Abstract
Objectives
To assess the association between market concentration of hospitals (as a proxy for competition) and patient-reported health gains after elective primary hip replacement surgery.
Methods
Patient Reported Outcome Measures data linked to NHS Hospital Episode Statistics in England in 2011/12 were used to analyse the association between market concentration of hospitals measured by the Herfindahl-Hirschman Index (HHI) and health gains for 337 hospitals.
Results
The association between market concentration and patient gain in health status measured by the change in Oxford Hip Score (OHS) after primary hip replacement surgery was not statistically significant at the 5% level both for the average patient and for those with more than average severity of hip disease (OHS worse than average). For 12,583 (49.1%) patients with an OHS before hip replacement surgery better than the mean, a one standard deviation increase in the HHI, equivalent to a reduction of about one hospital in the local market, was associated with a 0.104 decrease in patients’ self-reported improvement in OHS after surgery, but this was not statistically significant at the 5% level.
Conclusions
Hospital market concentration (as a proxy for competition) appears to have no significant influence (at the 5% level) on the outcome of elective primary hip replacement. The generalizability of this finding needs to be investigated.
Keywords: hip replacement surgery, hospital market concentration, patient reported outcome measures
Introduction
Health care reforms in England during the last decade have been influenced by the idea that encouraging competition between hospitals, with nationally fixed prices, will increase the quality of care for patients. However, the effect of competition on health care quality is controversial.1 It is not possible to measure competition directly. Research in health care and other sectors uses market concentration as a proxy for competition. Two empirical studies using national hospital administrative data from the National Health Service (NHS) in England suggested that the less the concentration of hospitals (more competition), the better the quality of care under a fixed price regime.2,3 Hospital quality, as measured by 30-day mortality after acute myocardial infarction (AMI), improved after the choice-based reforms were introduced in 2006 in less concentrated markets. However, in those studies,2–4 the methodology used has been challenged as have the assumptions.5 Bevan and Skellern also highlight the methodological challenges, arguing that ‘more research is required before conclusions can be drawn about the effect of recent reforms on hospital quality’.6
A principal criticism of existing empirical studies relates to the measure of quality of care7,8 which used AMI mortality rates as a proxy for overall hospital quality. Mortality rates will not capture small changes in patient health and ignore much hospital care which is directed at improving patients’ quality of life. Gravelle et al. examined the correlation between 16 hospital quality measures and their association with different measures of concentration.9 Their results suggest that the association between quality and concentration varies between measures and that correlations between different measures of quality within a hospital are weak. Furthermore, there are concerns about the adequacy of measurement of patients’ severity of illness before treatment in earlier studies and hence of the health gains achieved by treatment. Severity of a patient’s ill-health before treatment has typically been measured using proxies such as number of co-morbidities and of previous emergency admissions rather than directly. Use of such proxies raises concern about the accuracy of adjustments for severity.
A more direct way of assessing improvements in patients’ health, including quality of life, is now available for some treatments. Since April 2009, English NHS hospital trusts and independent sector providers treating NHS-funded patients have collected Patient Reported Outcome Measures (PROMs) data for four elective surgical procedures: hip replacement, knee replacement, varicose veins surgery and groin hernia surgery. A PROM is a set of questions that patients are asked about their views on their own health. Questionnaires are completed by patients shortly before, and 3 or 6 months after surgery. PROMs can be used to assess directly the quality of specific interventions. In addition, PROMs reported before an intervention indicate the severity of the patient’s ill-health.
In this study, we use the newly available PROMs data to examine the relationship between hospital market concentration and changes in patients’ self-reported health following surgery. We hypothesize that hospitals located in less-concentrated areas (i.e. more hospitals and thus more competition) will provide higher quality of care, which will be reflected in greater improvement in patients’ self-reported health status, compared to hospitals in more concentrated markets (i.e. fewer hospitals and less competition). We test this by comparing differences in a disease specific PROM, the Oxford Hip score (OHS), before and after surgery for elective primary hip replacement patients treated at hospitals facing different degrees of local market concentration. The focus on one particular treatment and a disease-specific health measure allows us to control for initial health status and overcome the criticisms of earlier studies that used AMI mortality as the measure of quality of care.
Methods
Linked PROMs and HES data
We use linked Hospital Episode Statistics (HES) and PROMs for financial year 2011/12 for all English NHS hospitals and independent sector providers undertaking NHS-funded elective primary hip replacement surgery. The ‘sitetret’ variable in HES data was used to identify hospital site. An observation is defined as one finished consultant episode (FCE), which covers the period of time a patient is under the care of one consultant. All elective episodes of primary hip replacement were counted. NHS-funded hospital activity is categorized by Healthcare Resource Groups (HRGs), which are groupings of clinically similar treatments that use common levels of health care resources.10 We examined those HRG version 3.5 codes that cover elective primary hip replacement whether cemented or uncemented. We selected admission records which had full information on the patient’s age; sex; ethnicity; a measure of the local area deprivation of the small area in which the patient lives (Index of Multiple Deprivation (IMD04)); an indicator of rural or urban location; patient-reported disability; patient-reported comorbidities11,12 in circulatory disease, liver disease, cancer, depression, heart disease, high blood pressure, stroke, lung disease, diabetes, kidney disease, nervous system disease and arthritis; previous similar surgery; additional hip procedures; duration of symptoms; living arrangement; EuroQol-Visual Analogue Scale (EQ-VAS) before treatment; and the OHS before and after treatment. The hospital characteristics considered were teaching status and location in Greater London. Other hospital characteristics were excluded as they were highly correlated with the measure of hospital concentration we used.
The mean OHS before treatment was 17.79 (on a scale of 0–48 in which a lower OHS score indicates a more severe hip condition). We categorized each FCE into one of two patient groups: less severe (with OHS before treatment of 18 or more) and more severe (with OHS before treatment less than 18). The linked HES and PROMs dataset contained 41,590 observations. We excluded 15,952 (38.4%) due to missing or invalid information on one or more variable. Our final sample contains 25,638 observations from 337 hospitals, comprising 215 NHS hospitals (belonging to 140 NHS trusts) and 122 independent sector providers (belonging to 12 private provider chains).
Main outcome measure
The PROMs available for hip patients include a condition-specific instrument (OHS) and a generic instrument (the EQ-5D). Condition-specific measures are generally more sensitive to minor changes in a patient’s health improvement after treatment, so we only used the OHS.13,14 The OHS includes 12 joint-specific items to assess symptoms and function in patients undergoing hip replacement surgery (Appendix 1, available online).15 Each is scored from 0 (most severe symptoms) to 4 (least or no symptoms). Thus, OHS values are between 0 (worst hip-related health) and 48 (best hip-related health). As the dependent variable in our analysis, we used the change in OHS after surgery to measure improvement in self-reported patient health.
Market concentration index
Two main measures of hospital market concentration are used in economics: the Herfindahl-Hirschman Index (HHI) and the number of alternative providers in an area.9 We define each hospital site as a discrete provider. We used the HHI for each hospital site, calculated from all eligible primary hip replacement episodes in HES, using the patient flow method to define the local market.3 The patient flow method has two steps. The first step measures the level of concentration in each location, defined as Middle Layer Super Output Areas (MSOAs). In 2011, there were 7102 MSOAs in England and Wales, with a mean population of 7800.16 In the second step, the level of concentration for each hospital is calculated as a weighted average of the MSOAs it serves where the weights are the share of the hospital’s patients that live in each MSOA.
We used the HHI because it allows for the relative sizes of different providers as well as their number and it is used widely in competition policy and literature on market power.17 The HHI in each MSOA is calculated as the sum of squared patient shares across all hospitals the MSOA sends its residents to for primary hip replacement surgery. The potential HHI lies in the range of 0–1, where 1 represents maximum market concentration or monopoly.
Statistical analysis
Patients’ health gain was measured by the change in OHS. We first investigated the relationship between market concentration and patient health gain for all patients. Gains in patients’ health were modelled as a function of the HHI, patient characteristics – OHS before treatment, EQ-VAS before treatment, patients self-reported disability, patients self-reported comorbidities, previous surgery, additional hip procedures, symptom period, living arrangement, age, sex, ethnicity, urban/rural indicator, IMD score and hospital characteristics – whether a London hospital and whether a teaching hospital. We then examine the effect of market concentration separately for patients whose hip problem was less severe and was more severe. All estimates were by random effects method at hospital site level. Data manipulation and analysis were performed with STATA/MP 12.1.
Results
The distribution of the HHI for NHS-funded primary hip replacements in 2011–2012 is shown in Figure 1. It ranges between 0.26 and 0.86, with a mean of 0.55. Note that the HHI is highly correlated with the number of providers (correlation coefficient = −0.882). Summary statistics are shown in Table 1.
Figure 1.
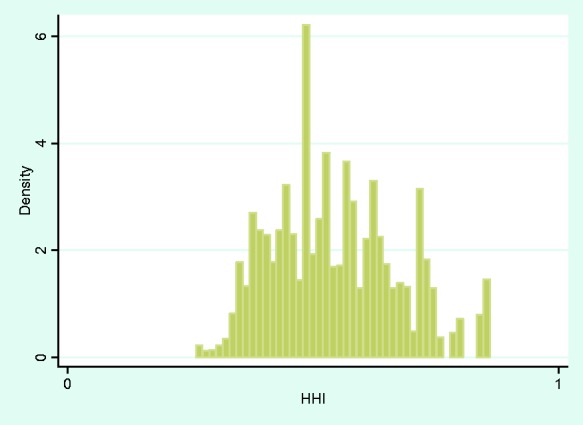
Distribution of market concentration of hospitals (n = 337) according to Herfindahl–Hirschman Index (HHI).
Table 1.
Summary statistics.
| Variable names | Mean | SD | Min | Max |
|---|---|---|---|---|
| Change in OHS after treatment | 20.66 | 9.97 | –32 | 46 |
| OHS before treatment | 17.79 | 8.14 | 0 | 48 |
| OHS after treatment | 38.45 | 9.13 | 0 | 48 |
| HHI | 0.55 | 0.13 | 0.26 | 0.86 |
| Number of competitors | 3.28 | 0.72 | 1.92 | 6.32 |
| Patients characteristics | ||||
| IMD score 2004 | 17.74 | 13.00 | 0.53 | 87.80 |
| Age in 2011 | 68.38 | 10.56 | 13 | 100 |
| EQ-VAS before treatment | 64.78 | 21.45 | 0 | 100 |
| Sex (men) | 40.52% | |||
| Ethnicity (British white) | 95.87% | |||
| Previous surgery | 3.04% | |||
| Disability before treatment | 39.66% | |||
| Living arrangements | ||||
| With partner/spouse/family/friends | 73.81% | |||
| Alone | 25.65% | |||
| Nursing home, hospital or other long-term care home | 0.15% | |||
| Other | 0.39% | |||
| Symptom period | ||||
| Less than 1 year | 13.84% | |||
| 1 to 5 years | 68.82% | |||
| 6 to 10 years | 10.68% | |||
| More than 10 years | 6.66% | |||
| Comorbidity | ||||
| Circulation disease | 6.15% | |||
| Liver disease | 0.51% | |||
| Cancer | 4.76% | |||
| Depression | 7.59% | |||
| Heart disease | 10.15% | |||
| High blood pressure | 40.67% | |||
| Stroke disease | 1.40% | |||
| Lung disease | 7.72% | |||
| Diabetes | 9.05% | |||
| Kidney disease | 1.65% | |||
| Nervous system | 0.67% | |||
| Arthritis | 74.13% | |||
| Rural/urban indicator | ||||
| Fraction urban (sparse) | 0.31% | |||
| Fraction town and fringe (sparse) | 0.89% | |||
| Fraction village (sparse) | 1.03% | |||
| Fraction hamlet and Isolated dwelling (sparse) | 0.74% | |||
| Fraction urban (less sparse) | 70.72% | |||
| Fraction town and Fringe (less sparse) | 11.87% | |||
| Fraction village (less sparse) | 10.02% | |||
| Fraction hamlet and Isolated dwelling (less sparse) | 4.42% | |||
| Hospital characteristics | ||||
| London hospital | 6.95% | |||
| Teaching hospital | 16.19% | |||
| Observations | 25,638 | |||
About 96.80% of patients (24,817/25,638) undergoing elective primary hip replacement surgery and reporting PROMs before and after surgery, reported a health gain. The distribution of changes in OHS following surgery is presented in Figure 2. We first analysed the relationship between average health gains at hospital level and the HHI without adjusting for the effect of any confounders. Figure 3 uses all 337 hospital sites and 24,817 FCEs. The circle size shows the amount of activity (number of FCEs) at each hospital. This shows that the more concentrated the market, the smaller the health gain from hip surgery, though the unadjusted slope is slight.
Figure 2.
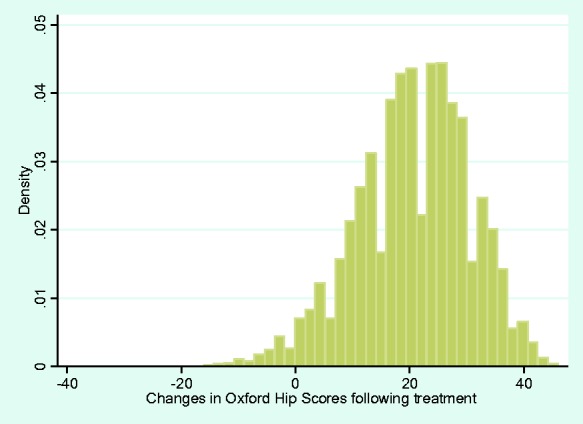
Distribution of the changes in Oxford Hip Scores following treatment (n = 25,638).
Figure 3.
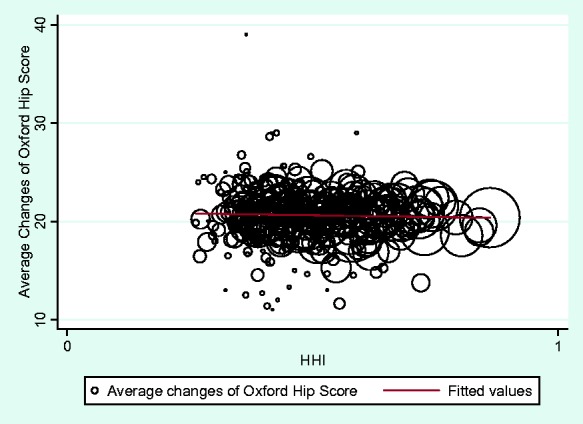
The relationship between HHI and the average unadjusted change of Oxford Hip Score for all patients for 337 hospitals.
The second column of Table 2 shows the results from the baseline model. It models patients’ health gains without adjusting for any patient or hospital characteristics. There is a statistically insignificant negative association between patient health gain and market concentration.
Table 2.
Modelling the change in Oxford Hip Score after hip replacement surgery.
| Column 1 |
Column 2 |
Column 3 |
Column 4 |
Column 5 |
|---|---|---|---|---|
| Variables | Baseline model (p-value) | Less healthy patients (p-value) | Healthier patients (p-value) | Full model (p-value) |
| HHI | −0.94* (0.05) | 0.13 (0.88) | −0.80* (0.09) | −0.12 (0.76) |
| OHS before | −0.65** (0.00) | −0.88** (0.00) | −0.77** (0.00) | |
| EQ-VAS before | 0.04** (0.00) | 0.04** (0.00) | 0.04** (0.00) | |
| Previous surgery | 2.04** (0.00) | 0.40 (0.28) | 1.35** (0.00) | |
| Disability | 2.70** (0.00) | 1.58** (0.00) | 2.08** (0.00) | |
| Living arrangement (living with partner/ spouse/family/friends as baseline) | ||||
| Alone | −0.40** (0.04) | 0.00 (0.98) | −0.21* (0.09) | |
| Long-term care home | 1.06 (0.57) | −1.26 (0.49) | −0.07 (0.96) | |
| Other | −2.16* (0.09) | 1.01 (0.31) | −0.65 (0.42) | |
| Symptom period (less than 1 year as baseline) | ||||
| 1–5 years | −0.96** (0.00) | −0.31* (0.09) | −0.64** (0.00) | |
| 6–10 years | −2.44** (0.00) | −0.35 (0.16) | −1.38** (0.00) | |
| More than 10 years | −2.25** (0.00) | −0.53* (0.08) | −1.49** (0.00) | |
| Comorbidity (12 diseases) | ||||
| Circulation disease | −3.27** (0.00) | −3.49** (0.00) | −3.49** (0.00) | |
| Liver disease | 1.12 (0.28) | −0.53 (0.58) | 0.43 (0.55) | |
| Cancer | −0.84** (0.02) | −0.17 (0.56) | −0.54** (0.02) | |
| Depression | −2.26** (0.00) | −1.91** (0.00) | −2.25** (0.00) | |
| Heart disease | −0.68** (0.01) | −0.83** (0.00) | −0.82** (0.00) | |
| High BP | −0.12 (0.47) | −0.38** (0.00) | −0.23** (0.03) | |
| Stroke disease | −1.54** (0.01) | −1.41** (0.02) | −1.53** (0.00) | |
| Lung disease | −1.01** (0.00) | −0.69** (0.01) | −0.95**(0.00) | |
| Diabetes | −1.44** (0.00) | −0.71** (0.00) | −1.17** (0.00) | |
| Kidney disease | −0.11 (0.84) | −0.04 (0.95) | −0.12 (0.77) | |
| Nervous system | −0.88 (0.29) | 0.59 (0.55) | −0.52 (0.40) | |
| Arthritis | −0.73** (0.00) | −0.31** (0.02) | −0.51** (0.00) | |
| Rural urban indicator (urban sparse as baseline) | ||||
| Town and fringe (sparse) | 1.29 (0.46) | 1.94 (0.12) | 1.72 (0.11) | |
| Village (sparse) | 2.05 (0.23) | 3.00** (0.01) | 2.56** (0.01) | |
| Hamlet and Isolated dwelling (sparse) | 1.75 (0.33) | 3.46** (0.01) | 2.74** (0.01) | |
| Urban (less sparse) | −0.37 (0.81) | 1.85* (0.09) | 0.78 (0.39) | |
| Town and Fringe (less sparse) | −0.26 (0.87) | 1.98* (0.07) | 0.94 (0.31) | |
| Village (less sparse) | 1.04 (0.49) | 2.48** (0.02) | 1.80* (0.05) | |
| Hamlet and Isolated dwelling (less sparse) | 0.54 (0.73) | 2.96** (0.01) | 1.86** (0.05) | |
| Index of deprivation | −0.07** (0.00) | −0.06** (0.00) | −0.07** (0.00) | |
| Sex (men as baseline) | −0.84** (0.00) | −0.87** (0.00) | −0.86** (0.00) | |
| Ethnicity (British white as baseline) | −1.04** (0.01) | −0.55* (0.09) | −0.91** (0.00) | |
| Patient age | −0.03** (0.00) | −0.05** (0.00) | −0.04** (0.00) | |
| London hospitals | −1.08** (0.01) | 0.03 (0.89) | −0.42** (0.04) | |
| Teaching hospitals | −0.17 (0.55) | 0.09 (0.58) | −0.01 (0.97) | |
| Constant | 21.18** (0.00) | 25.09** (0.00) | 31.03** (0.00) | 26.86** (0.00) |
| R-squared | 0.0001 | 0.138 | 0.320 | 0.336 |
| Observations | 25,638 | 13,055 | 12,583 | 25,638 |
Note: All models estimated with random effects.
p < 0.10.
p < 0.05.
Columns 3–5 of Table 2 present the results from modelling the health gains adjusted for patient and hospital characteristics. Column 5 shows the results if all patients are included. This shows no statistically significant association between patients’ health gain and hospital market concentration when patient and hospital characteristics are allowed for. We then ran regressions for the two subgroups of patients based on pre-operative severity. The results in column 3 show no significant association between patients’ health gain and market concentration for less healthy patients. But for 12,583 (49.1% of the sample) healthier patients the results in column 4 show a small negative association between market concentration and health gain, though this was not statistically significant at p < 0.05. A one standard deviation increase in HHI (equivalent to a decrease of about one hospital in each local market) was associated with a 0.010 (=0.13 × (−0.80)/9.97) standard deviation lower OHS gain or 0.104 (=0.13 × (−0.80)) less OHS gain.
Discussion
Main findings
The key finding from this study is that we found no statistically significant association (at the 5% level) between hospital market concentration and the improvement in health of hip patients after surgery.
For less severe hip patients, there is a small negative association between hospital market concentration and their health gains after treatment but this is not statistically significant at the 5% level. We intend to reinvestigate this relationship when data from later years become available. Our p-value (p = 0.09) is not small enough to justify rejection of the null hypothesis, i.e. no effect of hospital market concentration. Thus we did not find strong evidence that hospital market concentration has an effect on less severe patients’ health gains after treatment.
Limitations
We excluded 5320 (17.2%) observations from the analysis because of a missing OHS value before or after treatment. The majority (5131) were due to patients who did not return their post-operative OHS questionnaires despite completing pre-operative questionnaires. Only 48 were missing both pre- and post-operative OHS questionnaires and 141 were missing pre-operative OHS questionnaires but not post-operative. The missing observations could be systematically related to some patient characteristics and/or hospital characteristics. This would lead to biased estimates although the size and direction of the bias are not clear.
We included a rich set of patient and hospital characteristics in the model. However, the results could still be biased as the result of other potential confounding patient and hospital variables in the cross-sectional analysis. The size and direction of the bias are not clear in the model with more than two variables.18,19
In principle, we might try to deal missing confounders in two ways. First, we could look for an exogenous variable as the proxy for market concentration. In the present case, there is no obvious instrument. Second, we could run a fixed effects model at hospital level with more than one year’s data. However, we could not do a differences-in-difference analysis because of the nature of the way that PROMs data were collected, i.e. it does not provide information about a control group.
Conclusion
Hospital market concentration (as a proxy for competition) appears to have no significant (at the 5% level) influence on the outcome of elective primary hip replacement. The generalizability of this finding needs to be investigated.
Acknowledgements
The paper is co-funded by the Office of Health Economics, London, UK and the Nuffield Trust, London, UK. We are grateful for helpful advice from Mauro Laudicella, George Stoye and Adam Roberts. The views are those of the authors and not necessarily of the funders.
Supplementary Material
The online appendix is available at http://hsr.sagepub.com/supplemental-data
References
- 1.Office of Health Economics. Report of the Office of Health Economics Commission on competition in the NHS, London: Office of Health Economics, 2012. [Google Scholar]
- 2.Cooper Z, Gibbons S, Jones S, et al. Does hospital competition save lives? Evidence from the English NHS patient choice reforms. Econ J 2011; 121: 228–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaynor M, Moreno-Serra R, Propper C. Death by market power: reform, competition and patient outcomes in the National Health Service. Am Econ J: Econ Policy 2013; 5: 134–166. [Google Scholar]
- 4.Bloom N, Propper C, Seiler S, et al. The impact of competition on management quality: evidence from public hospitals, http://cep.lse.ac.uk/pubs/download/dp0983.pdf (2010).
- 5.Pollock A, Macfarlane A, Kirkwood G, et al. No evidence that patient choice in the NHS saves lives. Lancet 2011; 378: 2057–2060. [DOI] [PubMed] [Google Scholar]
- 6.Bevan G, Skellern M. Does competition between hospitals improve clinical quality? A review of evidence from two eras of competition in the English NHS. BMJ 2011; 343: d6470–d6470. [DOI] [PubMed] [Google Scholar]
- 7.Mays B. Is there evidence that competition in healthcare is a good thing? No. BMJ 2011; 343: d4205–d4205. [DOI] [PubMed] [Google Scholar]
- 8.Black N. Competition in healthcare. Preliminary findings on competition in healthcare should not be over-interpreted. BMJ 2011; 343: d4731–d4731. [Google Scholar]
- 9.Gravelle H, Santos R, Siciliani L, et al. Hospital quality competition under fixed prices, http://www.york.ac.uk/media/che/documents/papers/researchpapers/CHERP80_hospital_quality_competition_fixedprices.pdf (2012).
- 10.Health & Social Care Information Centre. Hospital episode statistics, admitted patient care – England, 2011–12, http://www.hscic.gov.uk/catalogue/PUB08288.
- 11.Neuburger J, Hutchings A, Allwood D, et al. Sociodemographic differences in the severity and duration of disease amongst patients undergoing hip or knee replacement surgery. J Public Health 2012; 34: 421–429. [DOI] [PubMed] [Google Scholar]
- 12.Chard J, Kuczawski M, Black N. Outcomes of elective surgery undertaken in independent sector treatment centres and NHS providers in England: the patients outcomes in surgery audit. BMJ 2011; 343: d6404–d6404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Appleby J and Devlin N. Measuring success in the NHS. Using patient-assessed health outcomes to manage the performance of healthcare providers. London: The King’s Fund, 2004.
- 14.Feng Y, Parkin D and Devlin N. Assessing the Performance of the EQ-VAS in the NHS PROMs Programme. Qual Life Res 2014; 23: 977–989. [DOI] [PMC free article] [PubMed]
- 15.Dawson J, Fitzpatrick R, Carr A, et al. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg 1996; 78: 185–190. [PubMed] [Google Scholar]
- 16.Office for National Statistics. Super Output Area mid-year population estimates for England and Wales, Mid-2011 (Census Based), http://www.ons.gov.uk/ons/rel/sape/soa-mid-year-pop-est-engl-wales-exp/mid-2011–census-based-/index.html (2013).
- 17.Tirole J. Short-run price competition. In: Tirole J (ed.) The theory of industrial organization. Cambridge: MIT Press, 1988, pp.209–238.
- 18.Clark KA. Return of the phantom menace: omitted variable bias in political research. Conflict Manage Peace Sci 2009; 26: 46–66. [Google Scholar]
- 19.Clark KA. The phantom menace: omitted variable bias in econometric research. Conflict Manage Peace Sci 2005; 22: 341–352. [Google Scholar]


