Abstract
Introduction
Sociodemographic differences have been observed in the treatment of extremely premature (periviable) neonates, but the source of this variation is not well understood. We assessed the feasibility of using simulation to test the effect of maternal race and insurance status on shared decision-making (SDM) in periviable counseling.
Methods
We conducted a 2 × 2 factorial simulation experiment in which obstetricians and neonatologists counseled two consecutive standardized patients (SPs) diagnosed with ruptured membranes at 23 weeks, counterbalancing race (black/white) and insurance status using random permutation. We assessed verisimilitude of the simulation in semi-structured debriefing interviews. We coded physician communication related to resuscitation, mode of delivery, and steroid decisions using a 9-point SDM coding framework; then compared communication scores by SP race and insurer using ANOVA.
Results
Sixteen obstetricians and 15 neonatologists participated; 71% were women, 84% married, and 75% parents; 91% of physicians rated the simulation as highly realistic. Overall, SDM scores were relatively high, with means ranging from 6.4–7.9 (out of 9). There was a statistically significant interaction between race and insurer for SDM related to steroid use and mode of delivery (p<0.01 and p=0.01, respectively). Between group comparison revealed non-significant differences p=<0.10) between SDM scores for privately-insured black patients vs privately-insured white patients, Medicaid-insured white patients vs Medicaid-insured black patients, and privately-insured black patients vs Medicaid-insured black patients.
Conclusions
This study confirms that simulation is a feasible method for studying sociodemographic effects on periviable counseling. SDM may occur differentially based on patients’ sociodemographic characteristics and deserves further study.
Introduction
Despite advances in neonatal intensive care, periviable neonates (i.e., born between 22 and 25 weeks of gestation) suffer substantial mortality and morbidity, and long-term neurodevelopmental outcomes for these infants have not improved in recent years.1,2 Periviable births present significant emotional and financial burdens3–5– burdens born most heavily by black families, as black infants are more than three times as likely to be born extremely premature compared to white and Hispanic infants.6 Families and physicians are faced with the challenge of having to make what we typically think of as ‘end-of-life decisions’ at the time of delivery. These are difficult decisions for any parent, but those with the least financial and social capital may be most in need of decision support from their providers. In particular, these patients may benefit from a shared decision-making (SDM) encounter in which providers facilitate the informed participation and engagement of patients in clinical decision-making.7 SDM has been advocated as the optimal communiation strategy for patient-centered care8,9, particularly in contexts where “potentially life threatening illnesses, where there are important decisions to be made at key points in the disease process, and several treatment options exist with different possible outcomes and substantial uncertainty.”10 More than imparting requisite information, SDM also requires physicians to deliberate with and engage patients in communication about treatment decisions.11 Unfortunately, several studies have documented that physicians are not always proficient and effective in communicating with women and racial/ethnic minorities—the very patients bearing the greatest burden of prematurity-related infant mortality.12–15
Racial differences, such as higher use of neonatal intubation for periviable neonates born to black and Hispanic women, have been observed in periviable care.16,17 Little is known about the source of these differences, although extrapolation from the end-of-life decision-making literature suggests that black and Hispanic patients may have fundamentally different treatment preferences.18–24 An alternative explanation is that ineffective and/or biased patient-provider communication may underlie these differences.12,13,25–27 In an effort to disentangle the impact of patient preference from physician counseling practices, we designed a randomized, simulation-based trial to gather empirical evidence about the effect of varying patient sociodemographic characteristics on physicians’ counseling practices for periviable deliveries. This study design was chosen because standardized patients would allow for us to control for the variation in preferences one would normally encounter with real patients, thereby allowing us to better isolate variation in physicians’ counseling practices. Because periviable deliveries occur infrequently, usually without warning and under significant distress, real-time attempts to observe doctor-patient interactions prospectively would be expensive, time-consuming, and ethically questionable. As a result, the aim of this pilot study was to assess the feasibility of using simulation to assess the relationship between maternal race and insurance status on the quality of periviable counseling with regards to the extent to which shared decision-making (SDM) occurs.
Methods
Study Population
With the approval of the Indiana University Institutional Review Board, we conducted a single-center, simulation-based, randomized study of obstetricians’ and neonatologists’ periviable counseling practices. Through presentations at faculty meetings, e-mails to department distribution lists, and calls/visits to physicians’ offices, we recruited attending physicians and fellows from the Indiana University School of Medicine’s divisions of General Obstetrics and Gynecology and Maternal Fetal Medicine, and from the division of Neonatology at Riley Hospital for Children. OB/GYNs practicing gynecology-only as generalists or subspecialists were excluded from eligibility as were obstetricians and neonatologists who participated in case development or pilot testing. This was a mixed-methods project, and our sample size was selected with two principles in mind: 1) in qualitative studies, thematic saturation is customarily reached with 10–15 participants in relatively homogeneous populations28; and 2) as a feasibility pilot, we did not sample for statistical power, but rather to conduct sample size calculations for a future study. Therefore, our target for recruitment was 16 OB/GYNs and 16 Neonatologists.
Case Development and Experimental Conditions
A multi-disciplinary team of specialists from neonatology, maternal fetal medicine, and palliative care contributed to case development. The cases depicted a 31 year-old woman presenting to OB triage with preterm premature rupture of membranes (PPROM) at 23 weeks gestational age (GA). We trained 4 experienced standardized patients (SPs), 2 black and 2 white, to play the role of the patient based on detailed symptom and psychosocial profiles. The clinical components of the simulation were developed and refined in a series of pre-tests with 3 physician volunteers. Based on previous simulation work,29 each SP received 10 hours of training, which included “actor readings” involving case discussion, profile development, and role-play to develop, practice, and refine response principles to ensure standardization. SPs were also provided question prompts to inquire about three management decisions if these topics were not spontaneously addressed by the physician:
Resuscitation – as periviable neonates are born too early to breathe on their own outside of the womb, a decision must be made whether to intervene to support breathing or whether palliative measures will be taken.
Steroid administration - for patients who remain pregnant, timing of steroids (before vs after 24 weeks) is controversial because there is limited data to suggest that giving them earlier improves outcomes.
Mode of delivery (MOD)– a decision must also be made between cesarean section or vaginal delivery. Cesarean delivery confers increased morbidity to the mother, without clear evidence of improving outcomes for neonates.
Previous work30 and clinical experience identified these as ‘preference-sensitive’ decisions guided by resuscitation preference.
One case consisted of a patient complaining of a yeast infection; the other complaining of a urinary tract infection. Otherwise, the SPs portrayed patients with comparable medical and obstetrical histories, both of which were ultimately noted to have PPROM rather than yeast or urinary tract infections. During the simulation, the physician was told that a resident or midwife had evaluated the patient and confirmed the diagnosis of PPROM at 23 weeks. To identify the patient’s insurance status, the written case history provided to the physician participant described the patient as Medicaid-insured, receiving care in the resident clinic; or as privately-insured, receiving care in a colleague’s private practice.
Figure 1 depicts the experimental conditions. We randomly assigned each physician subject to counsel two patients from diagonal cells. One encounter was simulated by a black SP; the other by a white SP. We counterbalanced the effects of case order by randomly alternating which case was presented first. Randomization was conducted using a table of random permutations, rather than independent randomization, due to the small sample size. This assured that each condition and order occurred with similar frequency. We used sealed envelopes to determine each subject’s randomization sequence; first race, then insurer. The second scenario was the complement of the first.
Figure 1.
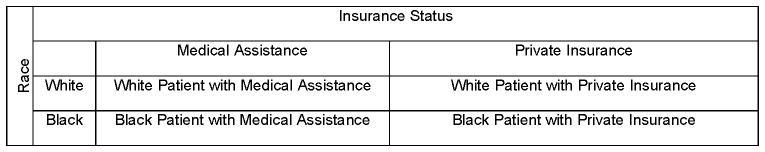
2×2 table depicting experimental conditions.
At the initiation of the simulation, study participants were told that a patient asked to speak to a doctor for information after being admitted for PPROM. The physician was then instructed to “Please counsel this patient as you would in your typical practice,” and was given time to review a written synopsis of the patient’s medical record. Each simulation ran until a physician completed counseling or 30 minutes elapsed. After simulation, the study participants completed a self-administered survey, which collected data on demographics expected to impact perviable decision-making based on previous literature,30 as well as institutional and individual thresholds for viability. Finally, physicians completed a debriefing interview to: 1) discuss the verisimilitude of the simulation; and 2) provide ‘think aloud’ commentary on reviewing segments of their counseling session. Study participants were not informed of the primary aim of the study until the end of their debrief interview. Each physician was compensated $100 for study participation.
Outcome of Interest
The American Academy of Pediatrics designates decision-making at the limits of viability as preference-sensitive and subject to shared decision-making.31 Therefore, we examined SDM behaviors as an indicator of the quality of periviable counseling. We operationalized the construct of SDM by adapting a previously described and validated coding scheme from work by Braddock.32 Though initially developed for primary care settings, the coding scheme has been applied to surgical and psychiatric settings.33,34 Based on Braddock’s scale,33 our codebook was comprised of the following 9 elements of SDM: 1) Discussion of the patient’s role in decision making; 2) Discussion of patient’s goal and the context of the decision; 3) Discussion of the clinical issue or nature of the decision; 4) Discussion of uncertainties associated with the decision; 5) Discussion of alternatives; 6) Discussion of risks and benefits associated with the decision; 7) Assessment of the patient’s understanding; 8) Assessment of patient’s desire for others’ input; and 9) Exploration of patient’s preference. The original scale was designed with three ratings per category (absent, partial, complete) scored at 0, 1, and 2 respectively. We developed a codebook that would apply to periviable encounters, and, given the exploratory nature of the study, adapted the scoring rubric into a dichotomized rating system of ‘present’ or ‘absent’ by collapsing partial and complete into one ‘present’ category, thereby creating a 9-point SDM score. Each of these three management decisions (resuscitation, steroids, or MOD) was analyzed and scored independently. If study participants explicitly discussed deferring counseling regarding risks, benefits, or alternatives for a particular management decision to the other specialty, they were given a point for those components of the discussion, so as not to penalize them for limiting their counseling conversation to their scope of practice. The maximum SDM score a provider could receive for each decision, even with a deferral, was 9 points. This decision may inflate SDM scores, but would not be expected to do so systematically.
Analyses
Coding and content analyses
Audio files of the simulation sessions, as well as the physician debriefing interviews, were transcribed verbatim. We applied the adapted coding scheme to evaluate SDM behaviors and calculate an SDM score (0–9). Two raters, both blinded to the primary aims of the study, independently coded each of the 62 encounters. Ten percent of the transcripts were coded by the PI for quality assurance. Coding discrepancies were resolved, and consensus ratings were used in the analyses. Verisimilitude was assessed qualitatively by reviewing the physician responses to the question ‘did the encounters feel realistic to you,’ which was asked of each physician in their debriefing interview.
Statistical analyses
Characteristics of the study participants were summarized using descriptive statistics. Multivariable analyses were conducted using a 2×2 Analysis of Variance (ANOVA). We accounted for repeated measures within each subject by including a random effect for each subject in the model. We controlled for order effects by including case order as a covariate in the model. We did not adjust for multiple comparisons, since this procedure can obscure potential findings in exploratory contexts.35 Sample size calculations were performed in order to power a subsequent study under a balanced incomplete block design where each physician represents a block of size two.
Results
Study Population
Sixteen of 37 eligible OB/GYN’s (43%) and 15 of 43 eligible Neonatologists (35%) participated. Seventy-one percent were White, 16% Black, and 10% Asian. Seventy-one percent were women, 84% married, and 75% parents. The average age of the study participants was 44 (SD= 11.1) and average time in practice was 12 years (SD = 11.1). Over half (61.3%) identified as Protestant or Catholic, and 71% viewed religion favorably, rating it as at least fairly important. Participants’ assessments of institutional and personal thresholds for viability and cesarean largely converged in the 23–24 week window. When asked to provide cutoffs for viability and periviable cesarean at their institution, 23 weeks was most frequently reported (modal response), receiving 58% and 48% of responses for viability and cesarean, respectively. Thirty two percent considered 24 weeks the limit of viability for themselves or a loved one; regarding cesarean, both 24 weeks and 26 weeks were the modal responses at 29% each. When asked specifically about optimal mode of delivery for a 23 week vertex fetus, 97% selected vaginal delivery compared to 52% for a 23 week breech fetus. When asked about the chances of survival for a 23 week fetus, the most common response was a 30% survival rate (reported by 29% of physicians).
Verisimilitude
The average duration of encounters was 18 minutes. Ninety-one percent of physicians rated the simulation as highly realistic. When asked, “Did the patient encounter feel real,” one physicians’ response captured the sentiment of most respondents:
“It did. This is a situation that I encounter on a monthly basis. The patient’s affect and clinical scenario in terms of they’re in a gown and in bed, not having been told much and so it’s very real.” [17-0]
Among the 3 physicians who responded that the scenario did not feel real, 2 neonatologists stated that it was unusual to encounter a patient who had not already been counseled to some extent by their OB, and 1 obstetrician stated that her patients usually looked for the ‘silver lining,’ and rarely ask questions about the possibility of a bad outcome.
SDM scoring
Table 2 presents the percentage of physicians receiving credit for each element of the SDM scoring rubric. Discussions of the ‘clinical issue’ were consistently present (100% for all four treatment groups). Conversely, discussions of the ‘patient’s goals’ were typically absent. With the exception of the encounters with Medicaid-insured black patients, these discussions were present for fewer than half of the physicians across treatment groups. These data are consistent with our qualitative observations that information regarding diagnosis and prognosis were heavily emphasized, while attempts to elicit goals and values were often lacking. Mean SDM scores are described in Table 3. Overall, scores ranged from 6.4–7.9. Across all three treatment decisions, physicians consistently received the lowest SDM scores in encounters with privately-insured black patients; conversely, SDM scores were highest for all three decisions in encounters with Medicaid-insured black patients.
Table 2.
Percentage of Physicians Scored ‘Present’ on Each SDM Element, by Experimental Group (N=62 encounters among 31 physicians)
| Treatment Group | ||||
|---|---|---|---|---|
|
| ||||
| Element of SDM | Black Medicaid (n=15) | Black Private (n=16) | White Medicaid (n=16) | White Private (n=15) |
|
| ||||
| Discussion of the patient’s role in decision-making, % (n) | 100 (15) | 88 (14) | 88 (14) | 100 (15) |
|
| ||||
| Discussion of patient’s goal and context of the decision, % (n) | 60 (9) | 19 (3) | 25 (4) | 47 (7) |
|
| ||||
| Discussion of the clinical issue or nature of the decision, % (n) | 100 (15) | 100 (16) | 100 (16) | 100 (15) |
|
| ||||
| Discussion of uncertainties associated with the decision, % (n) | 100 (15) | 94 (15) | 94 (15) | 100 (15) |
|
| ||||
| Discussion of alternatives, % (n) | ||||
| Resuscitation | 80 (12) | 81 (13) | 81 (13) | 80 (12) |
| Mode of Delivery | 87 (13) | 69 (11) | 69 (11) | 93 (14) |
| Steroids | 80 (12) | 56 (9) | 69 (11) | 87 (13) |
|
| ||||
| Discussion of risks and benefits associated with the decision, % (n) | ||||
| Resuscitation | 73 (11) | 50 (8) | 63 (10) | 53 (8) |
| Mode of Delivery | 73 (11) | 56 (9) | 56 (9) | 80 (12) |
| Steroids | 80 (12) | 56 (9) | 50 (8) | 67 (10) |
|
| ||||
| Assessment of the patient’s understanding, % (n) | 100 (15) | 100 (16) | 100 (16) | 93 (14) |
|
| ||||
| Patient’s desire for others’ input, % (n) | 80 (12) | 81 (13) | 94 (15) | 93 (14) |
|
| ||||
| Exploration of the patient’s preference, % (n) | 87 (13) | 50 (8) | 56 (9) | 73 (11) |
Table 3.
Mean SDM Scores per Treatment Decision, by Experimental Group
| Black Medicaid | Black Private | White Medicaid | White Private | |||||
|---|---|---|---|---|---|---|---|---|
| Treatment Decisions | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Resuscitation | 7.8 | 1.1 | 6.6 | 1.7 | 7.0 | 1.5 | 7.4 | 1.2 |
| Steroids | 7.9 | 1.2 | 6.6 | 1.7 | 6.8 | 1.6 | 7.8 | 0.9 |
| MOD | 7.9 | 0.8 | 6.4 | 1.8 | 6.8 | 1.8 | 7.6 | 1.0 |
SDM scoring by race and insurer
There was a statistically significant interaction between race and insurer for 2 of the 3 management decisions (steroids p=0.01; MOD p=0.01; resuscitation p=0.08). Between-group comparisons are presented in Table 2. Physicians received lower SDM scores when counseling privately-insured black patients compared to privately-insured white patients on MOD and steroids decisions (mean 6.6 vs 7.8, p=0.02 and 6.4 vs 7.6, p=0.03). Additionally, a racial difference was observed in steroid counseling for Medicaid-insured patients, with physicians receiving lower SDM scores when counseling white Medicaid-insured patients compared to their black counterparts (mean 6.8 vs 7.9, p=0.04). Among black patients, physicians received lower scores when counseling black privately-insured patients compared to black Medicaid-insured patients across all three decisions (resuscitation 6.6 vs 7.8, p=0.03; MOD 6.6 vs 7.8, p=0.02; steroids 6.4 vs 7.9, p=0.01).
Effect size assessments and sample size for subsequent studies
To assess effect sizes and calculate sample sizes needed for subsequent studies, we used the range of standard deviations detected in the current study to estimate the standard deviation in a subsequent study. In order to ensure 95% confidence with 80% power, we would need between 12 to 18 physicians’ participation to detect a one point mean difference in SDM scores. To detect a mean difference as small as 0.5 points, we would need 30–54 physician participants. In order to power for multiple comparisons (conservatively using Bonferroni adjustment), we would then need between 18 and 24 participants to detect a one point difference and between 42 and 78 participants to detect a 0.5 point difference.
Discussion
We set out to conduct a pilot study to establish the feasibility of using simulation to test the effect of patients’ race and insurer on the quality and content of periviable counseling encounters. Our findings confirm that simulation is a realistic and feasible method for studying the effects of sociodemographic characteristics on periviable counseling. We also identified trends suggesting that SDM may occur differentially based on patients’ race and insurer.
In previous work, we have observed racial differences in periviable resuscitation decisions16 but also found that race was not a predictor of periviable cesarean decisions in the same cohort of infants.36 It is difficult to know whether the observed racial differences in neonatal intubation reflect variations in patient preferences or provider counselling practices, but the fact that resuscitation differed by race, while mode of delivery did not, suggests that the variation may reflect differences in provider practice. Moreover, Marcello et al. found that healthcare providers’ willingness to resuscitate periviable neonates varied based on patients’ sociodemographic characteristics.17 The findings of the present study, while not conclusive, suggest that providers’ practice of SDM may occur differentially based on factors such as patients’ race and insurance payer. We found that SDM scores were consistently higher in interactions with Medicaid-insured black patients. This was somewhat unexpected, as we were initially concerned that physicians might be less likely to engage in SDM among patients who they believed were less capable of understanding the complexity of the decisions. It is possible that based on perceived limitations in patient understanding and/or ability to care for a potentially disabled child, physicians may, in fact, overcompensate--taking extra care to inform and involve such patients. It is plausible that increased SDM could result in more resuscitation attempts. This is particularly true because our SDM scores were driven by informational content more than values elicitation. One could postulate that providing more information and alternatives could result in greater decision fatigue37 or ultimate indecision, which might result in resuscitation by default.30
Our study has notable limitations. As a feasibility pilot study performed in a single academic medical center, the generalizability of our findings is limited. Furthermore, selection bias may be present. Those physicians willing to participate in this study may differ from other physicians in important ways. If our study participants were more comfortable with communication skills or placed higher value on them, our findings might overestimate communication skills and proficiency in SDM among providers. Hawthorne effects and social desirability biases are also a concern given the simulated nature of the study. In an attempt to diminish social desirability bias, we did not disclose the primary aim of the study until after the counseling encounters were completed. As well, the simulated nature of the encounter allowed us to ensure standardization across encounters and manipulate race and insurer independent of one another. These are important strengths of the study design. We also recognize the limitations of selecting insurer as a proxy for socioeconomic status. It is important to note that we selected this independent variable fully aware that Medicaid is solely an indicator of income and does not necessarily convey information about a patient’s occupational or educational status. At the same time ‘Medicaid’ insurance status is readily conflated with the notion of the ‘undeserving poor’,38 and financial concerns are relevant to families and the healthcare system when resuscitation discussions occur.39 Therefore, we believed that insurer was an important and meaningful initial construct to evaluate. Another limitation, due to the small sample size, is that we were not powered for hypothesis testing and findings may be influenced by sampling error and imbalanced randomization. By conducting multiple exploratory tests, we increased type 1 errors. By perfectly counterbalancing race and insurance status, we may have inadvertently introduced a design effect. Specifically, those randomized to the black-Medicaid/white-private condition appear to have been better performers (scores above 7) than those randomized to the white-Medicaid/black-private condition (scores below 7). Thus, as with any small pilot study, our findings should be interpreted cautiously.
In summary, our findings suggest that the degree to which SDM occurs may be influenced by social and financial factors. While we were not powered to detect overall differences across multiple comparisons, we found trends that will need to be studied in larger clinical or simulation-based settings. Because of the logistical, financial, and ethical challenges of prospectively observing periviable doctor-patient interactions ‘in vivo’, along with the difficulty of disentangling the relationships between variables such as race and socioeconomic status in clinical settings, we believe that, with reasonably attainable sample sizes, simulation studies hold promise for improved understanding of this important topic.
Table 1.
Study Population (N=31)
| Percentage | N | |
|---|---|---|
|
| ||
| Age | 44.0 (mean) | 30–69 (range) |
|
| ||
| Years in Practice | 12.2 (mean) | 1.5–40 (range) |
|
| ||
| Specialty | ||
| OB/Gyn Generalist | 38.7 | 12 |
| Maternal Fetal Medicine (MFM) | 6.5 | 2 |
| MFM Fellow | 6.5 | 2 |
| Neonatologist | 29.0 | 9 |
| Neonatology Fellow | 19.3 | 6 |
|
| ||
| Race/Ethnicity | ||
| White | 71.0 | 22 |
| Black | 16.1 | 5 |
| Asian | 9.7 | 3 |
| Biracial or Multiracial | 3.2 | 1 |
|
| ||
| Sex | ||
| Male | 29.0 | 9 |
| Female | 71.0 | 22 |
|
| ||
| Marital Status | ||
| Single, never married | 6.4 | 2 |
| Married or partnered | 83.9 | 26 |
| Divorced or separated | 9.7 | 3 |
|
| ||
| Parenting | ||
| Yes | 77.4 | 24 |
| No | 22.6 | 7 |
|
| ||
| Religious Affiliation | ||
| Catholic or Protestant | 61.3 | 19 |
| Jewish | 3.2 | 1 |
| Hindu, Buddhist, Muslim | 12.9 | 4 |
| Other | 9.7 | 3 |
| None | 12.9 | 4 |
|
| ||
| Ever Sued | ||
| Yes | 45.2 | 14 |
| No | 51.6 | 16 |
| Missing | 3.2 | 1 |
Table 4.
Between Group Comparisons across Treatment Decisions
| Resuscitation | MOD | Steroids | |||||
|---|---|---|---|---|---|---|---|
| Comparison Groups | Mean Diff. | P | Mean Diff. | P | Mean Diff. | P | |
| WM | WP | −0.41 | 0.426 | −1.01 | 0.056 | −0.85 | 0.111 |
| BP | WP | −0.78 | 0.133 | −1.26 | 0.019 | −1.16 | 0.032 |
| BM | WP | 0.38 | 0.338 | 0.02 | 0.960 | 0.27 | 0.520 |
| BP | WM | −0.38 | 0.326 | −0.25 | 0.550 | −0.31 | 0.431 |
| BM | WM | 0.79 | 0.130 | 1.03 | 0.052 | 1.12 | 0.040 |
| BM | BP | 1.17 | .029 | 1.28 | 0.017 | 1.43 | 0.010 |
BM = Black Medicaid, BP = Black Private, WM = White Medicaid, WP= White Private
Summary Statement.
We conducted a pilot study to establish the feasibility of using simulation to test the effect of patients’ race and insurance status on the quality and content of periviable counseling encounters. Our findings confirm that simulation is a feasible method for studying the effects of sociodemographic characteristics on periviable counseling. We also identified trends suggesting that SDM may occur differentially based on patients’ race and insurer. Because of the logistical, financial, and ethical challenges of prospectively observing periviable doctor-patient interactions ‘in vivo,’ along with the difficulty of disentangling the relationships among variables such as race and socioeconomic status in clinical settings, our findings have promise for studying shared decision-in larger simulation-based studies.
Acknowledgments
This publication was made possible in part by Grant Number KL2 TR000163 (A. Shekhar, PI) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award and the Robert Wood Johnson Foundation’s Amos Medical Faculty Development Program. Additional funding came from Indiana University Health Values Grant number VFR-372.
Footnotes
Financial Disclosure Summary
The authors have no financial conflicts of interest to disclose.
References
- 1.Kaempf JW, Tomlinson MW, Campbell B, Ferguson L, Stewart VT. Counseling pregnant women who may deliver extremely premature infants: medical care guidelines, family choices, and neonatal outcomes. Pediatrics. 2009 Jun;123(6):1509–1515. doi: 10.1542/peds.2008-2215. [DOI] [PubMed] [Google Scholar]
- 2.Hintz SR, Kendrick DE, Wilson-Costello DE, et al. Early-childhood neurodevelopmental outcomes are not improving for infants born at <25 weeks’ gestational age. Pediatrics. Jan;127(1):62–70. doi: 10.1542/peds.2010-1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petrou S, Mehta Z, Hockley C, Cook-Mozaffari P, Henderson J, Goldacre M. The impact of preterm birth on hospital inpatient admissions and costs during the first 5 years of life. Pediatrics. 2003 Dec;112(6 Pt 1):1290–1297. doi: 10.1542/peds.112.6.1290. [DOI] [PubMed] [Google Scholar]
- 4.Clements KM, Barfield WD, Ayadi MF, Wilber N. Preterm birth-associated cost of early intervention services: an analysis by gestational age. Pediatrics. 2007 Apr;119(4):e866–874. doi: 10.1542/peds.2006-1729. [DOI] [PubMed] [Google Scholar]
- 5.Gilbert WM, Nesbitt TS, Danielsen B. The cost of prematurity: quantification by gestational age and birth weight. Obstet Gynecol. 2003 Sep;102(3):488–492. doi: 10.1016/s0029-7844(03)00617-3. [DOI] [PubMed] [Google Scholar]
- 6.Martin JA, Kung H-C, Mathews TJ, et al. Annual Summary of Vital Statistics: 2006. Pediatrics. 2008 Apr 1;121(4):788–801. doi: 10.1542/peds.2007-3753. [DOI] [PubMed] [Google Scholar]
- 7.Braddock CH., 3rd Supporting shared decision making when clinical evidence is low. Med Care Res Rev. 2013 Feb;70(1 Suppl):129s–140s. doi: 10.1177/1077558712460280. [DOI] [PubMed] [Google Scholar]
- 8.Committee on Quality of Health Care in America IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: The National Academies Press; 2001. [PubMed] [Google Scholar]
- 9.Barry MJ, Edgman-Levitan S. Shared Decision Making — The Pinnacle of Patient-Centered Care. New England Journal of Medicine. 2012;366(9):780–781. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 10.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango) Social Science & Medicine. 1997;44(5):681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 11.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Social Science & Medicine. 1999;49(5):651–661. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- 12.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-Centered Communication, Ratings of Care, and Concordance of Patient and Physician Race. Annals of Internal Medicine. 2003;139(11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 13.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, Gender, and Partnership in the Patient-Physician Relationship. JAMA. 1999 Aug 11;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 14.Roter DL, Hall JA. Physician Gender and Patient-Centered Communication: A Critical Review of Empirical Research. Annual Review of Public Health. 2004;25(1):497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- 15.Johnson RL, Roter D, Powe NR, Cooper LA. Patient Race/Ethnicity and Quality of Patient-Physician Communication During Medical Visits. Am J Public Health. 2004 Dec 1;94(12):2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tucker Edmonds B, Fager C, Srinivas S, Lorch S. Racial and ethnic differences in use of intubation for periviable neonates. Pediatrics. 2011 May;127(5):e1120–1127. doi: 10.1542/peds.2010-2608. [DOI] [PubMed] [Google Scholar]
- 17.Marcello KR, Stefano JL, Lampron K, Barrington KJ, Mackley AB, Janvier A. The influence of family characteristics on perinatal decision making. Pediatrics. 2011 Apr;127(4):e934–939. doi: 10.1542/peds.2009-3010. [DOI] [PubMed] [Google Scholar]
- 18.Mebane EW, Oman RF, Kroonen LT, Goldstein MK. The influence of physician race, age, and gender on physician attitudes toward advance care directives and preferences for end-of-life decision-making. J Am Geriatr Soc. 1999 May;47(5):579–591. doi: 10.1111/j.1532-5415.1999.tb02573.x. [DOI] [PubMed] [Google Scholar]
- 19.Cohen LL. Racial/ethnic disparities in hospice care: a systematic review. J Palliat Med. 2008 Jun;11(5):763–768. doi: 10.1089/jpm.2007.0216. [DOI] [PubMed] [Google Scholar]
- 20.Smith AK, McCarthy EP, Paulk E, et al. Racial and ethnic differences in advance care planning among patients with cancer: impact of terminal illness acknowledgment, religiousness, and treatment preferences. Journal of Clinical Oncology. 2008 Sep 1;26(25):4131–4137. doi: 10.1200/JCO.2007.14.8452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carrion IV. When do Latinos use hospice services? Studying the utilization of hospice services by Hispanics/Latinos. Soc Work Health Care. Mar;49(3):197–210. doi: 10.1080/00981380903493038. [DOI] [PubMed] [Google Scholar]
- 22.Colon M. Hospice and Latinos: a review of the literature. J Soc Work End Life Palliat Care. 2005;1(2):27–43. doi: 10.1300/J457v01n02_04. [DOI] [PubMed] [Google Scholar]
- 23.Born W, Greiner KA, Sylvia E, Butler J, Ahluwalia JS. Knowledge, attitudes, and beliefs about end-of-life care among inner-city African Americans and Latinos. J Palliat Med. 2004 Apr;7(2):247–256. doi: 10.1089/109662104773709369. [DOI] [PubMed] [Google Scholar]
- 24.Johnson KS, Kuchibhatla M, Tanis D, et al. Racial differences in hospice revocation to pursue aggressive care. Archives of Internal Medicine. 2008 Jan 28;168(2):218–224. doi: 10.1001/archinternmed.2007.36. [DOI] [PubMed] [Google Scholar]
- 25.Ache KA, Shannon RP, Heckman MG, Diehl NN, Willis FB. A Preliminary Study Comparing Attitudes toward Hospice Referral between African American and White American Primary Care Physicians. J Palliat Med. 2011 Feb 5;:5. doi: 10.1089/jpm.2010.0426. [DOI] [PubMed] [Google Scholar]
- 26.Smith AK, Davis RB, Krakauer EL. Differences in the quality of the patient-physician relationship among terminally ill African-American and white patients: impact on advance care planning and treatment preferences. J Gen Intern Med. 2007 Nov;22(11):1579–1582. doi: 10.1007/s11606-007-0370-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Welch LC, Teno JM, Mor V. End-of-life care in black and white: race matters for medical care of dying patients and their families. J Am Geriatr Soc. 2005 Jul;53(7):1145–1153. doi: 10.1111/j.1532-5415.2005.53357.x. [DOI] [PubMed] [Google Scholar]
- 28.Guest G, Bunce A, Johnson L. How Many Interviews Are Enough? Field Methods. 2006 Feb 1;18(1):59–82. [Google Scholar]
- 29.Barnato AE, Mohan D, Downs J, Bryce CL, Angus DC, Arnold RM. A randomized trial of the effect of patient race on physicians’ intensive care unit and life-sustaining treatment decisions for an acutely unstable elder with end-stage cancer. Crit Care Med. 2011 Jul;39(7):1663–1669. doi: 10.1097/CCM.0b013e3182186e98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tucker Edmonds B, Krasny S, Srinivas S, Shea J. Obstetric decision-making and counseling at the limits of viability. Am J Obstet Gynecol. 2012 Mar;206(3):248 e241–245. doi: 10.1016/j.ajog.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 31.Batton B, Burnett C, Verhulst S, Batton D. Extremely preterm infant mortality rates and cesarean deliveries in the United States. Obstetrics and gynecology. 2011 Jul;118(1):43–48. doi: 10.1097/AOG.0b013e318221001c. [DOI] [PubMed] [Google Scholar]
- 32.Braddock CH, 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. Jama. 1999 Dec 22–29;282(24):2313–2320. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- 33.Braddock C, 3rd, Hudak PL, Feldman JJ, Bereknyei S, Frankel RM, Levinson W. “Surgery is certainly one good option”: quality and time-efficiency of informed decision-making in surgery. The Journal of bone and joint surgery. 2008 Sep;90(9):1830–1838. doi: 10.2106/JBJS.G.00840. American volume. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salyers MP, Matthias MS, Fukui S, et al. A coding system to measure elements of shared decision making during psychiatric visits. Psychiatric services (Washington, DC) 2012 Aug;63(8):779–784. doi: 10.1176/appi.ps.201100496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology (Cambridge, Mass) 1990 Jan;1(1):43–46. [PubMed] [Google Scholar]
- 36.Tucker Edmonds B, Fager C, Srinivas S, Lorch S. Predictors of cesarean delivery for periviable neonates. Obstet Gynecol. 2011 Jul;118(1):49–56. doi: 10.1097/AOG.0b013e31821c4071. [DOI] [PubMed] [Google Scholar]
- 37.Baumeister R. The psychology of irrationality: Why people make foolish, self-defeating choices. The psychology of economics decisions. 2003:1. [Google Scholar]
- 38.Stuber J, Kronebusch K. Stigma and other determinants of participation in TANF and Medicaid. Journal of policy analysis and management: [the journal of the Association for Public Policy Analysis and Management] 2004 Summer;23(3):509–530. doi: 10.1002/pam.20024. [DOI] [PubMed] [Google Scholar]
- 39.Boss RD, Hutton N, Sulpar LJ, West AM, Donohue PK. Values Parents Apply to Decision-Making Regarding Delivery Room Resuscitation for High-Risk Newborns. Pediatrics. 2008 Sep 1;122(3):583–589. doi: 10.1542/peds.2007-1972. [DOI] [PubMed] [Google Scholar]


