Johnson CC, Beynnon BD. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res. 1998 Nov;(356):111–8. doi: 10.1097/00003086-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 37.Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res. 1993 May;(290):259–68. [PubMed] [Google Scholar]
- 38.Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, et al. Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am. 2005;87(Suppl 2):71–80. doi: 10.2106/JBJS.E.00440. [DOI] [PubMed] [Google Scholar]


