Abstract
Based on observational studies there is a linear increase in cardiovascular risk with higher systolic blood pressure, yet clinical trials have not shown benefit across all systolic blood pressure categories. We assessed if troponin-T measured using high-sensitivity assay was associated with cardiovascular disease within systolic blood pressure categories in 11191 Atherosclerosis Risk in Communities study participants. Rested sitting systolic blood pressure by 10-mmHg increments and troponin categories were identified. Incident heart failure hospitalization, coronary heart disease and stroke were ascertained over a median of 12 years after excluding individuals with corresponding disease. Approximately 53% of each type of cardiovascular event occurred in individuals with systolic blood pressure<140 mmHg and troponin-T≥3ng/L. Higher troponin-T was associated with increasing cardiovascular events across most systolic blood pressure categories. The association was strongest for heart failure and least strong for stroke. There was no similar association of systolic blood pressure with cardiovascular events across troponin-T categories. Individuals with troponin-T≥3ng/L and systolic blood pressure<140mmHg had higher cardiovascular risk compared to those with troponin-T<3ng/L and systolic blood pressure 140-159 mmHg.
Higher troponin-T levels within narrow systolic blood pressure categories portend increased cardiovascular risk, particularly for heart failure. Individuals with lower systolic blood pressure but measurable troponin-T had greater cardiovascular risk compared to those with suboptimal systolic blood pressure but undetectable troponin-T. Future trials of systolic hypertension may benefit by using high-sensitivity troponin-T to target high-risk patients.
Keywords: High-sensitivity troponin-T, Hypertension, Atherosclerosis Risk In Communities (ARIC) Study, Cardiovascular disease, Heart failure
Introduction
Elevated blood pressure is a modifiable risk factor strongly associated with coronary heart disease (CHD), stroke and heart failure (HF) 1, 2. Observational studies have shown that beginning at a blood pressure (BP) of 115/75 mmHg, the risk for cardiovascular (CV) disease doubles with each 20/10-mmHg increment in BP 3. Similarly, the presence of hypertension (HTN) classifies an individual as having “Stage A” HF, i.e. at increased risk for future development of HF 4.
Clinical trials have generally shown that BP reduction in individuals with HTN resulted in decreased CV disease incidence, including HF 5. While BP lowering interventions are clearly associated with improved outcomes at systolic BP (SBP) >150 mmHg, recent studies evaluating intensive control of BP have shown no benefit 2. For example, in the Action to Control Cardiovascular Risk in Diabetes trial, SBP reduction in diabetics to <120 mmHg did not lower CV events when compared with lowering SBP to <140 mmHg 6. In fact, the 2014 report from the Panel Members Appointed to the Eighth Joint National Committee has revised the BP management targets in HTN such that for individuals 60 years or older, therapy is now advocated only for SBP ≥150 mmHg or diastolic BP ≥90 mmHg 2. Epidemiological studies, on the other hand, have shown a monotonic, linear increase in CV risk with increasing SBP starting at 115 mmHg 3. This disconnect between epidemiological studies and clinical trial results suggests that the risk associated with intensive antihypertensive treatment negates the potential benefit of lower BP when considering the population at large, although a recent meta-analysis suggested that individuals at highest risk may benefit from aggressive BP management 7. Hence, an individual's attributes may modify the putative benefits of BP lowering, in which case a better characterization may be important to assess the role for more-intensive/personalized BP management.
Recently, cardiac troponin-T measured by high sensitivity assay (cTnT) has been shown to detect subclinical cardiac injury 8 and to predict CHD, HF, mortality and stroke in epidemiological studies 9-11. While atherosclerosis mediates a significant proportion of the HTN-associated adverse CV events, evidence of myocardial injury from HTN in the absence of atherosclerosis also is well documented 12, 13. Furthermore, among individuals with left ventricular hypertrophy (LVH) measurable cTnT (≥3 ng/L) was associated with significantly increased incident HF and CV death compared to individuals with cTnT below the lower limit of measurement (<3 ng/L) 14, indicating that cTnT can be informative even in the presence of LVH. Therefore, we hypothesized that measurement of cTnT would improve risk stratification for incident CV disease (CHD, stroke and first HF hospitalization) across the range of SBP.
Methods
Study Population, Blood Pressure Measurement and Troponin Assay
Of 11,656 participants who attended visit 4 of the Atherosclerosis Risk in Communities (ARIC) study, a population based study of cardiovascular disease incidence (see supplemental methods for additional details), 11,191 were eligible for our analysis after exclusions (S. figure 1). For each outcome of interest, individuals with prevalent disease were excluded (for example, for incident HF, those with prevalent HF were excluded). Certified technicians used a random-zero sphygmomanometer to measure 2 BP readings in the sitting position after 5 minutes of rest and an average BP of the 2 measurements was recorded 15. Hypertension was defined as SBP ≥140 mmHg, diastolic BP ≥90 mmHg or use of antihypertensive medications. We used the following pre-specified categories of SBP for our analysis: <120, 120-129, 130-139, 140-149, 150-159 and ≥160 mmHg.
The specific details regarding the cTnT assay have been previously published 9. Briefly, cTnT concentrations were measured with a high-sensitivity assay, Elecsys Troponin T (Roche Diagnostics®), on an automated Cobas e411 analyzer with a lower limit of measurement of 3 ng/L. Similar to our previous analyses, we used 5 pre-specified categories of cTnT (<3, 3-5, 6-8, 9-13, and ≥14 ng/L) 9.
Ascertainment of incident cardiovascular events
All potential CV events were adjudicated based on published criteria 16, 17. Incident CHD was defined as hospitalization for myocardial infarction, definite coronary death, coronary revascularization procedure, or silent myocardial infarction as confirmed by electrocardiogram (ECG). Hard CHD events excluded coronary revascularization procedures. Stroke was defined as sudden or rapid onset of neurological symptoms lasting for >24 hours or leading to death, in the absence of evidence for a nonstroke cause 16. Incident HF was defined as the first HF hospitalization identified with International Classification of Diseases Code of 428.× (Ninth Revision) or I50 (Tenth Revision) in any position on the hospital discharge list or a death certificate with death from HF in any position 18.
Statistical analysis
Our main outcomes of interest were incident CHD (total or hard CHD), stroke (all types) and first HF hospitalization. All presented tests were 2-tailed and a p-value <0.05 was considered statistically significant. Using Cox proportional hazards model, the associations between categories of cTnT or SBP and incident events were assessed using a model adjusted for age, race, gender, antihypertensive medication use, log of N terminal pro-B-type natriuretic peptide (NT-proBNP), estimated glomerular filtration rate, diabetes, fasting glucose, total/high-density lipoprotein cholesterol ratio, body mass index, current cigarette smoking and CV disease status. Follow up time ended when the participant had an outcome, died, was lost to follow-up, or survived until December 31st 2009.
We used 2 reference groups in our main analysis, (i) cTnT <3 ng/L and SBP <120 mmHg, and (ii) cTnT <3 ng/L and SBP 140-159 mmHg. The second reference group was used to examine whether individuals with measurable cTnT at levels of SBP where therapy will not be required currently had increased CV risk compared to those with higher SBP but cTnT below the lower limit of measurement. We performed the following sensitivity analyses: adjusted the model further for LVH as determined by ECG; used each SBP category and cTnT<3 ng/L as a reference; used cTnT ≤5 ng/L as a reference because cTnT of 5 ng/L is considered the limit of detection; and modeled cTnT as a continuous variable by keeping the same categories of SBP. Finally, using 2 different references in separate analyses (SBP <120 mmHg and cTnT <3 ng/L and SBP 140-159 mmHg and cTnT<3 ng/L), we performed subgroup analyses by the status of antihypertensive medication use.
Results
Baseline characteristics
The mean age of the study population was 63 (standard deviation, 6) years, approximately 22% were African Americans and 56% were women (Table 1). The mean BP was 128/71 (19/10) mmHg, mean cTnT 7.5 (17) ng/L and median NT-proBNP 68 (interquartile range, 33-134) pg/mL. Approximately 3.5% of participants had ECG-diagnosed LVH and 44% were using antihypertensive medications. Increasing cTnT levels were associated with increasing age, male sex, increasing NT-proBNP level, diabetes, antihypertensive medication use and with declining estimated glomerular filtration rate across each category of SBP and with higher prevalence of ECG-assessed LVH across most SBP categories (Table S1).
Table 1.
Baseline characteristics in the study population [n=11,191]
| Characteristic | *Study population |
|---|---|
| Age (years) | 62.8±5.7 |
| African American | 2,477 (22.1) |
| Women | 6,263 (55.9) |
| Current smokers | 1,650 (14.8) |
| BMI (kg/m2) | 28.8±5.6 |
| Blood glucose (mg/dL) | 111±39 |
| Total cholesterol (mg/dL) | 200.8±37.1 |
| HDL-C (mg/dL) | 50.0±16.5 |
| Total /HDL-C ratio | 4.4±1.5 |
| LDL-C (mg/dL) | 122.6±33.4 |
| Triglycerides (mg/dL) | 122 (89–174) |
| hs-CRP (mg/L) | 2.5 (1.1–5.5) |
| Blood pressure (mmHg) | 128/71±19/10 |
| Mean BP (mmHg) | 99.3±13.1 |
| Pulse pressure (mmHg) | 56.6±16 |
| NT-proBNP (pg/mL) | 68 (33–134) |
| cTnT (ng/L) | 7.5±17.0 |
| Creatinine (mg/dL) | 0.76±0.43 |
| eGFR (ml/min/1.73m2) | 109.2±33 |
| Use of antihypertensive | 4,894 (43.7) |
| LVH | 291 (3.5) |
| Diabetes | 1,870 (16.8) |
| Hypertension | 5,418 (47.6) |
Data presented as mean±SD or median (interquartile range) for continuous variables and n (%) for dichotomous variables.
BMI = body mass index, BP = blood pressure, cTnT = high-sensitivity cardiac troponin-T, eGFR = estimated glomerular filtration rate, HDL-C = high-density lipoprotein cholesterol, hs-CRP = high-sensitivity C-reactive protein, LDL-C = low-density lipoprotein cholesterol, LVH = left ventricular hypertrophy, NT-proBNP = N-terminal pro–B-type natriuretic peptide.
Cardiovascular outcomes
There were a total of 1,144 incident HF hospitalizations, 1,377 incident CHD events, including 857 incident hard CHD events and 526 incident stroke events, resulting in incident rates of 9.9, 12.1, 7.2 and 4.3 per 1000 person-years, respectively. Approximately 53% of each CV outcome occurred in individuals with SBP<140 mmHg and cTnT≥3 ng/L.
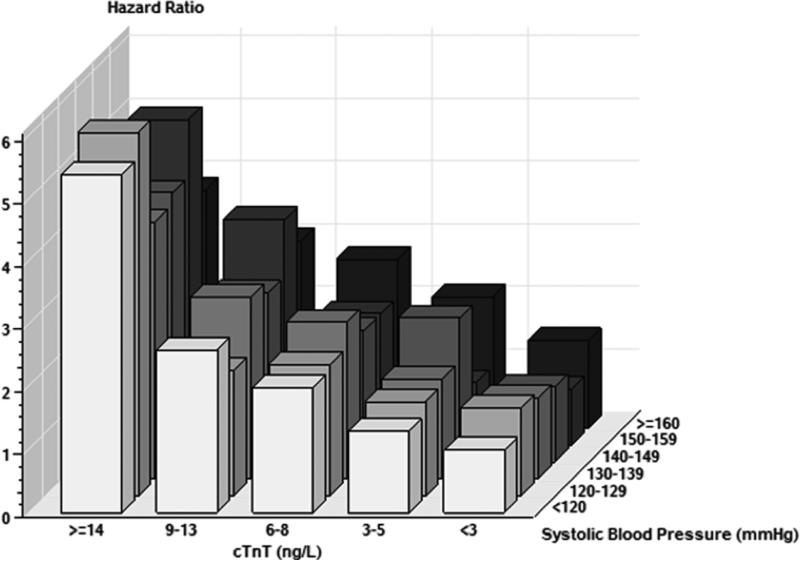
Increasing cTnT was significantly associated with increasing incidence of HF hospitalization for each category of SBP (Table 2 and Figure). The association with HF was very strong, with significant associations starting even at lower levels of cTnT across most SBP categories. There were similar but attenuated associations for CHD and hard CHD (Figures S2 A&B) and further weaker association for stroke, particularly at lower SBP categories (Figure S2 C). Compared to individuals with SBP <120 mmHg and cTnT <3 ng/L, those with SBP 130-139 mmHg and cTnT ≥14 ng/L had hazard ratios (HR) of 4.1 (95% confidence interval [CI], 2.6-6.4) for incident HF hospitalization; 2.0 (95% CI, 1.3-2.9) for CHD; 1.8 (95% CI, 1.1-2.9) for hard CHD; and 1.9 (95% CI, 1.0-3.6) for stroke (Table 2). In contrast, the trend and the strength of associations of increasing SBP with each CV event across each cTnT category were not as robust (Table 2).
Table 2.
Incident hazard rate ratios of cardiovascular outcomes in the study population across systolic blood pressure and troponin-T categories (reference group: systolic blood pressure <120 mmHg and troponin T <3 ng/L)
| SBP (mmHg) [n] | <3 | 3–5 | cTnT (ng/L) [n] 6–8 | 9–13 | ≥14 | P for trend* |
|---|---|---|---|---|---|---|
| HF [10416] | [3374] | [2647] | [2117] | [1405] | [873] | |
| <120 [3815] | reference | 1.3 (0.9-2.0) | 2.0 (1.3-2.9) | 2.6 (1.7-4.0) | 5.4 (3.6-8.0) | <0.001 |
| 120-129 [2380] | 1.4 (0.9-2.2) | 1.5 (1.0-2.3) | 2.1 (1.4-3.1) | 2.0 (1.2-3.1) | 5.8 (3.7-9.0) | <0.001 |
| 130-139 [1768] | 1.3 (0.8-2.0) | 1.6 (1.0-2.5) | 2.5 (1.6-3.8) | 2.9 (1.8-4.5) | 4.1 (2.6-6.4) | <0.001 |
| 140-149 [1179] | 1.2 (0.7-2.1) | 2.3 (1.5-3.6) | 2.1 (1.3-3.3) | 2.7 (1.7-4.3) | 4.3 (2.7-6.8) | 0.002 |
| 150-159 [656] | 0.9 (0.4-1.9) | 1.0 (0.5-2.0) | 2.1 (1.1-3.7) | 3.6 (2.2-5.7) | 5.2 (3.2-8.5) | <0.001 |
| ≥160 [618] | 1.4 (0.8-2.6) | 2.1 (1.2-3.9) | 2.7 (1.7-4.5) | 3.0 (1.9-4.9) | 3.8 (2.3-6.3) | <0.001 |
| P for trend † | 0.595 | 0.069 | 0.572 | 0.337 | 0.271 | |
| CHD [10518] | [3453] | [2666] | [2121] | [1397] | [881] | |
| <120 [3831] | reference | 1.0 (0.8-1.4) | 1.2 (0.8-1.6) | 1.3 (0.9-1.8) | 1.8 (1.2-2.5) | 0.570 |
| 120-129 [2373] | 1.1 (0.8-1.5) | 1.1 (0.8-1.6) | 1.3 (0.9-1.8) | 1.3 (0.9-1.9) | 2.5 (1.7-3.6) | 0.010 |
| 130-139 [1804] | 1.2 (0.8-1.7) | 1.4 (1.0-2.0) | 1.4 (0.9-1.9) | 1.6 (1.1-2.3) | 2.0 (1.3-2.9) | 0.062 |
| 140-149 [1203] | 1.2 (0.8-1.9) | 1.4 (1.0-2.1) | 1.5 (1.0-2.2) | 1.6 (1.1-2.4) | 2.1 (1.4-3.2) | 0.092 |
| 150-159 [658] | 1.0 (0.6-1.8) | 1.2 (0.7-2.0) | 1.9 (1.2-3.0) | 1.8 (1.2-2.9) | 2.7 (1.6-4.4) | 0.040 |
| ≥160 [649] | 1.4 (0.8-2.5) | 1.0 (0.5-1.9) | 2.1 (1.4-3.2) | 2.7 (1.8-3.9) | 2.4 (1.5-3.8) | 0.021 |
| P for trend † | 0.577 | 0.569 | 0.067 | 0.046 | 0.640 | |
| Hard CHD [10754] | [3474] | [2712] | [2183] | [1453] | [932] | |
| <120 [3907] | reference | 1.0 (0.6-1.4) | 1.0 (0.7-1.5) | 1.2 (0.8-1.9) | 2.0 (1.3-3.0) | 0.217 |
| 120-129 [2434] | 1.0 (0.7-1.6) | 0.9 (0.6-1.4) | 1.3 (0.9-1.9) | 1.2 (0.8-1.9) | 2.6 (1.7-4.1) | 0.001 |
| 130-139 [1842] | 1.0 (0.6-1.6) | 1.1 (0.7-1.8) | 1.1 (0.7-1.8) | 1.4 (0.8-2.3) | 1.8 (1.1-2.9) | 0.155 |
| 140-149 [1231] | 0.9 (0.5-1.5) | 1.1 (0.6-1.8) | 1.2 (0.7-2.0) | 1.0 (0.6-1.8) | 2.0 (1.2-3.3) | 0.006 |
| 150-159 [672] | 0.7 (0.3-1.6) | 0.8 (0.4-1.7) | 1.8 (1.0-3.3) | 1.7 (1.0-2.9) | 3.3 (1.9-5.6) | 0.004 |
| ≥160 [668] | 1.2 (0.7-2.4) | 1.4 (0.7-2.7) | 1.4 (0.8-2.5) | 2.1 (1.3-3.4) | 2.1 (1.2-3.5) | 0.724 |
| P for trend † | 0.884 | 0.841 | 0.253 | 0.391 | 0.418 | |
| Stroke [11042] | [3522] | [2749] | [2241] | [1513] | [1017] | |
| <120 [4030] | reference | 1.1 (0.7-1.9) | 0.6 (0.3-1.1) | 1.4 (0.8-2.5) | 1.1 (0.6-2.3) | 0.178 |
| 120-129 [2489] | 1.2 (0.7-2.0) | 1.3 (0.7-2.2) | 1.7 (1.0-2.9) | 1.5 (0.8-2.7) | 1.4 (0.7-2.9) | 0.530 |
| 130-139 [1889] | 1.2 (0.7-2.1) | 1.1 (0.6-2.0) | 1.6 (0.9-2.8) | 1.8 (1.0-3.4) | 1.9 (1.0-3.6) | 0.514 |
| 140-149 [1262] | 1.0 (0.5-2.0) | 1.8 (1.0-3.3) | 1.5 (0.8-2.7) | 1.5 (0.8-3.0) | 3.0 (1.6-5.6) | 0.173 |
| 150-159 [690] | 1.1 (0.4-2.5) | 1.0 (0.4-2.3) | 1.3 (0.5-3.2) | 3.2 (1.7-5.9) | 2.4 (1.1-4.8) | 0.037 |
| ≥160 [682] | 1.9 (1.0-3.8) | 2.2 (1.1-4.5) | 1.2 (0.6-2.7) | 1.9 (1.0-3.7) | 3.3 (1.8-6.1) | 0.318 |
| P for trend † | 0.674 | 0.483 | 0.044 | 0.181 | 0.014 |
Data presented are hazard ratios (95% confidence interval) as calculated using Cox proportional hazards model after adjusting for age, race, gender, antihypertensive medication use, log NT-proBNP, renal function (estimated glomerular filtration rate), diabetes status, fasting glucose, total cholesterol/HDL-C ratio, BMI, current cigarette smoking and previous CV disease status (except the outcome for each model; e.g., for HF, we adjusted for CHD and stroke).
CHD = coronary heart disease, CV = cardiovascular, HF = heart failure, SBP = systolic blood pressure, other abbreviations similar to Table 1.
Numbers in parentheses indicate number of participants.
P for trend was calculated based on the results of Wald chi-square test on linearity hypothesis of ordered cTnT or SBP categories.
P for trend across rows (i.e., trend across increasing cTnT at each SBP category)
P for trend across columns (i.e., trend across increasing SBP at each cTnT category)
Figure.
Hazard for heart failure by systolic blood pressure and high-sensitivity cardiac troponin-T categories
The figure shows hazards for incident heart failure hospitalization with increasing systolic blood pressure and high-sensitivity cardiac troponin-T in a fully adjusted model.
When the reference was changed to SBP 140-159 mmHg and cTnT <3 ng/L, there were similar trends for CV events (Table 3) with individuals with cTnT ≥3 ng/L (especially those with higher cTnT ranges) having significantly increased hazards for CV events. For example, individuals with SBP 130-139 mmHg and cTnT ≥14 ng/L had HRs of 3.7 (95% CI, 2.3-6.1) for incident HF hospitalization, 1.7 (95% CI, 1.1-2.6) for CHD, 2.2 (95% CI, 1.2-4.0) for hard CHD, and 1.8 (95% CI, 0.9-3.7) for stroke.
Table 3.
Incident hazard rate ratios of cardiovascular outcomes in the study population across systolic blood pressure and troponin-T categories (reference group: systolic blood pressure 140-159 mmHg and troponin T <3 ng/L)
| SBP (mmHg) | <3 | 3–5 | cTnT (ng/L) 6–8 | 9–13 | ≥14 | P for trend* |
|---|---|---|---|---|---|---|
| HF | ||||||
| <120 | 0.9 (0.6-1.5) | 1.2 (0.7-1.9) | 1.8 (1.1-2.8) | 2.4 (1.5-3.8) | 4.9 (3.1-7.7) | <0.001 |
| 120-129 | 1.3 (0.8-2.1) | 1.4 (0.9-2.2) | 1.9 (1.2-3.0) | 1.8 (1.1-3.0) | 5.3 (3.2-8.6) | <0.001 |
| 130-139 | 1.2 (0.7-1.9) | 1.4 (0.9-2.4) | 2.3 (1.4-3.6) | 2.6 (1.6-4.3) | 3.7 (2.3-6.1) | <0.001 |
| 140-159 | reference | 1.6 (1.0-2.6) | 1.9 (1.2-3.0) | 2.8 (1.8-4.4) | 4.2 (2.7-6.7) | <0.001 |
| ≥160 | 1.3 (0.7-2.4) | 1.9 (1.0-3.6) | 2.5 (1.5-4.3) | 2.7 (1.6-4.6) | 3.5 (2.0-5.9) | <0.001 |
| CHD | ||||||
| <120 | 0.9 (0.6-1.2) | 0.9 (0.6-1.3) | 1.0 (0.7-1.4) | 1.1 (0.8-1.7) | 1.5 (1.0-2.3) | 0.570 |
| 120-129 | 1.0 (0.6-1.4) | 1.0 (0.7-1.5) | 1.1 (0.7-1.6) | 1.1 (0.8-1.7) | 2.1 (1.4-3.3) | 0.010 |
| 130-139 | 1.0 (0.7-1.6) | 1.2 (0.8-1.8) | 1.2 (0.8-1.8) | 1.4 (0.9-2.1) | 1.7 (1.1-2.6) | 0.062 |
| 140-159 | reference | 1.2 (0.8-1.7) | 1.4 (0.9-2.1) | 1.5 (1.0-2.2) | 2.0 (1.3-3.0) | 0.172 |
| ≥160 | 1.3 (0.7-2.2) | 0.8 (0.4-1.7) | 1.8 (1.1-2.9) | 2.3 (1.5-3.5) | 2.1 (1.3-3.4) | 0.021 |
| Hard CHD | ||||||
| <120 | 1.3 (0.8-2.1) | 1.2 (0.7-2.0) | 1.3 (0.7-2.1) | 1.6 (0.9-2.7) | 2.5 (1.4-4.3) | 0.217 |
| 120-129 | 1.3 (0.7-2.2) | 1.1 (0.6-2.0) | 1.6 (1.0-2.7) | 1.5 (0.8-2.7) | 3.3 (1.9-5.7) | 0.001 |
| 130-139 | 1.3 (0.7-2.3) | 1.4 (0.8-2.5) | 1.4 (0.8-2.5) | 1.7 (0.9-3.1) | 2.2 (1.2-4.0) | 0.115 |
| 140-159 | reference | 1.2 (0.7-2.2) | 1.8 (1.0-3.0) | 1.6 (0.9-2.8) | 3.1 (1.8-5.3) | 0.010 |
| ≥160 | 1.6 (0.8-3.3) | 1.7 (0.8-3.6) | 1.8 (0.9-3.5) | 2.6 (1.4-4.7) | 2.6 (1.4-4.9) | 0.724 |
| Stroke | ||||||
| <120 | 1.0 (0.5-1.7) | 1.1 (0.6-2.0) | 0.5 (0.3-1.1) | 1.4 (0.7-2.6) | 1.1 (0.5-2.4) | 0.178 |
| 120-129 | 1.1 (0.6-2.1) | 1.2 (0.6-2.3) | 1.7 (0.9-3.0) | 1.4 (0.7-2.8) | 1.3 (0.6-2.9) | 0.530 |
| 130-139 | 1.2 (0.6-2.3) | 1.1 (0.5-2.1) | 1.5 (0.8-2.9) | 1.8 (0.9-3.5) | 1.8 (0.9-3.7) | 0.514 |
| 140-159 | reference | 1.4 (0.8-2.7) | 1.4 (0.7-2.6) | 2.1 (1.2-3.9) | 2.6 (1.4-4.9) | 0.583 |
| ≥160 | 1.8 (0.9-4.0) | 2.1 (1.0-4.6) | 1.2 (0.5-2.7) | 1.8 (0.9-3.8) | 3.2 (1.6-6.3) | 0.318 |
In additional analyses, similar results were obtained when the model was further adjusted for ECG-diagnosed LVH (Table S2) or when the reference was changed to each SBP category and cTnT<3 ng/L (data not presented). We obtained similar results when cTnT ≤5 ng/L replaced cTnT <3 ng/L (Table S3). When cTnT was modeled as a continuous variable, there were significant hazards for HF, CHD and hard CHD across each category of SBP per 1-standard deviation increase in cTnT (17 ng/L) (Table S4). Results were less robust for stroke. Finally, when we analyzed the hazards for the different end points stratified by use of anti-hypertensive medications the results were for the most part consistent with the primary analysis whether we used SBP <120 mmHg and cTnT <3 ng/L or SBP 140-159 and cTnT <3 ng/L as the reference (Tables S5 A&D and S6 A&D), except for CHD outcomes (Tables S5 B-C and S6 B-C).
Discussion
In these analyses, we show that individuals with higher levels of cTnT have significantly increased risk for incident CV events within narrow SBP categories, with the strongest hazards observed in individuals with the highest cTnT levels in each SBP category. The association was particularly strong for HF. While the association between cTnT and various CV events has been previously described in several studies 10, 12 including the ARIC study 9, 11, the value of measuring high-sensitivity troponin-T as a marker of the effect of BP on incident CV outcomes has not been previously reported. In a study of 176 Japanese hypertensive individuals free of CV disease, troponin-T ≥20 ng/L was independently associated with hospitalization for CV or cerebrovascular disease (HR 6.58, p <0.0001) compared to 39 normal controls 19; however this study did not use the higher sensitivity assay. Because cTnT is a marker of myocardial injury (an important step in the pathophysiology of adverse CV events such as HF), we hypothesized that cTnT assessment would identify those individuals in whom risk factors such as HTN has a particularly adverse impact and render them at higher risk for incident CV events. Indeed, one of the more important findings of our study was that among individuals with SBP that will not require therapy per current US guidelines 2 (e.g., <140 mmHg), those with increased cTnT levels had significantly higher hazards for CV events when compared to those with suboptimal SBP (e.g., SBP 140-159 mmHg) but cTnT below the lower limit of measurement (Table 3).
The association with stroke was not as robust, particularly at lower BP categories, likely related to the smaller number of individuals with incident stroke and perhaps also is a reflection of other important pathophysiological mechanisms of stroke. On the other hand, increase in SBP within each cTnT category was not generally associated with a significant trend for increasing risk for incident CV events (Table 2). This suggests that the effect of SBP was attenuated once we accounted for cTnT, indicating that myocardial injury may mediate the effects of SBP on HF and, to a lesser extent, on other CV endpoints. Therefore, cTnT may serve as a sensitive surrogate to identify individuals with elevated BP who have subclinical cardiac end-organ injury and hence are at greater risk for incident CV disease, especially HF. If replicated, such an observation has important clinical and research implications.
Elevated BP is a well-established risk factor for CV disease and interventions that lower BP have generally decreased CV events 5. This benefit has not been uniformly observed across all the BP and age ranges. The authors of the 2014 US guidelines for management of HTN concluded that while there is strong evidence to initiate pharmacologic treatment for individuals with BP of 150/90 mmHg or higher, the same level of evidence was not present at lower SBPs 2. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure recommended a goal BP of <130/80 mmHg in individuals with diabetes and chronic kidney disease as an attempt to identify high-risk groups who would likely derive the most benefit from intensive BP treatment 1. Although specific to diabetics, the Action to Control Cardiovascular Risk in Diabetes failed to show that intensive lowering of SBP (a mean of 119.3 mmHg was achieved) was superior to traditional management of SBP (a mean SBP of 133.5 mmHg was achieved in the placebo arm) among diabetics 6. Similarly, a lower BP goal (e.g., <130/80 mmHg) did not significantly lower renal or CV end points in patients with chronic kidney disease 2. On the other hand, a meta-analysis of epidemiological studies showed that the risk for CV disease doubles with each 20/10 mmHg increase in BP, beginning at BP of 115/75 mmHg 3, while another meta-analysis documented an increased risk of stroke in a dose-response manner as BP increased from 120-129/80-84 to 130-139/85-89 mmHg 20. Therefore, the literature reflects a clear disconnect between epidemiological studies and clinical trials, viz. the benefits of BP reduction at different BP levels. A deeper understanding of the circumstances under which the risk of the intervention exceeds the benefit of BP lowering as benchmarked against the population at large is needed. Identifying susceptible individuals, for instance those further advanced in the pathophysiological cascade of adverse CV events, may help optimize the risk to benefit balance and provide opportunities to personalize the management of elevated BP. Indeed a recent meta-analysis of clinical trials of antihypertensive medications showed that as the baseline CV risk increased there was progressively greater absolute risk reductions in major CV events 7.
Troponin T is a sensitive marker of myocardial injury 8, which is likely an important contribution in the pathogenesis of adverse CV events such as HF. This study found that approximately 53% of each type of CV event occurred in individuals with SBP<140 mmHg and cTnT≥3 ng/L. Taken together with other data such as that from the Dallas Heart Study where measurable cTnT (≥3 ng/L) was associated with further increased hazards for adverse CV events among individuals with LVH 14, we believe that future clinical trials can benefit from the use of cTnT to help characterize susceptible individuals in whom therapy options can be tested to personalize the management of elevate BP and the prevention of its sequelae.
The strengths of our study include a well-characterized large biracial population (majority women) followed for a median of 12 years with careful adjudication of incident CV events. There were some limitations as well. Some individuals with measurable cTnT and low SBP (e.g., <140 mmHg) could possibly have had subclinical left ventricular dysfunction, which could not be evaluated due to lack of echocardiography data. All individuals in our analysis were asymptomatic and hence echocardiogram would not have been clinically recommended 21. Hence despite our inability to evaluate for subclinical left ventricular dysfunction clinically our results will still have significant value. Furthermore, since the ARIC study conducts ongoing and comprehensive surveillance for CV-related hospitalizations and outcomes of its cohort 22, it is less likely that individuals with significant left ventricular dysfunction, who would most likely be symptomatic would have been missed. Additionally, one may expect use of BP lowering medications such as angiotensin converting enzyme inhibitors in these individuals, but our subgroup analyses stratified by antihypertensive medication use showed results similar to that of the overall population for most end points and SBP categories. We further showed that cTnT remains associated with CV events independent of NT-proBNP and other CV risk factors. The original ARIC cohort was selected based on random sampling of participants. It is possible that visit 4 participants were a healthier subcohort of the original sample. However, if the association is strong in a healthier population (as we report) then it is likely that the association would have persisted with a sicker population as well. Finally, the observational design of our study also requires that our results be interpreted with caution, particularly in contrast to the information emerging from clinical trials that have the benefit of randomization. Although prospective and rigorously standardized, as well as analyzed with inclusion of pertinent covariates, residual confounding cannot be ruled out.
Perspectives
cTnT is strongly associated with CV events across all SBP categories including “prehypertensives”. By perhaps identifying individuals with subclinical myocardial injury cTnT may help identify the individuals most compromised in their pathophysiology, and thus most prone to incident CV events. Future clinical trials should consider cTnT as a marker to identify subjects at higher risk for CV events in whom aggressive risk factor modification can be tested.
Supplementary Material
Novelty and significance.
What is new?
High-sensitivity troponin T is associated with increased adverse cardiovascular events across the range of systolic blood pressure within 10 mm Hg systolic blood pressure increments.
What is relevant?
The risk for incident adverse cardiovascular end points of individuals with cardiovascular risk factors such as systolic blood pressure can be better characterized by measuring a marker of myocardial injury (troponin T). Such approaches may contribute to personalize the delivery of care in individuals with elevated blood pressure by identifying those further advanced in the pathophysiological cascade toward incident cardiovascular events.
Summary
Clinical trials are needed to test the efficacy of aggressive risk factor modification in those with subclinical myocardial injury indexed by elevated, high-sensitivity troponin-T.
Acknowledgements
The authors thank the staff and participants of the ARIC study for their important contributions and Kerrie Jara for editorial assistance.
Source(s) of Funding
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C).
Footnotes
- DeLemos: Consulting: Abbott Diagnostics. Research grants: Abbott Diagnostics, Roche Diagnostics. Pending patent: Co-inventor on patent using high sensitivity cardiac troponin T and left ventricular hypertrophy as markers of heart failure risk (patent no. 61990386).
- Hoogeveen: Research grant: Roche. Provisional patent (patent no. 61721475) entitled “Biomarkers to Improve Prediction of Heart Failure Risk” filed by Baylor College of Medicine, Roche.
- Ballantyne: Research grants: Roche. Provisional patent (patent no. 61721475) entitled “Biomarkers to Improve Prediction of Heart Failure Risk” filed by Baylor College of Medicine, Roche.
- Nambi: Research/research grants: Tomtec, GE, National Institute of Health, National Heart, Lung, and Blood Institute, Veterans Affairs MERIT grant. Regional Advisory board: Sanofi. Other financial benefit: Anthera. Provisional patent (patent no. 61721475) entitled “Biomarkers to Improve Prediction of Heart Failure Risk” filed by Baylor College of Medicine, Roche.
- Others: None declared
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., Jones DW, Materson BJ, Oparil S, Wright JT, Jr., Roccella EJ. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The jnc 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr., Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr., Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the eighth joint national committee (JNC 8). JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 4.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Jr., Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. Acc/aha 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: A report of the american college of cardiology/american heart association task force on practice guidelines (writing committee to update the 2001 guidelines for the evaluation and management of heart failure): Developed in collaboration with the american college of chest physicians and the international society for heart and lung transplantation: Endorsed by the heart rhythm society. Circulation. 2005;112:e154–235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 5.Gueyffier F, Boutitie F, Boissel JP, Pocock S, Coope J, Cutler J, Ekbom T, Fagard R, Friedman L, Perry M, Prineas R, Schron E. Effect of antihypertensive drug treatment on cardiovascular outcomes in women and men. A meta-analysis of individual patient data from randomized, controlled trials. The indana investigators. Ann Intern Med. 1997;126:761–767. doi: 10.7326/0003-4819-126-10-199705150-00002. [DOI] [PubMed] [Google Scholar]
- 6.Cushman WC, Evans GW, Byington RP, Goff DC, Jr., Grimm RH, Jr., Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sundstrom J, Arima H, Woodward M, Jackson R, Karmali K, Lloyd-Jones D, Baigent C, Emberson J, Rahimi K, MacMahon S, Patel A, Perkovic V, Turnbull F, Neal B. Blood pressure-lowering treatment based on cardiovascular risk: A meta-analysis of individual patient data. Lancet. 2014;384:591–598. doi: 10.1016/S0140-6736(14)61212-5. [DOI] [PubMed] [Google Scholar]
- 8.Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, Biedert S, Schaub N, Buerge C, Potocki M, Noveanu M, Breidthardt T, Twerenbold R, Winkler K, Bingisser R, Mueller C. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361:858–867. doi: 10.1056/NEJMoa0900428. [DOI] [PubMed] [Google Scholar]
- 9.Saunders JT, Nambi V, de Lemos JA, Chambless LE, Virani SS, Boerwinkle E, Hoogeveen RC, Liu X, Astor BC, Mosley TH, Folsom AR, Heiss G, Coresh J, Ballantyne CM. Cardiac troponin t measured by a highly sensitive assay predicts coronary heart disease, heart failure, and mortality in the atherosclerosis risk in communities study. Circulation. 2011;123:1367–1376. doi: 10.1161/CIRCULATIONAHA.110.005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.deFilippi CR, de Lemos JA, Christenson RH, Gottdiener JS, Kop WJ, Zhan M, Seliger SL. Association of serial measures of cardiac troponin t using a sensitive assay with incident heart failure and cardiovascular mortality in older adults. JAMA. 2010;304:2494–2502. doi: 10.1001/jama.2010.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Folsom AR, Nambi V, Bell EJ, Oluleye OW, Gottesman RF, Lutsey PL, Huxley RR, Ballantyne CM. Troponin t, n-terminal pro-b-type natriuretic peptide, and incidence of stroke: The atherosclerosis risk in communities study. Stroke. 2013;44:961–967. doi: 10.1161/STROKEAHA.111.000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Lemos JA, Drazner MH, Omland T, Ayers CR, Khera A, Rohatgi A, Hashim I, Berry JD, Das SR, Morrow DA, McGuire DK. Association of troponin t detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA. 2010;304:2503–2512. doi: 10.1001/jama.2010.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sato Y, Yamamoto E, Sawa T, Toda K, Hara T, Iwasaki T, Fujiwara H, Takatsu Y. High-sensitivity cardiac troponin t in essential hypertension. Journal of Cardiology. 2011;58:226–231. doi: 10.1016/j.jjcc.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Neeland IJ, Drazner MH, Berry JD, Ayers CR, deFilippi C, Seliger SL, Nambi V, McGuire DK, Omland T, de Lemos JA. Biomarkers of chronic cardiac injury and hemodynamic stress identify a malignant phenotype of left ventricular hypertrophy in the general population. J Am Coll Cardiol. 2013;61:187–195. doi: 10.1016/j.jacc.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Heart L, and Blood Institute . Atherosclerosis Risk in Communities Study protocol: Manual 11: Sitting blood pressure:. Visit 4. Version 4.0 ed. ARIC Coordinating Center; Chapel Hill, NC: 1997. [Google Scholar]
- 16.Rathore SS, Hinn AR, Cooper LS, Tyroler HA, Rosamond WD. Characterization of incident stroke signs and symptoms: Findings from the atherosclerosis risk in communities study. Stroke. 2002;33:2718–2721. doi: 10.1161/01.str.0000035286.87503.31. [DOI] [PubMed] [Google Scholar]
- 17.White AD, Folsom AR, Chambless LE, Sharret AR, Yang K, Conwill D, Higgins M, Williams OD, Tyroler HA. Community surveillance of coronary heart disease in the atherosclerosis risk in communities (ARIC) study: Methods and initial two years' experience. J Clin Epidemiol. 1996;49:223–233. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 18.Rosamond WD, Chang PP, Baggett C, Johnson A, Bertoni AG, Shahar E, Deswal A, Heiss G, Chambless LE. Classification of heart failure in the atherosclerosis risk in communities (ARIC) study: A comparison of diagnostic criteria. Circ Heart Fail. 2012;5:152–159. doi: 10.1161/CIRCHEARTFAILURE.111.963199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Setsuta K, Kitahara Y, Arae M, Ohbayashi T, Seino Y, Mizuno K. Elevated cardiac troponin t predicts adverse outcomes in hypertensive patients. Int Heart J. 2011;52:164–169. doi: 10.1536/ihj.52.164. [DOI] [PubMed] [Google Scholar]
- 20.Huang Y, Cai X, Li Y, Su L, Mai W, Wang S, Hu Y, Wu Y, Xu D. Prehypertension and the risk of stroke: A meta-analysis. Neurology. 2014;82:1153–1161. doi: 10.1212/WNL.0000000000000268. [DOI] [PubMed] [Google Scholar]
- 21.Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL, Douglas PS, Faxon DP, Gillam LD, Kimball TR, Kussmaul WG, Pearlman AS, Philbrick JT, Rakowski H, Thys DM, Antman EM, Smith SC, Jr., Alpert JS, Gregoratos G, Anderson JL, Hiratzka LF, Hunt SA, Fuster V, Jacobs AK, Gibbons RJ, Russell RO. Acc/aha/ase 2003 guideline update for the clinical application of echocardiography: Summary article: A report of the american college of cardiology/american heart association task force on practice guidelines (acc/aha/ase committee to update the 1997 guidelines for the clinical application of echocardiography). Circulation. 2003;108:1146–1162. doi: 10.1161/01.CIR.0000073597.57414.A9. [DOI] [PubMed] [Google Scholar]
- 22. Https://www2.Cscc.Unc.Edu/aric/system/files/uc641701.Pdf. 26 April 2014.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.