Abstract
Objective
The purpose of this study is to assess regional parental barriers in the diagnostic and therapeutic process following abnormal newborn hearing screening (NHS) testing.
Study Design
Cross-sectional questionnaire study
Setting
Tertiary medical center
Patients
Parents of infants who failed NHS in Kentucky from January 2009 – February 2012
Main Outcome Measure
Demographic information, county of origin, and attitudes and perceptions regarding NHS and barriers in the NHS diagnostic process.
Results
There were 460 participants in the study, which included25.4% of parents were from the Appalachian region. 21% of Appalachian parents found the process on newborn hearing testing difficult. Appalachian parents were more likely to have no more than 12 years of education (OR 1.7, p=0.02) and Medicaid insurance (OR 2.3, p<0.001) compared with non-Appalachian parents. A higher percentage of Appalachian parents were unaware of the NHS results at the time of hospital discharge than non-Appalachians (14% v. 7%, p=0.03). Distance from the diagnostic/therapeutic center represented was a significant barrier for Appalachian parents (OR 2.8, p=0.001). Compared with urban parents, a greater percentage of rural parents had never heard of a cochlear implant (p=0.01). Appalachian parents expressed a strong interest in telemedicine and a desire for closer services.
Conclusion
Multiple barriers including education, distance, accessibility, socioeconomic factors can affect timely diagnosis and treatment of congenital hearing loss for children residing in rural areas. Educational and telemedicine programs may benefit parents in Appalachia, as well as parents in other rural areas.
Keywords: Infant hearing loss, Rural healthcare, Barriers to healthcare access, Appalachia
INTRODUCTION
Pediatric hearing loss is a common neonatal sensory disorder in the United States and represents a significant public health concern.1 The United States Preventive Services Task Force has recognized the significant effect that congenital hearing loss has on communication skills, psychosocial development, and educational progress and have found that early detection of hearing loss improves language development.2 Early identification of hearing loss leads to early treatment.3,4 Unfortunately, many infants fail to obtain or are delayed in receiving this diagnostic testing and intervention after abnormal infant screening at birth.
There are multiple steps in the diagnostic and therapeutic process for children with hearing loss. Several factors may affect the timing of the steps such as education, distance, accessibility and socioeconomic factors. The presence of disparities in diagnostic and intervention services result in some socioeconomic groups being at a high risk of becoming lost to follow-up.5–7 Patients in rural areas face limited access to care that compounds these concerns and are at risk for delayed diagnosis of hearing loss and necessary treatment.8 Appalachia is a largely rural region recognized nationally as suffering from extreme health disparities and is underserved in healthcare services.9,10 Children from this region with hearing loss are delayed in diagnosis and intervention.11,12 The purpose of this study was to investigate Appalachian and non-Appalachian parental attitudes, experiences and perceived barriers regarding newborn hearing screening (NHS)and the subsequent diagnostic and treatment process.
METHODS
The internal review boards of the University of Kentucky (protocol 11-0872-P3H) and the Kentucky Cabinet for Health and Family Services (protocol CHFS-IRB-CCSHCN-FY12-49) approved the study. Inclusion criteria included the parents/guardians of children that failed NHS in Kentucky from January 2009 through February 2012 from a database provided by the Cabinet for Health and Family Services and the Early Hearing Detection and Intervention (EHDI) system. This included names and last known addresses of these children. A 48-item questionnaire was developed to assess demographics, parental knowledge of NHS results and of general hearing healthcare, and attitudes regarding NHS and barriers in diagnostic and therapeutic steps following NHS. The multidisciplinary research team carefully developed this questionnaire with input from literature review, parents, and providers. The questionnaire was piloted with several parents prior to wide circulation and then modified to ensure clarity and ease of completion.
Question formats included fill in the blank, open-ended semi-structured questions, multiple choice, yes/no, and 4-pointgraded scale questions. The first several questions revolved around demographic information, including parent and child gender and age, parent education level, and type of insurance. The next set of questions asked whether they knew that their child had been screened, if they knew the results, and what they were told about the screening overall. Next, the parents were asked about their child’s actual diagnosis, including difficulties faced during the process. The questionnaire included inquiries about problems preventing follow up such as distance to the clinic, type of health insurance used, and family and physician attitudes. The parents were also asked about the hearing treatment their child received, including the age of the child when he or she received hearing aids, their attitudes about the timing of the treatment, as well as any clinical services utilized. A general knowledge question was included, which asked parents if they had ever heard of a cochlear implant. Parents’ willingness and desire to utilize a closer hearing healthcare center and telemedicine services was assessed. The final set of questions assessed parental attitudes regarding hearing loss overall, the importance of hearing for school and social performance, and the usefulness of early intervention services.
Based on the home address and county of residence, we determined the Appalachian residence status of participants prior to mailing based on Appalachian Regional Commission classification13 and Appalachian recipients received questionnaires printed on different color paper. This assisted with data analysis of returned questionnaires. Each mailing included an addressed stamped return envelope. A total of 5529 parents of eligible children were identified and mailed a questionnaire. Based on the reported county of residence on the returned questionnaires, we also determined rurality of the participant’s county using the US Department of Agriculture Rural-Urban Continuum coding system.14 This system utilizes a 9-point scale of Beale codes and code 1–3 were considered urban and 4–9 were considered rural.15 The lower the numerical designation, the more metropolitan the county. For instance, a Beale code of 1 indicates a population of 1 million or more. In contrast, a Beale code of 9 is defined as a very rural county with a population less than 2500 that is not adjacent to a metro area.
Returned questionnaires were analyzed by coding each item separately. Continuous variables were summarized by calculating means and categorical variables were described with counts and percentages. Multiple choice and graded-scale question answer frequencies were calculated. Data was managed using an Excel spreadsheet (Microsoft, Redmond, WA, USA), and statistical analysis was performed with Stata (StataCorp, College Station, TX, USA).A p-value < 0.05 was considered statistically significant. Associations between measured variables were assessed using chi square tests for dichotomous variables and ANOVA/Mann-Whitney U test for continuous variables (depending on distribution normality).
RESULTS
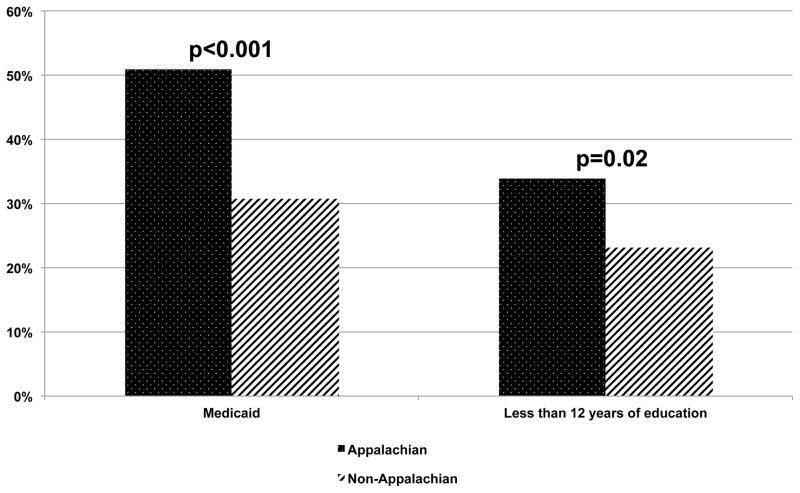
A summary of questionnaire response rates and demographic data is found in Table 1. Of the 5,529 questionnaires mailed to parents/guardians of children who failed newborn hearing screening, 460 surveys were returned (8.32% response rate) with 343 from non-Appalachians and 117 from Appalachians. Parents of children who failed infant hearing screening in 2009 had the lowest response rate (7.22%) and the response rate progressively increased in those from 2010 (7.58%) and those in 2011/12 (9.93%).There were significant differences in educational background and insurance status between Appalachian parents and non-Appalachian parents (Figure 1). A higher percentage of Appalachian parents had no more than 12 years of education (OR 1.7, p=0.02) than non-Appalachian parents. The question regarding insurance coverage revealed that approximately 51% of Appalachian parents reported Medicaid insurance coverage compared with 31% of non-Appalachian parents (OR 2.3, p<0.001). Related to those same figures, a higher percentage of non-Appalachian parents (62%)reported private insurance than the Appalachian parents (46.6%)(p=0.004).
TABLE 1.
Demographic Responses of Returned Surveys
| Appalachian | Non-Appalachian | Overall | |
|---|---|---|---|
| Total Surveys Sent | 1493 | 4036 | 5529 |
| Number of Returned Surveys | 117 | 343 | 460 |
| Percentage of Returned Surveys | 7.84 | 8.50 | 8.32 |
| Percentage of Returned Surveys from Rural County | 88.60 | 28.30 | 43.64 |
| Percentage of Returned Surveys from Urban County | 11.40 | 71.70 | 56.36 |
| Average Parent/Guardian Age (years) | 30.77 | 31.16 | 31.06 |
| Number (Percentage) of Female Parent/Guardian Responding | 109 (93.97%) | 319 (93.27%) | 428 (93.45%) |
| Number (Percentage) of Male Parent/Guardian Responding | 8 (6.03%) | 24 (6.73%) | 32 (6.55%) |
| Number (Percentage) of Female Children | 51 (43.59%) | 147 (42.98%) | 198 (43.14%) |
| Number (Percentage) of Male Children | 66 (56.41%) | 195 (57.02%) | 262 (56.86%) |
| Number (Percentage) of Reported Children with Hearing Loss Diagnosis | 16 (13.68%) | 44 (12.83%) | 60 (13.04%) |
| Number (Percentage)of Reported Children with Normal Hearing | 93 (79.49%) | 291 (84.84%) | 384 (83.45%) |
| Number (Percentage) of Reported Children with Unknown Hearing Status | 8 (6.84%) | 8 (2.33%) | 16 (3.48%) |
Figure 1.
Percentage of Parents with Medicaid insurance and Maximal level of education of parents.
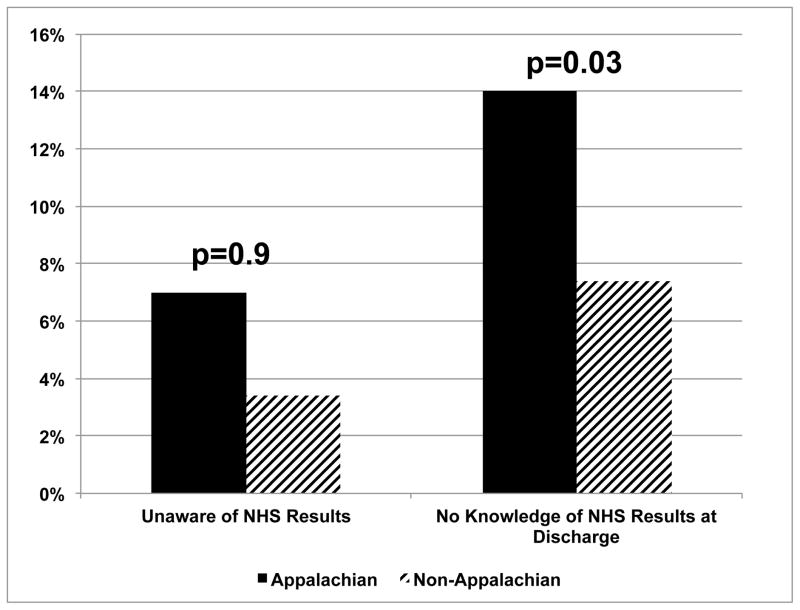
Questions regarding parental experiences with the NHS and follow-up process revealed valuable information. A total of 69 parents (15%) reported that their children were diagnosed with hearing loss as a result of the diagnostic process. 52.6% of Appalachian parents reported that their children were diagnosed after 3 months of age compared with 42% of non-Appalachian parents (p=0.4) and the parental reported average age of diagnosis of hearing loss for Appalachian children was 9.4 months after birth and 6.3 months after birth in non-Appalachian children (p=0.065). There is evidence of communication breakdown of the NHS results (Figure 2) with 7% of Appalachian parents never aware of the NHS results. A higher percentage of Appalachian parents (14%) were unaware of the NHS results at the time of hospital discharge compared with non-Appalachian parents (7%) (p=0.03).
Figure 2.
Percentage of parents who were never told at any time the results of their child’s newborn hearing screening test and the percentage who were unaware of the results by the time of hospital discharge.
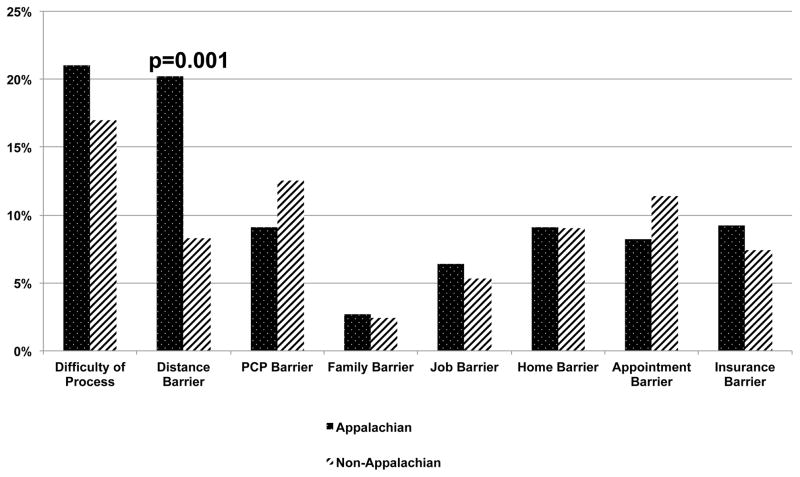
The difficulty of the diagnostic process and barriers to timely care after NHS was assessed (Figure 3). 18% of all parents and 33% of those parents with children with hearing loss reported the process of NHS and ensuing testing to be difficult to very difficult. Distance made the process difficult for 20% of Appalachian parents compared with 8.3% of non-Appalachian parents (OR 2.8, p=0.001). Other parental barriers to obtain follow-up testing reported by participants included lack of primary care doctor support for follow testing (11.6%), lack of family support (2.4%), conflicting job responsibilities (5.6%), conflicting home responsibilities (9%), problems with obtaining an appointment (10.5%), and insurance coverage problems (7.8%). There was no statistically significant difference in these reported barriers between Appalachian and non-Appalachian parents. Of the parents of children diagnosed with hearing loss, 11.6% felt that their child received hearing aids later than they desired. The reasons for the delay in amplification in those reporting this were not specified.
Figure 3.
Percentage of parents who reported that these barriers played a significant role in complicating the process for their child to have hearing testing after NHS.
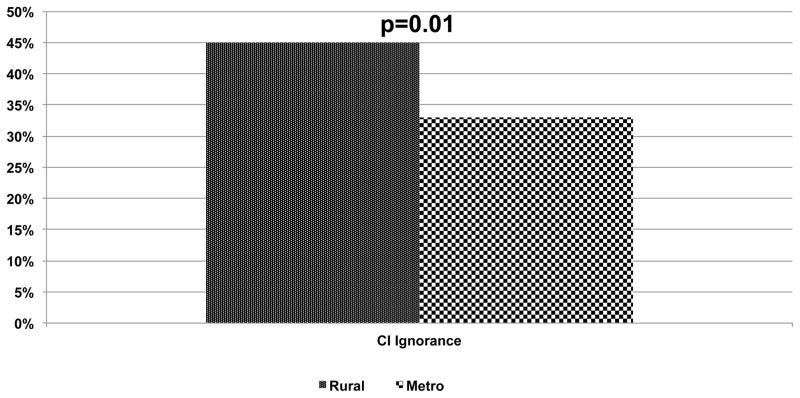
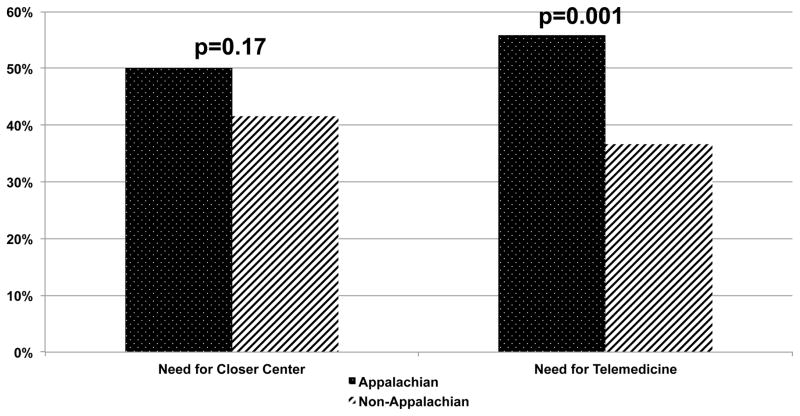
Questions addressing perceptions regarding hearing loss and access to diagnostic/therapeutic services demonstrated differences between Appalachian and non-Appalachian parents. 92% of non-Appalachian parents felt follow-up after failed NHS was very important for school performance and social relationships compared with 86% of Appalachians (p=0.046). 5% of Appalachians believed nothing could be done to treat infant hearing loss compared with 1% of non-Appalachians (p=0.047). Comparing rural county residents (both in Appalachian and non-Appalachian regions of Kentucky) with those in urban counties, 45.4% of rural participants had never heard of a cochlear implant while 33.8% of urban residence had knowledge of implants (p=0.01) (Figure 4). Both telemedicine and closer healthcare facilities were proposed as possible ways to make the follow-up diagnostic and treatment process less burdensome for parents(Figure 5). Additionally, 50.0% of Appalachian parents thought closer healthcare facilities would help while 41.5%of non-Appalachian parents reported the same(p=0.168). Appalachians expressed interest in telemedicine access to care with55.8% indicating that it was likely that they would utilize telemedicine services if the option were available compared with only 36.7%of non-Appalachians (p=0.001) (Figure 5).
Figure 4.
Percentage of parents who have heard of cochlear implants before.
Figure 5.
Percentage of parents who report a desire for a closer hearing center for children and a desire to seek hearing health care through telemedicine.
DISCUSSION
Appalachia is a rural region of the United States spanning twelve states and encompassing 205,000 square miles.16 Not unlike many rural regions, the residents of Appalachia have experienced a long history of hardship and poverty, and while significant economic and societal improvements have been made in the last several decades, many disparities still exist. In order to fully appreciate the specific population addressed in this study, it is important to compare the two regions. Compared with the non-Appalachian region of Kentucky, residents of Appalachian Kentucky are more likely to have less than a high school diploma (20.9% vs. 11.1%), be unemployed (9.0% vs. 7.5%), be in poverty (25.1% vs. 16.1%), and not be covered by health insurance (17.0% vs. 13.1%).17 From 2008 to 2012, the mean household income in Appalachian Kentucky was significantly lower than that in non-Appalachian Kentucky ($45,516 vs. $62,422), as was the mean family income ($53,845 vs. $74,198).17 Although to a lesser extent, these disparities hold true when comparing Appalachia as a whole to the entire United States. The high density of rural counties within Appalachian Kentucky is what makes this region somewhat unique; however, its uniqueness in that respect does not preclude the comparison of Appalachia with other rural areas around the country.
This pilot study represents an initial investigation of the factors involved in rural pediatric hearing healthcare disparity by assessing parental knowledge, attitudes and experiences in NHS and subsequent diagnostic and therapeutic steps. Certainly health disparity is multifactorial by nature; however, understanding parental perspectives in barriers to care is important, albeit difficult, to assess. Providing easy and timely access to care for rural residents is a significant public health concern as 20% of the US population lives in rural regions.18 In this study, Appalachian parents raised concern for lack of awareness of NHS results and found that distance to testing/treatment centers to be a significant barrier in newborn hearing healthcare. This study identified educational and insurance differences in rural parents living in Appalachia compared with non-Appalachian parents. Many rural parents were unaware of definitive treatment options available for children with hearing loss. Strong interest was expressed among participants in improving access to care through development of closer hearing centers and Appalachians desired to access care through telemedicine. This study does not fully assess all potential barriers or determine direct causation for delayed access to care; however, this study represents the first of its kind to frame some of the barriers encountered in pediatric hearing healthcare for those from rural regions and further investigation is needed to more clearly identify the most critical and influential factors that delay infant hearing loss rehabilitation in regions of health inequity.
Many rural patients, such as those from Appalachia, experience poorer health.19 When adjusting for demographic, ethnic, and socioeconomic factors, rural children are at greater risk of unmet medical needs compared with urban children.20 Appalachian healthcare services are sparse and underdeveloped transportation infrastructure can complicate access to care.19 Distance from hearing centers has been directly correlated to the timing of hearing healthcare services.8,11,12 There is significantly increased risk of non-adherence to the hearing testing recommendations among children whose mothers have low levels of education.21,22 Children are at a higher risk of being non-adherent with recommended testing and delayed in treatment of hearing loss if their mothers have a low socioeconomic status and are covered by public insurance.23,24 Lester and colleagues25 reported that children with severe sensori neural hearing loss with Medicaid are at a 21% higher risk of being delayed in receiving a cochlear implant compared to those with private insurance. There is an obvious relationship between low socioeconomic status and the likelihood of being on public insurance. It is likely that there are multiple variables contributing to the complex reasons for delayed identification and treatment of children in these regions. Distinguishing the role each of these variables and their contribution to these health disparities is complex. Further research is needed to further define these factors. These regional healthcare, educational, socioeconomic, and insurance differences have the potential to affect the timely diagnosis of congenital hearing loss and further research should investigate this issue.
Many parents reported an interest in telemedicine to improve access to care. Telemedicine is the transmission of health-related services and information by means of telecommunication technology and has the potential to be a useful tool to deliver care for those rural and underserved areas. The use of telemedicine in hearing healthcare is relatively new and the applications include patient education and counseling, otoscopy, hearing aid fittings,26 audiometric testing,27,28 electrophysiological testing29 and potentially cochlear implant programming. The possible benefits are far reaching and apart from research, telehealth may improve health care access, quality of service delivery, effectiveness and efficiency of health care, and ameliorate the inequitable distribution of health professionals.29 Internet connectivity and technology is providing a bridge between patients and health care providers who may otherwise be separated by distance, location, geographical and weather barriers as well as economic barriers. This bridge may also improve access for isolated health care providers to resources like training, professional interaction and mentoring.
A questionnaire study such as this is limited by a low response rate. The participants were identified through the state EHDI system, which may have inaccurate address information and thus inherently limits the number of participants who actually receive the questionnaire and may participate. Additionally, written and electronic questionnaires may not be completed by those with low literacy. The responses were subjective in nature and relied on the parent’s recollection of their past experiences and may not fully assess the barriers. This could potentially account for why the response rate of those parents who went through the NHS process in 2009 was the lowest and those from 2011/12 were the highest. It is quite possible that these results may underestimate the barriers encountered by parents due to these facts. There are limited methods to learn parental experiences of a vast number of parents whose children fail NHS over a several year period. This method served as a meaningful tool to identify general themes among potential barriers to access of care as well as to provide direction with respect to decreasing this healthcare disparity. Further investigation, involving focus groups and individual interviews of parents in this context, with qualitative analysis, is appropriate to further delineate common barriers for timely care. Considering the regional distribution of this questionnaire, these results may not be generalized to all other regions, including other rural areas. Certainly, concerns of education, insurance coverage, health literacy, and socioeconomic inequity are common themes throughout health care disparity research and we hypothesize these factors may influence pediatric hearing healthcare in other rural regions as well.
CONCLUSION
Newborn hearing screening and subsequent diagnostic and therapeutic care is vital to expeditiously address congenital hearing loss. Parents in this process may encounter many barriers. Rural patients are often delayed in diagnosis of hearing loss and this may be related to multiple factors. Appalachian parents report distance significantly complicates timely pediatric hearing healthcare and those also may lack important knowledge about their child’s hearing and available treatment options. Important steps, such as family education and engagement, are essential in promoting timely hearing healthcare. It will also be important to consider alternative delivery treatment approaches such as telemedicine services in order to provide much needed support for rural children with hearing loss and their families.
Acknowledgments
Acknowledgements and Disclosures: This work was supported by University of Kentucky Center for Clinical and Translational Science and the National Institute of Health (8 KL2 TR000116-02) (MLB and CRS), National Institutes of Health Loan Repayment Program (MLB), and National Institute of Deafness and Other Communication Disorders (1U24-DC012079-01)(MLB).
Footnotes
Presented at American Otological Society, May 17, 2014, Las Vegas, NV
References
- 1.Centers for Disease Control and Prevention. National Center on Birth Defects and Developmental Disabilities. [Accessed 2/5/2014];Hearing loss. Available at: http://www.cdc.gov/ncbddd/hearingloss/data.html.
- 2.U.S. Preventive Services Task Force. Universal screening for hearing loss in newborns: U.S. Preventive Services Task Force Recommendation Statement. Pediatrics. 2008;122:143–148. doi: 10.1542/peds.2007-2210. [DOI] [PubMed] [Google Scholar]
- 3.Apuzzo ML, Yoshinaga-Itano C. Early identification of infants with significant hearing loss and the Minnesota Child Development Inventory. Semin Hear. 1995;16:124–137. [Google Scholar]
- 4.Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3):E43. doi: 10.1542/peds.106.3.e43. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Hearing Loss in Children. [Accessed 8/26/2013];Data and Statistics. http://www.cdc.gov/ncbddd/hearingloss/data.html.
- 6.Guadagnolo BA, Dohan D, Raich P. Metrics for evaluating patient navigation during cancer diagnosis and treatment: Crafting a policy-relevant research agenda for patient navigation in cancer care. Cancer. 2011;117(15 suppl):3565–3574. doi: 10.1002/cncr.26269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moy B, Chabner BA. Patient navigator programs, cancer disparities, and the patient protection and affordable care act. The Oncologist. 2011;16:926–929. doi: 10.1634/theoncologist.2011-0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bush M, Burton M, Loan A, Shinn J. Timing Discrepancies of Early Intervention Hearing Services in Urban and Rural Cochlear Implant Recipients. Otology & Neurotology. 2013;34(9):1630–5. doi: 10.1097/MAO.0b013e31829e83ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Portnoy B. Healthy People in Rural Areas by the Year 2000. In: Couto RA, Simpson NK, Harris G, editors. Sowing Seeds in the Mountains: Community Based Coalitions for Cancer Prevention and Control. Bethesda, MD: Appalachia Leadership Initiative on Cancer, DCPC, National Cancer Institute; 1994. (DHHS Pub. No. (NIH) 94-3779.) [Google Scholar]
- 10.Lengerich EJ, Wyatt SW, Rubio A, Beaulieu JE, et al. The Appalachia Cancer Network: cancer control research among a rural, medically underserved population. J Rural Health. 2004;20(2):181–7. doi: 10.1111/j.1748-0361.2004.tb00026.x. [DOI] [PubMed] [Google Scholar]
- 11.Bush M, Bianchi K, Lester C, Shinn J, Gal T, Fardo D, Schoenberg N. Delays in Diagnosis of Congenital Hearing Loss in Rural Children. J Pediatr. 2014;164:393–7. doi: 10.1016/j.jpeds.2013.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bush M, Osetinsky M, Shinn J, Gal T, Fardo D, Schoenberg N. An Expanding Gap: Addressing Rural Pediatric Hearing Healthcare Disparities and Delays. Laryngoscope. 2014 Jan 8; doi: 10.1002/lary.24588. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Appalachian Regional Commission. [Accessed 9/16/13];The Appalachian Region. http://www.arc.gov/appalachian_region/TheAppalachianRegion.asp.
- 14.Rural-Urban Continuum Codes. USDA Economic Research Service. United States Department of Agriculture; [Accessed 2/7/2014]. http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. [Google Scholar]
- 15.Davis AF. Kentucky’s Urban/Rural Landscape: What is driving the differences in wealth across Kentucky? [Accessed 2/22/2014];Kentucky Annual Economic Report. 2009 http://cber.uky.edu/Downloads/annrpt09.html.
- 16.The Appalachian Region. Appalachian Regional Commission; [Accessed 7/15/2014]. http://www.arc.gov/appalachian_region/TheAppalachianRegion.asp. [Google Scholar]
- 17.The Appalachian Region: A Data Overview from the 2008–2012 American Community Survey. Appalachian Regional Commission; [Accessed 7/15/2014]. http://www.arc.gov/research/researchreportdetails.asp?REPORT_ID=109. [Google Scholar]
- 18.Office of Planning, Environment & Realty. United States Department of Transportation Federal Highway Administration; [Accessed 2/12/2014]. Census 2000 Population Statistics. Available at: http://www.fhwa.dot.gov/planning/census_issues/archives/metropolitan_planning/cps2k.cfm. [Google Scholar]
- 19.Shell R, Tudiver F. Barriers to cancer screening by rural Appalachian primary care providers. J Rural Health. 2004;20:368–373. doi: 10.1111/j.1748-0361.2004.tb00051.x. [DOI] [PubMed] [Google Scholar]
- 20.DeVoe JE, Krois L, Stenger R. Do children in rural areas still have different access to health care? Results from a statewide survey of Oregon’s food stamp population. J Rural Health. 2009;25:1–7. doi: 10.1111/j.1748-0361.2009.00192.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cavalcanti HG, Guerra RO. The role of maternal socioeconomic factors in the commitment to universal newborn hearing screening in the Northeastern region of Brazil. Int J Pediatr Otorhinolaryngol. 2012;76(11):1661–7. doi: 10.1016/j.ijporl.2012.07.041. [DOI] [PubMed] [Google Scholar]
- 22.Holte L, Walker E, Oleson J, Spratford M, et al. Factors influencing follow-up to newborn hearing screening for infants who are hard of hearing. Am J Audiol. 2012;21(2):163–74. doi: 10.1044/1059-0889(2012/12-0016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu CL, Farrell J, MacNeil JR, Stone S, Barfield W. Evaluating Loss to Follow-up in Newborn Hearing Screening in Massachusetts. Pediatrics. 2008;21(2):e335–343. doi: 10.1542/peds.2006-3540. [DOI] [PubMed] [Google Scholar]
- 24.Armstrong M, Maresh A, Buxton C, Craun P, et al. Barriers to early pediatric cochlear implantation. Int J Pediatr Otorhinolaryngol. 2013;77(11):1869–72. doi: 10.1016/j.ijporl.2013.08.031. [DOI] [PubMed] [Google Scholar]
- 25.Lester EB, Dawson JD, Gantz BJ, Hansen MR. Barriers to the Early Cochlear Implantation of Deaf Children. Otol Neurotol. 2011;32:406–12. doi: 10.1097/MAO.0b013e3182040c22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krumm M. Audiology telemedicine. J Telemed Telecare. 2007;13:224–229. doi: 10.1258/135763307781458912. [DOI] [PubMed] [Google Scholar]
- 27.Givens G, Elangovan S. Internet application to tele-audiology: ‘Nothin’ but net.’. Am J Audiol. 2003;12:50–65. doi: 10.1044/1059-0889(2003/011). [DOI] [PubMed] [Google Scholar]
- 28.Krumm M, Huffman T, Dick K, Klich R. Telemedicine for audiology screening of infants. J Telemed Telecare. 2008;14:102–104. doi: 10.1258/jtt.2007.070612. [DOI] [PubMed] [Google Scholar]
- 29.Wootton R. The future use of telehealth in the developing world. In: Wootton R, Patil NG, Scott RE, Ho K, editors. Telehealth in the Developing World. London: Royal Society of Medicine Press Ltd; 2009. pp. 299–308. [Google Scholar]