Abstract
Objectives
This analysis aimed to estimate the average annual cost of available reversible contraceptive methods in the United States. In line with literature suggesting long-acting reversible contraceptive (LARC) methods become increasingly cost-saving with extended duration of use, it aimed to also quantify minimum duration of use required for LARC methods to achieve cost-neutrality relative to other reversible contraceptive methods while taking into consideration discontinuation.
Study design
A three-state economic model was developed to estimate relative costs of no method (chance), four short-acting reversible (SARC) methods (oral contraceptive, ring, patch and injection) and three LARC methods [implant, copper intrauterine device (IUD) and levonorgestrel intrauterine system (LNG-IUS) 20 mcg/24 h (total content 52 mg)]. The analysis was conducted over a 5-year time horizon in 1000 women aged 20–29 years. Method-specific failure and discontinuation rates were based on published literature. Costs associated with drug acquisition, administration and failure (defined as an unintended pregnancy) were considered. Key model outputs were annual average cost per method and minimum duration of LARC method usage to achieve cost-savings compared to SARC methods.
Results
The two least expensive methods were copper IUD ($304 per women, per year) and LNG-IUS 20 mcg/24 h ($308). Cost of SARC methods ranged between $432 (injection) and $730 (patch), per women, per year. A minimum of 2.1 years of LARC usage would result in cost-savings compared to SARC usage.
Conclusions
This analysis finds that even if LARC methods are not used for their full durations of efficacy, they become cost-saving relative to SARC methods within 3 years of use.
Implications
Previous economic arguments in support of using LARC methods have been criticized for not considering that LARC methods are not always used for their full duration of efficacy. This study calculated that cost-savings from LARC methods relative to SARC methods, with discontinuation rates considered, can be realized within 3 years.
Keywords: LARC, SARC, Unintended pregnancy, Cost study, Cost savings
1. Introduction
Unintended pregnancy (UP) is a substantial public health problem in the United States leading to a sizeable, and potentially avoidable, cost burden [1]. Despite national public expenditure and investment on family planning services exceeding $2 billion and states reportedly spending as much as $68 million of their own funds, collectively, on abortion services in 2010 [2], the annual direct cost of UP remains high at an estimated $4.5 billion annually [1]. Furthermore, the total cost burden of UP to US taxpayers is reported to range from $9.6 to $12.6 billion per year [3]. Of those women who experience UP, historic survey data suggest that 50% were using contraception in the month of conception [4], and additional evidence suggests that the majority of UPs in women using contraception are due to incorrect or inconsistent use rather than method failure [1,5].
Long-acting reversible contraceptive (LARC) methods are effective contraceptive methods [6], but they are often considered to be costly relative to short-acting reversible contraceptive (SARC) methods and have limited uptake in the United States [7]. Of women using reversible contraception in the United States, 55% use SARC methods, 27% use barrier methods (mainly condoms), 10% use natural methods such as withdrawal or periodic abstinence, while only 9% use LARC methods [7]. These various methods vary greatly in their effectiveness, duration of effect, level of required user adherence and overall cost [6]. Condoms are relatively inexpensive but rely heavily on correct and consistent use; SARC methods [oral contraception (OC), patch, ring and injections] require administration that ranges from daily to once every 3 months but are similarly dependent on regular user adherence [6]. In contrast, LARC methods [the copper intrauterine device (IUD), hormonal intrauterine systems (IUSs) and implant] require administration much less frequently (once every 3 to 10 years), and their effectiveness is not reliant upon user adherence [6].
While LARC use is associated with substantial upfront costs, there are no further year-on-year costs unless the method is prematurely discontinued, and they are associated with low method failure rates [6]. Previous publications indicate that LARC methods are cost-effective options relative to SARC methods [1,8] and suggest that LARC methods become increasingly cost-saving with extended duration of use. This analysis aims to quantify the time point at which LARC methods achieve cost-neutrality relative to use of SARC methods, barrier methods (limited to condoms) and no method (chance). In doing so, the overall objective is to demonstrate that although LARC methods are not always used for their full duration of efficacy, cost-savings are realized even when LARC methods are used for a relatively short period of time.
2. Methods
2.1. Overview
A state transition model was developed to assess the total cost and effect of available contraceptive methods in the United States; the methods and results of this model are described in detail elsewhere [9]. The current analysis uses this model to estimate the annual costs associated with available LARC methods [levonorgestrel (LNG)-IUS) 20 mcg/24 h (total content 52 mg), implant and the copper IUD], SARC methods (generic OC, patch, ring and injections), condom and no method as the core contraceptive methods currently used by young women in the United States. The analysis is from the perspective of a public payer, so only direct medical costs are considered. The total costs of LARC methods are compared against the six individual alternative methods plus a ‘mixed-SARC basket’ (comprising a weighted average of available SARC methods which include generic OC, patch, ring and injections) in order to estimate the time point at which cost-neutrality is achieved with use of LARC methods. The weights assigned to each SARC method for the mixed-SARC basket are based on market share data from the most recent National Survey on Family Growth [7].
The analysis assumes a cohort of 1000 women aged 20–29 years. This cohort represents the age group with the highest uptake of SARC methods [7] and can be considered an ‘intervention’ cohort where a switch to LARC methods would likely have a positive impact on rates of UP. A fiveyear time horizon is assumed to reflect family planning preferences in the young women considered in the model as the cohort might be expected to remain in a ‘requiring contraception’ state throughout this period of time. Outcomes of the model are measured in terms of method failure and cost, where method failure was estimated as the cumulative number of UPs over the model time horizon and costs included were those associated with drug acquisition, administration and method failure (i.e., cost of UP).
The model was used to simulate and sum the costs accrued by the cohort of women as they progress through the model over a maximum 5-year period for each contraceptive method. The total and annual average cost of each method was calculated; comparison of the annual average LARC costs against each of the other methods allowed for an estimate of the time point at which LARC methods became cost-neutral relative to the other comparator methods included in the analysis.
2.2. Model structure
The model structure builds on a previously published study [9] and consists of three mutually exclusive states: (a) initial contraceptive method, (b) UP resulting from contraceptive failure and (c) subsequent contraceptive method. All women began in the initial contraceptive method state. Fig. 1 illustrates allowable transitions within the model.
Fig. 1.
Model schematic. Note: p, probability.
Published first-year discontinuation rates inform the rate of transition from initial method to subsequent method [6]. Discontinuation in this model refers to women who stop taking their initial method but continue to choose to avoid pregnancy (i.e., for reasons excluding a planned pregnancy or no longer exposed). Due to lack of robust data, subsequent-year discontinuation rates are assumed to be 5% for all methods. First-year typical-use failure rates inform transition from initial method to UP [6]. Following UP, women move to subsequent method and remain in this state unless an additional UP is experienced.
In the initial and subsequent method states, women incur the cost of method acquisition and administration; upon failure or discontinuation, they also incur a cost of contraceptive removal, if applicable. In the UP state, women incur the cost of a UP defined as a weighted average of possible UP outcomes.
Following previous analyses, a ‘mixed-market basket’ of available contraceptives is used as a proxy for the subsequent method; weights are reflective of uptake by the population of interest [7]. This proxy is used because an assumption cannot be made regarding subsequent method choice. The failure rates, discontinuation rates and costs for the subsequent method state are calculated as the weighted average of the failure rates, discontinuation rates and costs of included methods.
2.3. Model inputs
The transition probabilities applied in the model are summarized in Table 1. These data were identified through a systematic literature review which concluded that due to the disparate and heterogeneous nature of the available data, a meta-analysis was not appropriate. Therefore, the study of Trussell et al. (2011) [6] was selected for these inputs as the publication reported values based on a nationally representative cross-section of women of reproductive age, it was published recently (within the last 5 years), and it covered both failure and discontinuation values for all methods considered in the analysis, ensuring internal consistency within the model.
Table 1. Health state transitions, per annual cycle.
| Method failure (p) | Discontinuation 1st year (p) | Discontinuation subsequent year (p)d | ||
|---|---|---|---|---|
|
| ||||
| Base case | Scenario analysis 1c | |||
| Copper IUD | .0080 | .2200 | .1600 | .05 |
| Implant | .0005 | .1600 | .1670 | .05 |
| LNG-IUS 20 mcg/24 h | .0020 | .2000 | .1250 | .05 |
| Generic OC | .0900 | .3300 | .4490 | .05 |
| Ring | .0900 | .3300 | .4580 | .05 |
| Patch | .0900 | .3300 | .5090 | .05 |
| Injection | .0600 | .4400 | .4350 | .05 |
| Mixed-SARCa | .0870 | .3409 | .4495 | .05 |
| Condom | .1800 | .5550 | Same as base case | .05 |
| No method (chance) | .4600b | .0500d | Same as base case | .05 |
Source: Trussell et al. (2011) [6], unless otherwise indicated.
Note: p, probability.
Estimated for base case age group of 20–29 years as a weighted average of data reported in Jones et al. (2012) [7]; see Table 3 for weights.
Source: Vaughan et al. (2008) [12].
Source: CHOICE Project [18].
Source: assumption.
Cost of method acquisition is based on the wholesale acquisition cost (WAC) price. The cost used in the analysis for OC was a weighted-average cost of all generic OCs with a market share greater than 2%; the weight of each OC was determined by the respective market share. In order to estimate the cost associated with condoms and no methods, coital frequency was estimated to be 83 times per year [17]. Cost of administration includes the cost of clinician visits for the initial prescribing, insertion, removal and/or follow-up consultations required for each method. Cost of UP is the weighted-average cost of the possible outcomes of UP — namely, live birth, induced abortion, spontaneous abortion and ectopic pregnancy. In line with previous methodology [10], the cost of live birth is additionally adjusted based on published data [11] to reflect the likelihood of the UP being simply mistimed rather than truly unwanted. Cost inputs are summarized in Table 2.
Table 2. Unit costs.
| Unit | Cost | Comment |
|---|---|---|
| Method cost (annual for non-LARC methods, per unit for LARC methods) [13] | ||
| Copper IUD | $598.00 | Incurred only in year of insertion. |
| Implant | $659.42 | Incurred only in year of insertion. |
| LNG-IUS 20 mcg/24 h | $703.05 | Incurred only in year of insertion. |
| Generic OCa | $370.34 | Based on 13 packs per year. |
| Ring | $945.49 | Based on 13 packs per year. |
| Patch | $982.41 | Based on 13 packs per year. |
| Injection | $240.02 | Based on 4 injections per year. |
| Mixed-SARCb | $416.42 | Calculated as weighted average |
| Condom | $34.75 | Based on 83 units per year [17]. |
| No method (chance) | $0.00 | N/A |
| Subsequent method | $290.73 | Please refer to the Technical Appendix for details |
| Resource cost (per resource)[14–16] | ||
| Initial clinician consultation (LARC methods) | $104.16 | Higher fee as longer consult; CPT code 99214 |
| Initial clinician consultation (non-LARC methods) | $42.55 | Lower fee as shorter consult; CPT code 99212 |
| Insertion consultation: IUD, IUS | $70.80 | Incurred only in year of insertion; CPT code 58300 |
| Insertion consultation: implant | $135.47 | Incurred only in year of insertion; CPT code 11981 |
| Follow-up consultation (LARC methods) | $104.16 | To check placement in year of insertion; CPT code 99214 |
| Follow-up consultation (non-LARC methods) | $0 | Assuming prescription renewals are provided during annual check-up therefore, no additional follow-up costs. |
| Injection administration | $129.50 | Assuming 4 injections per year at $32.38 per administration; CPT code 96372 |
| Removal consultation: IUD, IUS | $97.01 | Incurred only in year of discontinuation or at end of method life span; CPT code 58301 |
| Removal consultation: implant | $145.68 | Incurred only in year of discontinuation or at end of method life span; CPT code 11976 |
| Pregnancy outcome cost (per outcome) [14–16] | ||
| Live birth | $4988.24 | Weighted average of DRG codes 767, 768, 774, 775, 765 and 766 |
| Spontaneous abortion | $889.25 | DRG code 778 |
| Induced abortion | $734.03 | Weighted average of DRG codes 770 and 779 |
| Ectopic pregnancy | $4919.21 | DRG code 777 |
Distributions of contraceptive uptake assumed for derivation of the mixed-SARC basket and mixed-market basket are detailed in Table 3.
Table 3. Uptake distribution in women 20–29 years.
| Mixed-SARC basket (comparator) | Mixed-market basket (proxy for subsequent method) | |
|---|---|---|
| Copper IUD | – | 0.03 |
| Implant | – | 0.01 |
| LNG-IUS 20 mcg/24 h | – | 0.03 |
| Generic OC | 0.79 | 0.38 |
| Ring | 0.08 | 0.04 |
| Patch | 0.02 | 0.01 |
| Injection | 0.11 | 0.05 |
| Condom | – | 0.22 |
| Tubal ligation | – | 0.05 |
| Tubal occlusion | – | 0.05 |
| No method (chance) | – | 0.13 |
| Total | 1.00 | 1.00 |
Note: Data are recalibrated based on uptake data reported in Jones et al. (2012) [8] for age group of 20–29 years.
2.4. Model analysis
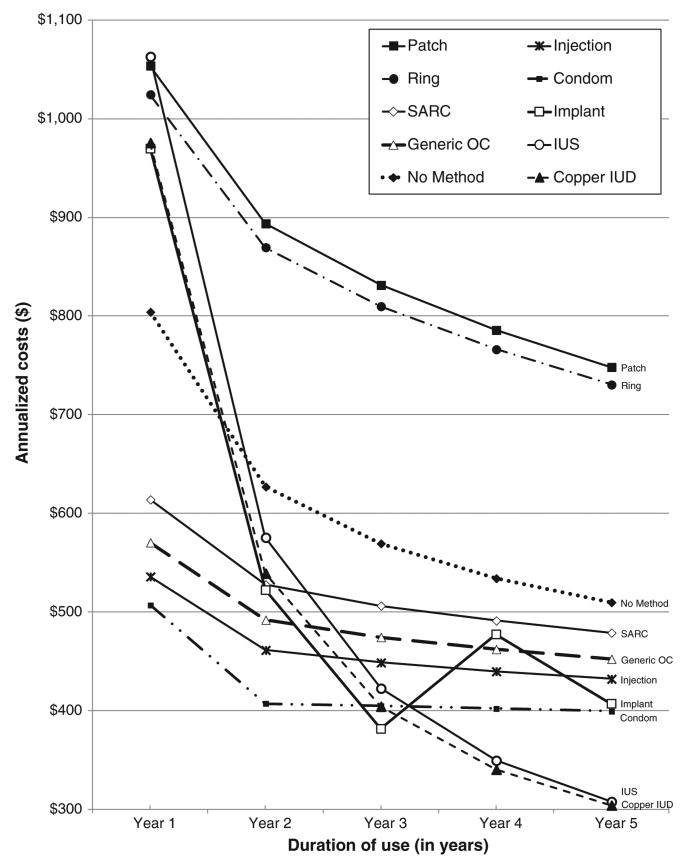
The cost accrued by a cohort of women as they progress through the model over a 5-year time horizon is estimated for each of the 11 contraceptive methods considered. A total cost per year per method per woman is calculated for years 1 to 5. Annualized costs are then estimated for each method as per previously published methodology, where the annualized cost at year x is the total cost for x years divided by x. These annualized costs for years 1 to 5 are plotted over time for each method, illustrating how the 11 methods compare to one another as duration of use increases.
The intersection at which the plotted lines for two methods (e.g., copper IUD and OC) cross marks the point in time when one product (e.g., copper IUD) becomes costneutral relative to the other (e.g., OC). This intersection point is determined for each of the three LARC methods versus each of the four individual SARC methods, the mixed-SARC basket, the condom and no method.
As the primary interest of this analysis was the average duration of LARC usage required, the intersection for each of the seven non-LARC methods versus each of the three LARC methods was calculated such that for each non-LARC method, three respective intersections were estimated. The average of these three intersections was taken to calculate the average duration of a ‘mixed-LARC basket’ usage required relative to each non-LARC method.
Uncertainty within the model is addressed through twoscenario analysis in order to explore the robustness of the model findings:
Scenario 1: Alternative discontinuation rates were available from the CHOICE study which was an observational cohort study developed to promote the use of LARC methods in the St. Louis region [18]. The alternative rates were used in place of the data from Trussell et al. (2011) [6] to assess the impact that discontinuation rates may have on results as this was a key input within the analysis.
Scenario 2: An alternative population consisting of all women of reproductive age (15–44 years) was carried out to see if analysis considering the overall age group has an impact on the average duration of LARC usage required to reach cost-savings.
2.5. Further details
A technical appendix supporting this publication contains further details on methodology. It provides sources and explanations on the costs used in this analysis and the calculations applied to estimate the points of intersection reported in the results section.
3. Results
3.1. Base case analysis
The annualized costs per year, per method, per woman are summarized in Table 4. As expected, the average cost decreases for all methods as duration of use increases. Fig. 2 presents these data graphically and illustrates that despite high upfront costs associated with LARC methods, as duration of use increases, the average cost of LARC methods drops to become less expensive than the methods which have lower upfront costs.
Table 4. Annualized average cost ($) as duration of use increases by year, per woman.
| Duration of use | 1 Year | 2 Years | 3 Years | 4 Years | 5 Years |
|---|---|---|---|---|---|
| Copper IUD | 975.59 | 539.02 | 404.06 | 340.07 | 303.83 |
| Implant | 969.68 | 522.07 | 381.37 | 477.16 | 406.86 |
| LNG-IUS 20 mcg/24 h | 1063.00 | 575.39 | 422.39 | 349.29 | 307.56 |
| Generic OC | 570.33 | 491.92 | 474.33 | 462.15 | 452.18 |
| Ring | 1024.61 | 869.54 | 809.80 | 766.14 | 730.35 |
| Patch | 1053.77 | 893.79 | 831.33 | 785.66 | 748.21 |
| Injection | 535.76 | 461.24 | 448.54 | 439.63 | 431.97 |
| Mixed-SARCa | 613.85 | 527.60 | 506.17 | 491.12 | 478.76 |
| Condom | 506.78 | 407.08 | 404.64 | 401.88 | 399.16 |
| No method (chance) | 804.10 | 626.86 | 569.32 | 533.97 | 509.60 |
Fig. 2.
Annualized costs associated with contraceptive method.
The various points of intersection between the LARC methods and SARC, condom and no method which are shown graphically in Fig. 2 have been calculated numerically and are summarized in Table 5. These intersection points represent the duration of use required to reach costneutrality in the comparison between any two methods. LARC methods become cost-neutral compared with the mixed-SARC basket after approximately 2.1 years of usage.
Table 5. Years usage required to reach cost-neutrality.
| vs. | Implant | Copper IUD | LNG-IUS 20 mcg/24 h | Average LARC |
|---|---|---|---|---|
| Generic OC | 2.1 | 2.4 | 2.6 | 2.4 |
| Ring | <1.0 | <1.0 | 1.1 | 0.4 |
| Patch | <1.0 | <1.0 | 1.0 | 0.3 |
| Injection | 2.5 | 2.6 | 2.8 | 2.6 |
| Mixed-SARCa | 2.0 | 2.1 | 2.4 | 2.1 |
| Condom | 2.8 | 3.0 | 3.3 | 3.0 |
| No method (chance) | 1.6 | 1.7 | 1.8 | 1.7 |
In comparison to condoms, LARC methods would need to be used for approximately 3.0 years before they become cost-saving, while in comparison to no method, 1.7 years of LARC usage would be required. Cost-neutrality is achieved rapidly for LARC methods when compared to the ring and patch at 0.4 and 0.3 year, respectively.
3.2. Scenario analysis
Two scenario analyses were carried out to test the model results for robustness. Firstly, alternative discontinuation rates were applied, and secondly, the overall population of women aged 15 to 44 years was assessed.
Scenario 1: The alternative discontinuation rates suggest that results are minimally sensitive to discontinuation assumptions. Application of the alternative data indicated that LARC methods may need to be used for 4.2 weeks less in order to reach costneutrality versus the mixed-SARC basket in comparison to the duration of use estimated under the base case discontinuation data.
Scenario 2: As would be expected, conducting the analysis for a difference population has an impact on results, but this impact is minimal as well. When assessing the full population of women of reproductive age who would be eligible for contraceptive usage, LARC methods would need to be used for a duration 3.6 weeks less than in the base case age group of women aged 20–29 years in order to become costneutral in comparison to the mixed-SARC basket.
3.3. Discussion
This analysis finds that, on average, within the intervention group considered, LARC methods become cost-neutral in comparison to SARC methods within 3 years of use, after which point the continued use of LARC methods is costsaving. Specifically, this analysis suggests that if LARC methods are used for longer than 2.1 years in this cohort, they become a less costly contraceptive option than SARC methods despite their high upfront costs. A slightly longer duration of use is required for LARC methods to reach costneutrality in comparison to the condom and no method as these options have little to no acquisition or administration costs associated with them. However, even in these comparisons, LARC methods reach cost-neutrality within 3 years. Cost-neutrality is reached quite rapidly when comparing usage of LARC methods to the ring and patch (within 0.4 and 0.3 year, respectively), resulting from the combined impact of substantial difference in failure rates between LARC methods and the ring or patch as well as the high product costs of the ring and patch (see Table 2).
The results were reassessed considering the availability of a fourth LARC method — LNG-IUS 13.5 mg (total content), a new 3-year LNG-IUS. An assumption was made that LNG-IUS 13.5 mg would gain 2% share of the overall contraceptive market upon launch, and the results suggest that including this method would not impact the average duration of LARC usage required to reach costneutrality by very much; the duration required would increase by only half a week (0.6 week). These results are based on perfect-use failure rate of LNG-IUS 13.5 mg as the typical-use failure rate is subject to future research.
Discontinuation of LARC methods is costly since a clinician consultation is necessary in order to carry out the removal procedure. Inclusion of discontinuation costs therefore further exacerbates the already high upfront costs associated with LARC methods. However, despite the inclusion of these costs, findings suggest rapid attainment of cost-neutrality. As such, the inclusion of these costs in the model calculations serves to strengthen the results of this analysis.
The findings were robust to variation in the discontinuation rates applied, the study population assessed and the alternative calculation methodologies applied. LARC methods continued to prove cost-saving compared to SARC methods within a relatively short period of use.
There were a number of limitations to this analysis:
‘Typical-use’ failure rates were available for the first year of contraceptive use only, and these were applied across all years. Subsequent-year failure rates may be lower than in the first year; hence, the cost impact of UP may have been overestimated in the model.
An assumption was made regarding subsequent-year discontinuation rates due to a lack of robust literature on continuation of contraceptive methods beyond the first year of use; subsequent-year discontinuation is likely lower than first year and likely to change as women age and, with that, their contraceptive preference and suitability change; however, it is unlikely to be the same across all methods as assumed in this analysis.
The absence of robust data on switching preferences necessitated a mixed-market basket to act as a proxy for patients choosing to switch methods; however, this construct aimed to approximate the average choices of women switching contraceptive method.
Medicare prices were used to calculate costs associated with the outcomes of UP in the model, and these are expected to be lower than those of private insurers. This is likely to have led to an underestimate of the cost impact of UP in this analysis; thus, the figures presented here are conservative, and duration of use needed for costneutrality may in practice be less than that reported here.
This analysis was conducted from the public payer perspective, but as WAC costs were used to estimate the acquisition cost of the various contraceptives, the results should support a similar conclusion under the private payer perspective because WAC costs are similar to the costs that private payers pay would face. Cost survey and analysis from the private payer perspective are subject to future research.
The trends in the annualized costing patterns demonstrated by this analysis are consistent with those of Trussell et al. (2009), despite the fact that the analysis assumed that women remained on their initial method for the duration of the analysis. Despite the uncertainty introduced to the model through application of assumptions around the composition of the subsequent method (i.e., the mixed-market basket), inclusion of both discontinuation rates and an ability to switch to a subsequent method mirrors the real-world scenario where, in any given year, women discontinue and switch between existing contraceptive methods. This study therefore adds to the literature by considering discontinuation and demonstrating that despite a proportion of women switching off method, LARC methods are cost-saving over time compared to SARC methods, condom and no method and that cost-neutrality compared to the most used methods (approximated by the mixed–SARC basket) is reached within 2 years of use.
These findings suggest that despite high upfront costs and the costly implications of possible discontinuation, use of LARC methods within the proposed intervention group of young women aged 20–29 years is associated with minimal costs in the years which follow initiation. Costs are minimized due to a combination of higher efficacy (lower failure-related costs) and lower discontinuation rates when compared against other commonly used methods. This study supports the argument that LARC methods become increasingly cost-saving as duration of use increases and suggests that cost-neutrality can be attained even over short durations of use.
Supplementary Material
Acknowledgments
This study and manuscript development were conducted by IMS Health and funded by Bayer Healthcare Pharmaceuticals Inc. This work was also supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant for Infrastructure for Population Research at Princeton University, Grant R24HD047879 (J.T.).
Anna Filonenko is a full-time employee of Bayer Pharma AG, and Amy Law is a full-time employee of Bayer Healthcare Pharmaceuticals Inc. Fareen Hassan and Julia Lowin are full-time employees of IMS Health and served as paid consultants to Bayer Healthcare Pharmaceuticals Inc. for the development of this study and manuscript. James Trussell is a full-time professor of economics and public affairs at Princeton University and received a consultancy fee from Bayer Pharma AG for his contribution to this work.
Footnotes
Funding: This study and manuscript development were funded by Bayer Healthcare Pharmaceuticals Inc. and supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant for Infrastructure for Population Research at Princeton University, grant R24HD047879 (J.T.).
Appendix A. Supplementary data: Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.contraception.2014.08.011.
References
- 1.Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2012;87(2):154–61. doi: 10.1016/j.contraception.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sonfield A, Gold RB. New York: Guttmacher Institute; 2012. Public funding for family planning, sterilization and abortion services, FY 1980–2010. [Available from: http://www.guttmacher.org/pubs/Public-Funding-FP-2010.pdf] [Google Scholar]
- 3.Monea E, Thomas A. Unintended pregnancy and taxpayer spending. Perspect Sex Reprod Health. 2011;43(2):88–93. doi: 10.1363/4308811. [DOI] [PubMed] [Google Scholar]
- 4.Finer LB, Darroch JE, Frost JJ. US agencies providing publicly funded contraceptive services in 1999. Perspect Sex Reprod Health. 2002;34(1):15–24. [PubMed] [Google Scholar]
- 5.Moreau C, Cleland K, Trussell J. Contraceptive discontinuation attributed to method dissatisfaction in the United States. Contraception. 2007;76(4):267–72. doi: 10.1016/j.contraception.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones J, Mosher W, Daniels K. National health statistics reports. no 60. Hyattsville, MD: National Center for Health Statistics; 2012. Current contraceptive use in the United States, 2006 -2010, and changes in patterns of use since 1995. [PubMed] [Google Scholar]
- 8.Mavranezouli I. The cost-effectiveness of long-acting reversible contraceptive methods in the UK: analysis based on a decision-analytic model developed for a National Institute for Health and Clinical Excellence (NICE) clinical practice guideline. Hum Reprod. 2008;23(6):1338–45. doi: 10.1093/humrep/den091. [DOI] [PubMed] [Google Scholar]
- 9.Trussell J, Hassan F, Henry N, Pocoski J, Law A, Filonenko A. Cost-effectiveness analysis of levonorgestrel-releasing intrauterine system (LNG-IUS) 13.5 mg in contraception. Contraception. 2014;89(5):451–9. doi: 10.1016/j.contraception.2013.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trussell J. The cost of unintended pregnancy in the United States. Contraception. 2007;75:168–70. doi: 10.1016/j.contraception.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 11.Mosher WD, Jones J, Abma JC. National health statistics reports. no. 55. Hyattsville, MD: National Center for Health Statistics; 2012. Intended and unintended births in the United States: 1982–2010. [PubMed] [Google Scholar]
- 12.Vaughan B, Trussell J, Kost K, Singh S, Jones R. Discontinuation and resumption of contraceptive use: results from the 2002 National Survey of Family Growth. Contraception. 2008;78(4):271–83. doi: 10.1016/j.contraception.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolters Kluwer Health. Medi-Span master drug database. 2012 Available from: http://www.medi-span.com/drug-pricing-analysis-pricerx.aspx.
- 14.Centers for Medicare & Medicaid Services. Medicare physician fee schedule, CPT code book and Medicare outpatient prospective payment system. 2012 Available from https://www.cms.gov/home/medicare.asp.
- 15.HCUPnet. Healthcare cost and utilization project. Rockville, MD: Agency for Healthcare Research and Quality; 2012. [Available from: http://hcupnet.ahrq.gov] [PubMed] [Google Scholar]
- 16.Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy — section 2b physician services. 2007 Available from http://www.medpac.gov/chapters/Mar07_Ch02b.pdf.
- 17.Chiou CF, Trussell J, Reyes E, Knight K, Wallace J, Udani J, et al. Economic analysis of contraceptives for women. Contraception. 2003;68:3–0. doi: 10.1016/s0010-7824(03)00078-7. [DOI] [PubMed] [Google Scholar]
- 18.Peipert JF, Zhao Q, Allsworth JE, Petrosky E, Madden T, Eisenberg D, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117(5):1105–13. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ventura SJ, Curtin SC, Abma JC, Henshaw SK. National vital statistics reports. no 7. Vol. 60. Hyattsville, MD: National Center for Health Statistics; 2012. Estimated pregnancy rates and rates of pregnancy outcomes for the United States 1990-2008. [PubMed] [Google Scholar]
- 20.Hoover KW, Tao G, Kent CK. Trends in the diagnosis and treatment of ectopic pregnancy in the United States. Obstet Gynecol. 2010;115(3):495–502. doi: 10.1097/AOG.0b013e3181d0c328. [DOI] [PubMed] [Google Scholar]
- 21.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38(2):90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.