Abstract
Research concerning the assessment of turns during walking in healthy older adults is scarce. This study compared three independent assessments of entry and exit points of turns during walking; participant, clinical rater, and a computer algorithm. Nineteen non-demented and nondisabled older adults (mean age 75.40 ± 5.52 years) participated in the current study. Results revealed that overall the three assessment methods were consistent (68 – 100 % agreement). However, participants determined their turn exit point before the algorithm, (−304.53 ± 326.67 ms), t(18) = −4.06, p = .001, 95% CI [−461.98, −147.08], and clinical rater, (−225.79 ± 303.79 ms), t(18) = −3.24, p = .005, 95% CI [−372.21, −79.37]. The differences in turn determination between the algorithm and rater were significant at turn entry points (131.24, ± 127.25 ms), t(18) = 4.50, p < .001, 95% CI [69.91, 192.58]) but not at turn exit points (−78.74 ± 259.66 ms), t(18) = −1.32, p < .20, 95% CI [−203.89, −46.41]). Greater time discrepancies in assessing turn exit points between the participants and both the algorithm and clinical rater were associated with worse visuospatial performance. Despite the relatively small difference among the three assessments of turns, they were consistent and can be utilized interchangeably. Further studies are necessary to determine whether differences in the ability to accurately determine turns entry and exit points are related to fall risk in normal and disease populations.
Keywords: older adults, walking turns, visual perception
Approximately a third of the steps taken throughout the day involves turns while walking [1]. The limited research on turns has focused on idiopathic Parkinson’s disease (IPD) [2]. Individuals with mild IPD display difficulty with turning, but maintain normal walking in a straight line [2]. However, little is known about turns in aging and no studies examined the individuals’ perspective of turns. Understanding the individuals’ awareness of turns could provide important insight into the phenomenology, risk assessment and interventions of falls.,
To address these knowledge gaps, we compared three assessments of turns while walking in older adults: participant, clinical rater and computer-based algorithm. We further examined whether differences between the three assessments were associated with visuospatial performance, which is known to affect turning abilities [3].
Methods
Participants
Nineteen participants were recruited from a cohort study titled “Central Control of Mobility in Aging” [4].. Written informed consent was obtained from the participants in person according to study protocols approved by the institutional review board.
Measures and Procedures
Walking protocol
Participants walked on a 4 × 14 foot instrumented walkway (Zenometrics, LLC; Peekskill, NY) for two blocks. Each block consisted of three loops; each loop contained two 180° left turns and two straight walks, yielding a total of six turns and six straight segments. The walkway was embedded with pressure sensors and Protokinetics Movement Analysis Software (PKMAS) was utilized to quantitatively assess gait. The outline of the walking area was demarcated by black tape. No indicators were placed on the recording surface to indicate the turn points. Participants began and ended each block in the right proximal corner of the walkway, relative to the clinical rater. Walking started with the instruction “begin,” and ended with the instruction “stop.”
Turns assessments
Turns were operationally defined as ‘a change in direction while walking.’ The turn includes an entry point, curved path, and an exit point.
1. Algorithm
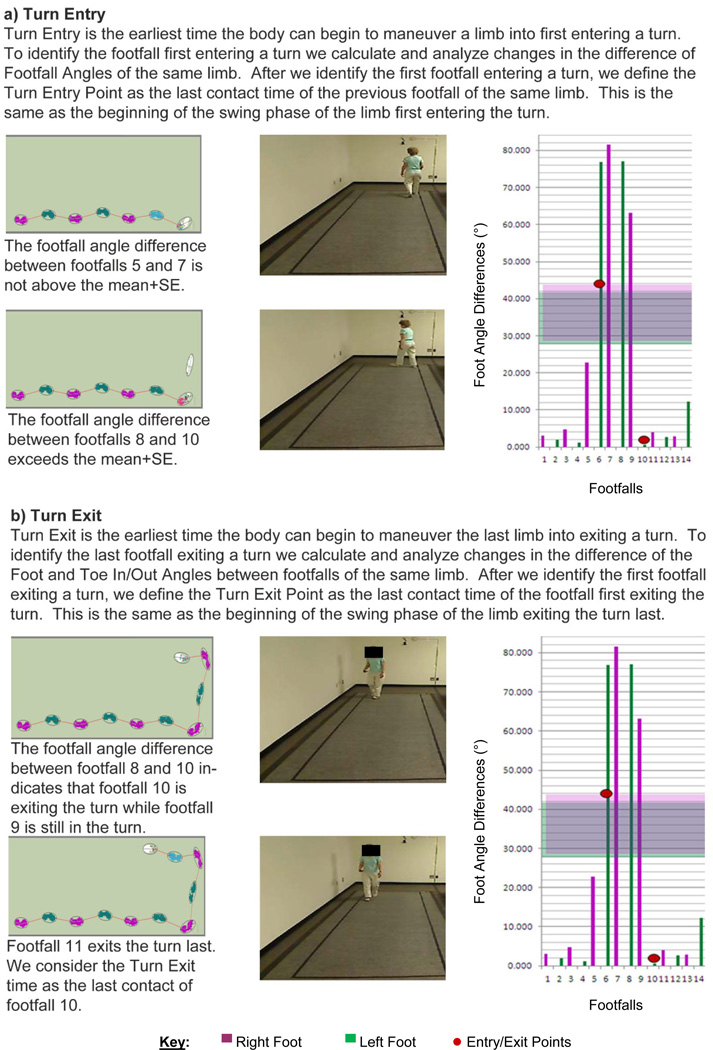
The computerized algorithm determines the first footfall entering or exiting a turn by analyzing the changes of footfall angles of the same limb. It then defines the turn entry or exit point as the beginning of the swing phase of the opposite limb (last contact of opposite limb; Figure 1).
Figure 1.
2. Participant rating
The participants held a switch in their right hand while walking, and were instructed to press the button on the device upon turn-entry, hold it down during the turn, and release it at the turn-exit. Pressing and releasing the switch sent a time-stamped TTL pulse to the PKMAS software in real time. In Block 1, participants walked at their normal pace while indicating entry- and exit-points of each turn using the switch. In Block 2, participants walked while holding the switch without assessing entry- and exit-points to determine the effect of the switch on walking. The order of the two blocks was counterbalanced.
3. Clinical rater
The clinical rater received the same instructions as the participants for rating turns using an identical switch. The clinical rater was stationed at the far end of the walkway affording an unobstructed view for each turn.
Covariates
The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) measures attention, language, visuospatial skills and, memory. It also provides a global cognitive function score [5]. The 30-item Geriatric Depression Scale (GDS) was used to assess depressive symptoms [6].
Statistical Analysis
The first five turns were used for statistical analyses. The sixth turn was not fully completed and thus omitted. The outcomes of interest included the timing of entry and exit and duration of turns (milliseconds). Differences in the three assessments were calculated by subtracting time points for the entry and exit of turns. Differences were averaged across the five turns per participant. Hence, each participant had one difference score for their entry, exit, and duration of turns relative to the algorithm and clinical rater.
One-sample t-tests examined differences between participant determined turns’ entry/exit points, and those of the algorithm, and clinical rater. One and two SDs of the mean differences among assessment pairs were used to determine agreement.
Pearson r correlations examined whether greater time discrepancies in assessing turn exit points among ratings were associated with worse visuospatial performance.
Results
The sample consisted of 19 non-demented participants (mean age=75.37y; mean education=14.25y; 47% female), with no clinical evidence of stroke, Parkinsonian signs or clinical gait abnormalities as determined by the study clinician. Two participants reported a previous fall.
Block 1 vs. Block 2 comparison revealed that pressing the switch did not affect walking performance (Table 2).
Table 2.
Results
| Paired t-test Block A and Block B | |||||
| 95% CI | |||||
| Difference M (SD) ms | t(18) | p | LL | UL | |
| Straights | −1048.24 (8622.09) | 0.80 | .60 | −5203.95 | 3107.48 |
| Turns | −983.58 (8788.28) | −0.49 | .63 | −5219.39 | 3252.24 |
| One-Sample t-test Participant and Algorithm | |||||
| 95% CI | |||||
| Turn | Difference M (SD) ms | t(18) | p | LL | UL |
| Entry | 62.11 (340.41) | 0.80 | .44 | −101.96 | 226.18 |
| Exit | −304.53 (326.67) | −4.06 | .001 | −461.98 | −147.08 |
| Duration | −331.73 (520.07) | −2.78 | .01 | −582.40 | −81.07 |
| One-Sample t-test Participant and Rater | |||||
| 95% CI | |||||
| Turn | Difference M (SD) ms | t(18) | p | LL | UL |
| Entry | −104.04 (343.14) | −1.32 | .20 | −269.43 | 61.35 |
| Exit | −225.79 (303.79) | −3.24 | .005 | −372.21 | −79.37 |
| Duration | −121.75 (474.83) | −1.12 | .28 | −350.61 | 107.11 |
| One-Sample t-test Rater and Algorithm | |||||
| 95% CI | |||||
| Turn | Difference M (SD) ms | t(18) | p | LL | UL |
| Entry | 131.24 (127.25) | 4.50 | <.001 | 69.91 | 192.58 |
| Exit | −78.74 (259.66) | −1.32 | .20 | −203.89 | −46.41 |
| Duration | −209.98 (251.16) | −3.64 | .002 | −331.04 | −88.93 |
Note. CI = confidence interval; LL = lower limit; UL = upper limit.
Agreement between the participants and algorithm for turn entry ranged from 68.42% to 100% for 1 and 2 SDs of the difference (M=62.11±340.41 ms) respectively. Agreement for turn exit ranged from 84.21% to 94.74% for 1 and 2 SDs of the difference (M=−304.43±326.67 ms), respectively. Agreement between the clinical rater and the algorithm for turn entry ranged from 73.68% to 94.74% for 1 and 2 SDs of the difference (M=131.24±127.25 ms) respectively. Agreement for turn exit ranged from 68.42% to 94.74% for 1 and 2 SDs of the difference (M=− 78.74±259.66 ms), respectively. Bland-Altman plots demonstrated good agreement between the three rating methods (not shown). Comparisons of the three turn assessments are summarized in Table 2.
The differences between participants and algorithmically determined turn-exit-points were negatively correlated with RBANS line orientation scores (r=−.47, p=.04). Differences between the participants and clinical rater in determining turn-exit-points showed a negative trend with line orientation scores (r=−.45, p=.06). To explore the influence of age on the relationship between visuospatial abilities and turns the sample was stratified by median split. Differences between older participants and algorithmically determined turn-exit-points showed a negative trend with line orientation scores (r=−.59, p=.13). Differences between the participants and clinical rater in determining turn-exit-point were negatively correlated with line orientation (r=−.71, p=.05). Differences between younger participants and the algorithm or clinical rater for turn entry or exit were not associated with visuospatial abilities.
Discussion
The present study evaluated algorithmic, individual and rater determinations of turns during walking. These assessments of turns were in reasonable agreement and therefore can be utilized interchangeably. Participants, however, determined turn exit points earlier than both the algorithm and clinical rater though the differences were small. The tendency for participants to determine turn-exit-points earlier than the other two assessments may represent anticipation and planning for the completion of a turn.
Worse visuospatial abilities were associated with greater differences between the participants’ determination of turn-exit-points and algorithm. A similar trend was observed for the association between visuospatial abilities and differences between the participants’ and rater’s determination of turn-exit-points. Exploratory stratified analyses revealed that the associations of visuospatial abilities with differences in turn determination between the participants and the other two methods were more evident among the older participants. These findings provide preliminary evidence for age-related higher order cognitive control of turns, and should be further evaluated.
Future research should examine extrinsic/intrinsic factors including but not limited to cognitive functions and individual awareness of turns that influence turning in more diverse and larger samples in the laboratory and in naturalistic settings. Knowledge about modifiable factors that impact turns will provide insights into fall mechanisms and potential risk assessment and interventions.
Table 1.
Locations and Foot Angle Differences by Footfalls
| Footfalls | First Contact (s) |
Last Contact (s) |
Foot Toe X Location (cm) |
Foot Toe Y Location (cm) |
Foot Heel X Location (cm) |
Foot Heel Y Location (cm) |
Foot Angle (°) |
RIGHT Foot Angle Difference |
LEFT Foot Angle Difference |
|
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Right 1 | 1.91 | 2.58 | 351.47 | 107.18 | 377.03 | 105.75 | −3.20 | ||
| 2 | Left 1 | 2.40 | 3.06 | 294.69 | 100.46 | 321.39 | 99.38 | −2.32 | ||
| 3 | Right 2 | 2.95 | 3.53 | 240.65 | 104.89 | 266.82 | 104.79 | −0.22 | 2.99 | |
| 4 | Left 2 | 3.43 | 4.03 | 183.82 | 98.10 | 210.07 | 96.12 | −4.30 | 1.98 | |
| 5 | Right 3 | 3.88 | 4.51 | 131.93 | 105.56 | 157.38 | 103.34 | −4.99 | 4.77 | |
| 6 | Left 3 | 4.38 | 5.04 | 74.72 | 101.64 | 101.74 | 99.10 | −5.38 | 1.08 | |
| 7 | Right 4 | 4.92 | 5.77 | 17.58 | 106.68 | 45.41 | 115.60 | 17.77 | 22.76 | |
| 8 | Left 4 | 5.58 | 6.38 | 17.68 | 54.96 | 26.27 | 80.59 | 71.48 | 76.86 | |
| 9 | Right 5 | 6.18 | 7.03 | 5.48 | 36.78 | 17.41 | 12.64 | −63.70 | 81.47 | |
| 10 | Left 5 | 6.87 | 7.54 | 43.97 | 24.72 | 71.59 | 22.01 | −5.60 | 77.08 | |
| 11 | Right 6 | 7.43 | 7.98 | 93.88 | 13.50 | 120.20 | 13.24 | −0.58 | 63.12 | |
| 12 | Left 6 | 7.85 | 8.38 | 148.76 | 25.53 | 175.23 | 23.18 | −5.08 | 0.52 | |
| 13 | Right 7 | 8.28 | 8.80 | 205.79 | 15.00 | 231.71 | 12.95 | −4.53 | 3.95 | |
| 14 | Left 7 | 8.68 | 9.23 | 260.79 | 20.29 | 289.05 | 16.44 | −7.77 | 2.69 | |
| 15 | Right 8 | 9.12 | 9.70 | 311.58 | 7.08 | 338.67 | 6.28 | −1.69 | 2.84 | |
| 16 | Left 8 | 9.56 | 10.10 | 353.52 | 11.13 | 379.10 | 13.23 | 4.52 | 12.29 | |
| 17 | Right 9 | 9.98 | 10.64 | 394.75 | 0.08 | 414.54 | 18.40 | 42.79 | 44.48 | |
| 18 | Left 9 | 10.47 | 11.18 | 406.78 | 42.08 | 412.72 | 69.06 | 77.58 | 73.06 | |
| 19 | Right 10 | 11.03 | 11.96 | 400.11 | 108.77 | 420.21 | 92.46 | −39.06 | 81.85 | |
| 20 | Left 10 | 11.76 | 12.41 | 344.61 | 101.95 | 369.78 | 98.53 | −7.73 | 85.31 | |
| 21 | Right 11 | 12.30 | 12.85 | 290.21 | 108.22 | 315.56 | 108.16 | −0.12 | 38.94 | |
| 22 | Left 11 | 12.75 | 13.27 | 228.18 | 104.73 | 254.51 | 100.90 | −8.29 | 0.57 | |
| 23 | Right 12 | 13.18 | 13.70 | 171.42 | 109.74 | 197.44 | 110.60 | 1.89 | 2.01 | |
| 24 | Left 12 | 13.60 | 14.16 | 108.72 | 103.94 | 137.25 | 101.25 | −5.38 | 2.92 | |
| 25 | Right 13 | 14.05 | 14.63 | 51.20 | 112.29 | 82.38 | 113.57 | 2.34 | 0.45 | |
| 26 | Left 13 | 14.5 | 15.125 | 21.508 | 91.244 | 44.548 | 105.75 | 32.19 | 37.57 | |
| 27 | Right 14 | 14.98 | 15.53 | 11.42 | 53.55 | 13.84 | 79.89 | 84.76 | 82.41 | |
| 28 | Left 14 | 15.41 | 16.10 | 18.23 | 38.77 | 28.62 | 14.64 | −66.69 | 98.88 | |
| --- | ---- | ---- | ----- | ---- | ----- | ----- | ---- | ---- | ------ | ------ |
| M | 35.30 | 36.61 | ||||||||
| SD | 34.45 | 37.82 | ||||||||
| SE | 6.63 | 7.28 | ||||||||
| M+SE | 42.23 | 43.88 | ||||||||
| M−SE | 28.67 | 29.33 | ||||||||
Note. Data from the PKMAS software are exported to Excel for analysis. The foot angle is calculated based on the X and Y location for the Heel and Toe. The Absolute Foot Angle Difference between consecutive footfalls of same limb is then computed. For each limb we compute the M, SD, SE, M+SE and M−SE. When the Absolute Foot Angle Difference exceeds the M+SE then the subject is considered to be inside a turn otherwise is on a straight walk.
Research.Highlights.
Examined three turn rating methods: participant, clinical rater and algorithm
Determined that the three assessment methods were consistent
Participants determined earlier turn exit than the algorithm and clinical rater
Visuo-spatial abilities were related to participants’ determination of turns
Anticipation may partially explain the variability in participants’ turns assessment
Acknowledgements
This research was supported by a grant from the National Institute on Aging (R01AG036921; Holtzer R. PI).
References
- 1.Glaister BC, Bernatz GC, Klute GK, Orendurff MS. Video task analysis of turning during activities of daily living. Gait and Posture. 2007;25(2):289–294. doi: 10.1016/j.gaitpost.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Crenna P, Carpinella I, Rabuffetti M, et al. The association between impaired turning and normal straight walking in Parkinson's disease. Gait and Posture. 2007;26(2):172–178. doi: 10.1016/j.gaitpost.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Akram SB, Frank JS, Fraser J. Coordination of segments reorientation during on-the-spot turns in healthy older adults in eyes-open and eyes-closed conditions. Gait and Posture. 2010;32(4):632–636. doi: 10.1016/j.gaitpost.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Holtzer R, Wang C, Verghese J. Performance variance on walking while talking tasks: theory, findings, and clinical implications. Age (Dordrecht, Netherlands) 2013 doi: 10.1007/s11357-013-9570-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duff K, Patton D, Schoenberg MR, Mold J, Scott JG, Adams RL. Age- and education-corrected independent normative data for the RBANS in a community dwelling elderly sample. Clin Neuropsychol. 2003;17(3):351–366. doi: 10.1076/clin.17.3.351.18082. [DOI] [PubMed] [Google Scholar]
- 6.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]