Abstract
OBJECTIVES
To assess the literature on outcomes of corticosteroid injections for adhesive capsulitis, and in particular, image-guided corticosteroid injections.
TYPE
Systematic search and review
LITERATURE SURVEY
The databases used were PubMed (1966-present), Embase (1947-present), Web of Science (1900–present), and the Cochrane Central Register of Controlled Trials. Upon reviewing full text articles of these studies, a total of 25 studies were identified for inclusion. The final yield included 7 prospective studies, 16 randomized trials, and 2 retrospective studies.
METHODOLOGY
This systematic review was formatted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Study criteria were limited to clinical trials, prospective studies, and retrospective studies that specifically evaluated intra-articular corticosteroid injections, both alone and in combination with other treatment modalities, for shoulder adhesive capsulitis. We included studies that were not randomized control trials because our review was not a meta-analysis. Data items extracted from each study included: study design, study population, mean patient age, duration of study, duration of symptoms, intervention, single or multiple injections, location of injections, control population, follow up duration, and outcome measurements. A percent change in outcome measures was calculated when corresponding data was available. Risk of bias in individual studies was assessed when appropriate.
SYNTHESIS
All studies involved at least one corticosteroid injection intended for placement in the glenohumeral joint but only eight studies used image-guidance for all injections. Seven of these studies reported statistically significant improvements in ROM at 12 weeks of follow-up or earlier. Ninety-two percent of all studies documented a greater improvement in either visual analog pain scores or range of motion after corticosteroid injections in the first 1–6 weeks as compared with the control or comparison group.
CONCLUSIONS
Corticosteroid injections offer rapid pain relief in the short-term (particularly in the first 6 weeks) for adhesive capsulitis. Long-term outcomes seem to be similar to other treatments including placebo. The added benefit of image-guided corticosteroid injections in improving shoulder outcomes needs further assessment.
INTRODUCTION
Adhesive capsulitis is a long lasting, painful shoulder condition commonly known as “frozen shoulder.” Patients also experience severe loss of range of motion (ROM) at the glenohumeral joint. The condition results from progressive fibrosis and eventual contracture of the capsule of the glenohumeral joint, which causes pain and stiffness1–3. The specific pathophysiology of adhesive capsulitis is unknown and altering its natural history and shortening recovery time remains challenging.
Adhesive capsulitis is prevalent in about 2% of the general population1. Most patients are between the ages of 40–60 years and more female patients are affected than male patients1,4,5. Type I diabetics have a 40% chance of developing adhesive capsulitis in their lifetimes1. Up to 29% of type II diabetics may present with this condition6. Hyperthyroidism7, hypothyroidism8, Parkinson’s disease9, cardiac disease4,10, and autoimmune disorders11 are also associated with adhesive capsulitis.
Adhesive capsulitis is a clinical diagnosis made on patient history and physical examination5. The key clinical feature is the restriction of passive shoulder range of motion, particularly in forward flexion, abduction, external rotation, and internal rotation5,12. The natural history of adhesive capsulitis is described in three consecutive stages1,13,14. The first stage, the “freezing” stage, is marked by progressive pain and loss of motion lasting up to nine months. The second stage, the “frozen” stage, lasts from four to twenty months. In this stage, pain improves but stiffness persists and continues to impact patients’ ability to perform activities of daily living. The third and final “thawing” stage is a period of recovery marked by gradual improvement in range of motion that can take up to five to twenty-six months.
Treatment options include non-steroidal anti-inflammatory drugs (NSAIDs) or other analgesics, physical therapy, manipulation under anesthesia (MUA), dilation or distension of the capsule, arthroscopic or open capsular release, and injections of sodium hyaluronate or corticosteroids15–18. Intra-articular corticosteroid injections target the inflammatory process at the site of pathology, the glenohumeral joint2,19. To improve the accuracy of injections, image guidance with fluoroscopy or ultrasound may be used.
In the existing literature, three reviews found short-term benefits in pain and range of motion from corticosteroid injections specifically for the treatment of adhesive capsulitis14,20,21. However, no reviews have focused their analysis on image-guided injections to assess any added benefit of image-guided injections on shoulder outcomes. There is still debate as to the efficacy of image-guided corticosteroid injections in the treatment of adhesive capsulitis. While the complete pathophysiology of adhesive capsulitis is still unclear, the anatomical location of the pathology lies in the glenohumeral joint2. The accuracy of blind corticosteroid injections into the glenohumeral joint is debatable22–24. Utilizing the additional measure of ultrasound or another image modality to guide injections improves accuracy25,26 but their ability to improve clinical outcomes compared to that of palpation guided injections remains unclear.
Therefore, we conducted a systematic literature review to assess outcomes of intra-articular corticosteroid injections on adhesive capsulitis. We also specifically assessed the outcomes of image-guided corticosteroid injections.
METHODS
The systematic literature review was formatted and based upon guidelines suggested by “The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration”, which seeks to provide a method of producing more standardized and complete systematic reviews27. Study criteria were limited to clinical trials, prospective studies, and retrospective studies that specifically evaluated intra-articular corticosteroid injections, both alone and in combination with other treatment modalities, for shoulder adhesive capsulitis. We included studies that were not randomized control trials because our review was not a meta-analysis. We excluded case reports but included prospective, retrospective, and randomized trial studies. Studies investigating injections for subacromial bursitis, shoulder impingement, or for generalized shoulder stiffness or pain were excluded. Studies investigating subacromial injections or injections of sodium hyaluronate and other non-corticosteroids were also excluded. Other limits included papers written in the English language and those involving human subjects.
The databases used in our literature search were PubMed (1966-present), Embase (1947-present), Web of Science (1900–present), and the Cochrane Central Register of Controlled Trials. Two authors (A.S., N.J.) collaboratively conducted the search in September 2012 with the assistance of a trained librarian with expertise in medical literature search. The two authors then screened and discussed study titles and abstracts returned from the searches to determine inclusion eligibility. The bibliography of review articles and articles selected for final inclusion was also manually searched for any relevant articles but did not reveal any additional articles.
Our search terms are included in Appendix A (in the Supplementary Material). Data was extracted by one author (A.S.) using a standardized table of relevant data items. The second author (N.J.) then checked the extracted data items. Data items extracted from each study included: study design, study population, diagnosis, mean patient age, duration of study, duration of symptoms before treatment, intervention, single or multiple injections, location of injections, control population (if any), follow up period, and outcome measurements.
The included studies defined adhesive capsulitis as the progressive limitation in shoulder motion. There was wide variability in the outcome measures for pain and range of motion (ROM) used across studies. Outcome measures included passive and active range of motion measures, visual analog scale (VAS), shoulder disability questionnaire (SDQ), shoulder pain and disability index (SPADI), SF-36 (Short Form 36 Health Survey), and Constant-Murley score. In order to facilitate comparisons across studies, we calculated a percent change in outcome measures when these data were presented in the manuscript. We did not statistically combine data or conduct a meta-analysis because outcome measures among studies were too heterogeneous. In addition to outcome measure, studies varied widely in interventions, study design, and comparison group. Risk of bias was assessed within randomized controlled studies. Concealment of randomization and blinding of study participants was determined for each study. Prospective and retrospective studies were not applicable for risk of bias analysis. We determined if concealment of randomization, blinding of patients, health care providers, data collectors, and outcome assessors had been reported for randomized trials. However, not all of the included studies were randomized trials and thus certain risk of bias assessments did not apply to all studies.
RESULTS
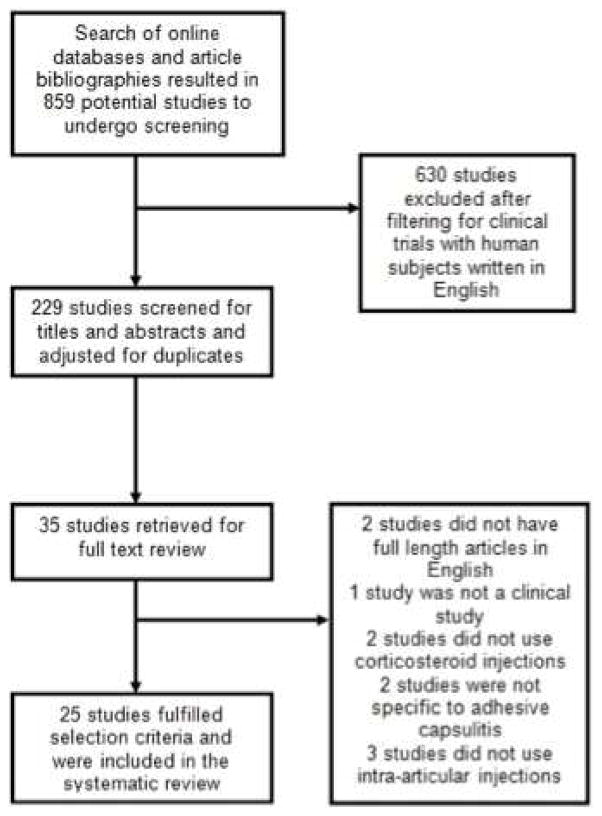
Our search strategy is depicted in Figure 1. The initial search returned 859 studies, of which 630 studies were excluded after filtering for studies with human subjects in the English language. After screening for titles and abstracts simultaneously and then adjusting for duplicates, 35 unique articles were retrieved. Upon reviewing full text articles of these studies, a total of 25 studies were identified for inclusion. The final yield included 7 prospective studies, 16 randomized trials, and 2 retrospective studies. The mean duration of symptoms in selected studies ranged from 3.5 to 11 months, including 7 studies with patients who had greater than 18 months of symptom duration. Not all studies reported the range of symptom duration (n=5). The total duration of follow-up in these studies ranged from 4 weeks to 3 years.
Figure 1.
A flow diagram of study selection.
All interventions involved at least one corticosteroid injection. All 25 studies claimed their injections to be intra-articular but only eight studies used image-guidance for all glenohumeral injections. Two studies used image-guidance for some, but not all injections28,29. Several studies used a combined treatment approach in which one or more steroid injections were provided in conjunction with another treatment (such as corticosteroid injection and supervised physical therapy). The type of corticosteroid used, dose, and injection technique varied across studies. We categorized the included studies by the comparison group (Table I).
Table I. Studies by comparison group.
All studies included at least one injection of a corticosteroid to the glenohumeral joint in the treatment of adhesive capsulitis. Only eight studies used image guidance with either fluoroscopy or ultrasound to perform all glenohumeral injections.
| Number of studies | Number of subjects | |
|---|---|---|
| Steroid Injection Alone or Steroid Injection vs. Placebo Injection | 2 | 124 |
| Steroid Injection vs. Physical Therapy | 6 | 460 |
| Steroid Injection vs. Manipulation Under Anesthesia | 3 | 113 |
| Steroid Injection vs. Dilation/Distension | 2 | 96 |
| Comparison of steroid injection dosages, location of injection, or types of steroid. | 6 | 435 |
| Steroid injections in combination with distension, dilation, or manipulation under anesthesia | 4 | 136 |
| Image-guided steroid injections alone or vs. blind steroid injections* | 2 | 65 |
| Total | 25 | 1429 |
Studies that explicitly and specifically investigated the efficacy of image-guided injections
Risk of bias within each individual randomized trial study was assessed (Table II). Seven randomized trials reported concealment of randomization, four reported blinding patients, three reported blinding health care providers, one reported blinding data collectors, and eight reported blinding outcome assessors.
Table II. Risk of bias within randomized controlled studies.
The 25 studies included in the review were individually evaluated for risk of bias. Study type, concealment of randomization, blinding of patients, health care providers, data collector, and outcome assessors were evaluated when applicable.
| Trials | Concealment of Randomization | Patients Blinded | Health Care Providers Blinded | Data Collectors Blinded | Outcomes Assessors Blinded |
|---|---|---|---|---|---|
| Bal18 (2008) | Yes | Yes | No | NR | Yes |
| Arslan30 (2001) | No | No | No | NR | NR |
| Carette31 (2003) | Yes | Yes | Yes | NR | Yes |
| Ryans32 (2005) | Yes | Yes | Yes | NR | NR |
| Bulgen41 (1984) | No | No | No | NR | Yes |
| De Carli17 (2011) | NR | No | No | NR | Yes |
| Jacobs34(2009) | Yes | No | No | NR | NR |
| Kivimaki33 (2001) | No | No | No | NR | NR |
| Gam35 (1998) | Yes | No | No | NR | Yes |
| Tveita16 (2008) | Yes | No | No | NR | No |
| de Jong36 (1998) | Yes | Yes | Yes | NR | NR |
| Lorbach37 (2010) | No | No | No | NR | NR |
| Oh28 (2011) | No | NR | No | Yes | NR |
| Rizk38 (1991) | NR | NR | NR | NR | Yes |
| White44 (1996) | NR | No | No | No | NR |
| Lee39 (2009) | NR | No | No | NR | Yes |
Appendix B (in the Supplementary material) provides a summary of the studies and data on this topic. By the end of their respective study periods, all intervention groups across all studies, including placebo and no treatment groups, found improvements in range of motion and pain scores.
Intra-articular steroid injection alone or vs. Placebo injection
Two studies examined steroid injection alone or compared to a placebo injection. In one of these studies, there was a mean 58% improvement in abduction, a 100% increase in internal rotation, and a 60% decrease in VAS score (p = .001)30. In the other study, there were no statistically significant differences between the corticosteroid injection group and the placebo injection group in SPADI score and range of motion19.
Intra-articular steroid injection vs. Physical Therapy
The next group of studies compared steroid injection to physical therapy. In one study, the injection group had no statistically significant differences in range of motion and pain improvements to the physical therapy group at the end of the 12 weeks31. Another study compared four groups of treatment: corticosteroid injection and physical therapy, corticosteroid injection alone, physical therapy alone, and placebo injection. At the end of the 12 month study, there were no statistically significant differences between the four groups in SPADI score, SF-36 score, active and passive ROM32. Another study also compared corticosteroid injection and physical therapy in combination or alone. They found no significant differences in Shoulder Disability Questionnaire (SDQ), VAS, and passive external rotation at the end of 16 weeks33.
Intra-articular steroid injection vs. Manipulation
Three studies considered manipulation under anesthesia (MUA) versus injection. One study found no additional advantage to adding corticosteroid injection to a manipulation treatment at 4 months34. Another study found similar regression coefficients of decrease in VAS for a MUA group and a group treated with injection and distension (β = 2.75 vs. 2.77)35. The third study reported satisfactory changes in both the steroid injection group and the manipulation group at 12 months in passive forward flexion, abduction, internal rotation, and external rotation in neutral abduction18.
Intra-articular steroid injection vs. Dilation/Distension
Two studies compared a corticosteroid injection with dilation or distension with steroid. One study found no statistically significant difference between hydrodilation and injection in SPADI score and ROM improvements 17. Gam et al. showed that at 7 and 12 weeks, dilation with steroid and anesthetic had favorable improvements to injection in extension (p = .03) and external rotation (p = .01)36. However, the actual numerical data of these findings were not reported in the study.
Comparison of steroid dosages, location of injection, or types of steroid
Other studies compared steroid dosages, location of injection, or types of steroid. de Jong et al. found a mean VAS improvement of 49.3 for a higher dosage of triamcinolone acetonide (40 mg) compared to a 31.2 VAS improvement for a lower dosage of triamcinolone acetonide (10 mg) (p = .04)37. Lorbach et al. compared a corticosteroid injection and an oral corticosteroid taper. No significant differences between the two treatments were found in VAS pain scores. However, abduction in the injection group was significantly more improved after 12 months (p = .017)38. Three of the studies compared the location of injection in the shoulder. Oh et al. found a glenohumeral injection did not have a significantly greater decrease in VAS compared with a subacromial injection29. Another study found similar improvements in ROM between intra-articular and bursal injections39.
Image guided intra-articular steroid injections
The final group of studies investigated ultrasound or fluoroscopically guided corticosteroid injections. Lee et al. compared ultrasound-guided injections of triamcinolone with blind injections. At 6 weeks, the ultrasound guided injection group did not have statistically superior improvements than blind injections in flexion, abduction, external rotation or internal rotation, although improvements from baseline were significant within both groups (p < .001). The ultrasound guided injection group also did not have significantly better VAS score improvements after 3 weeks40. Lorbach et al. prospectively followed patients who had received 3 fluoroscopically-guided injections followed by physical therapy and, after one year follow-up, found improvements of 181% in abduction (p < .0001), 52% in flexion (p < .0001), 257% in external rotation (p < .0001), and 26% in internal rotation (p < .005)41.
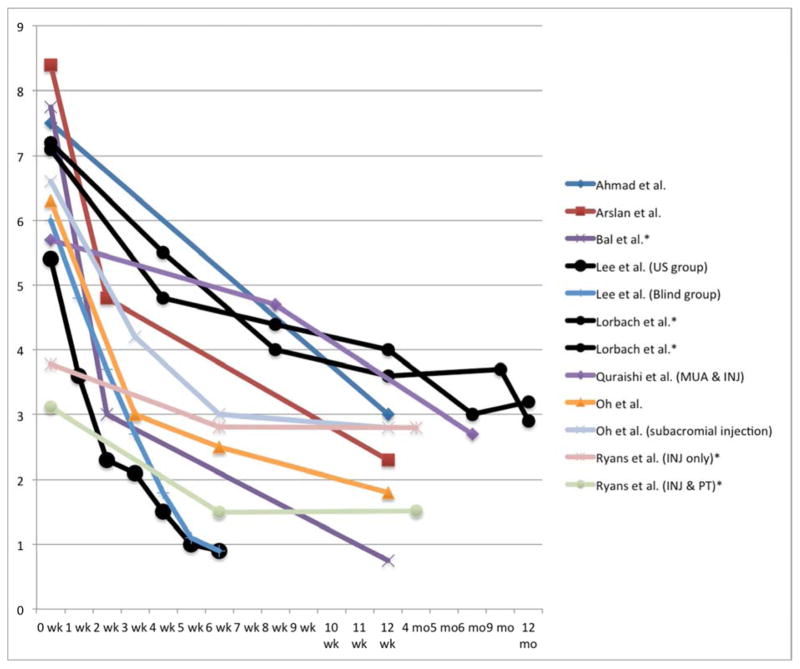
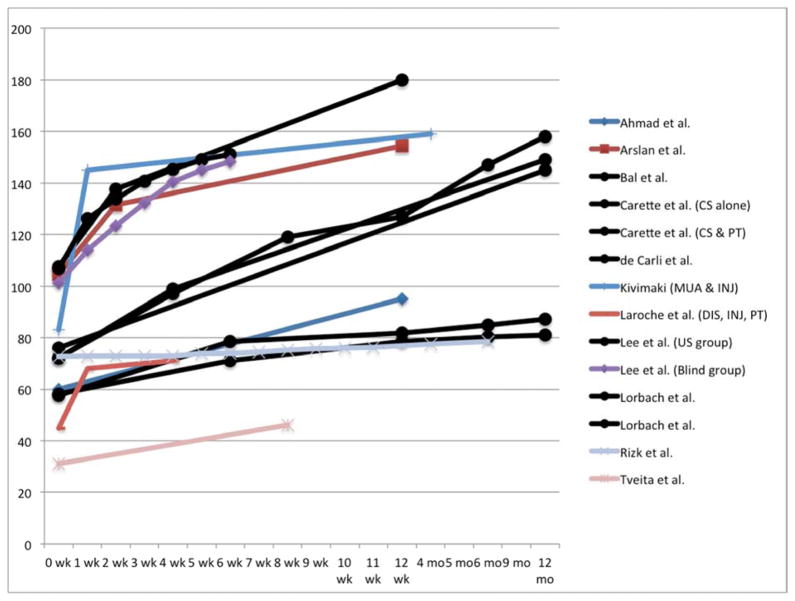
Overall, most studies show an increased improvement in VAS scores and ROM after corticosteroid injections in the first 1–6 weeks as compared with the control or comparison group (Figures 2 and 3). Also, seven of the eight studies that provided image-guided injections showed statistically significant ROM improvements by within 12 weeks of follow-up.
Figure 2.
VAS improvements over time in corticosteroid injection groups. Image-guided injections are indicated with black lines and circle data points. (US = ultrasound, INJ = injection, PT = physical therapy)
*Visual analog scale adjusted to a 0 to 10 scale where 0 represents “no pain” and 10 represents the “worst possible pain”
Figure 3.
Abduction improvements over time in corticosteroid injection groups. Image-guided injections are indicated with black lines and circle data points. (CS = Corticosteroid injection; DIS = Distension; INJ = injection; MUA = manipulation under anesthesia; PT = physical therapy; US = ultrasound)
DISCUSSION
The review of the literature indicates that corticosteroid injections in the setting of adhesive capsulitis may offer initial improvements in shoulder pain and function for the first 1–6 weeks. However, beyond 6 to 12 weeks, corticosteroid injections may not offer significantly added benefits in improving pain and ROM compared to physical therapy. Studies comparing corticosteroid injection to manipulation under anesthesia or dilation have mixed results. Image-guided injections also provide improvements in function, pain, and ROM within the first 12 weeks but their added benefit over non-image guided shoulder injections is inconclusive.
The injection groups of the two studies investigating steroid injections alone or along with a placebo injection showed improvement in range of motion and pain at 12 weeks19,30. It can also be hypothesized that a placebo injection can provide therapeutic benefit by distention of the joint capsule. Compared to a physical therapy regimen alone, corticosteroid injections may offer significantly greater improvements in SPADI score32, Shoulder Disability Questionnaire score33, and range of motion42 by six weeks follow-up. But a combined corticosteroid injection and physical therapy treatment may have greater ROM improvements than either treatment alone32. The results of dilation or distension of the glenohumeral joint compared to injection is mixed36,17. The results for studies comparing MUA to injection are also mixed28,34,35.
Based on the results of studies that compared steroid dosages, location of injection, or types of steroid, injections of intra-articular, 40 mg triamcinolone acetate provide the greatest relief in terms of pain and ROM improvement when compared with extra-articular injections, injections of methylprednisolone, injection of 10 mg of triamcinolone acetate, or oral prednisolone.
Although a clear conclusion on the long-term effectiveness of corticosteroid injections cannot be made due to disparate findings between studies, inadequate study designs and research methodology, and inconsistent outcomes across studies, several studies show that injections provide rapid relief of pain and increase ROM in the first 6 weeks after treatment. The control or comparison groups also show a decrease in VAS, although the improvement occurs at a slower rate than the corticosteroid injection groups. Similarly, abduction improves more rapidly for corticosteroid injection groups relative to the control or comparison groups.
We hypothesize two possible reasons for inconclusive findings between studies. First, only eight studies specifically included patients in the second or third stage of adhesive capsulitis or those with less than 12 months of symptom duration18,19,32,33,38,40,41,43. Studies including patients with greater than 12–18 months of symptom duration may have injected corticosteroids well into the second/third stage of adhesive capsulitis when the painful inflammatory process is reduced. Thus, the efficacy of corticosteroid injections may be reduced in these studies.
Second, the lack of image-guidance may have lead to disparate conclusions in studies. Only eight studies in this review reported an image-guided injection technique that ensured intra-articular placement of all corticosteroid injections - five used fluoroscopy and three used ultrasound17,18,32,36,38,40,41,44. Studies have shown low accuracy of glenohumeral injections performed without image guidance. Only 26.8%–64.7% of injections using an anterior approach without the use of image-guidance were intra-articular22–24. Tobola et al. found the accuracy of an anterior approach glenohumeral injection was 64.7%, regardless of clinician experience24. In comparison to a blind posterior injection technique, ultrasound guided injections had a greater success rate of reaching of the glenohumeral joint (72.5% vs. 92.5%)26. Daley et al. reported glenohumeral joint injections with image guidance had an average accuracy rate of 95% (range: 83–100%) compared to 79% without image guidance (27–100%)25. Kim et al. found a 100% injection accuracy score using ultrasound to guide glenohumeral injections on 12 cadavers45. However, there is a paucity of data on the clinical efficacy of image-guided injections for improved shoulder outcomes when performing glenohumeral corticosteroid injections.
The studies using image-guided injections were effective for improving range of motion and pain. Seven of these studies reported statistically significant improvements in ROM at 12 weeks of follow-up or earlier for groups receiving an image guided corticosteroid injection17,18,32,38,40,41,44. It is unclear if the accurate placement of corticosteroid into the glenohumeral joint has a positive impact on shoulder outcomes in the treatment of adhesive capsulitis. However, we hypothesize that if corticosteroids are not consistently being placed into the glenohumeral joint without the aid of imaging, the potential benefits of corticosteroids on shoulder pain and function may not be fully realized. Nevertheless, the literature in this area is lacking and we are unable to comment on the added benefit or lack thereof of adding an imaging component to guide corticosteroid injections.
CONCLUSION
Corticosteroid injections offer rapid relief of pain and improved range of motion in the short-term (particularly in the first 6 weeks) although long-term outcomes seem to be similar to other treatments including placebo. This is likely because the natural history of adhesive capsulitis is to spontaneously resolve over time. Hence, corticosteroid injections may offer pain relief in the initial phases of adhesive capsulitis when patients have the most pain. Also, seven of 8 studies using image-guided injections in this review found ROM improvements within 12 weeks. Image-guided corticosteroid injections increase the accuracy of the injection, which may improve shoulder outcomes. However, there is limited data on the clinical efficacy ultrasound or fluoroscopically guided injections to make conclusions on their added benefit over non-image guided injections. The necessity and efficacy of image-guided corticosteroid injections, by ultrasound or otherwise, in the management of adhesive capsulitis warrants further investigation.
Acknowledgments
Funding: Dr. Jain is supported by funding from National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) project number 1K23AR059199, Foundation for PM&R, and Biomedical Research Institute at Brigham and Women’s Hospital.
This paper is not a clinical trial and was not applicable for review by an institutional review board (IRB). We declare no financial support or other benefits from commercials sources for the work reported on the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tasto JP, Elias DW. Adhesive capsulitis. Sports Med Arthrosc Rev. 2007;15(4):216–221. doi: 10.1097/JSA.0b013e3181595c22. [DOI] [PubMed] [Google Scholar]
- 2.Neviaser AS, Neviaser RJ. Adhesive capsulitis of the shoulder. J Am Acad Orthop Surg. 2011;19(9):536–542. doi: 10.5435/00124635-201109000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Hannafin JA, Chiaia TA. Adhesive capsulitis. A treatment approach. Clin Orthop. 2000;(372):95–109. [PubMed] [Google Scholar]
- 4.Boyle-Walker KL, Gabard DL, Bietsch E, Masek-VanArsdale DM, Robinson BL. A profile of patients with adhesive capsulitis. J Hand Ther. 1997;10(3):222–228. doi: 10.1016/S0894-1130(97)80025-7. [DOI] [PubMed] [Google Scholar]
- 5.Neviaser AS, Hannafin JA. Adhesive Capsulitis A Review of Current Treatment. Am J Sports Med. 2010;38(11):2346–2356. doi: 10.1177/0363546509348048. [DOI] [PubMed] [Google Scholar]
- 6.Balci N, Balci MK, Tüzüner S. Shoulder Adhesive Capsulitis and Shoulder Range of Motion in Type II Diabetes Mellitus: Association with Diabetic Complications. J Diabetes Complications. 1999;13(3):135–140. doi: 10.1016/S1056-8727(99)00037-9. [DOI] [PubMed] [Google Scholar]
- 7.Wohlgethan JR. Frozen shoulder in hyperthyroidism. Arthritis Rheum. 1987;30(8):936–939. doi: 10.1002/art.1780300815. [DOI] [PubMed] [Google Scholar]
- 8.Bowman CA, Jeffcoate WJ, Pattrick M, Doherty M. Case report: bilateral adhesive capsulitis, oligoarthritis and proximal myopathy as presentation of hypothyroidism. Rheumatology. 1988;27(1):62–64. doi: 10.1093/rheumatology/27.1.62. [DOI] [PubMed] [Google Scholar]
- 9.Riley D, Lang AE, Blair RD, Birnbaum A, Reid B. Frozen shoulder and other shoulder disturbances in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1989;52(1):63–66. doi: 10.1136/jnnp.52.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tuten HR, Young DC, Douoguih WA, Lenhardt KM, Wilkerson JP, Adelaar RS. Adhesive capsulitis of the shoulder in male cardiac surgery patients. Orthopedics. 2000;23(7):693–696. doi: 10.3928/0147-7447-20000701-16. [DOI] [PubMed] [Google Scholar]
- 11.Ewald A. Adhesive Capsulitis: A Review. American Family Physician; Feb 15, 2011. [Accessed July 17, 2012]. Available at: http://www.aafp.org.ezproxy.bu.edu/afp/2011/0215/p417.html. [PubMed] [Google Scholar]
- 12.Weinstein SL, Buckwalter JA, editors. Turek’s Orthopaedics, Principles and Their Application. 5. Philadelphia, PA: J.B. Lippincott Company; 1994. [Google Scholar]
- 13.Shoulder Frozen. OrthoInfo. AAOS; [Accessed July 17, 2012]. Available at: http://orthoinfo.aaos.org/topic.cfm?topic=a00071. [Google Scholar]
- 14.Griesser MJ, Harris JD, Campbell JE, Jones GL. Adhesive capsulitis of the shoulder: a systematic review of the effectiveness of intra-articular corticosteroid injections. J Bone Joint Surg Am. 2011;93(18):1727–1733. doi: 10.2106/JBJS.J.01275. [DOI] [PubMed] [Google Scholar]
- 15.Blockey NJ, Wright JK, Kellgren JH. Oral Cortisone Therapy in Periarthritis of the Shoulder. Br Med J. 1954;1(4877):1455–1457. doi: 10.1136/bmj.1.4877.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buchbinder R, Hoving JL, Green S, Hall S, Forbes A, Nash P. Short course prednisolone for adhesive capsulitis (frozen shoulder or stiff painful shoulder): a randomised, double blind, placebo controlled trial. Ann Rheum Dis. 2004;63(11):1460–1469. doi: 10.1136/ard.2003.018218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tveitå EK, Tariq R, Sesseng S, Juel NG, Bautz-Holter E. Hydrodilatation, corticosteroids and adhesive capsulitis: a randomized controlled trial. BMC Musculoskelet Disord. 2008;9:53. doi: 10.1186/1471-2474-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Carli A, Vadalà A, Perugia D, et al. Shoulder adhesive capsulitis: manipulation and arthroscopic arthrolysis or intra-articular steroid injections? Int Orthop. 2012;36(1):101–106. doi: 10.1007/s00264-011-1330-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bal A, Eksioglu E, Gulec B, Aydog E, Gurcay E, Cakci A. Effectiveness of corticosteroid injection in adhesive capsulitis. Clin Rehabil. 2008;22(6):503–512. doi: 10.1177/0269215508086179. [DOI] [PubMed] [Google Scholar]
- 20.Blanchard V, Barr S, Cerisola FL. The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: A systematic review. Physiotherapy. 2010;96(2):95–107. doi: 10.1016/j.physio.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Shah N, Lewis M. Shoulder adhesive capsulitis: systematic review of randomised trials using multiple corticosteroid injections. Br J Gen Pract J R Coll Gen Pract. 2007;57(541):662–667. [PMC free article] [PubMed] [Google Scholar]
- 22.Eustace JA, Brophy DP, Gibney RP, Bresnihan B, FitzGerald O. Comparison of the accuracy of steroid placement with clinical outcome in patients with shoulder symptoms. Ann Rheum Dis. 1997;56(1):59–63. doi: 10.1136/ard.56.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sethi PM, Kingston S, Elattrache N. Accuracy of anterior intra-articular injection of the glenohumeral joint. Arthrosc J Arthrosc Relat Surg. 2005;21(1):77–80. doi: 10.1016/j.arthro.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 24.Tobola A, Cook C, Cassas KJ, et al. Accuracy of glenohumeral joint injections: comparing approach and experience of provider. J Shoulder Elbow Surg. 2011;20(7):1147–1154. doi: 10.1016/j.jse.2010.12.021. [DOI] [PubMed] [Google Scholar]
- 25.Daley EL, Bajaj S, Bisson LJ, Cole BJ. Improving injection accuracy of the elbow, knee, and shoulder: does injection site and imaging make a difference? A systematic review. Am J Sports Med. 2011;39(3):656–662. doi: 10.1177/0363546510390610. [DOI] [PubMed] [Google Scholar]
- 26.Patel DN, Nayyar S, Hasan S, Khatib O, Sidash S, Jazrawi LM. Comparison of ultrasound-guided versus blind glenohumeral injections: a cadaveric study. J Shoulder Elbow Surg. 2012;21(12):1664–1668. doi: 10.1016/j.jse.2011.11.026. [DOI] [PubMed] [Google Scholar]
- 27.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 28.Sharma R, Bajekal R, Bhan S. Frozen shoulder syndrome: A comparison of hydraulic distension and manipulation. Int Orthop. 1993;17:275–278. doi: 10.1007/BF00181697. [DOI] [PubMed] [Google Scholar]
- 29.Oh JH, Oh CH, Choi J-A, Kim SH, Kim JH, Yoon JP. Comparison of glenohumeral and subacromial steroid injection in primary frozen shoulder: a prospective, randomized short-term comparison study. J Shoulder Elbow Surg. 2011;20(7):1034–1040. doi: 10.1016/j.jse.2011.04.029. [DOI] [PubMed] [Google Scholar]
- 30.Ahmad I, Askar Z, Durrani Z, et al. Intraarticular injection of methylprednisolone for idiopathic frozen shoulder. J Med Sci. 2009;17(1):16–18. [Google Scholar]
- 31.Arslan, Çeliker R. Comparison of the efficacy of local corticosteroid injection and physical therapy for the treatment of adhesive capsulitis. Rheumatol Int. 2001;21(1):20–23. doi: 10.1007/s002960100127. [DOI] [PubMed] [Google Scholar]
- 32.Carette S, Moffet H, Tardif J, et al. Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: A placebo-controlled trial. Arthritis Rheum. 2003;48(3):829–838. doi: 10.1002/art.10954. [DOI] [PubMed] [Google Scholar]
- 33.Ryans I, Montgomery A, Galway R, Kernohan WG, McKane R. A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatol Oxf Engl. 2005;44(4):529–535. doi: 10.1093/rheumatology/keh535. [DOI] [PubMed] [Google Scholar]
- 34.Kivimäki J, Pohjolainen T. Manipulation under anesthesia for frozen shoulder with and without steroid injection. Arch Phys Med Rehabil. 2001;82(9):1188–1190. doi: 10.1053/apmr.2001.24169. [DOI] [PubMed] [Google Scholar]
- 35.Jacobs LG, Smith MG, Khan SA, Smith K, Joshi M. Manipulation or intra-articular steroids in the management of adhesive capsulitis of the shoulder? A prospective randomized trial. J Shoulder Elbow Surg. 2009;18(3):348–353. doi: 10.1016/j.jse.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 36.Gam AN, Schydlowksy P, Rossel I, Remvig L, Jensen E. Treatment of “Frozen Shoulder” with distension and glucorticoid compared with glucorticoid alone. Scand J Rheumatol. 1998;27:425–30. doi: 10.1080/030097498442244. [DOI] [PubMed] [Google Scholar]
- 37.De Jong B, Dahmen R, Hogeweg J. Intra-articular triamcinolone acetonide injection in patients with capsulitis of the shoulder: a comparative study of two dose regimens. Clin Rehabil. 1998;12:211–215. doi: 10.1191/026921598673772420. [DOI] [PubMed] [Google Scholar]
- 38.Lorbach O, Anagnostakos K, Scherf C, Seil R, Kohn D, Pape D. Nonoperative management of adhesive capsulitis of the shoulder: Oral cortisone application versus intra-articular cortisone injections. J Shoulder Elbow Surg. 2010;19(2):172–179. doi: 10.1016/j.jse.2009.06.013. [DOI] [PubMed] [Google Scholar]
- 39.Rizk TE, Pinals RS, Talaiver AS. Corticosteroid injections in adhesive capsulitis: investigation of their value and site. Arch Phys Med Rehabil. 1991;72(1):20–22. [PubMed] [Google Scholar]
- 40.Lee H-J, Lim K-B, Kim D-Y, Lee K-T. Randomized Controlled Trial for Efficacy of Intra-Articular Injection for Adhesive Capsulitis: Ultrasonography-Guided Versus Blind Technique. Arch Phys Med Rehabil. 2009;90(12):1997–2002. doi: 10.1016/j.apmr.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 41.Lorbach O, Kieb M, Scherf C, Seil R, Kohn D, Pape D. Good results after fluoroscopic-guided intra-articular injections in the treatment of adhesive capsulitis of the shoulder. Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1435–1441. doi: 10.1007/s00167-009-1030-7. [DOI] [PubMed] [Google Scholar]
- 42.Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S. Frozen shoulder: prospective clinical study with an evaluation of three treatment regimens. Ann Rheum Dis. 1984;43(3):353–360. doi: 10.1136/ard.43.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Quraishi NA, Johnston P, Bayer J, Crowe M, Chakrabarti AJ. Thawing the frozen shoulder A RANDOMISED TRIAL COMPARING MANIPULATION UNDER ANAESTHESIA WITH HYDRODILATATION. J Bone Jt Surg. 2007;89(9):1197–1200. doi: 10.1302/0301-620X.89B9.18863. [DOI] [PubMed] [Google Scholar]
- 44.Mitra R, Harris A, Umphrey C, Smuck M, Fredericson M. Adhesive Capsulitis: A New Management Protocol to Improve Passive Range of Motion. PM&R. 2009;1(12):1064–1068. doi: 10.1016/j.pmrj.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 45.Kim JS, Kim M-W, Park DY. Indirect ultrasound guidance increased accuracy of the glenohumeral injection using the superior approach: a cadaveric study of injection accuracy. Ann Rehabil Med. 2013;37(2):202–207. doi: 10.5535/arm.2013.37.2.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.White A, Tuite J. The accuracy and efficacy of shoulder injections in restrictive capsulitis. J Orthop Rheumatol. 1996;9:37–40. [Google Scholar]
- 47.Sakeni R, Al-Nimer MS. Comparison between intraarticular tria. Saudi Med J. 2007;28(5):707–712. [PubMed] [Google Scholar]
- 48.Levine WN, Kashyap CP, Bak SF, Ahmad CS, Blaine TA, Bigliani LU. Nonoperative management of idiopathic adhesive capsulitis. J Shoulder Elbow Surg. 2007;16(5):569–573. doi: 10.1016/j.jse.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 49.Laroche M, Ighilahriz O, Moulinier L, Constantin A, Mazieres B. Adhesive capsulitis of the shoulder: an open study of 40 cases treated by joint distension during arthrography followed by an intraarticular corticosteroid injection and immediate physical therapy. Rev Rhum Engl Ed. 1998;65(5):313–319. [PubMed] [Google Scholar]
- 50.Siraj M, Anwar W, Iqbal MJ, et al. Effectiveness of Intra-articular Corticosteroid Injection in the Treatment of Idiopathic Frozen Shoulder. J Surg Pak. 2012;17(2):57–60. [Google Scholar]