Abstract
AIM
To characterize the prospective trajectory of parent-reported behavior and social competence problems in children with new or recent onset epilepsy from diagnosis to 5 to 6 years after diagnosis compared to healthy control participants.
METHOD
Thirty-five children (21 males, 14 females; mean age 14y 1mo, SD 3y 4mo, range 8–18y) with new/recent onset idiopathic generalized (IGE) and 34 children with localization-related epilepsies (LRE; 19 males, 15 females; mean age 10y 8mo, SD 2y 2mo, range 8–18y) underwent behavioral assessment (Child Behavior Checklist) at baseline, 2 years, and 5 to 6 years after diagnosis. The assessment comprised summary scales Total Behavior Problems Internalizing Problems, Externalizing Problems, and Total Competence. Sixty-two children with normal development served as comparison participants. Analyses were based on random effects regression modeling comparing trajectories with respect to time since epilepsy diagnosis among groups.
RESULTS
Differences in parent-reported behavioral problems between LRE and IGE groups and healthy comparison participants were detectable at or near the time of diagnosis and remained either stable (competence) or tended to abate (behavior problems) over the ensuing 5 to 6 years without evidence of progressive worsening. These trends were evident for both LRE and IGE groups, with no difference between them.
INTERPRETATION
Behavior and competence problems in children with LRE and IGE epilepsy are not characterized by progressive worsening over a 5- to 6-year period. Behavioral problems are present near the time of diagnosis and tend to abate over time, with competence problems being more persistent across serial assessments, and present in both LRE and IGE groups.
Population-based investigations have demonstrated that behavior problems are over-represented among children and adolescents with epilepsy compared to adolescents with other non-neurological health conditions and adolescents with typical development.1,2 However, much remains to be learned about the natural history of these issues, including when and why they develop and, especially, their course over time.3 To address this point, longitudinal studies of behavioral adjustment beginning at or near the time of epilepsy diagnosis are required.
Clinical investigations have examined children at or near the time of diagnosis, and in some cases before the onset of recurrent seizures. Studies have reported increased behavior problems in adolescents with new onset epilepsy, using observations from parents,4–11 teachers,4,12,13 or parents and children themselves.7,10,14 Additionally, a small number of epidemiological investigations report that antecedent psychiatric disorders constitute a risk factor for the development of later epilepsy.15,16 The findings from these investigations suggest that factors other than recurrent seizures, chronic medication use, or social complications underlie the observed behavioral complications associated with epilepsy.
Controlled longitudinal examinations of the course of behavioral and social complications in children from the time of diagnosis of epilepsy are infrequent. To our knowledge, only two research groups have presented controlled prospective behavioral change data in children with newly diagnosed epilepsy, with end-point assessments ranging from 36 to 42 months after diagnosis.12,17–19 These studies targeted behavioral problems reported by parents and teachers. Areas of competence (e.g. school, social, activities) were not examined. The reported long-term outcomes have been variable, with children with new onset epilepsy continuing to show significant behavioral problems compared to participants with typical development over time (although with considerable individual variability)4,17 or exhibiting abating behavioral difficulties up to 26 months after diagnosis.19 The role of underlying etiology (cryptogenic versus idiopathic)17 and seizure type (partial versus generalized)19 have been examined, but not the contribution of traditionally defined epilepsy syndromes.
In the current study, we report results from a controlled prospective cohort investigation of children with new/recent onset epilepsies, examining parent reports of problematic behavior and social competence over three waves of assessment including at or near the time of epilepsy diagnosis, 2 years later, and then 5 to 6 years after diagnosis. We focus on a comparison of the behavioral and social competence trajectories between children with localization-related (LRE) and idiopathic generalized epilepsies (IGE) healthy comparison participants, given the longstanding interest in the relationship between epilepsy syndrome and neurobehavioral comorbidities including cognition, behavior, and quality of life.3 Based on our prior prospective cognitive investigation,20 we hypothesized that both syndrome groups would exhibit more problematic behavior than comparison participants but would not differ from each another, and the heightened behavioral and social problems in children with epilepsy would not worsen over time.
METHOD
Participants
Sixty-nine children with recent onset epilepsy and 62 healthy first-degree cousin comparison participants were recruited from pediatric neurology clinics at three Midwestern medical centers (University of Wisconsin-Madison, Marshfield Clinic, Dean Clinic). The study group was recruited based on the following inclusion criteria: (1) diagnosis of epilepsy within the past 12 months, (2) no other developmental disability, (3) no other neurological disorder, and (4) normal clinical magnetic resonance imaging (MRI). Each child’s epilepsy syndrome was elucidated and adjudicated in a research consensus meeting by the research pediatric neurologist who reviewed all available clinical data (e.g. seizure description and phenomenology, electroencephalogram, clinical imaging, neurodevelopmental history) while blinded to all research cognitive, behavioral, and neuroimaging data.
First-degree cousins were used as healthy comparison participants and exclusion criteria were as follows: history of (1) classic initial precipitating injuries (e.g. simple or complex febrile seizures), (2) any seizure or seizure-like episode, (3) diagnosed neurological disease,(4) loss of consciousness greater than 5 minutes, or (5) other family history of a first-degree relative with epilepsy or febrile convulsions (see the previously published report for additional details21). We used cousin comparison participants rather than siblings or other potential comparison groups for the following reasons: (1) first-degree cousins are more genetically distant from the participants with epilepsy (one-eighth of shared genes) and thus less pre-disposed than siblings to shared genetic factors that may contribute to anomalies in brain structure and cognition; (2) a greater number of first-degree cousins are available than siblings in the target age range; and (3) the family link was anticipated to facilitate participant recruitment, and especially retention over time (which is our intent) compared to more general control populations (e.g. unrelated school mates). Retention rate (94%) was strong with only 8 of the initial 137 participants lost to follow up across waves 2 and 3 (four children with epilepsy and four control participants). Further details on baseline characteristics are available in an earlier publication from our group.21
Standard protocol approvals and patient consents
This study was reviewed and approved by the institutional review boards of all institutions involved in the study. On the day of study participation, written informed consent was obtained from the parent/legal guardian of the children and adolescents participating in the study, while written informed consent was obtained from research participants aged 18 and over and written informed assent was obtained from research participants aged 8 to 17 years. All procedures were consistent with the Declaration of Helsinki.22 Medical records pertinent to the child’s epilepsy diagnosis and treatment were obtained after signed release of information was garnered from the parent.
Procedures
As part of the study visit, the children underwent neuropsychological assessment, clinical interview, MRI, and questionnaire-based assessments. Each participating child was accompanied to their study visit by a parent who underwent a clinical interview and completed questionnaires characterizing the child’s gestation, delivery, neurodevelopment, and seizure history. Children were seen for three waves of assessment including baseline (wave 1), 2 years later (wave 2), and 5 to 6 years after diagnosis (wave 3).
Parents completed the Child Behavior Checklist (CBCL) for children aged 6 to 18 years (CBCL/6–18) from the Achenbach System of Empirically Based Assessment.23 The primary dependent behavioral variables of interest included the overall CBCL/6–18 summary scales of Total Competence, Problems, Internalizing Problems, and Externalizing Problems. Total Competence scores were reverse coded so that all scale elevations reflected more problematic behavior and lower scores reflected better/less problematic behavior. For readers who would like detailed information pertaining to CBCL reliability, validity, and other information please see http://www.aseba.org/ordering/reliabilityvalidity.html. Cronbach’s alphas were examined for the Internalizing, Externalizing and Total Problems scales and found to be 0.86, 0.92, and 0.96 for epilepsy participants and 0.77, 0.89, and 0.92 for comparison participants. These values are comparable to Achenbach System of Empirically Based Assessment (control) values of 0.90, 0.94, and 0.97, respectively.
Statistical analyses
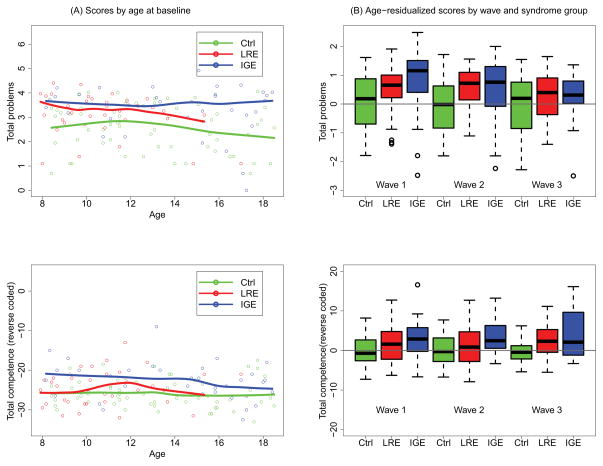
As exploratory analyses compared LRE and IGE epilepsy syndromes to healthy comparison participants for each of the four behavioral scales of interest, the three groups were first compared at baseline (wave 1) by plotting individual test scores against age, including a flexible curve for the mean test score as a function of age.24 These plots served to present the joint distribution of test scores and age at baseline and to display any systematic differences between the three groups across the range of ages of onset (see Fig. 1a). Second, a flexible curve (not shown) for each scale was fitted to the test scores of the healthy control participants as a function of age, aggregating across the three waves, thus providing a reference for removal of normative age effects from test scores in the epilepsy group. Residuals from this model were computed for each group (LRE, IGE, and healthy comparison participants), and the distribution of these residuals was compared via boxplots across the three groups at each of three waves (Fig. 1b), providing an age-adjusted comparative summary of the group differences as a function of number of years after diagnosis.
Figure 1.
Total Problems and Total Competence (reverse coded) by age, wave, and diagnostic group. (a) Scatterplot of scores by age at baseline, with accompanying flexible curve fitted to data, for each of two epilepsy syndrome groups (LRE and IGE) and healthy control participants. (b) Boxplots of age-residualized scores by syndrome group (LRE and IGE versus healthy control) and wave. Comparison participants were used as a reference to compute residuals as explained in the text. The p values for fully adjusted comparisons are given in Table II. Boxplots follow standard statistical practice. Briefly, the top, bottom, and middle of the box represent the third and first quartiles and the median, respectively. The bar at the top of the upper whisker is the largest data point that is within 1.5 times the interquartile range (IQR) from the third quartile, where the IQR is the difference between the third and first quartiles. A symmetric description applies to the bar at the bottom of the lower whisker. The data points outside the whiskers are greater than 1.5 times the IQR from the third or first quartiles, may be considered outliers, and hence are worthy of their own display. Comp., healthy comparison group; IGE, idiopathic generalized epilepsy; LRE, localization-related epilepsy.
Formal analyses were conducted to determine whether there were systematic behavioral differences between the LRE and IGE groups as well as relative to healthy comparison participants at either baseline and/or prospective assessments. Standard growth curve models were specified with fixed effects for age, age-squared, sex, and age-by-sex. The age-squared and the age-by-sex interaction allowed for non-linear relationships between test scores and age and allowed for age effects to differ between males and females. The aim was to thoroughly adjust for effects of age and sex even if they do not operate linearly. The models also included a random intercept and a random slope in age to account for response (behavioral score) trajectories varying from person to person within group. Age at baseline and age at onset were so highly correlated (r=0.97) that it was not necessary or appropriate to include age at onset in the models. Group and group x wave effects were then added into these models, and were tested in three ways. First, in an omnibus test of group differences in overall trajectory, the main effect of (dummy-coded) group and the interaction of group x wave were jointly tested (see Table 2, column 2). This assessed the null hypothesis of no group effect at any time versus the alternative of a group effect at baseline and/or a trend in group differences (i.e. differences in slope) across the three waves of assessment. Second, only if the omnibus test rejected the null hypothesis, post-hoc tests were conducted for group differences at each of three waves of assessment (see Table 2, columns 4–6). This was accomplished by entering a dummy-coded wave into the model as a categorical variable interacted with a group, and then constructing contrasts reflecting group differences at each wave. Finally, again, only if the omnibus test rejected the null hypothesis, a trend test of group x wave interactions was conducted to determine if there were differences in slope among the groups across the three waves (see Table 2, column 7). This test provides further insight into whether omnibus differences reflect relatively constant group differences over time since diagnosis or, alternatively, whether group differences grow or shrink over time. Tests are presented in terms of p values derived from F tests, accompanied by indicators of direction of effect across the three waves.
Table II.
Omnibus tests and post-hoc follow up tests of longitudinal diagnostic and syndrome group differences in four tests
| Response | Omnibusa | Post-hoc p values | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| p | Direction | Baseline | Year 2 | Year 5 | Trend | |
| Total Problems | 0.0003 | IGE = LRE > HC | 0.0005 | 0.0040 | 0.4733 | 0.0277 |
| Total Competence | 0.0013 | IGE = LRE > HC | 0.0105 | 0.0194 | 0.0031 | 0.0615 |
| Internalizing Problems | 0.0025 | IGE = LRE > HC | 0.0013 | 0.0134 | 0.5997 | 0.0820 |
| Externalizing Problems | 0.0274 | IGE = LRE > HC | 0.0177 | 0.1164 | 0.9115 | 0.0530 |
Details and multiple comparison corrections are given in the text.
Critical value for these tests is based on ordered Hochberg correction for multiple comparisons; the largest value is less than 0.05, so all omnibus tests are declared significant. IGE, idiopathic generalized epilepsy; HC, healthy comparison participants; LRE, localization-related epilepsy.
Analyses were repeated for each of the target CBCL variables. Log transformation was used for non-normally distributed measures (Total Problems, Internalizing Problems, and Externalizing Problems). Graphics were prepared in R25 and models were fitted and tested using PROC MIXED in SAS software, version 9.2 (SAS Institute, Cary, NC, USA). Secondary analyses were conducted on the specific (narrow-band) CBCL scales and the results are presented in Figures S1 and S2 (online supporting information).
Multiple comparisons
The analyses described above involved omnibus tests for four behavioral measures. To control family wise or overall type I error rate (alpha=0.05), we used a procedure developed by Hochberg.26 This procedure is more powerful than both the Holm modification to the Bonferroni procedure or the Bonferroni procedure itself.27 Briefly, this procedure puts the four p values in descending order. If the first one is less than 0.05, the entire set of null hypotheses is rejected. If not, we advance to the next test and compare it to alpha=0.05/2, and so on comparing to 0.05/3, 0.05/4 until one test rejects, in which case all subsequent tests (with smaller p values) are also rejected. Having controlled the family-wise error rate for the omnibus test, post-hoc tests for a given outcome are only performed when the omnibus test for that outcome is significant according to this procedure. The results are presented in terms of nominal p values and the table indicates when those p values fall below the Hochberg critical value.
RESULTS
The 131 research participants, aged 8 to 18 years, included 35 adolescents with recent onset LRE epilepsy (21 males, 14 females; mean age 10y 8mo, SD 2y 2mo), 34 with recent onset IGE epilepsy (19 males, 15 females; mean age 14y 1mo, SD 3y 4mo), and 62 healthy comparison participants (28 males, 34 females; mean age 13y, SD 3y; Table I). Participants with IGE had later ages at epilepsy onset and therefore, as result of the design, were older than participants with LRE, with comparison participants falling in between the two epilepsy groups. Participants with epilepsy were more predominantly male relative to comparison participants. Participants with LRE were less likely to be on antiepileptic drugs at baseline than participants with IGE. At baseline, 5 of the 69 children with epilepsy had repeated a grade (7%) versus 1 of the 62 healthy comparison participants (2%). Thus, the vast majority of children (93% of epilepsy group and 98% of comparison group) were in the appropriate grade for age. A small number of children with epilepsy were not taking antiepileptic drugs either because the child’s parents elected not to initiate medications and/or the treating child neurologist elected not to start medication (e.g. in cases of benign epilepsy with centrotemporal spikes).
Table I.
Baseline demographic and clinical characteristics of the participants with epilepsy and the comparison participants without epilepsy
| Variables | LRE (n=35) | IGE (n= 34) | Comparison group (n=62) |
|---|---|---|---|
| Age (mean/SD, y) | 10.8 (2.2) | 14.1 (3.4) | 13.0 (3.0) |
| Seizure duration mean (SD) mo | 7.7 (3.7) | 8.6 (3.6) | – |
| Age at onset mean (SD), y | 9.8 (2.4) | 13.2 (3.5) | – |
| Sex Male/Female | 21/14 | 19/15 | 28/34 |
| Antiepileptic drugs (polytherapy/monotherapy/none) | 0 / 23 / 12 | 3/ 31 /0 |
Localization-related epilepsy (LRE) participants comprised 16 children with benign epilepsy with centrotemporal spikes, seven with temporal lobe epilepsy, and 12 with focal seizures not otherwise specified (NOS); Idiopathic generalized epilepsy (IGE) participants comprised 22 children with juvenile myoclonic epilepsy, 11 with absence, 1 with IGE NOS.
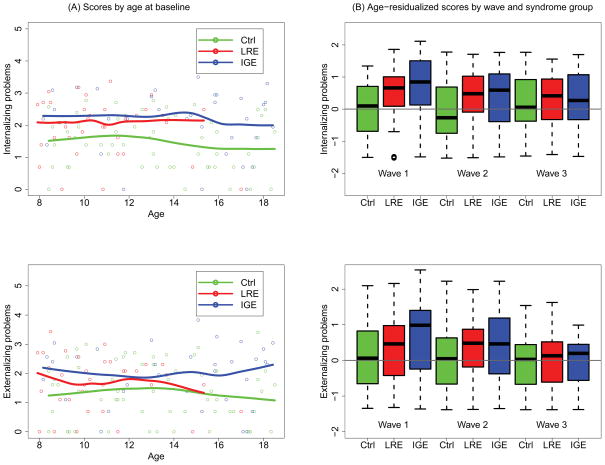
Scatterplots and flexible curve fits for all four measures depict patterns of no age effect and of greater impairment at baseline in the LRE versus healthy comparison participants and in the LRE versus IGE groups (Figs Ia and IIa). The plots also show good coverage across the younger age range for all three groups; however, for the LRE group, there is weak representation in the older ages.
Figure 2.
Internalizing Problems and Externalizing Problems by age, wave, and diagnostic group. (a) Scatterplot of scores by age at baseline, with accompanying flexible curve fitted to data, for each of two epilepsy syndrome groups (LRE and IGE) and healthy control participants. (b) Boxplots of age-residualized scores by syndrome group (LRE and IGE versus healthy control) and wave. See Figure 1 for interpretation. Ctrl, Healthy control group; LRE, localization-related epilepsy; IGE, idiopathic generalized epilepsy.
There were significant differences by omnibus test among the three groups (LRE, IGE, and healthy comparison participants) across time in measures of Total Problems, Internalizing Problems, Externalizing Problems, and Total Competence (Table II).
Total Problems, Internalizing Problems, and Externalizing Problems showed strong group differences at baseline with LRE and IGE showing greater impairment than healthy comparison participants (Figs Ib and IIb). These differences declined over time (trend p values all italic>0.1), with non-significant group effects in Externalizing Problems by year 2, and no significant group effects across these scales at year 5 (Table II, columns 4 to 7). Total Competence was significantly different and in the same direction comparing LRE, IGE, and healthy comparison groups across all three waves of testing, although differences between LRE and IGE groups were reduced by wave 3 relative to baseline (trend p value = 0.06).
Table SI and Figure S1 (online supporting information) summarize the results of secondary analyses for the narrow-band CBCL scales. No scale showed worsening of behavioral abnormalities relative to healthy comparison participants over time; most scales showed significant differences at baseline with weakened effects by wave 3. Persisting epilepsy effects (regardless of syndrome) were seen for the School and Attention Problems scales. Only Social Problems showed a markedly different pattern. Here, at baseline the IGE group was impaired relative to the LRE and healthy comparison groups, which were indistinguishable. By wave 3, the LRE and IGE groups were similarly impaired relative to healthy comparison participants.
DISCUSSION
Three primary findings were identified in this investigation. First, using the parent-completed CBCL as the measure of problem behavior and social competence, differences between the comparison and epilepsy groups were apparent at baseline. Second, there was no evidence of progression of behavioral and competence problems over serial waves of assessment. In fact, there were few persisting significant differences in behavioral problems at 5 to 6 years post-diagnosis, but there were persisting deficits in social competence in the two epilepsy groups. Third, there were weak, if any, syndrome-specific differences on the behavioral and competence measures at baseline as well as at assessment waves at 2 years and 5 to 6 years post-diagnosis. Overall, our hypotheses regarding the lack of progression/worsening of behavioral problems and minimal effects associated with seizure syndrome were supported. These findings are discussed below.
Baseline behavior and competence findings
At baseline, there were significant group differences across CBCL measures of Total Problems, Internalizing Problems, Externalizing Problems, and Total Competence, with the epilepsy groups exhibiting more problems and less competence compared to healthy comparison participants. These findings are consistent with the small number of earlier CBCL studies of new onset childhood epilepsy.4,8 The results are also consistent with findings from other controlled investigations using other measures of behavioral adjustment including the teacher report version of the CBCL.4,6,7,9,13,14 Thus, this appears to be a reliable and robust finding.
Behavioral and competence problems over time
Our cohort was seen and evaluated across three assessment waves including at or near the time of diagnosis of epilepsy (baseline), at 2 years, and then 5–6 years after diagnosis. There was no evidence of significant worsening of behavior problems over time; in fact, there were no significant group differences between the epilepsy and comparison groups at long-term follow up (5–6 years after diagnosis), although very mild differences were suggested. These findings are consistent with previous findings, as neither Oostrom et al.17 nor Austin et al.19 reported progressive behavioral difficulties. However, our results are most consistent with Austin et al.19 who also reported an overall trend of declining behavioral problems in the children with new onset epilepsy over time. We observed this to be the case for Total Behavioral Problems as well as the Internalizing and Externalizing scales. However, Total Competence continued to exhibit a significant effect across all time points up to 5 to 6 years post-diagnosis assessment, with more competence problems exhibited by the epilepsy groups (both LRE and IGE) compared to comparison participants, representing the most persistent abnormality. Social skills deficits can have long-term effects on the development and maintenance of interpersonal relationships, social acceptance, and mental health, and there is evidence to support the long-term implications of social skills’ deficits in epilepsy and their potential contributions to poor long-term psychosocial outcomes in adulthood.25 These findings extend our reported baseline CBCL findings,28 indicating that early behavior and social problems do not worsen over time.
The persisting effect of epilepsy for school and attention problems is expected. We have found that the cognitive problems that underlie academic achievement difficulties are stable over time, neither worsening nor improving,20 and our result of persisting school problems is consistent with those findings. Similarly, the persisting parental reports of attention problems is in agreement with the elevated rate of attention-deficit–hyperactivity disorder diagnoses in the children with epilepsy.7 These ongoing school and attention problems should be of clinical concern given their potential and likely impact on future vocational, financial, and quality of life trajectories.3
Impact of seizure syndrome
This investigation also inquired into the possible impact of epilepsy syndrome on the nature and course of behavior and competence limitations. The results were consistent in that the LRE and IGE groups were comparable in their differences from comparison participants at baseline and over time without a clear or unique syndrome-specific relationship to behavior or competence problems. In addition, secondary exploratory analyses of the CBCL narrow-band scales comprising the Total Competence and Total Problems scales were congruent with the effects described above in that abnormalities, when present, were evident at baseline, did not worsen over time with the group effects weakening and often dissipating by the 5 to 6 year follow up, and with minimal association of problems with specific syndrome type (see Table SI and Fig. S1).
Limitations
Several limitations are associated with this investigation. First, we used only the parent report version of the CBCL, the predominant method of investigation in this literature. In the future it would be useful to incorporate reports from teachers as well as the child self-report to assess the consistency and generalizability of these findings. Second, the patterns of results presented here apply just to the CBCL. It is possible that other behavioral measures, such as formal psychiatric diagnoses derived through structured interview procedures (e.g. Kiddie-Schedule for Affective Disorders and Schizophrenia - Present and Lifetime version),29 might reveal somewhat different syndrome separation and time course, and should, therefore, be investigated. Third, we examined only the broad effects of LRE and IGE. It is possible that there may be detectable variation among specific LRE and IGE syndromes, but this remains to be addressed in the future. Fourth, the questions regarding the children’s gestation and delivery, assessed at the baseline evaluation, contain the potential for error and recall bias associated with parent reporting, especially for older children. Fifth, there is weak representation in the older ages for the LRE group, so that conclusions at older ages only apply to the IGE versus comparison participants. Finally, cautions have been raised regarding the validity of some specific CBCL items and scales in children with chronic illness (including epilepsy),30,31 cautions that are generally important and pertain to many self-report measures when applied to medical and neurological groups (e.g. use of the Minnesota Multiphasic Personality Inventory with epilepsy, general neurological, and even general medical patients;32,33 self-report depression measures where antiepileptic drug effects can influence test scores).34 That said, there is reassuring evidence regarding the use and validity of the CBCL in childhood epilepsy.35
CONCLUSION
The childhood epilepsies investigated here are characterized by early (near onset and diagnosis) behavioral and competence abnormalities that do not worsen over time, either remaining stable (competence) or abating to control levels (behavioral problems) up to 6 years post-diagnosis, with minor epilepsy syndrome (LRE versus IGE) effects. Our results, and the results of others, indicate that behavioral, cognitive and academic issues may be evident at the time, and sometimes antecedent to, the first recognized seizure and diagnosis and are not necessarily caused by epilepsy chronicity. These children do not necessarily get worse; however, some problems (e.g. social competence, school problems, attention problems) do not resolve and thereby require assessment and intervention early in the course of the child’s epilepsy in order to improve the quality of life and poor psychosocial outcomes that have been documented to follow these individuals into adulthood.3
Supplementary Material
Eleven cognitive–behavioral tests by age, wave, and diagnostic group. (a) Scatterplot of scores by age at baseline, with accompanying flexible curve fitted to data, for each of two epilepsy syndrome groups (LRE and IGE) and healthy controls. (b) Boxplots of age-residualized scores by syndrome group (LRE and IGE versus healthy comparison) and wave. Controls were used as a reference to compute residuals as explained in the text. The p values for fully adjusted comparisons are given in Table SI.
Note: Boxplots follow standard statistical practice. Briefly, the top, bottom, and middle of the box represent the third and first quartiles and the median respectively. The bar at the top of the upper whisker is the largest data point that is within 1.5 times the interquartile range (IQR) from the third quartile, where the IQR is the difference between the third and first quartiles. A symmetric description applies to the bar at the bottom of the lower whisker. The data points outside the whiskers are greater than 1.5 times the IQR from the third or first quartiles, may be considered outliers, and hence are worthy of their own display.
Ctrl, Healthy control group; IGE, idiopathic generalized epilepsy; LRE, localization-related epilepsy.
Omnibus tests and post hoc follow up tests of longitudinal diagnostic and syndrome group differences in 11 tests
What this paper adds.
Problems in behavior and competence are a recognized comorbidity of childhood epilepsy.
There is limited information regarding their natural history.
Behavior problems are evident at/near the time of diagnosis and are attenuated 5 to 6 years after diagnosis.
Competence problems persist across all waves of assessment.
There is no difference in these findings between LRE and IGE.
Acknowledgments
All phases of this study were supported by NINDS 3RO1-44351 and by the Clinical and Translational Science Award (CTSA) program through the NIH Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. The funding source was not involved in study design, data collection, analysis or manuscript preparation. We thank Raj Sheth MD and Monica Koehn MD for study participation and subject recruitment. Also greatly appreciated are Dace Almane, Melissa Hanson, Kate Young, and Bjorn Hanson for overall study coordination, participant recruitment, cognitive assessment, and data management.
ABBREVIATIONS
- CBCL
Child Behavior Checklist
- IGE
Idiopathic generalized epilepsy
- LRE
Localization-related epilepsy
Footnotes
The authors have stated that they had no interests that might be perceived as posing a conflict or bias
Additional supporting information may be found in the online version of this article:
References
- 1.Rutter M, Graham P, Yule W. A Neuropsychiatric Study in Childhood. London: S.I.M.P./William Heineman Medical Books; 1970. [Google Scholar]
- 2.Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics. 2012;129:256–64. doi: 10.1542/peds.2010-1371. [DOI] [PubMed] [Google Scholar]
- 3.Lin JJ, Mula M, Hermann BP. Uncovering the neurobehavioural comorbidities of epilepsy over the lifespan. Lancet. 2012;380:1180–92. doi: 10.1016/S0140-6736(12)61455-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oostrom KJ, Smeets-Schouten A, Kruitwagen CL, Peters AC, Jennekens-Schinkel A. Not only a matter of epilepsy: early problems of cognition and behavior in children with “epilepsy only”--a prospective, longitudinal, controlled study starting at diagnosis. Pediatrics. 2003;112:1338–44. doi: 10.1542/peds.112.6.1338. [DOI] [PubMed] [Google Scholar]
- 5.Austin JK, Risinger MW, Beckett LA. Correlates of behavior problems in children with epilepsy. Epilepsia. 1992;33:1115–22. doi: 10.1111/j.1528-1157.1992.tb01768.x. [DOI] [PubMed] [Google Scholar]
- 6.Hoare P. The development of psychiatric disorder among schoolchildren with epilepsy. Dev Med Child Neurol. 1984;26:3–13. doi: 10.1111/j.1469-8749.1984.tb04399.x. [DOI] [PubMed] [Google Scholar]
- 7.Jones JE, Watson R, Sheth R, et al. Psychiatric comorbidity in children with new onset epilepsy. Dev Med Child Neurol. 2007;49:493–7. doi: 10.1111/j.1469-8749.2007.00493.x. [DOI] [PubMed] [Google Scholar]
- 8.Austin JK, Harezlak J, Dunn DW, Huster GA, Rose DF, Ambrosius WT. Behavior problems in children before first recognized seizures. Pediatrics. 2001;107:115–22. doi: 10.1542/peds.107.1.115. [DOI] [PubMed] [Google Scholar]
- 9.Dunn DW, Austin JK, Huster GA. Behaviour problems in children with new-onset epilepsy. Seizure. 1997;6:283–7. [PubMed] [Google Scholar]
- 10.Bhise VV, Burack GD, Mandelbaum DE. Baseline cognition, behavior, and motor skills in children with new-onset, idiopathic epilepsy. Dev Med Child Neurol. 2010;52:22–6. doi: 10.1111/j.1469-8749.2009.03404.x. [DOI] [PubMed] [Google Scholar]
- 11.Samaitiene R, Norkuniene J, Jurkeviciene G, Grikiniene J. Behavioral problems in children with benign childhood epilepsy with centrotemporal spikes treated and untreated with antiepileptic drugs. Medicina. 2012;48:338–44. [PubMed] [Google Scholar]
- 12.Dunn DW, Austin JK, Caffrey HM, Perkins SM. A prospective study of teachers’ ratings of behavior problems in children with new-onset seizures. Epilepsy Behav. 2003;4:26–35. doi: 10.1016/s1525-5050(02)00642-x. [DOI] [PubMed] [Google Scholar]
- 13.Dunn DW, Harezlak J, Ambrosius WT, Austin JK, Hale B. Teacher assessment of behaviour in children with new-onset seizures. Seizure. 2002;11:169–75. doi: 10.1053/seiz.2001.0612. [DOI] [PubMed] [Google Scholar]
- 14.Taylor J, Jacoby A, Baker GA, Marson AG. Self-reported and parent-reported quality of life of children and adolescents with new-onset epilepsy. Epilepsia. 2011;52:1489–98. doi: 10.1111/j.1528-1167.2011.03094.x. [DOI] [PubMed] [Google Scholar]
- 15.Hesdorffer DC, Ludvigsson P, Olafsson E, Gudmundsson G, Kjartansson O, Hauser WA. ADHD as a risk factor for incident unprovoked seizures and epilepsy in children. Arch Gen Psychiatry. 2004;61:731–6. doi: 10.1001/archpsyc.61.7.731. [DOI] [PubMed] [Google Scholar]
- 16.McAfee AT, Chilcott KE, Johannes CB, Hornbuckle K, Hauser WA, Walker AM. The incidence of first provoked and unprovoked seizure in pediatric patients with and without psychiatric diagnoses. Epilepsia. 2007;48:1075–82. doi: 10.1111/j.1528-1167.2007.01108.x. [DOI] [PubMed] [Google Scholar]
- 17.Oostrom KJ, Schouten A, Kruitwagen CL, Peters AC, Jennekens-Schinkel A. Behavioral problems in children with newly diagnosed idiopathic or cryptogenic epilepsy attending normal schools are in majority not persistent. Epilepsia. 2003;44:97–106. doi: 10.1046/j.1528-1157.2003.18202.x. [DOI] [PubMed] [Google Scholar]
- 18.Oostrom KJ, van Teeseling H, Smeets-Schouten A, Peters AC, Jennekens-Schinkel A Dutch Study of Epilepsy in Childhood (DuSECh) Three to four years after diagnosis: cognition and behaviour in children with ‘epilepsy only’. A prospective, controlled study. Brain. 2005;128:1546–55. doi: 10.1093/brain/awh494. [DOI] [PubMed] [Google Scholar]
- 19.Austin JK, Perkins SM, Johnson CS, et al. Behavior problems in children at time of first recognized seizure and changes over the following 3 years. Epilepsy Behav. 2011;21:373–81. doi: 10.1016/j.yebeh.2011.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rathouz P, Zhao Q, Jones JE, et al. Cognitive development in children with new onset epilepsy. Dev Med Child Neurol. doi: 10.1111/dmcn.12432. published online 21 March 2014. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hermann B, Jones J, Sheth R, Dow C, Koehn M, Seidenberg M. Children with new-onset epilepsy: neuropsychological status and brain structure. Brain. 2006;129:2609–19. doi: 10.1093/brain/awl196. [DOI] [PubMed] [Google Scholar]
- 22.World Medical Association. World Medical Association Declaration of Helsinki. J Law Med Ethics. 1991;19:264–5. [PubMed] [Google Scholar]
- 23.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth and Families; 2001. [Google Scholar]
- 24.Hastie TJ, Tibshirani RJ. Generalized Additive Models. 1. London: Chapman & Hall/CRC Press; 1990. [Google Scholar]
- 25.Team RDC. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2010. [Google Scholar]
- 26.Hochberg Y. A sharper Bonferroni procedure for multiple test of significance. Biometrika. 1998;75:800–2. [Google Scholar]
- 27.Sankoh AJ, Huque MF, Dubey SD. Some comments on frequently used multiple endpoint adjustment methods in clinical trials. Stat Med. 1997;16:2529–42. doi: 10.1002/(sici)1097-0258(19971130)16:22<2529::aid-sim692>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 28.Almane D, Jones JE, Jackson DC, Seidenberg M, Hermann BP. The social competence and behavioral problem substrate of new- and recent-onset childhood epilepsy. Epilepsy Behav. 2014;31:91–6. doi: 10.1016/j.yebeh.2013.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaufman J, Birmaher B, Brent D, Rao U. Schedule for Affective Disorders and Schizophrenia for School-age Children—Present and Lifetime version (K-SADS-PL):initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–8. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 30.Perrin EC, Stein RE, Drotar D. Cautions in using the Child Behavior Checklist: observations based on research about children with a chronic illness. J Pediatr Psychol. 1991;16:411–21. doi: 10.1093/jpepsy/16.4.411. [DOI] [PubMed] [Google Scholar]
- 31.Ferro MA, Boyle MH, Scott JG, Dingle K. The child behavior checklist and youth self- report in adolescents with epilepsy: testing measurement invariance of the attention and thought problems subscales. Epilepsy Behav. 2014;31:34–42. doi: 10.1016/j.yebeh.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 32.Dikmen S, Hermann BP, Wilensky A, Rainwater G. Validity of the MMPI to psychopathology in epilepsy. J Nerv Ment Dis. 1983;171:114–122. doi: 10.1097/00005053-198302000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Swenson W. An MMPI Source Book; Basic Item, Scale, and Pattern Data on 50,000 Medical Patients. Minneapolis, MN: University of Minnesota Press; 1973. [Google Scholar]
- 34.Gilliam F, Barry JB, Hermann BP, Meador KJ, Vahle V, Kanner A. Rapid detection of major depression in epilepsy: a multicentre study. Lancet Neurol. 2006;5:399–405. doi: 10.1016/S1474-4422(06)70415-X. [DOI] [PubMed] [Google Scholar]
- 35.Gleissner U, Fritz NE, Von Lehe M, Sassen R, Elger CE, Helmstaedter C. The validity of the Child Behavior Checklist for children with epilepsy. Epilepsy Behav. 2008;12:276–80. doi: 10.1016/j.yebeh.2007.10.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Eleven cognitive–behavioral tests by age, wave, and diagnostic group. (a) Scatterplot of scores by age at baseline, with accompanying flexible curve fitted to data, for each of two epilepsy syndrome groups (LRE and IGE) and healthy controls. (b) Boxplots of age-residualized scores by syndrome group (LRE and IGE versus healthy comparison) and wave. Controls were used as a reference to compute residuals as explained in the text. The p values for fully adjusted comparisons are given in Table SI.
Note: Boxplots follow standard statistical practice. Briefly, the top, bottom, and middle of the box represent the third and first quartiles and the median respectively. The bar at the top of the upper whisker is the largest data point that is within 1.5 times the interquartile range (IQR) from the third quartile, where the IQR is the difference between the third and first quartiles. A symmetric description applies to the bar at the bottom of the lower whisker. The data points outside the whiskers are greater than 1.5 times the IQR from the third or first quartiles, may be considered outliers, and hence are worthy of their own display.
Ctrl, Healthy control group; IGE, idiopathic generalized epilepsy; LRE, localization-related epilepsy.
Omnibus tests and post hoc follow up tests of longitudinal diagnostic and syndrome group differences in 11 tests