Abstract
Objective
To compare landing mechanics and neuromuscular recruitment strategies between women with semitendinosus-gracilis anterior cruciate ligament reconstruction (SG-ACLr) and non-injured women during double and single-legged drop jumps.
Design
Cross-sectional biomechanical study
Setting
Single university-based biomechanics laboratory
Participants
Fourteen women 1–5 years post SG-ACLr and 16 non-injured women participated in this study.
Methods
After anthropometric measurements, warm-up, and familiarization procedures, participants performed five trials of a double and single-legged drop jumps.
Main Outcome Measurements
Dynamic knee valgus was measured as the distance between knee joints during the landing phase of the double-leg drop jumps. Medial knee displacement was the outcome considered during the landing phase of the single-leg drop jumps. For both drop jumps tasks neuromuscular recruitment was evaluated through rectified normalized electromyography (EMG) activity of the quadriceps and hamstrings (amplitude and latency), and quadriceps/hamstrings EMG co-contraction ratio.
Results
Although the SG- ACLr group demonstrated a tendency towards a greater dynamic knee valgus during both drop jumps, these differences did not reach statistical significance. EMG data revealed different neuromuscular strategies for each group depending on the specific jump.
Conclusions
These findings suggest that women with SG-ACLr have a tendency towards greater dynamic knee valgus which could predispose to additional knee injuries. Rehabilitation specialists need to be aware of existing kinematic and neuromuscular deficiencies years after SG-ACLr. Taking this into consideration will aid in prescribing appropriate interventions designed to prevent re-injury.
INTRODUCTION
Anterior cruciate ligament reconstruction (ACLr) is often recommended after an ACL tear, especially for young active individuals who desire to return to high levels of physical activity [1,2]. Although ACLr technique with bone-patellar-tendon-bone (BPTB) autograft is considered as the gold standard [3], some orthopedic surgeons prefer the Semitendinosus-Gracilis (SG) autograft because of its apparent structural strength, sparing of the extensor mechanism, and less graft morbidity [4,5]. These traits are important during high impact activities in which the majority of ACL injuries often occur. Additionally, the literature reports that SG reconstruction yields better results in patient satisfaction surveys, knee strength and endurance, and functional hop tests [4].
It is known that women exhibit small joint angles and larger joint moments when landing from jumps or performing cutting maneuvers when compared to their male counterparts, increasing their predisposition to knee injury [6–9]. These gender-specific biomechanical differences represent less than optimal biomechanical control, leading to decreased dynamic knee stability and increased risk for ACL injury. Knee stability during dynamic tasks is accomplished by combining passive restrictors and dynamic mechanisms. Thus, both kinematic and neuromuscular factors such as muscle activation, recruitment, or firing patterns, must be taken into consideration to accurately characterize dynamic knee stability.
In order to quantify knee stability, researchers have measured knee valgus during static and dynamic tasks [10–13]. Dynamic knee valgus is characterized by the motion of the distal femur towards midline, and the distal tibia away from the midline of the body. This movement is a combination of reduced knee flexion and increased hip adduction, hip internal rotation, and knee abduction [14,15]. Proper recovery of neuromuscular activity after ACLr is of vital importance to regain appropriate mechanical function of the knee joint and prevent further injuries [6,16]. Evidence suggests that women with ACL reconstructions exhibit compensatory neuromuscular strategies such as altered quadriceps/hamstring co-contraction ratios upon landing, reduced quadriceps femoris activation, increased plantar flexor activation, and quadriceps and hamstrings timing adaptations [6,17,18]. In addition, normal voluntary muscle control has shown to be reestablished to pre-surgery status after SG reconstruction [5]. When researchers compared pre-surgery and post-surgery (6 months after surgery) muscle control of the semitendinosus and gracilis, no differences were found in the ability of these muscles to control voluntary contractions [5]. In addition, modifications to neuromuscular strategies have been reported to occur after ACLr in order to achieve dynamic stability during drop jumps [6]. Greater quadriceps/hamstring EMG co-contraction ratios, greater activation of gluteal muscles, greater rectus femoris activation, and similar hamstrings muscle activity during single-leg drop jumps have also been reported in the literature. However, these compensatory strategies could negatively impact sports performance by increasing reaction time and reducing the capacity to absorb impact [13,19]. Following ACLr, subjective procedures and instrumented strength measurements are frequently used to determine recovery. However, these tests and procedures have shown only moderate correlation with functional performance [20].
Examination of athletic tasks in individuals with SG-ACLr may provide insight about functional capacity and assessment of post-surgical re-injury risk, and may prove beneficial for the development of diagnostic and rehabilitative tools [6,18]. Drop jumps are an appropriate task to test functional performance after ACLr due to their resemblance to sports specific maneuvers and their capability of generating knee valgus moments and challenging the neuromuscular system [10].
The existent body of evidence has not determined if kinematic predisposing factors and lack of muscular control persist after SG-ACLr during unplanned athletic activities that require high-levels of dynamic stability [6,21]. To our knowledge, no previous study has compared landing mechanics and muscle recruitment and firing patterns between women with SG-ACLr and healthy controls during the performance of drop jump tasks. Therefore, the purpose of this study was to compare dynamic knee stability and neuromuscular control between women with SG-ACLr and non-injured women during drop jumps. It was hypothesized that women with SG-ACLr would exhibit larger knee valgus and EMG activity predisposing to knee injury during both jumps and these differences would be greater in the single leg drop jump.
METHODS
Study Design
A cross sectional study comparing landing mechanics between healthy women and women with SG-ACL reconstruction during two drop jump conditions was conducted. A 60-cm double-legged and 40-cm single-legged drop jumps were used as functional tasks to assess bilateral and unilateral landing strategies, respectively. The dependent variables were comprised of kinematic (valgus) and neuromuscular (electromyography) factors. Specifically, the kinematic assessment consisted of dynamic knee valgus, while the EMG analyses comprised of amplitude, latency, and co-contraction assessments. Sample size was determined based on previous studies [6]. Based on a previously published effect size of 0.32 for knee valgus and a significance level of 0.05, a total sample of 39 subjects was needed to reach 80% of power. However, due to the inability to identify more than 15 subjects with ACL reconstruction from the same orthopedic surgeon and the desire to keep an even number of participants per group, a total of 30 participants were contacted for possible recruitment.
Participants
Fifteen women with SG-ACLr (height: 167.71 ± 9.0 cm, body mass: 67.68 ± 11.66 kg) who underwent ACLr with the same orthopedic surgeon and performed the same rehabilitation protocol were recruited. Non-injured control subjects (n=16) were recruited from the collegiate community (height: 160.50 ± 5.17 cm, body mass: 59.35 ± 10.37 kg). Both groups were between the ages of 21–35 years old. All of the women with ACL reconstruction, except two, were injured while participating in competitive volleyball at the collegiate or professional level. To ensure a similar level of athletic skills, the control subjects were participating in volleyball, basketball, and soccer at the collegiate or intramural sports level. At the moment of recruitment, all participants reported engaging in sports-specific physical activities as described by the Activity Rating Scale [22]. Participants reported scores ranging from twelve to sixteen; consistent with activities such as running, cutting, decelerating, and pivoting over two times a week, which is, considered a high-level of participation [22]. All participants read and signed an informed consent approved by the Institutional Review Board previous to participation in the study.
All SG-ACLr women were selected from the computer database of a single orthopedic surgeon to control for possible bias due to surgical technique. In the same manner, all patients underwent the same rehabilitation protocol set by the orthopedic surgeon. The rehabilitation protocol initially targeted acute inflammation and range of motion with progression towards strengthening, functional activities, and neuromuscular reeducation until return to pre-injury level was accomplished. Patients were contacted chronologically from 2006 to 2010 and asked if they were willing to participate in the study. Time since surgery was between twelve months and five years. Although time since surgery had a five year range, all subjects were allowed to return to all of their pre-injury activities without restrictions. Control participants were recruited from the collegiate community using flyers. Participants with ACLr were excluded if they demonstrated at least one of the following: inability to stick the landing or perform two screening tasks (single-hop for distance and cross-over hop), and signs and symptoms of knee instability in the reconstructed limb during these tasks. These two tasks are commonly used as physical performance measures in individuals recovering from ACL injury or surgical reconstruction. Moreover, these tasks have been reported as being comparable to high functional demands needed in sports [11,23]. Further exclusion criteria for the ACLr group were: signs or reports of swelling and/or effusion after physical activity fear to perform high-demand physical activity, multiple (>1) surgeries in the same knee, and/or self-reported pregnancy. Non-injured subjects were excluded if they had experienced any lower back or lower extremity injury within the past six months, had any surgery of the lower back or lower extremity, and/or self-reported pregnancy.
Instrumentation
Three-dimensional lower extremity kinematics was captured using a real time motion analysis system with five infrared cameras (Nexus 1.3; MX13+; 120 Hz sampling rate, Vicon Motion Systems, Denver, CO). Twenty-five millimeter spherical reflective markers were placed over the skin of both lower extremities according to Vicon’s lower extremity Plug-in Gait model (Fig. 1). Prior to each data collection session, the equipment was calibrated according to manufacturer’s recommendations and a static trial to estimate participant’s joint centers was conducted.
Figure 1.
Plug-in-gait Model Retro-reflective Marker Setting (Vicon Motion System, Denver, CO).
Muscle activity of the vastus medialis, vastus lateralis, rectus femoris, and medial and lateral hamstrings were measured in the involved leg of women with ACLr and the dominant leg of the control subjects using surface electromyography (EMG) (Bagnoli™ EMG System; Delsys®, Inc. Boston, MA). Pre-amplified Ag/AgCI surface EMG electrodes (Signal Bandwidth: 20Hz–450Hz [-3dB]; Impedance: >100KΩ; Noise: <1.2µV RMS; Sampling rate: 1kHz) with two embedded 10.0 × 1.0 mm bars (10.0 mm space between bars) were used to record muscular activity. Surface EMG electrodes were applied on the skin over the muscles of interest as reported previously [6]. Prior to positioning the electrodes over the muscles of interest, the skin over those locations was cleansed in order to decrease skin impedance. Hypoallergenic tape and stretchable straps were used over the electrodes to minimize artifact movement during performance of functional tasks. The EMG unit was connected to the main amplifier where signals were amplified (gain = 1000) and filtered by using a bandpass filter (20Hz – 450 Hz). The amplifier was connected via BNC cables to an analog-to-digital (A/D) interface unit connected to a Vicon MX system linked to a Vicon MX Ultranet interfaced with the computer. Two foot-switches (Delsys® Foot Switch Biosensors, Sampling rate: 500 Hz, Boston, MA, USA) placed at the mid-plantar aspect of the hallux and plantar aspect of the calcaneus were secured with athletic tape to the foot of the limb with the ACLr and to the foot of the dominant leg to identify the events of initial contact and toe-off during the ground contact phase of the drop jumps for the SG-ACLr and control groups, respectively.
Procedures
After consenting, each participant performed a set of two screening tasks as clearance for participation. For the control subjects, leg dominance was determined as the preferred leg to perform the two screening tasks to ensure the best possible jumping landing performance. The single hop for distance and cross-over hop were performed as previously reported [6]. Any participant unable to perform either of these tasks was excluded from participating in the investigation. Following screening procedures, anthropometric measures according to Vicon’s Plug-in-Gait procedures were recorded. Subsequently, each participant was instrumented with reflective markers, surface EMG electrodes and foot switches. Each participant performed a standardized warm-up protocol consisting of five minutes on a cycle ergometer at 40–60 revolutions per minute, 10 squats, and five seconds of repetitive counter-movement jumps previous to the drop-jumps.
After warm-up, all women were allowed to practice both jump tasks three times. During practice jumps, women with ACLr performed the Single Leg Landing Countermovement Jump (SLJ) task with the reconstructed leg, while the non-injured control group performed the task with their dominant leg. Study data was recorded only after a rest period of five minutes following the completion of the warm-up and practice protocol. The specific procedures for each of the jump tasks were as follows:
Double Leg Landing Countermovement Jump (DLJ)
Each participant stood on top of a 60-cm box. Participants were given the command “on your mark” as a signal to stand ready and prepare to perform the jump. A second command, “get set”, was given as a signal to let the participant know she may jump whenever ready. Participants were instructed to drop from the box instead of jumping. If any participant was observed jumping from the box creating an upward movement the trial was invalidated and repeated. Participants were allowed to use their arms for balance at any time after initiating the jump. After landing, each participant had to perform a maximal upward jump. In order to ensure a maximal effort upward jump, participants were instructed to try to touch the ceiling of the laboratory [24]. Each participant performed five trials of this task, and was required to rest at least 30 seconds between trials in order to avoid fatigue [8].
Single Leg Landing Countermovement Jump (SLJ)
Each participant stood on top of a 40-cm box. The procedures of this task were similar to the DLJ. Each participant performed five trials with a single leg. Subjects with ACL reconstruction performed this task using their leg with the reconstructed knee, while control subjects used their dominant leg (preferred leg to perform a single-hop for distance). Rest intervals were similar to the rest in the double-legged drop jump.
Data Reduction
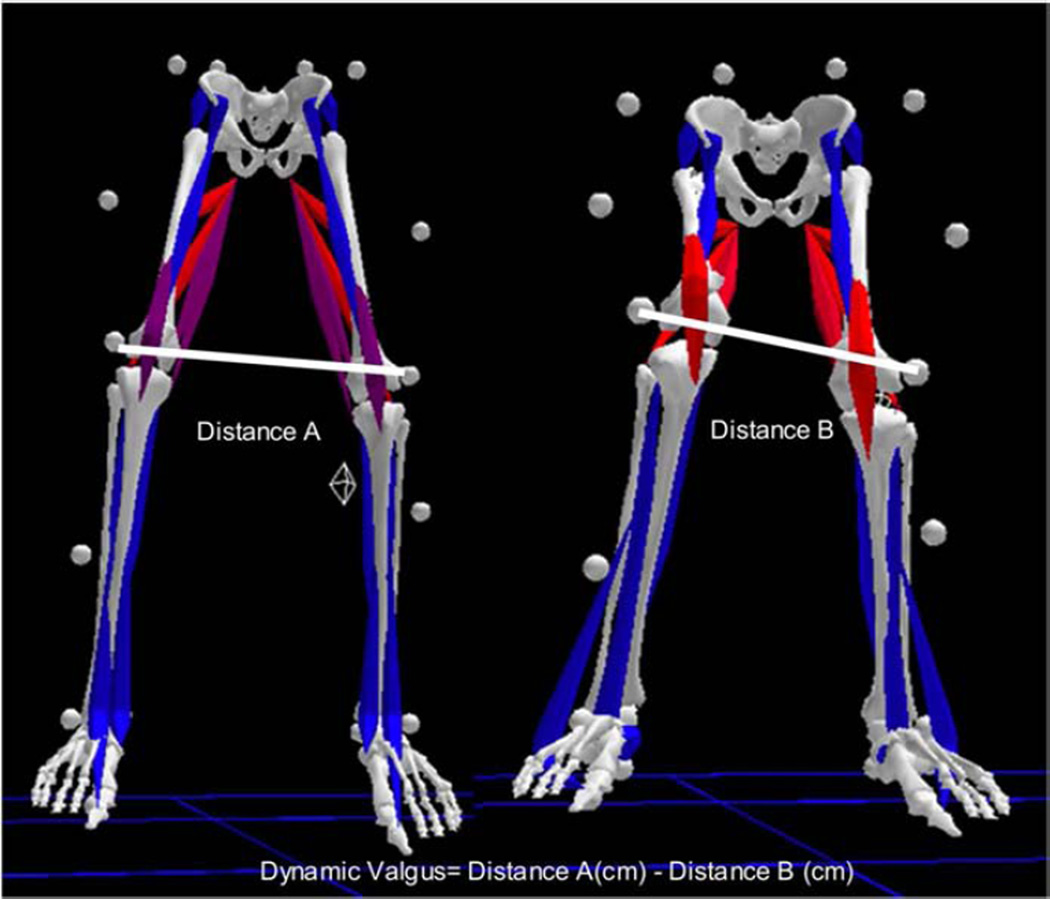
The kinematic outcome evaluated during the jumps was the dynamic knee valgus during the entire ground contact phase (initial contact to takeoff). The average of five trials was used for analysis. The ground contact phase was defined as the period between initial foot floor contact and foot push off towards the vertical jump. The trajectory of both lateral femoral epicondyle markers and knee joint centers were derived from the three-dimensional trajectory of markers filtered through a Woltring filter. Dynamic knee valgus was defined as the distance between markers, placed at left and right lateral femoral epicondyles, from initial contact to maximum valgus (maximum valgus – initial contact) during the contact phase of the DLJ (Fig 2). Dynamic knee valgus during the SLJ was measured for the landing leg as the maximum distance traveled medially by the knee joint center, from the moment of initial contact to maximum valgus, during the ground contact phase.
Figure 2.
Dynamic knee valgus was defined as the distance between markers placed at the lateral femoral epicondyles at initial contract minus minimum distance between these two markers.
Electromyographic (EMG) data was time-synchronized to kinematic data via a voltage change from foot switches during the ground contact phase of both drop jumps. The time period for the data of interest was similar to kinematic data; from initial contact to push-off. A dynamic normalization procedure was conducted by dividing the mean signal during each specific task trial by the maximum signal generated during the middle three seconds of the five-second tuck jumps performed during warm-up. This normalization approach is recommended to analyze EMG data during dynamic tasks to reduce participants’ variability between trials caused by fatigue and to reduce intersubject variation [6,25–27]. The normalized results were averaged to represent quadriceps and hamstring muscle groups in their entirety; the rectus femoris and vastii averaged muscle activity represented the quadriceps muscle group, and the averaged medial and lateral hamstring muscle activity represented the hamstrings muscle group. To obtain the latency variable for both quadriceps and hamstrings, the time taken to reach maximum contraction from the moment of initial contact was measured in seconds. A co-contraction ratio (CCR) was calculated [6,25,28] by obtaining the normalized values for both the quadriceps and hamstring muscle groups during the targeted window of time. The co-contraction value was always less than or equal to one, representing joint stiffness and the relative activation of the knee flexor and extensor muscle groups [6,25,28]. A co-contraction closer to one indicated optimal co-contraction, protecting the knee joint by increasing joint stability to prevent injury. Values closer to zero represented poor co-contraction between muscle groups, increasing the probability for knee instability and injury.
Data Analysis
The kinematic and EMG data were screened for normality assumptions, homoscedasticity, and outliers using Shapiro-Wilks’ test, Levene’s test, and histograms and box plots, respectively. Intraclass correlation coefficients (ICC) for the average of all five trials (3, k) were estimated to establish the reliability for all kinematic and EMG data across trials for both tasks. The ICC’s were established by correlating the dependent measures across five trials for each subject and then performing a repeated measures analysis of variance (ANOVA) to test for systematic differences between jumping trials for each subject [29]. Given the significant differences for height and weight between groups at baseline, analyses of covariance (ANCOVA) to adjust for these covariates were considered. Given height and weight were different between groups, regression analyses, exploring the relationship between height and weight on dynamic knee valgus, were pursued showing no statistically significant association among these variables. Recent literature has shown that BMI does not affect outcomes in patients after ACL reconstruction [30]. Therefore, we decided to keep the analysis according to Portney and Watkins’ [31] criteria using the baseline differences between groups as covariate to artificially equate both groups based on height and weight. All EMG variables were evaluated using a one-way multivariate analysis of variance (MANOVA). Separate one-way MANOVA for EMG variables was performed for each of the tasks. Univariate tests were conducted only if the MANOVA was statistically significant. Significance was considered at p<0.05. All analyses were performed using SPSS® 16.0 (SPSS Inc., Chicago, IL USA).
RESULTS
Two subjects from the control group were excluded from the SLJ analysis due to computer difficulties in kinematic reconstruction and one subject with ACLr was excluded due to her inability to stick the landing during both tasks. As a result, 14 women with SG-ACLr (height: 167.71 ± 9.0 cm, body mass: 67.68 ± 11.66 kg) were used for analysis for both tasks, whilst 16 and 14 non-injured women (height: 160.50 ± 5.17 cm, body mass: 59.35 ± 10.37 kg) were used for analyses for the double- and single-legged drop jumps, respectively (Table 1). Thus, a total of 30 and 28 subjects were included in the DLJ and SLJ, respectively. Kinematic and EMG amplitude data met all assumptions of normality and homoscedasticity. However, latency variables showed statistically significant differences between their variances. Therefore, Kruskal-Wallis tests were conducted for this variable for both drop jumps. The reliability analyses for kinematic and EMG variables showed that both tasks exhibited excellent reliability (ICC ≥ 0.80) (Table 2).
TABLE 1.
Anthropometric Characteristics
| Anthropometric Measures |
ACL (n=14) | Control (n=16) | p |
|---|---|---|---|
| Age (years) | 28.50 ± 4.59 | 27.69 ± 3.91 | 0.61 |
| Body Mass (kg) | 67.68 ± 11.66 | 59.35 ± 10.37 | 0.044 |
| Height (cm) | 167.71 ± 9.01 | 160.50 ± 5.17 | 0.009 |
| Activity Rating Scale | 14.29 ± 1.38 | 13.81 ± 1.60 | 0.39 |
TABLE 2.
Intraclass Correlation Coefficients (3, k) for the average of five trials during both tasks.
| Task | Group | |
|---|---|---|
| ACL ICC (SEM) |
Control ICC (SEM) |
|
| Double Drop Jump | ||
| Dynamic Knee Valgus (cm) | 0.98 (0.53) | 0.95 (0.52) |
| Normalized Quadriceps (%) | 0.95 (0.83) | 0.99 (0.57) |
| Normalized Hamstrings (%) | 0.97 (0.57) | 0.99 (0.48) |
| Co-contraction Ratio | 0.93 (4.33) | 0.96 (3.72) |
| Latency Quadriceps (s) | 0.95 (0.18) | 0.80 (0.05) |
| Latency Hamstrings (s) | 0.95 (0.17) | 0.92 (0.04) |
| Single Drop Jump | ||
| Dynamic Knee Valgus (cm) | 0.83 (0.72) | 0.86 (0.46) |
| Normalized Quadriceps (%) | 0.96 (0.85) | 0.97 (0.64) |
| Normalized Hamstrings (%) | 0.98 (0.61) | 0.98 (0.56) |
| Co-contraction Ratio | 0.94 (4.20) | 0.95 (4.53) |
| Latency Quadriceps (s) | 0.89 (0.05) | 0.95 (0.26) |
| Latency Hamstrings (s) | 0.89 (0.06) | 0.86 (0.43) |
Double Leg Landing Countermovement Jump (DLJ)
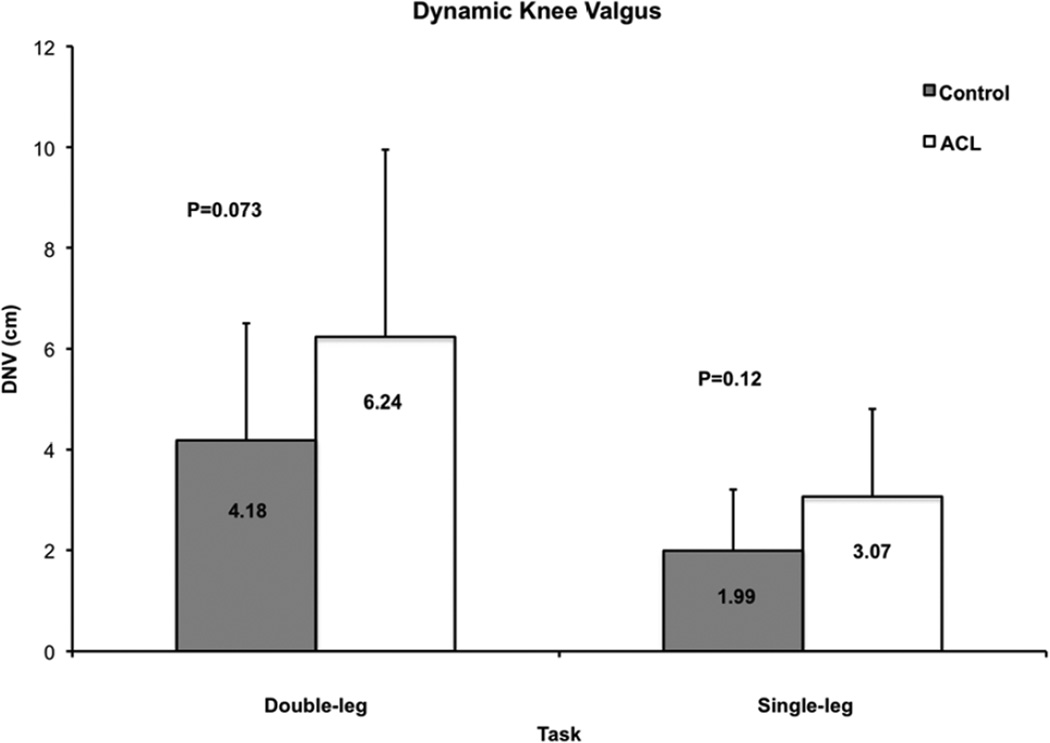
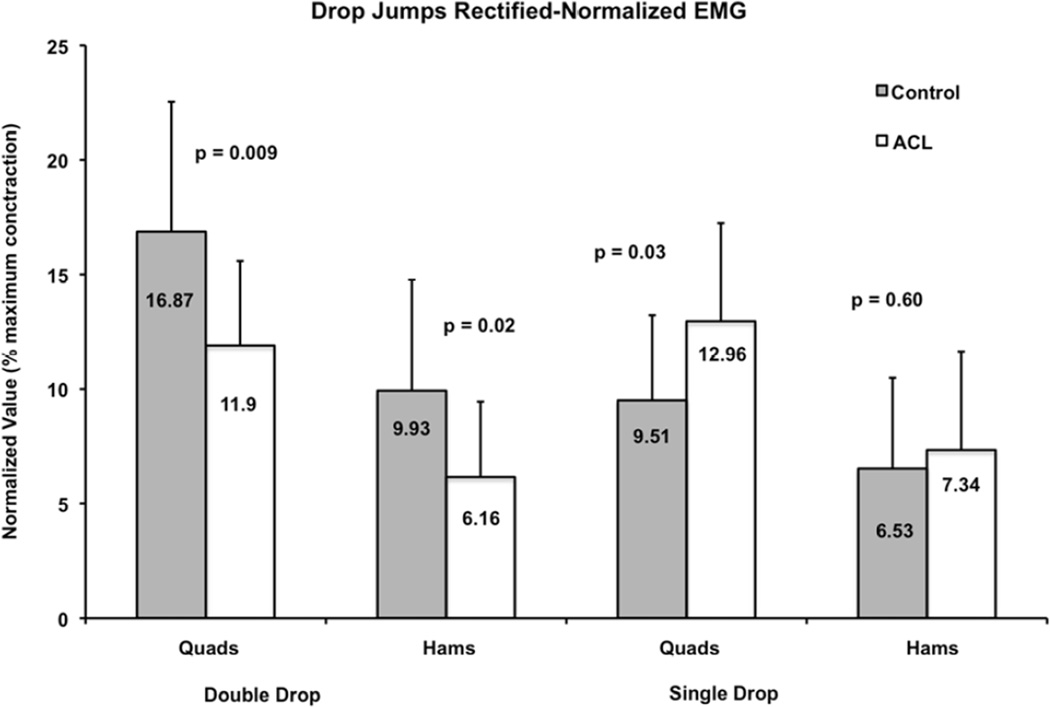
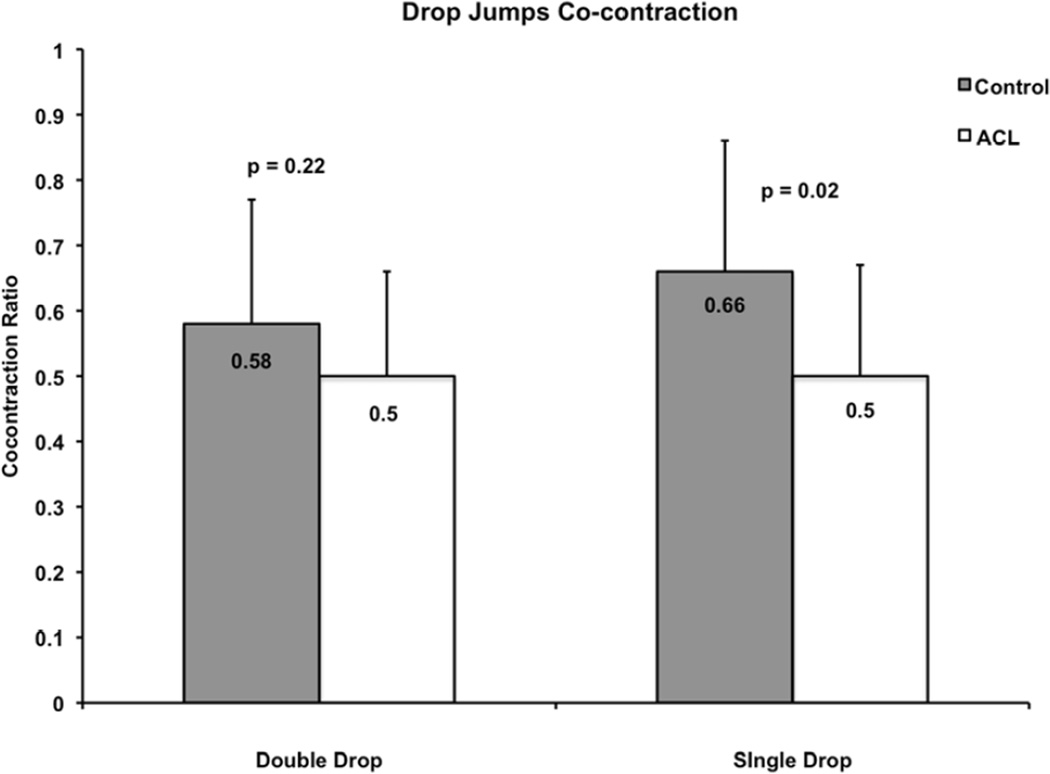
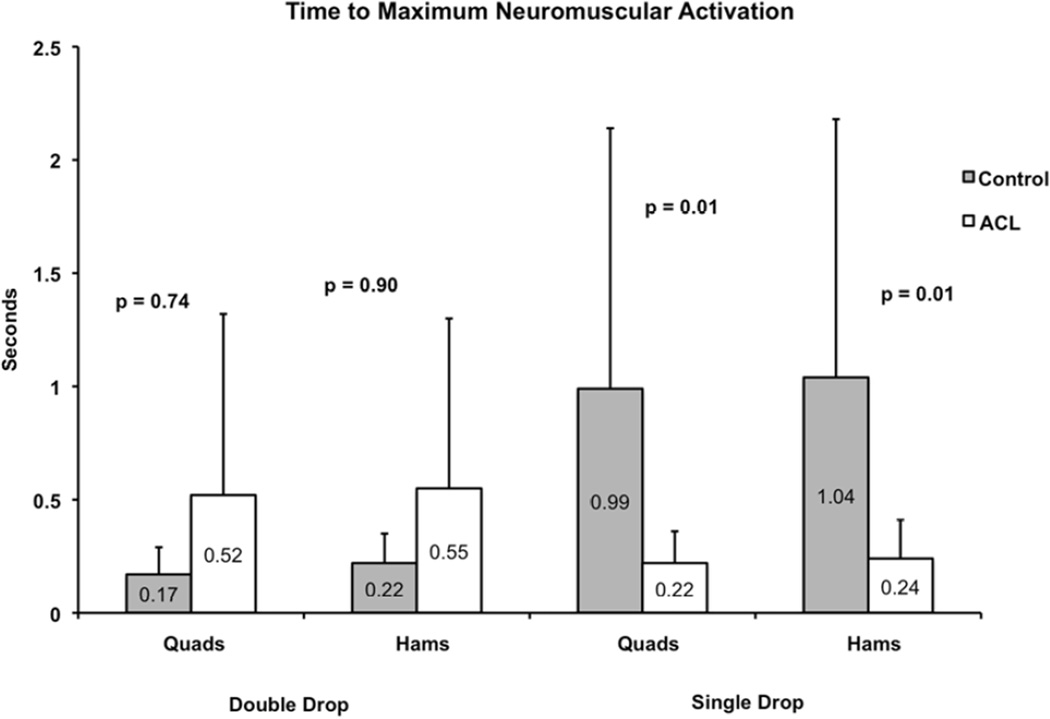
The adjusted means of the one-way ANCOVA (using weight and height as covariates) showed that women with SG-ACLr exhibited a non-statistically significant difference in dynamic valgus compared to the non-injured group (Fig. 3; F1, 26 = 3.50; p=0.07, effect size=0.12). One-way MANOVA adjusted means significant differences in EMG factors between groups (p<0.001). Post-hoc analyses showed lower quadriceps muscle activity (Fig. 4; F1, 28 = 7.81; p=0.01, effect size=0.22), and lower hamstring muscle activity (Fig. 4; F1, 28 = 6.08; p=0.02, effect size=0.18) for the SG-ACLr group compared to the control group. The co-contraction ratio results did not reach statistical significance, but showed a tendency to be reduced in the SG-ACLr group compared to the control group (Fig. 5). Latency analyses through Kruskal-Wallis revealed no differences between groups for quadriceps (p=0.74) and hamstring (p=0.91) muscle groups (Fig. 6).
Figure 3.
Adjusted means for dynamic knee valgus between groups per task. Although the group of women with SG-ACLr exhibited greater dynamic knee valgus, the results were not statistically significant.
Figure 4.
Adjusted means for rectified-normalized EMG MANOVAs were statistically significant during both tasks. Follow-up univariate analyses showed lower EMG activity for quadriceps and hamstrings muscle groups in the ACLr group during the double-legged drop jump. Conversely, the EMG activity of the quadriceps was greater in the SG-ACLr group during the single-legged drop jump.
Figure 5.
The SG-ACLr group exhibited lower co-contraction ratio between quadriceps and hamstrings. However, statistically significant differences were found only during the single legged drop jump.
Figure 6.
The group of women with SG-ACLr exhibited significantly less time to reach maximal activation of the quadriceps and hamstrings during the single-legged drop jump.
Single Leg Landing Countermovement Jump (SLJ)
One-way ANCOVA (weight and height as covariates) showed that women with SG-ACLr exhibited a tendency towards a greater dynamic knee valgus; however, this difference was not statistically significant (Fig. 3; F1, 24 = 2.60; p=0.12, effect size=0.60). The one-way MANOVA for EMG amplitude factors was statistically significant (p=0.02). The univariate post-hoc analysis revealed a statistically significant greater quadriceps muscle activity in the ACLr group compared to the control group (Fig. 4; F1, 28 = 5.60; p=0.03, effect size=0.17). Hamstring muscle activity (Fig. 4; F1, 28 = 0.30; p=0.60, effect size=0.01) did not reach significance, but showed a tendency to be increased in the SG-ACLr groups compared to the control group. Also, the SG-ACLr group exhibited a significantly lower co-contraction ratio (Fig. 5; F1, 28 = 5.77; p=0.02, effect size=0.17) compared to the control group. In terms of latency, the Kruskal-Wallis revealed that women with SG-ACLr exhibited significantly faster time-to-peak muscle activation than non- injured women for both quadriceps (p=0.01) and hamstring (p=0.01) muscle groups (Fig. 6).
DISCUSSION
Results for kinematic outcomes on this study suggest that women with SG-ACLr exhibit altered dynamic knee valgus during the double- (control: 4.18cm; ACL: 6.24cm) and single-legged (control: 1.99cm; ACL: 3.07cm) drop jumps when compared to non-injured individuals. These changes did not reach statistical significance due to lack of statistical power, yet, the effect size detected warrants consideration. Neuromuscular recruitment results supported in part our hypothesis showing significantly different neuromuscular recruitment strategies for landing stability, as compared to non-injured women. More specifically, during the double-legged drop jumps (DLJ), SG-ACLr participants showed: 1) lower quadriceps (control: 16.87%; ACL: 11.9%) and hamstring (control: 9.93%; ACL: 6.16%) muscle activity. Conversely, results of the single-legged drop jump (SLJ) showed: 1) greater quadriceps muscle activity (control: 9.51%; ACL: 12.96%), 2) lower co-contraction ratio (control: 0.66; ACL: 0.50), and 3) lower latency for both quadriceps (control: 0.99s; ACL: 0.22s), and hamstring (control: 1.04s; ACL: 0.24s) muscles in the ACLr group, when compared to the control group. In general, these results suggest different injury-predisposing neuromuscular recruitment strategies when higher levels of performance of the reconstructed knee are required.
Neuromuscular control is the ability to produce and modulate forces facilitating performance of any activity [5]. Hence, some individuals with complete ACL tear are able to dynamically stabilize their knee, even during high impact activities [1]. This indicates that the neuromuscular system response dictates dynamic knee stability in the absence of ligamentous support [1,32]. On the contrary, there are some individuals lacking dynamic knee stability after an ACL rupture and therefore, are advised to undergo ligament reconstruction [1]. Additionally, women with ligamentous injuries exhibit strength deficiencies and timing delays when compared to non-injured individuals [17]. Impact forces at the knee without adequate neuromuscular control will potentially provide less opportunity to accommodate muscle contractions and attenuate forces [19], consequently leading to further knee injuries [2,12]. Our EMG findings during both drop jumps are, to some extent, congruent with the aforementioned reports.
The results for the DLJ agreed with our hypothesis and showed that participants with SG-ACLr exhibited lower quadriceps and hamstring EMG amplitudes, but no significant differences in terms of co-contraction and latency, when compared to women without surgery. We propose that these results represent a neuromuscular control deficit that prohibits the generation of required forces for adequate knee stability. As seen in the co-contraction ratio, this difference was not statistically significant between groups (control: 0.58; ACLr: 0.50), giving the impression that participants with ACLr have similar anterior-posterior knee stability when compared to the control group. However, both normalized EMG values within the co-contraction formula in the ACLr group (quadriceps: 11.9%; hams: 6.16%) were significantly lower when compared to the control group (quadriceps: 17%; hamstrings: 10%). This implies a false impression of knee joint stability as such muscle activities might not protect against injury due to the inability of the quadriceps and hamstrings to tolerate large loads. The tendency of a slight increase in the dynamic knee valgus observed in individuals with SG-ACLr corroborates the concept of decreased dynamic knee stability. However, the nature of the task (DLJ) allows individuals to use a variety of landing strategies; including an increased use of the non-reconstructed lower extremity to control landing. Therefore, the obtained results may not represent the neuromuscular strategies used during high-level impact activities in the extremity with the ACLr. Although, the obtained results for the SLJ may provide clearer results towards dynamic knee stability during landing in these individuals. The magnitude of the effect size (0.60) may indicate clinical significance, although the differences in dynamic valgus between the ACL and control groups during the SLJ were not statistically significant. Therefore, although women with SG-ACLr exhibit greater dynamic knee valgus that could predispose them to re-injury, a greater sample size would be needed to reach such a conclusion.
Results from the single-legged drop jumps supported in part our hypothesis showing evidence of lower co-contraction ratio that could predispose women with SG-ACLr to further injury. On the other hand, the SG-ACLr group presented significantly greater quadriceps muscle activity and less time to reach maximum activation in comparison to the control group contradicting our initial hypothesis. These findings differ from a previous investigation in which women demonstrated an increased quadriceps/hamstrings latency period (time delays) and decreased quadriceps/hamstrings muscle activation [17]. We hypothesize that results of the SLJ are evidence of compensatory mechanisms in which lower activation time allows muscle forces to be generated at the appropriate time, in order to be successful at the required task. Bryant et al. (2007) showed that patients with ACL reconstruction with semitendinosus-gracilis graft, who were successful in reaching high levels of function, exhibited earlier hamstring and quadriceps muscle activity prior to initial contact during single-legged hops when compared to matched non-injured patients [33]. They hypothesized that this early muscle activation is part of a compensatory feed-forward mechanism, with the purpose of increasing joint compression to prevent instability during the landing phase of a jump. However, the increased quadriceps activation without hamstring muscle counteraction could predispose the individual to further injuries by promoting anterior translation of the tibia [34,35]. If the hamstrings do not offset with sufficient force the counter force generated by the quadriceps, the ACL might not be able to prevent, by itself, anterior tibial translation. A hamstring/quadriceps co-contraction ratio lower than 60% can be indicative of neuromuscular deficiencies that may predispose athletes to ACL injury [34]. In this study, the co-contraction ratio results supported our hypothesis that SG-ACLr patients would exhibit a greater injury-predisposing neuromuscular profile during the SLJ. The SG-ACLr group co-contraction ratio was 50%, showing a higher probability of injuries in this population. More research in this area is needed to elucidate neuromuscular mechanisms developed by these patients after ACL reconstruction.
The double-legged dynamic knee valgus values observed in our investigation (DLJ: control: 4.17 cm; ACL: 6.24 cm; p = 0.07.) were similar to values previously reported by other investigators [36,37] who evaluated knee injury predisposition, finding greater risk for knee injury in women when compared to their male counterparts. Previous investigators have reported that double-legged landing dynamic knee valgus measures of 4.15 cm [37] and 5 cm [36] predispose females to injuries when compared to their male counterparts. Therefore, we hypothesize that both groups exhibited landing mechanics that may predispose them to knee injuries given that our dynamic knee valgus values during the double-legged drop jump were 4.17 ± 2.32 cm and 6.24 ± 3.71 cm for the control and SG-ACLr groups, respectively.
Limitations
Although the purpose of the valgus analysis in this study was more clinically oriented, it had its own inherent limitations. Our valgus measure assessed the displacement of the knees from the moment of initial contact to maximum valgus, and therefore, was highly affected by the landing alignment. Hence, participants already landing in valgus will have less available motion towards more valgus than those landing with minimal or no valgus. An additional possible limitation arises from the rehabilitation protocol. Even though rehabilitation programs were the same per orthopedic surgeon and all individuals were cleared to return to their regular activities after their rehabilitation protocol was completed, this variable might have had an effect on individual biomechanical responses. Rehabilitation programs are comprised of standard ACL interventions such as inflammation management, range of motion, progression towards neuromuscular reeducation, and strengthening interventions. Individuals with ACLr who perform neuromuscular training as part of their rehabilitation protocol develop reactive muscle activation strategies that may protect the knee joint from excessive loads [17]. Future studies should examine the correlation between rehabilitation protocols and neuromuscular strategies presented during high impact landing activities, as well as the type of ACL reconstruction. Our study included women who had undergone SG-ACLr 12-months to 5 years. Alterations in muscular performance and level of physical activity change according to time of injury and thus, might have an effect on functional parameters and performance of various tasks [21,38]. Therefore, future studies should include a larger sample size and limit the range of time after surgery to control for this potential bias. Finally, the lack of matching individuals for dominant limb and only assessing biomechanics in one leg in both groups could have left out possible valuable information that may have helped further explain the differences found.
CONCLUSIONS
Individuals who have undergone ACLr have shown impaired muscle activity and timing adaptations. These neuromuscular deficits might affect dynamic knee stability, and consequently affect performance of high-impact sporting activities. Dynamic knee valgus has been proposed as a measure for knee stability during dynamic tasks. In the current study, we observed that individuals who had undergone ACLr presented appropriate dynamic knee valgus, although neuromuscular deficits were also observed. These neuromuscular deficits may predispose them to re-injury. Moreover, neuromuscular deficits are more noticeable when increased use of the reconstructed knee is required, as would be required during single-legged high-demand activities. Therefore, neuromuscular assessments after ACLr should include tests that are more sensitive for neuromuscular control during sporting activities. Consequently, neuromuscular assessments may have the potential to help guide the rehabilitation and/or training programs of these individuals by determining the specific deficits that require attention, in order to return to sporting activities, and reduce the risk of re-injury.
ACKNOWLEDGEMENTS
This project was funded by 8U54MD007587–03, NCRR-NIH U54RR026139–01, G12RR003051, and the National Strength & Conditioning Association Foundation. We would like to acknowledge Luis Rivas, Elena Roman, and Gloria Colon for their work as research assistants on this project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Moksnes H, Snyder-Mackler L, Risberg MA. Individuals with an anterior cruciate ligament-deficient knee classified as noncopers may be candidates for nonsurgical rehabilitation. J Orthop Sports Phys Ther. 2008 Oct;38(10):586–595. doi: 10.2519/jospt.2008.2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudroff T. Functional capability is enhanced with semitendinosus than patellar tendon ACL repair. Med Sci Sports Exerc. 2003 Sep;35(9):1486–1492. doi: 10.1249/01.MSS.0000084425.07852.7D. [DOI] [PubMed] [Google Scholar]
- 3.Hospodar SJ, Miller MD. Controversies in ACL reconstruction: bone-patellar tendon-bone anterior cruciate ligament reconstruction remains the gold standard. Sports Med Arthrosc. 2009 Dec;17(4):242–246. doi: 10.1097/JSA.0b013e3181c14841. [DOI] [PubMed] [Google Scholar]
- 4.Aune AK, Holm I, Risberg MA, Jensen HK, Steen H. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction A randomized study with two-year follow-up. Am J Sports Med. 2001 Nov-Dec;29(6):722–728. doi: 10.1177/03635465010290060901. [DOI] [PubMed] [Google Scholar]
- 5.Williams GN, Snyder-Mackler L, Barrance PJ, Axe MJ, Buchanan TS. Neuromuscular function after anterior cruciate ligament reconstruction with autologous semitendinosus-gracilis graft. J Electromyogr Kinesiol. 2005 Apr;15(2):170–180. doi: 10.1016/j.jelekin.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Ortiz A, Olson S, Libby CL, et al. Landing mechanics between noninjured women and women with anterior cruciate ligament reconstruction during 2 jump tasks. Am J Sports Med. 2008 Jan;36(1):149–157. doi: 10.1177/0363546507307758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ortiz A, Olson S, Trudelle-Jackson E, Rosario M, Venegas HL. Landing mechanics during side hopping and crossover hopping maneuvers in noninjured women and women with anterior cruciate ligament reconstruction. PM R. 2011 Jan;3(1):13–20. doi: 10.1016/j.pmrj.2010.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grindstaff TL, Jackson KR, Garrison JC, Diduch DR, Ingersoll CD. Decreased quadriceps activation measured hours prior to a noncontact anterior cruciate ligament tear. J Orthop Sports Phys Ther. 2008 Aug;38(8):508–516. doi: 10.2519/jospt.2008.2761. [DOI] [PubMed] [Google Scholar]
- 9.Mizner RL, Kawaguchi JK, Chmielewski TL. Muscle strength in the lower extremity does not predict postinstruction improvements in the landing patterns of female athletes. J Orthop Sports Phys Ther. 2008 Jun;38(6):353–361. doi: 10.2519/jospt.2008.2726. [DOI] [PubMed] [Google Scholar]
- 10.Earl JE, Monteiro SK, Snyder KR. Differences in lower extremity kinematics between a bilateral drop-vertical jump and a single-leg step-down. J Orthop Sports Phys Ther. 2007 May;37(5):245–252. doi: 10.2519/jospt.2007.2202. [DOI] [PubMed] [Google Scholar]
- 11.Fitzgerald GK, Lephart SM, Hwang JH, Wainner RS. Hop tests as predictors of dynamic knee stability. J Orthop Sports Phys Ther. 2001 Oct;31(10):588–597. doi: 10.2519/jospt.2001.31.10.588. [DOI] [PubMed] [Google Scholar]
- 12.Huston LJ, Vibert B, Ashton-Miller JA, Wojtys EM. Gender differences in knee angle when landing from a drop-jump. Am J Knee Surg. 2001 Fall;14(4):215–219. discussion 219–220. [PubMed] [Google Scholar]
- 13.Williams GN, Chmielewski T, Rudolph K, Buchanan TS, Snyder-Mackler L. Dynamic knee stability: current theory and implications for clinicians and scientists. J Orthop Sports Phys Ther. 2001 Oct;31(10):546–566. doi: 10.2519/jospt.2001.31.10.546. [DOI] [PubMed] [Google Scholar]
- 14.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003 Nov;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- 15.Zazulak BT, Ponce PL, Straub SJ, Medvecky MJ, Avedisian L, Hewett TE. Gender comparison of hip muscle activity during single-leg landing. J Orthop Sports Phys Ther. 2005 May;35(5):292–299. doi: 10.2519/jospt.2005.35.5.292. [DOI] [PubMed] [Google Scholar]
- 16.Huston LJ, Greenfield ML, Wojtys EM. Anterior cruciate ligament injuries in the female athlete. Potential risk factors. Clin Orthop Relat Res. 2000 Mar;(372):50–63. doi: 10.1097/00003086-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Hewett TE, Zazulak BT, Myer GD, Ford KR. A review of electromyographic activation levels, timing differences, and increased anterior cruciate ligament injury incidence in female athletes. Br J Sports Med. 2005 Jun;39(6):347–350. doi: 10.1136/bjsm.2005.018572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Decker MJ, Torry MR, Noonan TJ, Riviere A, Sterett WI. Landing adaptations after ACL reconstruction. Med Sci Sports Exerc. 2002 Sep;34(9):1408–1413. doi: 10.1097/00005768-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Lephart SM, Ferris CM, Riemann BL, Myers JB, Fu FH. Gender differences in strength and lower extremity kinematics during landing. Clin Orthop Relat Res. 2002 Aug;(401):162–169. doi: 10.1097/00003086-200208000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Vairo GL, Myers JB, Sell TC, Fu FH, Harner CD, Lephart SM. Neuromuscular and biomechanical landing performance subsequent to ipsilateral semitendinosus and gracilis autograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008 Jan;16(1):2–14. doi: 10.1007/s00167-007-0427-4. [DOI] [PubMed] [Google Scholar]
- 21.Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med. 2005 Sep;33(9):1337–1345. doi: 10.1177/0363546504274145. [DOI] [PubMed] [Google Scholar]
- 22.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001 Mar-Apr;29(2):213–218. doi: 10.1177/03635465010290021601. [DOI] [PubMed] [Google Scholar]
- 23.van der Harst JJ, Gokeler A, Hof AL. Leg kinematics kinetics in landing from a single-leg hop for distance A comparison between dominant and non-dominant leg. Clin Biomech (Bristol, Avon) 2007 Jul;22(6):674–680. doi: 10.1016/j.clinbiomech.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 24.Ford KR, Myer GD, Smith RL, Byrnes RN, Dopirak SE, Hewett TE. Use of an overhead goal alters vertical jump performance and biomechanics. J Strength Cond Res. 2005 May;19(2):394–399. doi: 10.1519/15834.1. [DOI] [PubMed] [Google Scholar]
- 25.Besier TF, Lloyd DG, Ackland TR. Muscle activation strategies at the knee during running and cutting maneuvers. Med Sci Sports Exerc. 2003 Jan;35(1):119–127. doi: 10.1097/00005768-200301000-00019. [DOI] [PubMed] [Google Scholar]
- 26.Croce RV, Russell PJ, Swartz EE, Decoster LC. Knee muscular response strategies differ by developmental level but not gender during jump landing. Electromyogr Clin Neurophysiol. 2004 Sep;44(6):339–348. [PubMed] [Google Scholar]
- 27.Soderberg GL, Knutson LM. A guide for use and interpretation of kinesiologic electromyographic data. Phys Ther. 2000 May;80(5):485–498. [PubMed] [Google Scholar]
- 28.Lloyd DG, Buchanan TS. Strategies of muscular support of varus and valgus isometric loads at the human knee. J Biomech. 2001 Oct;34(10):1257–1267. doi: 10.1016/s0021-9290(01)00095-1. [DOI] [PubMed] [Google Scholar]
- 29.Kang HG, Dingwell JB. Intra-session reliability of local dynamic stability of walking. Gait & posture. 2006 Nov;24(3):386–390. doi: 10.1016/j.gaitpost.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 30.Ballal MS, Khan Y, Hastie G, Hatcher A, Coogan S, McNicholas MJ. Functional outcome of primary hamstring anterior cruciate ligament reconstruction in patients with different body mass index classes. Arthroscopy. 2013 Aug;29(8):1314–1321. doi: 10.1016/j.arthro.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 31.Portney LG, Watkins MP. Foundations of clinical research : applications to practice. 3rd ed. Upper Saddle River, N.J: Pearson/Prentice Hall; 2009. [Google Scholar]
- 32.Hurd WJ, Axe MJ, Snyder-Mackler L. Influence of age, gender, and injury mechanism on the development of dynamic knee stability after acute ACL rupture. J Orthop Sports Phys Ther. 2008 Feb;38(2):36–41. doi: 10.2519/jospt.2008.2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bryant AL, Newton RU, Steele J. Successful feed-forward strategies following ACL injury and reconstruction. J Electromyogr Kinesiol. 2009 Oct;19(5):988–997. doi: 10.1016/j.jelekin.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 34.Hewett TE. Neuromuscular hormonal factors associated with knee injuries in female athletes Strategies for intervention. Sports Med. 2000 May;29(5):313–327. doi: 10.2165/00007256-200029050-00003. [DOI] [PubMed] [Google Scholar]
- 35.Swanik CB, Lephart SM, Giraldo JL, Demont RG, Fu FH. Reactive muscle firing of anterior cruciate ligament-injured females during functional activities. J Athl Train. 1999 Apr;34(2):121–129. [PMC free article] [PubMed] [Google Scholar]
- 36.Noyes FR, Barber-Westin SD, Fleckenstein C, Walsh C, West J. The drop-jump screening test: difference in lower limb control by gender and effect of neuromuscular training in female athletes. Am J Sports Med. 2005 Feb;33(2):197–207. doi: 10.1177/0363546504266484. [DOI] [PubMed] [Google Scholar]
- 37.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med. 2010 Oct;38(10):2025–2033. doi: 10.1177/0363546510370933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Risberg MA, Holm I, Myklebust G, Engebretsen L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007 Jun;87(6):737–750. doi: 10.2522/ptj.20060041. [DOI] [PubMed] [Google Scholar]