Abstract
Non-invasive bioengineering technologies continuously discovered and developed in recent decades provide a significant input to research development and remarkably contribute to the improvement of medical education and care to our patients.
Aim:
Assessing skin hydration by using the capacitance method for a group of patients with allergic contact dermatitis versus healthy subjects, before and after applying a moisturiser (assessing the immediate and long-term effectiveness of hydration).
Results:
For both groups, but especially for the patients with dry skin, there was a clear improvement of hydration, statistically significant after applying the moisturiser. In the case of the patients with allergic contact dermatitis, hydration was at a maximum immediately after the first application, and then maintained an increased level after 7 and 28 days, respectively. In the healthy subjects, the increase in hydration was lower, but progressive. The moisturiser determined an increase in hydration for all age groups, but those who showed the most obvious effect were the young adults (18-29 years old) with an increase of 19.9%.
The maintenance effect of hydration lasted for 28 days, while the improvement was important for allergic skin (17.1%) and significant for healthy skin (10.9%).
Conclusion:
The assessment of epidermal hydration performed by using the corneometer showed very good hydration of the stratum corneum for both groups studied, with immediate and long-term effect. This study also showed that the degree of skin hydration was inversely proportional with age. The corneometer is easy to use, efficient and widely utilised in international studies for measurements in healthy or pathological conditions, for quantitative assessment of the effectiveness of various preparations intended for application to the skin surface, under well-controlled and standardised conditions.
Keywords: corneometer, degree of hydration, capacitance, allergic contact dermatitis
INTRODUCTION
Non-invasive bioengineering technologies continuously discovered and developed in recent decades provide a significant input in dermatology and also have great potential for research development, medical education and patient care.
The study we present aims at following the assessment of an important skin parameter: the degree of skin hydration. This indicator was determined for a group of patients with allergic contact dermatitis, the chronic form, versus a control group of healthy individuals. We also wanted to assess the changes in the skin, using the same indicator above, after applying a moisturiser to both groups, while demonstrating the effectiveness of this moisturiser for both healthy and unhealthy skin. ❑
MATERIALS AND METHODS
This experimental prospective controlled non-invasive study (control group) was performed over a period of 3 years (March 2010–March 2013), on a group of 44 patients diagnosed with allergic contact dermatitis, the chronic type, with recurrent episodes, and on another group of 44 healthy subjects.
Both groups of patients signed informed consent sheets and the patients were subject to a thorough case history and a careful clinical examination.
The inclusion criteria were the following:
subjects aged between 18 and 70;
patients with contact dermatitis who had their allergic condition confirmed by previous epicutaneous tests positive for certain allergens (patch test);
during the study other topical or systemic treatments were excluded, with the exception of the application of the moisturisers in the study;
all the subjects were carefully selected, were cooperative, discerning and able to follow instructions and comply with the study requirements.
The exclusion criteria taken into account were the following:
known history of allergy to the ingredients contained in the composition of the cream tested;
pregnant female patients, nursing mothers or those under treatment with oral contraceptives;
recent vaccinations, 2 weeks prior to the commencement of the study;
recent dermo-cosmetic or aesthetic treatments, 2 months prior to the commencement of the study (dermabrasion, peeling, laser therapy, IPL, botulinum toxin or filler injections);
recent (one month prior to the study) and intense exposure to ultraviolet radiation (sun/tanning beds).
The measurements were carried out using a multiple probe for skin measurements, made by Courage-Khazaka Electronic GmbH in Germany, under standard conditions of temperature and humidity (T° = 20-22°C, humidity 40-60%) and after a rest period of 15-20 minutes for each subject tested. In order to determine the hydration, the capacitance method was used with the help of the Corneometer CM 825.
The study aimed at conducting an instrumental assessment of the degree of hydration for each of the two groups, at the middle third of the forearm, on the front side. The measurements were carried out before and after applying a moisturiser. After using the cream the hydration was assessed again, this time in dynamic, at certain time intervals.
Results are presented as the mean ± SD for a Gaussian distribution and as the median and 25th- to 75th-percentile values for a non-Gaussian distribution and counts.
We use the Mann-Whitney U test or unpaired Student t test if data were continuous and independents and for paired data we use the Paired Student's t-test. The Pearson's correlation coefficient was used to assess correlation between the continuous variable. For all tests, significance was achieved at p < 0.05. Statistical tests were performed using SPSS software (version 15).
Assessment of skin hydration
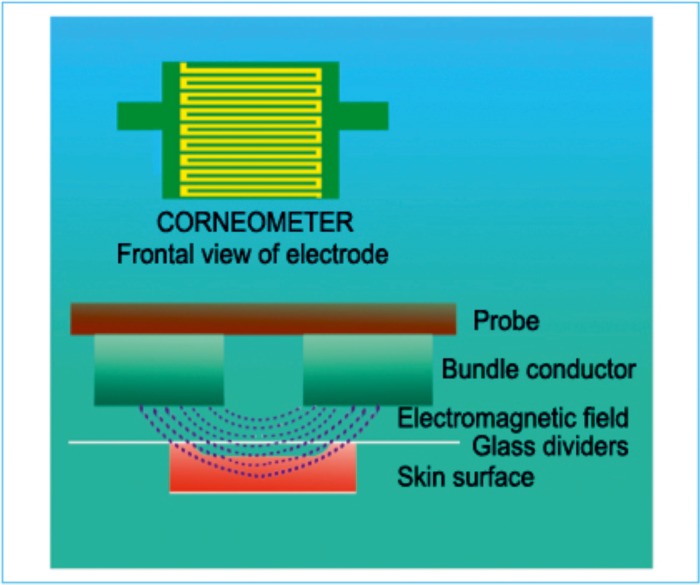
The electrical properties of the skin are dependent on the water content of the stratum corneum of the epidermis. Epidermal hydration was assessed for both groups by measuring the electrical capacitance with the help of the Corneometer CM 825. The principle of the method is based on the difference between the dielectric constant of water (81) and other substances by measuring the capacitance of a dielectric medium. Any change in the dielectric constant subsequent to the variation in skin surface hydration leads to an impaired calculated capacitance of a capacitor. The Corneometer contains two electrodes with different electrical charges that form an electromagnetic field that determines the dielectricity of the stratum corneum. The depth of measurement is low (the first 10-20 µm of the stratum corneum) due to the construction of the measuring head (Figure 1).
Figure 1. Principle of the corneometer.
The range of variation of the values of skin hydration degree is between 0-130 arbitrary units (AU). In standard working conditions (T°= 20-22°C, humidity 40-60%), the variations of the values of skin hydration degree for the middle area of the front side of the forearm are the following: under 30 AU – very dry, between 30 and 45 AU – dry, 45 AU – sufficiently hydrated.
The advantages of this method are: very short measurement time (one second), high reproducibility of measurements and lack of galvanic contact between the measured area and the measuring apparatus (the results obtained are not influenced by ion conductivity or polarisation effects). In addition, the modern electronics of the probe enables temperature stability and excludes the interference of the base capacity and any power supply fluctuations. Compared to other methods, the preparations applied to the skin exert very little influence on the measurements, while being able to detect the slightest changes in the hydration level.
The key therapy for the treatment of allergic contact dermatitis is the application of emollients (moisturisers). A moisturising cream was applied twice a day (in the morning and in the evening) to the patients of both groups, for 28 days. The composition thereof included: active principles (bisabolol, panthenol, tocopheryl acetate, prunus amygdalus dulcis oil), emollients (paraffin, isopropyl myristate, petrolatum, cetyl alcohol, cera alba), humectants (glycerin, urea, sodium lactate), emulsifiers (glyceryl monostearate, PEG 100 stearate, palmitic stearic acid), stabilisers, pH adjusters, curing agents, all in a carrier represented by water.
The analysis conducted followed the described parameter values at baseline time (T0) before using the cream, one hour after the first application of the emollient - T1h, 7 days after the application – T7d and 28 days after the application – T28d. ❑
RESULTS
Originally equal in number (44 subjects), the two groups later included 81 patients, predominantly female (85.18%), almost evenly distributed across the 3 age groups (the majority in the group aged 50-70 – 34.57%). Female preponderance may be justified by their higher interest, by their desire to have a smoother skin without the discomfort caused by the need to apply the moisturising cream.
Assessment of skin hydration in the chronic contact dermatitis group versus healthy subjects
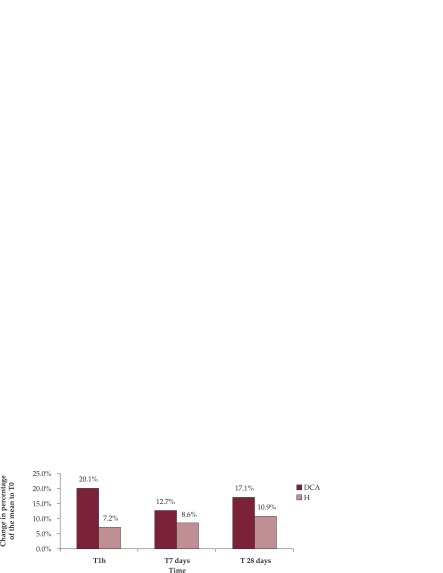
In both groups there was a clear improvement in hydration, highly statistically significant (p = 0.000). In the group of patients with allergic contact dermatitis such increase was even more evident compared to the baseline time T0, versus the group of healthy subjects. This group experienced an improvement in hydration, which reached the maximum level (20.1% compared to T0) immediately after the application of the moisturising cream (after one hour – T1h), followed by a slightly smaller increase after 7 days (12.7% compared to T0) and after 28 days respectively (17.1% compared to T0). In the control group there was also a gradual increase in hydration (reaching the maximum level after 28 days – 10.9% compared to T0), but it was much lower than in the patients with allergic dermatitis. Such dynamics is normal for dry, altered skin as is the case of allergic contact dermatitis. The maintenance effect of hydration may be noticed on the 28th day of application of the moisturiser (it is general knowledge that 28 days is the average human cell renewal period), and the improvement is important for allergic skin (17.1%) and significant respectively for healthy skin (10.9%) (Figure 2).
Figure 2. Assessment of hydration in dynamics on the 2 groups.
Mann-Whitney, Student T, p = 0.000
Comparative assessment of hydration in different age groups
Regarding the analysis of the degree of hydration in the three age groups, the assessments carried out using the corneometer show for young adults, aged 18-29, a dynamics similar to the entire group: the healthy subjects experienced a progressive increase (7.5% after one hour, 8.4% after 7 days and 10.9% after 28 days; for the patients with dermatitis there was a maximum increase immediately after one hour (21.4%), followed by a slight decrease after 7 days (12.0%) and a new increase after 28 days (19.9%) (Figure 3).
Figure 3. Assessment of hydration for 18-29 year group.
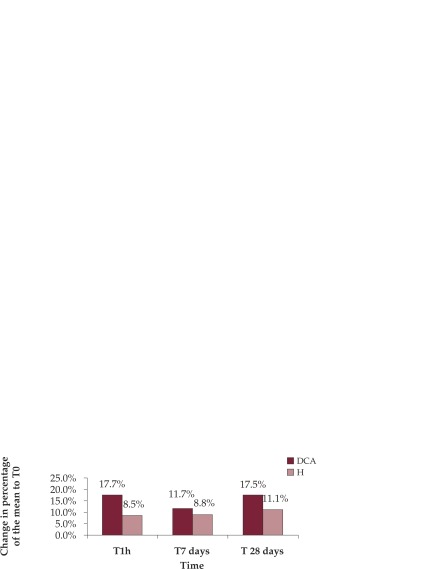
For the group aged 30-49 (Figure 4), the corneometer showed a maximum hydration after one hour from the application of the cream to the patients with dermatitis (17.7%), but lower compared to the previous group, followed by a decrease in hydration (11.7% compared to T0) and a recovery almost equal to the initial value (17.5%). For the group of healthy subjects, hydration improvement followed an upward trend as in the previous cases, but the increase was slightly higher (8.5% after one hour, 8.8% after 7 days and 11.1% after 28 days).
Figure 4. Assessment of hydration for 30-49 year group.
The last age group, 50-70 years, (Figure 5) benefited from effective hydration of the stratum corneum for both types of subjects as follows: for the healthy subjects, the hydration degree increased progressively as in the other age groups described above, but the increase was slightly lower (5.6% after one hour, 8.5% after 7 days and 10.7% after 28 days); for the patients with dermatitis there was a significant increase, which reached its maximum immediately after the application of the moisturiser (21.8% after one hour), followed by a decrease in values over time (14.4% after 7 days and 13.9% after 28 days).
Figure 5. Assessment of hydration for 50-70 year group.
The graphical representation below (Figure 6) shows on an overall basis the hydration degree for the two groups, at the 4 time points, using in this case the average values of the results rendered by the corneometer. First we notice that initially, without treatment, the hydration of the patients with contact dermatitis is much lower than that of the control group. After applying the moisturiser a continuous progressive increase in the degree of hydration may be observed for the group of healthy subjects, while for the other group the increase is discontinuous, reaching its maximum at T0, immediately after applying the cream and providing a very good hydration effect after 7 and after 28 days respectively. ❑
Figure 6. Overall assessment of the degree of hydration.
Mann-Whitney, Student T, p = 0.000
DISCUSSIONS
The smooth, well hydrated aspect of a healthy skin compared to a dry skin, the flexibility of the skin compared to accelerated skin peeling and the formation of an intact and functional barrier, all these necessarily require the existence of an appropriate amount of water in the stratum corneum of the epidermis. Studies in the literature (1-3) repeatedly confirm the positive physiological effect of moisturising preparations on the skin, in dry skin conditions. The connection between the electrical properties of the skin and the water contained in the state corneum is also known (4,5).
The assessment of skin hydration by using the corneometer showed a very good hydration of the stratum corneum for both groups studied after the application of the moisturiser twice a day, for 28 days. Initially, at T0 at which the measurements were made on the untreated skin of both groups, it was noticed that the patients with dermatitis had significantly lower hydration values than the healthy subjects. Such results confirm the data in the literature (5, 6). Later, the measurements carried out after applying the moisturiser allowed the obtaining of excellent results on both groups, with more spectacular results for the patients with chronic contact dermatitis, whose skin hydration improved by 17.1% compared to the baseline time. For the healthy subjects, the hydration increase was gradual, but as expected lower than for the former (10.9% improvement compared to the baseline).
The measurements of the hydration degree allowed us to observe an effect in the short term (maximum increase in hydration after one hour from the application of the cream) (7,8) and an effect in the long term (maintenance of moisturising effect after 7 and 28 days respectively, but at a lower level compared to the first application – due to the evaporation of excess water) of the moisturising preparation for the patients with dermatitis (9,10). In the healthy subjects the increase was gradual, continuous. This increase in water content can be explained by the effects of humectants or natural moisturising factors in the product, ingredients that retain or bind water or draw it from the deeper layers; by the occlusive properties of the lipids in the cream, which have a protective effect, acting as a shield and preventing excessive water loss; by the action of some active ingredients on the intercellular cement.
This study also shows that the degree of skin hydration is inversely proportional with age. The moisturiser determined an increase in hydration in both types of subjects, in all three age groups, but those who showed the most obvious effect were the young adults (18-29 years old), experiencing an increase of 19.9% compared to the commencement of the therapy. They were followed by the group aged 30-49, and then by the patients in the segment aged 50-70. This pattern is repeated in the healthy subjects, but with lower increase, and is confirmed by data obtained in other studies (11). ❑
CONCLUSIONS
The method of measuring the degree of epidermal hydration by using the electrical capacitance is effective and reproducible and recommends the Corneometer as a non-invasive, in vivo, easy and inexpensive work tool. The Corneometer CM 825 is easy to use and reliable, widely utilised in international studies for measurements of hydration degree in healthy or pathological conditions, for quantitative assessment of the effectiveness of various preparations intended for application to the skin surface, under well-controlled and standardised conditions (12).
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
none declared.
References
- 1.Prall JK, Theiler RF, Bowser PA, et al. The effectiveness of cosmetic products in alleviating a range of skin dryness conditions as determined by clinical and instrumental techniques. Int J Cosmet Sci. 1986;8:159–159. doi: 10.1111/j.1467-2494.1986.tb00444.x. [DOI] [PubMed] [Google Scholar]
- 2.Batt MD, Davis WB, Fairhurst E, et al. Changes in the physical properties of the stratum corneum following treatment with glycerol. J Soc Cosmet Chem. 1988;39:367–367. [Google Scholar]
- 3.Bornkessel A, Flach M, Arens-Corell M, et al. Functional assessment of a washing emulsion for sensitive skin: mild impairment of stratum corneum hydration, pH, barrier function, lipid content, integrity and cohesion in a controlled washing test. Skin Res Technol. 2005;11:53–60. doi: 10.1111/j.1600-0846.2005.00091.x. [DOI] [PubMed] [Google Scholar]
- 4.Blichman CW, Serup J. Assessment of skin moisture. Measurement of electrical conductance, capacitance and transepidermal water loss. Acta Derm Venereol. (Stockh.) 1988;68:284–284. [PubMed] [Google Scholar]
- 5.Tagami H. In: Cutaneous Investigation in Health and Disease, Noninvasive Methods and Instrumentation. Ed. Marcel Dekker; Lévêque JL, New York: 1989. Impedance measurements for evaluation of the hydration state of the skin surface. pp. 5–5. [Google Scholar]
- 6.Mosely H, English JS, Coghill GM, et al. Assessment and use of a new skin hygrometer. Bioeng Skin. 1985;1:177–177. [Google Scholar]
- 7.Clarys P, Barel AO, Gabard B. Non-invasive electrical measurements for the evaluation of the hydration state of the skin: comparison between three conventional instruments: the Corneometer, the Skicon and the Nova DPM. Skin Res Technol. 1999;5:14–14. [Google Scholar]
- 8.Fluhr JW, Gloor M, Lazzerini SL, et al. Comparative study of five instruments measuring stratum corneum hydration (Corneometer CM 820 and CM 825, Skicon-200, Nova DPM 9003 and Dermalab). Part I. In vitro. Part II. In vivo. Skin Res Technol. 1999;5:161–171. [Google Scholar]
- 9.Barel AO, Clarys P, Gabard B. In Cosmetics: Controlled Efficacy Studies and Regulations, Elsner P, Merk HF and Maibach HI. Eds. Springer; Berlin: 1999. In vivo evaluation of the hydration state of the skin: measurements and methods for claim support. pp. 57–57. [Google Scholar]
- 10.Barel AO. In: Bioengineering of the Skin: Skin Biomechanics. Elsner P, Berardesca E, Wilhelm KP and Maibach HI. Eds. CRC Press; Boca Raton: 2002. Product testing: moisturizers. pp. 241–241. [Google Scholar]
- 11.Heinrich U, Koop U, Leneveu-Duchemin MC, et al. Members of the DGK Task Force "Skin Hydration," multi-center comparison of skin hydration in terms of physical, physiological and product dependent parameters by the capacitive method (Corneometer CM 825). J Cosmet Sci. 2003:25–31. doi: 10.1046/j.1467-2494.2003.00172.x. [DOI] [PubMed] [Google Scholar]
- 12.Rogiers V, Derde MP, Verleye G, et al. Standardized conditions needed for skin surface hydration measurements. Cosmet Toiletries. 1990;105:73–73. [Google Scholar]