Abstract
Background:
Poly cystic ovary syndrome (PCOS) is considered one of the most common endocrine disorders of women in reproductive age. The aim of this study was evaluating the efficacy of calcium and Vitamin D supplementation on the regularity of menstrual cycles, body mass index (BMI) and hyper androgenism state of women with PCOS.
Materials and Methods:
In this clinical trial, 80 women with PCOS were evaluated. They randomly located in four groups receiving metformin (group 1), metformin plus calcium and Vitamin D (group 2), calcium and Vitamin D (group 3) and placebo (group 4) for 4 months. BMI, regularity of menstrual cycles, hyperandrogenism (hirsutism and acne) and serum calcium and Vitamin D levels were compared in four studying groups at baseline and 4 months after the trial.
Results:
All studied subjects were similar at baseline (P > 0.05). After trial, the frequency of hirsutism and acne were not different among groups. Frequency regular menstrual cycle and dominant follicle were significantly higher in group 1 and 2 than others (P < 0.05). After trial, there was no significant difference with respect to BMI among groups.
Conclusion:
Vitamin D and calcium supplementation in addition to metformin therapy in women with PCOS could result in a better outcome in a variety of PCOS symptoms including menstrual regularity, and ovulation.
Keywords: Calcium, metformin, poly cystic ovary syndrome, vitamin D
INTRODUCTION
Poly cystic ovary syndrome (PCOS) is considered one of the most common endocrine disorders of women in reproductive age with an estimated prevalence rate of 10-15%.[1]
It was first described by Stein and Leventhal in 1935. According to the National Institute Of Health (NIH 1990), it is characterized by chronic anovulation and clinical or biochemical evidence of hyper androgenism.[1,2,3] PCOS is associated with multiple cardiovascular risk factors such as insulin resistance, central obesity, hypertension, impaired glucose tolerance, type 2 diabetes, metabolic syndrome, infertility, endometrial hyperplasia, endometrial and ovary cancers.[2] Moreover, it is associated with nontraditional markers of cardiovascular risk, including inflammation, thrombosis, oxidative stress, sleep apnea, endothelial dysfunction, and arterial stiffness.[4,5]
Evidences suggested that weight loss and metformin administration could improve hyper androgenic signs and symptoms of patients with PCOS possibly due to decreasing in androgen levels. Others demonstrated that changing in dietary habits, even without any significant weight loss may also improve endocrine feature and reproductive functions in this group of patients.[4]
The role of calcium (500 mg) and Vitamin D (400 unit) consumption and its deficiencies in different features of PCOS have been studied in some previous studies.[6,7,8] Their effectiveness is mainly due to their effect on body weight and follicular maturation. Both calcium and Vitamin D deficiency are considered as potential risk factors for obesity.[6,7,8] In addition, it is well established that increased body weight has a considerable negative effect on 25(OH) Vitamin D and 1, 25(OH)2 Vitamin D3 concentration in women with PCOS.[7]
The role of Vitamin D (50.000 unit) in the reproductive system has been also demonstrated in several studies.[9,10,11] Impaired calcium regulatory system could cause follicular arrest. Moreover, animal studies in this field indicated that the calcium has a crucial role in oocyte maturation as well as resumption and progression of follicular development.[12]
Considering that proper interventions could improve outcomes of PCOS and its related complications, we aimed to evaluate the effect of calcium and Vitamin D supplementations on menstrual regularity, follicle response, body mass index (BMI) and hyper androgenism symptoms in women with PCOS.
MATERIALS AND METHODS
In this prospective double-blind, placebo controlled trial study, women with PCOS aged 20-40 years who referred to obstetrics and gynecology clinic of Alzahra hospital, affiliated to Isfahan University of Medical Sciences, from July to December 2013 were evaluated. The diagnosis of PCOS was based on NIH 1990 criteria.[3] Women with the following criteria were diagnosed as having PCOS:
Chronic un ovulation,
Clinical or biochemical evidence of hyper androgenism and
Roll out of other causes (thyroid stimulating hormone, follicle-stimulating hormone, prolactin and testosterone measurement).
Those with Cushing syndrome, renal failure (Cr ≥1.5), androgenic ovarian and adrenal tumor, primary and secondary hyper parathyroidism, osteomalasia, cancers, gasterectomy, mental retardation, anticonvulsive drugs use and congenital adrenal hyper plasia were not included in the study.
The Regional Bioethics Committee of Isfahan University of Medical Sciences approved the protocol of the study (Research project Number: 392196). The study was also registered in the Iranian Registry of Clinical Trials (IRCT), IRCT registration number (201308037513 N 3). Written informed consent was obtained from all selected patients after explanation of the methods and goal of the study.
Selected women randomized in three interventional and one placebo groups based on allocation software. All cases had Vitamin D deficiencies. The three interventional groups were as follows [Figure 1]:
Figure 1.
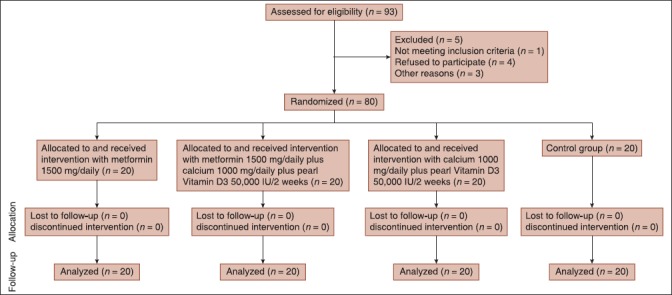
Consort diagram of the study
Metformin group (group1); received 1500 mg/day metformin (Osvah pharmaceutical company tablet 500 mg) (n = 20).
Metformin plus calcium and Vitamin D (group 2); received 1500 mg/day metformin plus 1000 mg/day calcium (Sobhan darou pharmaceutical company tablet 500 mg) plus 50,000 IU/2 weeks pearl Vitamin D3 (Zahravi pharmaceutical company pearl vitamin D3 50000 IU) (n = 20).
Calcium and Vitamin D (group 3); received 1000 mg/day calcium plus 50,000 IU/2 weeks pearl Vitamin D3 (n = 20).
Placebo group (group 4) received two low calorie sweetener tablets per day (n = 20).
All the studied groups received mentioned treatment for 4 months. Patients who have reported diarrhea, vomiting and severe abdominal distention during intervention were excluded from the study.
All patients examined clinically, and their demographic and menstrual and medical history recorded by a trained nurse using a check list. Trans abdominal sonography and laboratory analysis performed for evaluation of menstrual regularity and calcium, Vitamin D measurements, respectively.
Regularity of menstrual cycles, hyper androgenism (hirsutism and acne), BMI and serum calcium and Vitamin D level were compared in four studied groups at baseline and 4 months after trial.
Physical examination
Body weight and height of patients were measured to the nearest 0.1 kg and 0.5 cm using calibrated devices. BMI was calculated as weight (kg) divided by the height squared (m2).
Hirsutism was evaluated using the Ferriman-Gallwey method. Score >8 was considered as hirsutism.[2] In addition, the methods used to remove hairs and the frequency of using these methods (shaving, plucking) were asked and recorded for better scoring of hirsutism.
Acne was assessed based on the early involvement of the face in the areas of forehead, cheeks and nose.
Biochemical measurements
Venous blood sample was obtained from studied population. Serum total calcium was measured by the cresolphthalein complex method using Pars Azmoon Inc., kits (Tehran, Iran).
Serum 1-25(OH)2 Vitamin D3 was measured by using the enzyme-linked immunosorbent assay method using Euroimmun kit (Germany).
Ultrasonographic assessments
Ovarian transabdominal sonography was performed in all studied patients at the mid cycle (regularity of the menstrual cycle according to time intervals of 21-35 days) before and after trial for evaluating the evidences of ovulation and regularity of the menstrual cycle by SIUI CTS 8800 ultrasound.
Presence of the dominant follicle >14 mm considered as an evidence of ovulation.
Statistical analysis
Data were analyzed using SPSS version 20 (SPSS Inc., Chicago, IL, U.S.A.) software.
Qualitative variables were presented as number (%) and compared between the four studied groups using the Chi-square test. Quantitative variables were presented as the mean ± standard deviation (SD). The comparison of quantitative data between the four studied groups was done using one-way ANOVA and Post-hoc Scheffe test.
RESULTS
In this study, 80 women with PCOS were selected and randomized in four studied groups (20 in each group). Mean age of the studied population was 27.4 ± 2.2, 28.7 ± 4.5, 31.3 ± 4.6 and 27.2 ± 6.5 years old in groups 1, 2, 3 and 4, respectively (P = 0.09).
Familial history of PCOS was present in 8 (40%), 9 (45%), 8 (40%) and 10 (50%) of studied women with PCOS in groups 1, 2, 3, and 4 respectively (P = 0.09).
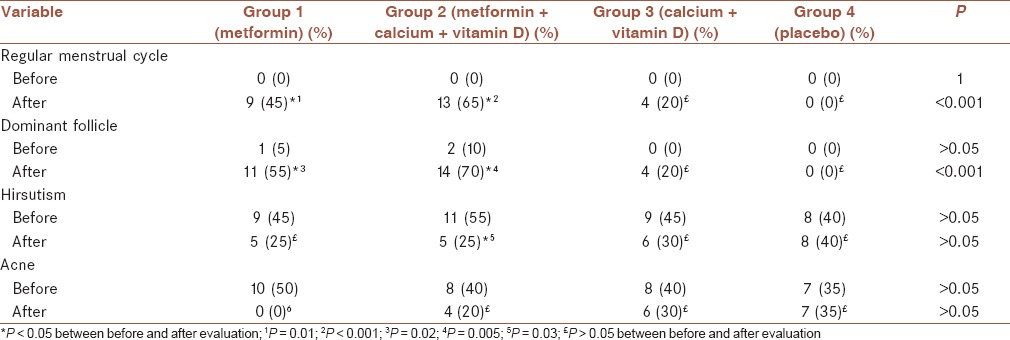
Frequency of regular menstrual cycle, dominant follicle and symptoms of hyperandrogenism in four studied groups before and after trial are presented in Table 1. Frequency of all mentioned factors before trial was similar in all studied groups. After trial, the values were similar for hirsutism and acne (P > 0.05). Frequency of regular menstrual cycle and dominant follicle were significantly higher in groups 1 and 2 than others (P < 0.05). Comparing frequencies for studied variables before and after trial showed that the differences for regular menstrual cycles and dominant follicle were more significant in group 1 and 2 (P < 0.05). Frequency of acne decreased significantly in group 1 after metformin administration (P < 0.001). Frequency of hirsutism decreased significantly in group 2 (P = 0.05).
Table 1.
Frequency (n [%]) of regular menstrual cycle, dominant follicle and symptoms of hyperandrogenism (hirsutism and acne) in four studied groups before and after trial
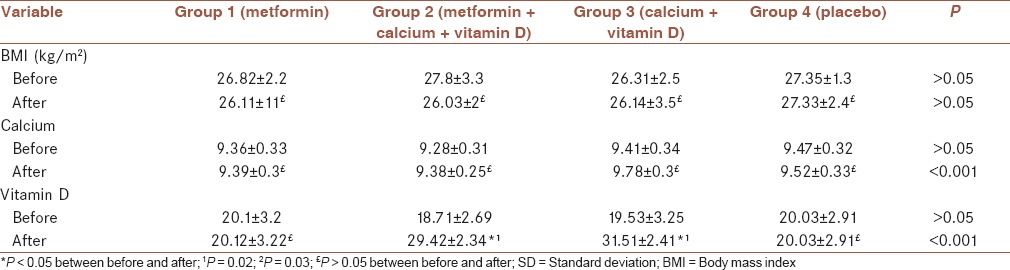
Mean ± SD of BMI, calcium and Vitamin D in four studied groups before and after trial are presented in Table 2. Mean of calcium and Vitamin D was significantly increased in group 2 and 3 than others. Mean differences of calcium was 0.026 ± 0.05, 0.56 ± 0.14, 0.38 ± 0.06 and 0.05 ± 0.24 in group 1, 2, 3, and 4 respectively. It was significantly higher in group 2 and 3 (P < 0.05). Mean differences of Vitamin D was 0.019 ± 0.08, 10.7 ± 3.75, 11.99 ± 2.19 and 0.008 ± 0.12 in group 1, 2, 3, and 4 respectively. It was significantly higher in group 2 and 3 (P < 0.05).
Table 2.
Mean ± SD of BMI, calcium and vitamin D in four studied groups before and after trial
DISCUSSION
In this clinical trial, we evaluated the effect of metformin, Vitamin D and calcium and combination of metformin with Vitamin D and calcium on menstrual regularity and symptoms of hyperandrogenism among women with PCOS. The results indicated that using metformin with Vitamin D and calcium seems to have more significant effects on improvement of mentioned symptoms. Though metformin therapy had a significant effect also but the effectiveness of metformin with Vitamin D and calcium seems to be more specially for hirsutism and regularity of menstrual cycles and ovulation. Metformin had more significant effect on acne.
Several studies investigated different therapeutic strategies of PCOS because PCOS is very common and can change the life style PCOS often with obesity and hirsutism and irregular menstruation that can very important for a person.[13,14]
The role of calcium and Vitamin D in the pathogenesis of PCOS, follicle maturation and ovulation have been demonstrated in many studies.[9,10,11,15] It is suggested that their role in this field is independent of the effect of insulin resistance. Accordingly, it seems that they have an important role in the conversion of testosterone to estrogens in granulosa cells, which consequently made an appropriate balance on androgen and estrogen level in patients with PCOS.[16,17]
Many studies have demonstrated the potential improving effects of combined Vitamin D and calcium supplementation on PCOS symptoms such as infertility, regularity of menstrual cycles, BMI, insulin resistance and features of hyper androgenism.[4,5,18] Recently in a review study Galusha concluded that though their positive effects in this field have been reported in many studies, but there are many controversies in this regard and quality of evidences are not satisfactory enough.[2] Hans, in the current study, we evaluated the effectiveness of Vitamin D and calcium as supplement therapy in addition to routine metformin therapy and also solely use of the supplements without metformin in improving the symptoms of PCOS.[6]
The results of our study showed that using Vitamin D and calcium without metformin had not any significant effect on clinical and biochemical variables related to PCOS. Both metformin and metformin with Vitamin D and calcium have a potential role in improving menstrual regularity and follicular maturation. According to before-after results, it seems that the effectiveness of using metformin with Vitamin D and calcium in improving menstrual regularity and follicular maturation were more significant than using metformin (65% vs. 45% for menstrual regularity and 60% vs. 50% for follicular maturation). However for comparing the effectiveness of the two treatment strategies, further studies with larger sample size and long duration is recommended. Using metformin with Vitamin D and calcium have a significant effect on hirsutism, whereas it metformin administration had not significant effect on it. Metformin had a significant effect on acne. Though BMI reduction was not statistically significant in all studied groups, but the reduction was higher in group that received metformin with Vitamin D and calcium.
Several studies in Iran and different countries have also investigated the effectiveness of Mentioned treatment strategy.[4,5,18,19,20,21,22] In a similar study in Yazd-Iran, Firouzabadi et al. have compared the effectiveness of metformin and metformin plus Vitamin D and calcium supplementation on PCOS symptoms of 100 women. The treatment period was 6 months. They concluded that Vitamin D and calcium supplementation have a positive effect on BMI, follicular maturation, regularity of menses, androgen related symptoms, infertility and insulin resistance specially in women with Vitamin D deficiency. The limitation of their study was lack of a control group.[4]
In another study in Tehran, Rashidi et al. have studied the role of these supplementations on PCOS outcomes in 60 patients. Their studied groups were similar to ours. Treatment period was 3 months, which followed up for a further 3 months. They showed that Vitamin D and calcium in combination with metformin have significant effect on menstrual regulation and follicular development.[5]
Pal et al. in the United States have assessed the effects of Vitamin D and calcium on hormonal and metabolic factors of twelve overweight and Vitamin D deficient women with PCOS in a 3 months trial. They indicated the significant effect of Vitamin D on androgen level and blood pressure profile of studied population.[19]
Ardabili et al. in Tabriz-Iran did not show any significant effect of Vitamin D supplementation on insulin sensitivity and insulin resistance in women with PCOS and Vitamin D deficiency.[20]
Selimoglu et al. in Turkey suggested that Vitamin D in patients with PCOS could improve hirsutism.[21]
Bonakdaran et al. have shown that Vitamin D has a crucial role in ovulation induction in women with PCOS.[22]
Different reports regarding the effectiveness of Vitamin D and calcium supplementation on the outcomes of PCOS may be due to differences in population selection, methodology, duration of study and treatment strategies.
The design and results of our study was similar to Rashidi et al. study, in addition to that we have a placebo group also which is considered as the strength of this study.
The limitations of the current study were small sample size of patients, lack of follow up period, and short duration of study. In this study, we did not compare the results of studied treatment strategies in PCOS women with and without Vitamin D deficiency because of small sample size. We used transabdominal ultrasonography for evaluation of follicular maturation due to that we have virgin patients with PCOS, whereas it seems that transvaginal sonography is more accurate.
It seems that other hormonal and biochemical measurements would be helpful in understanding the mechanisms of mentioned supplements. Long-term prospective studies with larger sample size of patients would remove the confounding effects of variables such as ethnicity, familiar history, environmental factors, and lifestyle methods in this regard.
CONCLUSION
The results of this trial indicated that Vitamin D and calcium supplementation in addition to metformin therapy in women with PCOS could result in better outcome in a variety of PCOS symptoms including menstrual regularity, ovulation, some features of hyperandrogenism (hirsutism) and BMI. Considering that both Vitamin D and calcium are safe, inexpensive and easily accessible treatment in patients with PCOS, it is recommended to use this treatment strategy in this group of patients especially those with Vitamin D deficiency. However for achieving more conclusive results regarding the effectiveness of mentioned treatment strategies as well as its pathophysiology, further studies with consideration of mentioned limitations are recommended.
AUTHORS’ CONTRIBUTIONS
All authors have contributed in designing and conducting the study. All authors have assisted in preparation of the first draft of the manuscript or revising it critically for important intellectual content. All authors have read and approved the content of the manuscript and confirmed the accuracy or integrity of any part of the work.
ACKNOWLEDGMENT
For his many helpful and constructive gramtical and linguistic comments would like to express our endless gratitude and indebtedness to Mr. Rohollah Datli Beigi, M.A. in English literature, University of Isfahan. The regional bioethics committee of Isfahan university of medical science approved the project of the study (research project number; 392196).
REFERENCES
- 1.Gibbs R, Karian B, Haney A, Nygaard I. Philadelphia: Lippincott Williams and Wilkins; 2008. Danforth's Obstetrics and Gynecology; p. 655. 661. [Google Scholar]
- 2.Fritz M, Speroff L. Philadelphia: Lippincott Williams and Wilkins; 2011. Clinical Gynecologic Endocrinology and Infertility; pp. 512–8. 523, 525, 29, 728-34. [Google Scholar]
- 3.Cohen D. Amenorrhea. In: Berek J, editor. Berek and Novak's Gynecology. Vol. 2. Philadelphia: Lippincott Williams and Wilkins; 2012. pp. 1050–6. [Google Scholar]
- 4.Firouzabadi RD, Aflatoonian A, Modarresi S, Sekhavat L, MohammadTaheri S. Therapeutic effects of calcium & vitamin D supplementation in women with PCOS. Complement Ther Clin Pract. 2012;18:85–8. doi: 10.1016/j.ctcp.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Rashidi B, Haghollahi F, Shariat M, Zayerii F. The effects of calcium-vitamin D and metformin on polycystic ovary syndrome: A pilot study. Taiwan J Obstet Gynecol. 2009;48:142–7. doi: 10.1016/S1028-4559(09)60275-8. [DOI] [PubMed] [Google Scholar]
- 6.Hahn S, Haselhorst U, Tan S, Quadbeck B, Schmidt M, Roesler S, et al. Low serum 25-hydroxyvitamin D concentrations are associated with insulin resistance and obesity in women with polycystic ovary syndrome. Exp Clin Endocrinol Diabetes. 2006;114:577–83. doi: 10.1055/s-2006-948308. [DOI] [PubMed] [Google Scholar]
- 7.Muscogiuri G, Sorice GP, Prioletta A, Policola C, Della Casa S, Pontecorvi A, et al. 25-Hydroxyvitamin D concentration correlates with insulin-sensitivity and BMI in obesity. Obesity (Silver Spring) 2010;18:1906–10. doi: 10.1038/oby.2010.11. [DOI] [PubMed] [Google Scholar]
- 8.Wehr E, Pilz S, Schweighofer N, Giuliani A, Kopera D, Pieber TR, et al. Association of hypovitaminosis D with metabolic disturbances in polycystic ovary syndrome. Eur J Endocrinol. 2009;161:575–82. doi: 10.1530/EJE-09-0432. [DOI] [PubMed] [Google Scholar]
- 9.Anagnostis P, Karras S, Goulis DG. Vitamin D in human reproduction: a narrative review. Int J Clin Pract. 2013;67:225–35. doi: 10.1111/ijcp.12031. [DOI] [PubMed] [Google Scholar]
- 10.Brzozowska M, Karowicz-Bilinska A. The role of vitamin D deficiency in the etiology of polycystic ovary syndrome disorders. Ginekol Pol. 2013;84:456–60. doi: 10.17772/gp/1604. [DOI] [PubMed] [Google Scholar]
- 11.Thomson RL, Spedding S, Buckley JD. Vitamin D in the aetiology and management of polycystic ovary syndrome. Clin Endocrinol (Oxf) 2012;77:343–50. doi: 10.1111/j.1365-2265.2012.04434.x. [DOI] [PubMed] [Google Scholar]
- 12.Thys-Jacobs S, Donovan D, Papadopoulos A, Sarrel P, Bilezikian JP. Vitamin D and calcium dysregulation in the polycystic ovarian syndrome. Steroids. 1999;64:430–5. doi: 10.1016/s0039-128x(99)00012-4. [DOI] [PubMed] [Google Scholar]
- 13.Setji TL, Brown AJ. Polycystic ovary syndrome: Update on diagnosis and treatment. Am J Med. 2014 doi: 10.1016/j.amjmed.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 14.Sirmans SM, Pate KA. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin Epidemiol. 2013;6:1–13. doi: 10.2147/CLEP.S37559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Showell MG, Brown J, Clarke J, Hart RJ. Antioxidants for female subfertility. Cochrane Database Syst Rev. 2013;8:CD007807. doi: 10.1002/14651858.CD007807.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Das M, Djahanbakhch O, Hacihanefioglu B, Saridogan E, Ikram M, Ghali L, et al. Granulosa cell survival and proliferation are altered in polycystic ovary syndrome. J Clin Endocrinol Metab. 2008;93:881–7. doi: 10.1210/jc.2007-1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lou YR, Murtola T, Tuohimaa P. Regulation of aromatase and 5alpha-reductase by 25-hydroxyvitamin D(3), 1alpha, 25-dihydroxyvitamin D(3), dexamethasone and progesterone in prostate cancer cells. J Steroid Biochem Mol Biol. 2005;94:151–7. doi: 10.1016/j.jsbmb.2005.01.024. [DOI] [PubMed] [Google Scholar]
- 18.Galusha AM. Improvement of Symptoms in Patients with Polycystic Ovarian Syndrome by vitamin D and Calcium Supplementation. School of Physician Assistant Studies. Paper. 2013;461 [Google Scholar]
- 19.Pal L, Berry A, Coraluzzi L, Kustan E, Danton C, Shaw J, et al. Therapeutic implications of vitamin D and calcium in overweight women with polycystic ovary syndrome. Gynecol Endocrinol. 2012;28:965–8. doi: 10.3109/09513590.2012.696753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ardabili HR, Gargari BP, Farzadi L. Vitamin D supplementation has no effect on insulin resistance assessment in women with polycystic ovary syndrome and vitamin D deficiency. Nutr Res. 2012;32:195–201. doi: 10.1016/j.nutres.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Selimoglu H, Duran C, Kiyici S, Ersoy C, Guclu M, Ozkaya G, et al. The effect of vitamin D replacement therapy on insulin resistance and androgen levels in women with polycystic ovary syndrome. J Endocrinol Invest. 2010;33:234–8. doi: 10.1007/BF03345785. [DOI] [PubMed] [Google Scholar]
- 22.Bonakdaran SH, Mazloom Z, Davachi B, Mazloom J. The effects of calcitriol on improvement of insulin resistance, ovulation and comparison with Metformin therapy in PCOS patients: A randomized placebo-controlled clinical trial. Iran J Reprod Med. 2012;10:465–72. [PMC free article] [PubMed] [Google Scholar]


