Abstract
Introduction
Earlier reports of laparoscopic adrenalectomy (LA) for adrenal myelolipoma are limited.
Presentation of case
Between June 2000 and September 2012, we performed right adrenal resections using LA and open adrenalectomy (OA) in patients with myelolipoma (n = 3 and n = 3, respectively). Then, we evaluated patients' background characteristics and short- and long-term outcomes for both groups. The median maximum diameters of tumors were 3.5 (3.0–4.4) cm and 7.1 (7.0–9.5) cm for the LA and OA groups, respectively. The median durations of the operation were 152 (117–188) min and 218 (153–230) min, and the median blood loss volumes were 50 (20–160) mL and 290 (62–1237) mL in the LA and OA groups, respectively. The median postoperative lengths of hospital stay were 4 (4–4) days and 11 (11–13) days for the LA and OA groups, respectively. Conversion from LA to an open approach during surgery was not necessary in any of the cases. Additionally, perioperative morbidity and mortality were not observed.
Discussion
The limitation of this study is its methodological design; it is a case series and not a matched-control study, which would be difficult to conduct owing to the rare nature of adrenal myelolipoma. However, we esteem that LA will become widespread in the future because it is feasible, cosmetic, and less invasive.
Conclusion
LA was a safe, feasible, and effective approach to adrenal myelolipoma, assisted by advancement in preoperative imaging diagnostic techniques.
Keywords: Adrenal myelolipoma, Laparoscopic adrenalectomy, Open adrenalectomy
Abbreviations: CT, computed tomography; LA, laparoscopic adrenalectomy; OA, open adrenalectomy; MRI, magnetic resonance imaging; BMI, body mass index
1. Introduction
Adrenal myelolipoma was first described in 1905 by Gierke and was named by Oberling [1]. Its incidence varies between 0.08% and 0.4%, and is usually discovered incidentally on autopsies, surgeries, or imaging studies such as ultrasonography or computed tomography (CT) performed for other purposes. Adrenal myelolipomas constitute 1.9% of adrenal incidentalomas [2], often occur in both men and women between the ages of 50 and 70 years, and more frequently affect the right adrenal gland [2–4]. Most of the extra-adrenal myelolipomas develop in the presacral region (50%), followed by the stomach, liver, lymph nodes, spleen, and skull. With the recent advancement in diagnostic imaging methods, the discovery of small adrenal incidentalomas has been increasing. Considering the benign and non-functioning nature of these tumors, feasible and less-invasive surgical removal is desirable. Earlier reports of laparoscopic adrenalectomy (LA) for benign non-functioning adrenal incidentalomas are limited, but the results showed a considerable decrease in perioperative morbidity, hospital stay, and postoperative revival period compared with open adrenalectomy (OA) [5]. In the present study, we evaluated and compared the background characteristics and outcomes of patients who underwent surgical resection of adrenal myelolipoma using either LA or OA.
2. Materials and methods
2.1. Study population
We retrospectively reviewed and analyzed adrenal myelolipoma cases treated by 2 of the authors (KI and SK) at the NTT Medical Center in Tokyo, Japan, between June 2000 and September 2012, by examining patient records for details of demographic characteristics, therapeutic procedures, complications after treatment, pathological findings, and postoperative long-term outcomes.
2.2. Preoperative examinations
We evaluated tumor size and components using ultrasonography, CT, and magnetic resonance imaging (MRI), and analyzed initial laboratory data including hemograms, biochemical analyses results, and endocrine function test results.
2.3. Technical aspects of LA and OA
To perform LA, patients (Case 1–3) were placed in the supine position. A 5-mm scope was set between trocars for manipulation. One or two 5-mm trocars were placed around the epigastric region to facilitate retraction of the liver and gall bladder (Fig. 1). During the operation, the right liver and second portion of the duodenum were moved to identify the vena cava. Short hepatic veins were sacrificed, if they prevented identification. Meticulous dissection along the lateral vena cava allowed identification of the right adrenal vein. The surgeon then applied clips and ligated the adrenal vein, and dissected the residual tissue surrounding the right adrenal gland mainly using an ultrasonically activated cautery device with care to avoid tumor rupture. The resected tumor was placed in a sterilized specimen bag and removed through the most lateral incision. In OA, patients (Case 4–6) underwent laparotomy in the lateral or semi-lateral position using a reverse L incision or a retroperitoneal approach using a flank incision [6,7].
Fig. 1.
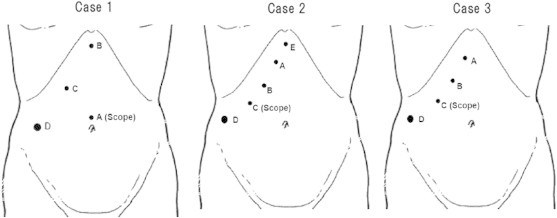
Laparoscopic port sites for adrenalectomy. In laparoscopic adrenalectomy, the scope was placed between the operator's hands. The operator manipulated C and D ports in Case 1, and B and D ports in Cases 2 and 3, respectively. The first assistant manipulated the B port in Case 1, and A and E ports in Case 2. A port was used in Case 3 to facilitate liver and gall bladder retraction by the first assistant.
2.4. Postoperative follow-up
Systemic follow-up including physical examinations and CT were performed every year for up to 5 years after surgical resection.
3. Results
3.1. Characteristics of patients
Adrenalectomy was performed in 6 patients with adrenal myelolipoma (5 men and 1 woman, median age, 43 [26–52] years) during the study period (Table 1). Three patients underwent LA and the remaining 3 underwent OA. The median body mass index (BMI) was 29.8 (24.4–31.5) kg/m2. Initially, Cases 1 and 2 were diagnosed with right adrenal cortical adenoma, but the maximum tumor diameter progressively increased (increases of 14 mm during 4 years and 15 mm during 2 years, respectively). The other patients were diagnosed with right adrenal myelolipoma initially and underwent right adrenalectomy promptly after the diagnosis. Preoperative imaging studies showed that all the tumors included fat components of various degrees, and that the median maximum diameter of the tumors was 5.1 (3.5–8.0) cm as illustrated in the enhanced abdominal CT and MR images of Case 2 (Fig. 2). While Case 6 preoperatively developed sudden right flank pain, other patients were asymptomatic. All these tumors were incidentally discovered during either routine medical check-ups or ambulatory follow-up for unrelated disorders. None of the patients presented with obvious abnormalities during endocrine examinations.
Table 1.
Background characteristics and clinical data of all patients.
| Case | Sex | Age (years) | BMI | Site | Symptom | Maximum diameter of the tumor (cm) | Operation | Operative time (min) | Blood loss volume (mL) | Hospital stay (days) | Morbidity | Follow-up duration (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 49 | 24.4 | Right | – | 4.5 | LA | 117 | 20 | 4 | – | 60 |
| 2 | F | 40 | 29.8 | Right | – | 5 | LA | 188 | 160 | 4 | – | 20 |
| 3 | M | 45 | 29.7 | Right | – | 3.5 | LA | 152 | 50 | 4 | – | 3 |
| 4 | M | 26 | 31.5 | Right | – | 8 | OA | 218 | 62 | 11 | – | 52 |
| 5 | M | 52 | 30.8 | Right | – | 5.2 | OA | 153 | 290 | 11 | – | 89 |
| 6 | M | 30 | 26.9 | Right | Right flank pain | 8 | OA | 230 | 1237 | 13 | Vocal cord paralysisa | 37 |
BMI, body mass index; LA, laparoscopic adrenalectomy; OA, open adrenalectomy.
One patient experienced postoperative vocal cord paralysis owing to the compression of tracheal tube during general anesthesia.
Fig. 2.
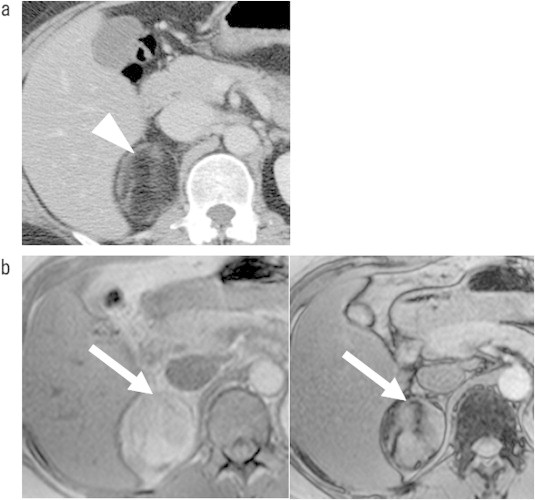
Imaging findings of a typical right adrenal myelolipoma. (a) Computed tomography shows a right adrenal tumor, measuring up to 5.0 cm in diameter with approximately – 80 Hounsfield units, which is suggestive of fat. (b) In-phase (left) and out-of-phase (right) gradient-echo magnetic resonance imaging reveals a right adrenal tumor (white arrow) with a partial fatty component.
3.2. Characteristics of operative procedures and pathological findings
The median duration of the operative procedures was 152 (117–188) min and 218 (153–230) min, and the median blood loss volume was 50 (20–160) mL and 290 (62–1237) mL in the LA and OA groups, respectively. The median hospital stay after adrenalectomy in the LA and OA groups was 4 (4–4) days and 11 (11–13) days, respectively. Postoperative pathological examinations confirmed adrenal myelolipomas in all cases. The macroscopic and microscopic findings of Case 2 are shown in Fig. 3. Pathological findings revealed intratumoral hemorrhage in Case 6.
Fig. 3.
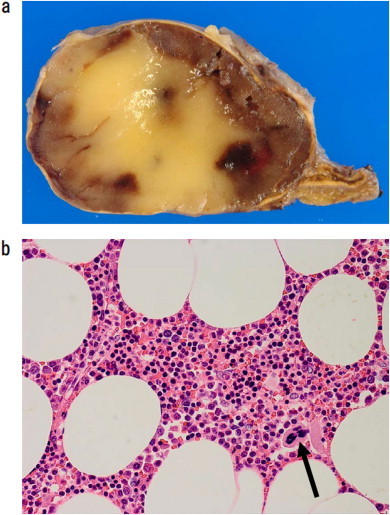
Macroscopic and microscopic findings of a typical case (a) A section of the surface of the resected tumor with a 5-cm diameter showed a mixture of tan-brown and pale yellow areas with abundant cells and fat, respectively. (b) Microscopically, the section showed characteristics of myelolipoma with mature fat and hematopoietic elements such as megakaryocytes (black arrow; hematoxylin and eosin, ×200). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
3.3. Short- and long-term outcomes after adrenalectomy
As for postoperative complications, vocal cord paralysis was observed in one case but no patient developed intraperitoneal complications. Conversion from LA to an open approach during surgery was not necessary in any of the cases. None of the patients presented with recurrent tumors during the median follow-up period of 44.5 (3–89) months.
4. Discussion
Adrenal myelolipoma is a neoplasm composed of various degrees of fatty tissue and hematopoietic elements [8]. Hematopoietic components develop outside sinusoids, and thus, cannot enter the systemic circulation, which makes myelolipomas hormonally nonfunctional [2,9]. Differential diagnoses for this condition based on imaging studies include retroperitoneal lipoma and liposarcoma, upper pole renal angiomyolipoma, retroperitoneal teratoma, adrenal cortical adenoma, and adrenal carcinoma. In rare cases, it is difficult to attain a definitive diagnosis of myelolipoma by cross-sectional imaging because of low fat content. While the origin of this neoformation has not been identified, Pascual et al. suggested that adrenal myelolipoma might be a site of extramedullary hematopoiesis [10]. In contrast, Meaglia and Schmidt proposed in 1992 that these tumors might originate from metaplasia of reticuloendothelial cells of blood capillaries in the adrenal gland in response to stimuli such as infection, stress, necrosis, or prolonged exposure to adrenocorticotropic hormone; this has become the most widely accepted theory [8,10]. Actually, some studies have reported adrenal myelolipomas concomitant with hypertension, obesity, diabetes mellitus, and hematological abnormalities [11,12]. For instance, obesity-related hyperaldosteronism may lead to myeloid metaplasia through overproduction of steroids, as well as degeneration and destruction of adrenal cortical cells. In the present study, most of the patients were obese and their bodily habitus might mediate myelolipomatous changes of the adrenal medulla. Additionally, certain diseases and conditions such as Cushing syndrome, Addison disease, adrenal hyperplasia, and chronic exogenous administration of steroids have been associated with the development of myelolipomas. Moreover, these tumors can be induced in subcutaneous tissue in the laboratory by grafting pituitary tissue and stimulating it with thyroid hormones or androgens (mainly testosterone) [13–15].
While most cases are clinically asymptomatic, according to the earlier reports, approximately 20% of patients can experience abdominal or lumbar pain secondary to hemorrhage, tumor necrosis, or mechanical compression by the tumor [2]. Some rarer symptoms include hematuria and abdominal mass. Treatments of adrenal myelolipoma vary from case to case and there is no global consensus. Doddi et al. argued that asymptomatic cases with a small lesion <3–4 cm in diameter should be followed up for 1 or 2 years and monitored by CT or MRI [2]. Symptomatic patients with a tumor diameter >4–5 cm or a tumor considered to be malignant are indicated for surgical intervention. Even asymptomatic tumors need to be removed if growth is detected during the follow-up period. Indeed, Gershuni et al. established that abdominal or flank pain, large tumor size, atypical radiologic appearance, and/or inferior vena cava compression were operative indications for patients with a presumptive diagnosis of adrenal myelolipoma [16]. Retroperitoneal hemorrhage caused by spontaneous rupture of adrenal myelolipoma is very rare, and surgical resection is also recommended in those cases [17–20]. However, the correlation between rupture rate and tumor size has not been established.
We performed OA in 3 cases (Cases 4–6) using the reverse L incision or a retroperitoneal approach using a flank incision in laparotomy, and LA in 3 cases (Cases 1–3) successfully. The limitation of this study is its methodological design; it is a case series and not a matched-control study, which would be difficult to conduct owing to the rare nature of this tumor. However, we esteem that LA will become widespread in the future because it is feasible, cosmetic, and less invasive. Toniato et al. demonstrated that LA had superior short-term outcomes compared with OA in the majority of pheochromocytoma cases regardless of the tumor size [21]. Additionally, Gershuni et al. reported that the safety of LA for adrenal myelolipomas and other pathologies appeared comparable in a retrospective cohort study of prospectively collected data [16]. Additional data, ideally noninferiority and case-matched control data, relevant to adrenal myelolipomas are needed to establish the safety and superiority of laparoscopic surgery versus the open approach. Through the recent advancement of diagnostic imaging methods, the discovery of smaller adrenal incidentalomas, including myelolipomas, will continuously increase. Under these circumstances, LA is considered a more efficient technique. In the present study, patients in the LA group were diagnosed with tumors in earlier stages than those in patients in the OA group, and progressive size increments were confirmed in 2 out of 3 cases in the LA group. LA revealed more favorable short-term outcomes in terms of operative duration, blood loss volume, and length of hospital stay than OA despite the small patient sample. Some surgeons stated that there was no tumor size limit for LA indication, although this approach should not be used when there are adhesions or infiltration to adjacent organs [10,22]. In addition, retroperitoneoscopic adrenalectomy is an increasingly valuable alternative to LA, especially for small tumors, and may reduce postoperative pain and length of hospital stay [23,24].
LA for adrenal myelolipoma has been sporadically reported, but short- and long-term outcome studies based on sufficient patient samples are lacking. The results of the present case series needs to be supported by further trials with longer follow-up periods to understand the real role of this laparoscopic surgical approach.
5. Conclusion
The study showed that LA was a safe, feasible, and effective approach for the treatment of adrenal myelolipoma assisted by the advancement in preoperative diagnostic imaging techniques.
Conflict of interest
The authors have no conflict of interest.
Funding
None.
Consent of patient
Informed consent was obtained from all patients.
References
- 1.López Martín L., García Cardoso J.V., Gómez Muñoz J., González Enguita C. Adrenal myelolipoma. Contribution of a case and bibliographic review. Arch Esp Urol. 2010;63:880–883. [PubMed] [Google Scholar]
- 2.Doddi S., Singhal T., Leake T., Sinha P. Management of an incidentally found large adrenal myelolipoma: a case report. Cases J. 2009;2:8414. doi: 10.4076/1757-1626-2-8414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jung S.I., Kim S.O., Kang T.W., Kwon D.D., Park K., Ryu S.B. Bilateral adrenal myelolipoma associated with hyperaldosteronism: report of a case and review of the literature. Urology. 2007;70:1223.e11–1223.e13. doi: 10.1016/j.urology.2007.09.046. [DOI] [PubMed] [Google Scholar]
- 4.Ong K., Tan K.B., Putti T.C. Myelolipoma within a non-functional adrenal cortical adenoma. Singapore Med J. 2007;48:e200–202. [PubMed] [Google Scholar]
- 5.Novitsky Y.W., Czerniach D.R., Kercher K.W., Perugini R.A., Kelly J.J., Litwin D.E. Feasibility of laproscopic adrenalectomy for large adrenal masses. Surg Laparosc Endosc Percutan Tech. 2003;13:106–110. doi: 10.1097/00129689-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Ferreira U., Nardi Pedro R., Matheus W.E., Prudente A., Mendonça Borges G., Rodrigues Netto N., Jr. Open surgical treatment of right-sided adrenal carcinomas >15cm. Urol Int. 2007;78:46–49. doi: 10.1159/000096934. [DOI] [PubMed] [Google Scholar]
- 7.Wani N.A., Kosar T., Rawa I.A., Qayum A. Giant adrenal myelolipoma: incidentaloma with a rare incidental association. Urol Ann. 2010;2:130–133. doi: 10.4103/0974-7796.68865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romano G., Cocchiara G., Calderone F., Buscemi G., Gioè F.P., Alongi G. Laparoscopic treatment of adrenal myelolipoma: case report and review of the literature. G Chir. 2006;27:228–231. [PubMed] [Google Scholar]
- 9.Pascual García X., Bujons Tur A., Rodríguez Faba O., Gómez Ruiz J.J., Palou Redorta J., Villavicencio Mavrich H. Extraadrenal perirenal myelolipoma: report of a case and review of the literature. Actas Urol Esp. 2007;31:932–934. doi: 10.1016/s0210-4806(07)73751-8. [DOI] [PubMed] [Google Scholar]
- 10.Tyritzis S.I., Adamakis I., Migdalis V., Vlachodimitropoulos D., Constantinides C.A. Giant adrenal myelolipoma, a rare urological issue with increasing incidence: a case report. Cases J. 2009;2:8863. doi: 10.4076/1757-1626-2-8863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olsson C.A., Krane R.J., Klugo R.C., Selikowitz S.M. Adrenal myelolipoma. Surgery. 1973;73:665–670. [PubMed] [Google Scholar]
- 12.Inuzuka M., Tamura N., Sone M., Taura D., Sonoyama T., Honda K. A case of myelolipoma with bilateral adrenal hyperaldosteronism cured after unilateral adrenalectomy. Intern Med. 2012;51:479–485. doi: 10.2169/internalmedicine.51.5777. [DOI] [PubMed] [Google Scholar]
- 13.Cha J.S., Shin Y.S., Kim M.K., Kim H.J. Myelolipomas of both adrenal glands. Korean J Urol. 2011;52:582–585. doi: 10.4111/kju.2011.52.8.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brogna A., Scalisi G., Ferrara R., Bucceri A.M. Giant secreting adrenal myelolipoma in a man: a case report. J Med Case Rep. 2011;5:298. doi: 10.1186/1752-1947-5-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Babinska A., Nałecz A., Swiatkowska-Stodulska R., Sworczak K. Adrenal myelolipomas composed with adrenal nodular hyperplasia in the same gland. Pol J Pathol. 2012;63:45–48. [PubMed] [Google Scholar]
- 16.Gershuni V.M., Bittner J.G., 4th, Moley J.F., Brunt L.M. Adrenal myelolipoma: operative indications and outcomes. J Laparoendosc Adv Surg Tech A. 2014;24:8–12. doi: 10.1089/lap.2013.0411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castillo O.A., Vitagliano G., Cortes O., Sánchez-Salas R., Arellano L. Laparoscopic adrenalectomy for adrenal myelolipoma. Arch Esp Urol. 2007;60:217–221. doi: 10.4321/s0004-06142007000200022. [DOI] [PubMed] [Google Scholar]
- 18.Amano T., Takemae K., Niikura S., Kouno M., Amano M. Retroperitoneal hemorrhage due to spontaneous rupture of adrenal myelolipoma. Int J Urol. 1999;6:585–588. doi: 10.1046/j.1442-2042.1999.611109.x. [DOI] [PubMed] [Google Scholar]
- 19.Moran R.E., Older R.A., De Angelis G.A., Baghdady B.H., Chrisman H.B., Ciambotti J.M. Genitourinary case of the day: giant adrenal myelolipoma. AJR Am J Roentgenol. 1996;167:246–251. doi: 10.2214/ajr.167.1.8659386. [DOI] [PubMed] [Google Scholar]
- 20.Goldman H.B., Howard R.C., Patterson A.L. Spontaneous retroperitoneal hemorrhage from a giant adrenal myelolipoma. J Urol. 1996;155:639. [PubMed] [Google Scholar]
- 21.Toniato A., Boschin I.M., Opocher G., Guolo A., Pelizzo M., Mantero F. Is the laparoscopic adrenalectomy for pheochromocytoma the best treatment? Surgery. 2007;141:723–727. doi: 10.1016/j.surg.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 22.Lin Po-Chun, Yang Fei-Shih. Bilateral giant adrenal myelolipomas: a case report and literature review. Chin J Radiol. 2008;33:261–264. [Google Scholar]
- 23.Constantinides V.A., Christakis I., Touska P., Palazzo F.F. Systematic review and meta-analysis of retroperitoneoscopic versus laparoscopic adrenalectomy. Br J Surg. 2012;99:1639–1648. doi: 10.1002/bjs.8921. [DOI] [PubMed] [Google Scholar]
- 24.Constantinides V.A., Christakis I., Touska P., Meeran K., Palazzo F. Retroperitoneoscopic or laparoscopic adrenalectomy? A single-centre UK experience. Surg Endosc. 2013;27:4147–4152. doi: 10.1007/s00464-013-3009-1. [DOI] [PubMed] [Google Scholar]


