Abstract
IMPORTANCE
Novel strategies are needed to increase the uptake of voluntary medical male circumcision (VMMC) in sub-Saharan Africa and enhance the effectiveness of male circumcision as an HIV prevention strategy.
OBJECTIVE
To determine whether small economic incentives could increase circumcision prevalence by addressing reported economic barriers to VMMC and behavioral factors such as present-biased decision making.
DESIGN, SETTING, AND PARTICIPANTS
Randomized clinical trial conducted between June 22, 2013, and February 4, 2014, among 1504 uncircumcised men aged 25 to 49 years in Nyanza region, Kenya. VMMC services were provided free of charge and participants were randomized to 1 of 3 intervention groups or a control group.
INTERVENTIONS
Participants in the 3 intervention groups received varying amounts of compensation conditional on undergoing circumcision at 1 of 9 study clinics within 2 months of enrollment. Compensation took the form of food vouchers worth 200 Kenya shillings (≈US $2.50), 700 Kenya shillings (≈US $8.75), or 1200 Kenya shillings (≈US $15.00), which reflected a portion of transportation costs and lost wages associated with getting circumcised. The control group received no compensation.
MAIN OUTCOMES AND MEASURES
VMMC uptake within 2 months.
RESULTS
Analysis of data for 1502 participants with complete data showed that VMMC uptake within 2 months was higher in the US $8.75 group (6.6%; 95% CI, 4.3%–9.5% [25 of 381]) and the US $15.00 group (9.0%; 95% CI, 6.3%–12.4% [34 of 377]) than in the US $2.50 group (1.9%; 95% CI, 0.8%–3.8% [7 of 374]) and the control group (1.6%; 95% CI, 0.6%–3.5% [6 of 370]). In logistic regression analysis, the US $8.75 group had significantly higher VMMC uptake than the control group (adjusted odds ratio [AOR] 4.3; 95% CI, 1.7–10.7), as did the US $15.00 group (AOR 6.2; 95% CI, 2.6–15.0). Effect sizes for the US $8.75 and US $15.00 groups did not differ significantly (P = .20).
CONCLUSIONS AND RELEVANCE
Among uncircumcised men in Kenya, compensation in the form of food vouchers worth approximately US $8.75 or US $15.00, compared with lesser or no compensation, resulted in a modest increase in the prevalence of circumcision after 2 months. The effects of more intense promotion or longer implementation require further investigation.
Following 3 randomized trials demonstrating that medical male circumcision reduces men’s risk of HIV acquisition by 50% to 60%,1–3 in 2007 UNAIDS and the World Health Organization recommended the scale-up of voluntary medical male circumcision (VMMC) in 14 countries in eastern and southern Africa.4 To achieve 80% circumcision prevalence among HIV-uninfected men aged 15 to 49 years, a total of 20.3 million and 8.4 million circumcisions will need to be performed in these countries between 2011–2015 and 2016–2025, respectively.5 Despite considerable scale-up efforts, most countries are far short of the targets associated with 80% circumcision prevalence.6 Although Kenya is one of few countries where circumcision prevalence has risen substantially, uptake has been highest among adolescents and lowest among men aged 25 to 49 years.7 Novel strategies are needed to increase VMMC uptake. To date, no trials of interventions to increase demand for VMMC have been conducted and recent reviews have identified this as a priority for implementation science research.6,8
Although VMMC is generally acceptable in noncircumcising communities in sub-Saharan Africa,9 numerous barriers to VMMC uptake have also been documented.9–11 Concern about lost wages during and after the circumcision procedure has been one commonly reported barrier. Low circumcision uptake may be further explained by the behavioral economics concept of present-biased preferences, which posits that individuals place greater emphasis on costs and benefits that are immediate rather than those that are delayed.12,13 To address these barriers, this study tested an intervention to increase demand for VMMC among older men in Kenya, based on prior research showing that incentives can modify health behaviors.14,15
We conducted a randomized clinical trial in Kenya that examined whether the provision of small amounts of conditional economic compensation could increase VMMC uptake among men aged 25 to 49 years.
Methods
Study Setting
The study took place within 3 districts in the Nyanza region of western Kenya. Adult HIV prevalence in the region is 15.1%,16 and primary occupations include subsistence farming, fishing, wage labor, and various forms of skilled and casual wage labor. The study was conducted in collaboration with Impact Research and Development Organization (IRDO), the largest VMMC service delivery organization in Kenya and primary provider of VMMC services in the study area.
Study Design and Participants
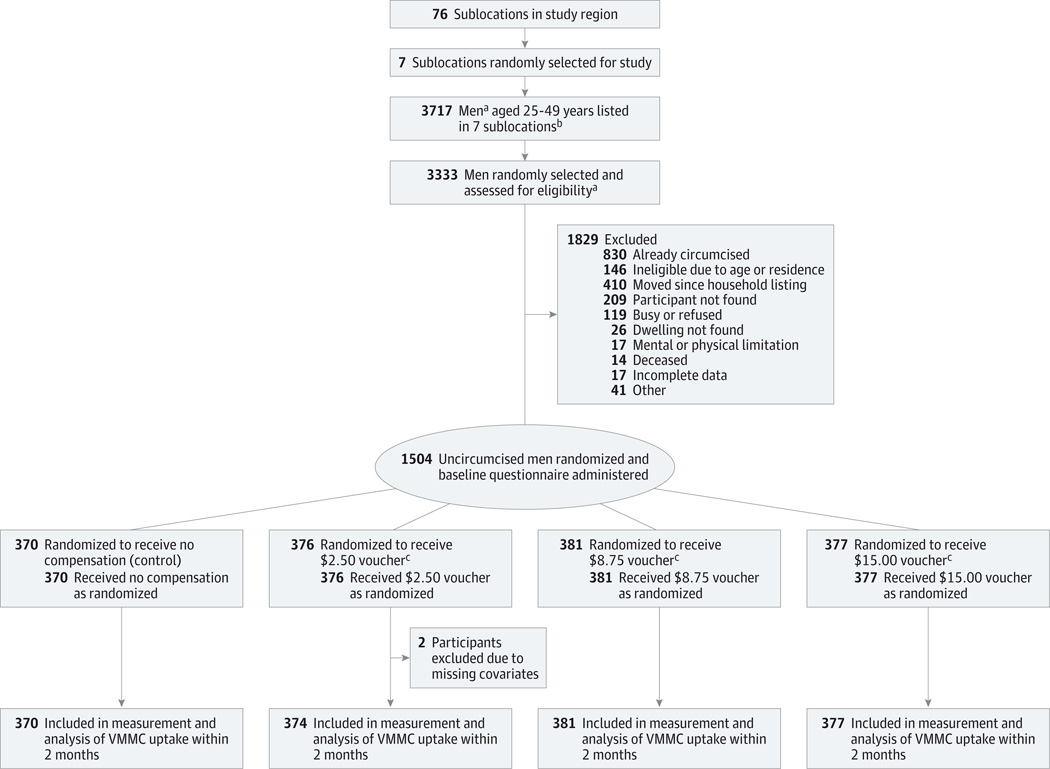
The study received approval from the Office of Human Research Ethics at the University of North Carolina at Chapel Hill and the ethics and research committee at Kenyatta National Hospital, University of Nairobi (trial protocol is provided in the Supplement). Seven of 76 sublocations in the study area were first randomly selected using selection probabilities proportional to each sublocation’s population (Figure). Two of these sublocations were subsequently determined to have been subdivided since the 2009 Kenya Population and Housing Census, resulting in a total of 9 sublocations from which study participants were selected. Trained research assistants conducted a listing of households in the study sublocations from March 2013 through April 2013 and recorded names of all male household members aged 25 to 49 years.
Figure. Flow of Study Participants for Voluntary Medical Male Circumcision.
a Includes the listing of men as well as the subsequent random selection of men, which allowed for more than 1 man per household.
b Two sublocations were subsequently subdivided since the 2009 Kenya Population and Housing Census, resulting in 9 sublocations from which participants were selected.
c Participants received the voucher upon the condition of undergoing voluntary medical male circumcision (VMMC). Because of varying exchange rates, US dollar conversions (from Kenya shillings) are approximate.
A random sample of men who were listed was then selected for home visits by research assistants, which took place from June 22, 2013, to December 4, 2013. Initially a random sample of 2100 men was selected and subsequently additional men were randomly selected to serve as replacements until the study had enrolled the target number of men who met eligibility criteria. Research assistants attempted to contact the randomly selected men and recruit those who met eligibility criteria: self-reported age between 25 and 49 years, self-reported to be uncircumcised, and with no intention to leave the study area in the next 3 months. The trained research assistants, who were fluent in Kiswahili and Dholuo (the 2 languages that are spoken in the study region), obtained written informed consent from the participants. Afterwards, the eligible participants were administered a brief questionnaire, provided with general information about the risks and benefits of VMMC, and then randomized in a 1:1:1:1 ratio to 1 of the 4 study groups. Randomization was performed using computer-generated scratch cards and balanced block randomization (block size, 100). Scratch cards were offered to participants sequentially and revealed the study group assignment to the participant and research assistant at the same time. The cards also served as referrals for undergoing circumcision so that VMMC uptake could be recorded at clinics. Unless participants voluntarily chose to seek VMMC services at IRDO clinics in the study area, they had no further contact with research assistants after the enrollment visit.
Interventions
All participants received information about 9 IRDO clinics in the study area where VMMC services were available free of charge, as is the case in most of Kenya. Participants in the control group received no economic compensation if they underwent circumcision at one of the clinics. Participants randomized to the 3 intervention groups were informed that they would receive food vouchers worth 200 Kenya shillings (≈US $2.50), 700 Kenya shillings (≈US $8.75), or 1200 Kenya shillings (≈US $15.00) if they underwent circumcision at one of the clinics within 2 months. These amounts approximated transportation costs from participants’ homes to a clinic or dispensary (≈US $2.50); transportation costs plus 1 to 2 days’ wages for most men based on the interquartile range (IQR) of study participants’ daily wages (≈US $8.75); and transportation costs plus 2 to 3 days’ wages for most men based on the IQR of study participants’ daily wages (≈US $15.00). Importantly, the largest food voucher amount was comparable to likely costs associated with circumcision in order to minimize the risk of coercion. The duration of time that the compensation offer remained valid was 2 months because this study sought to rapidly determine the acceptability, feasibility, and short-term effectiveness of the interventions. Food vouchers were selected as the form of compensation because of concerns about the potential for social harms that could result from distributing cash. The food vouchers listed 12 shops in the study area where they could be redeemed.
When developing the interventions, researchers for this study consulted with various community stakeholders and national and provincial VMMC task forces. Support was also obtained from the local Ministry of Health officials and a community advisory board.
VMMC Uptake Data Collection
VMMC uptake was monitored at study clinics until February 4, 2014. All participants were asked to present their scratch cards to a study research assistant at the IRDO clinics if they decided to uptake VMMC within 2 months of enrollment. Participants in the 3 intervention groups were offered the food vouchers by study research assistants immediately after the circumcision procedure, which the research assistants verified by consulting with surgeons at the clinic. Research assistants also verified the participants’ identity with national identification cards or another form of identification. VMMC uptake was also verified at the end of the study by comparing names of participants with names appearing on official VMMC registers maintained by IRDO. No discrepancies in VMMC uptake were found in this comparison.
Statistical Analyses
The primary, prespecified outcome was VMMC uptake within 2 months of enrollment. The outcome was coded as a binary variable equal to 1 if the participant underwent circumcision at study clinics within 2 months of enrollment and 0 if the participant did not. The primary analysis compared VMMC uptake in each intervention group to the control group using logistic regression. A Wald test was performed to compare the coefficients for the US $8.75 and US $15.00 groups. The analysis also estimated logistic regression models that adjusted for participants’ age, educational attainment, marital status, and wealth. Age was defined as a categorical variable with 5-year age categories (using age 25–29 years as the reference standard); and education was defined as a categorical variable indicating different levels of school completion (using less primary school attainment as the reference standard). Marital status was defined as a binary variable to indicate whether the participant was married. Participants’ wealth was measured by an asset index defined as the sum of affirmative responses to ownership of 11 household items. Participants with missing information on these covariates were excluded from the analyses.
In secondary analyses, VMMC uptake among participants in the US $8.75 and US $15.00 groups (those receiving high compensation) was compared with uptake among participants in the control and US $2.50 groups (low compensation) using logistic regression. Subgroup analyses were conducted to determine the effects of providing high compensation to participants with certain demographic and socioeconomic characteristics, self-reported sexual behavior or HIV risk, and attitudes toward circumcision. Subgroup analyses included significance testing of the subgroup-intervention interaction term in logistic regression models that also adjusted for the covariates described above. All statistical tests were 2-sided and significance was set at a P value of less than .05. Statistical analyses were performed using Stata version 13.1 (StataCorp).
The planned sample size for the trial was 1500, with 375 participants in each study group. Power calculations indicated that with a sample size of 375 per study group and 10% VMMC uptake in the control group, there would be 90% power to detect a difference in uptake as small as 9% and 80% power to detect a difference in uptake as small as 7%. At the time that power calculations were performed, there were no data available to our knowledge on the incidence of VMMC uptake among 25- to49-year-old men in the study region. This study was powered to detect a 7% to 9% difference in circumcision uptake because it was thought that this would constitute a large enough increase to be significant from a policy standpoint. Informal discussions with VMMC implementing organizations and policy makers led authors for this study to believe that such an effect size within a 2-month period would warrant consideration for scale-up of the intervention.
Results
Participant Recruitment and Flow
A total of 3717 men aged 25 to 49 years were listed in study sublocations and 3333 of these men were randomly sampled and assessed for eligibility and enrollment. Among the 3333 men, 1504 were enrolled and randomized to the 4 study groups (Figure). Enrollment of uncircumcised participants required considerable effort because many men did not meet eligibility criteria; 830 reported already being circumcised and 146 did not meet self-reported age and residential criteria. Because a period of 3 to 8 months elapsed between household listing and enrollment, a larger than expected number of men had left the study area by the time of enrollment (n = 410). Other reasons for nonenrollment included difficulty locating men at home (n = 209) and being busy or declining to participate (n = 119). Among the 2334 participants (1504 + 830) whose self-reported circumcision status was obtained, circumcision prevalence was 35.6% (830 of 2334). Two of the 1504 participants were excluded from the analyses due to missing information on covariates, resulting in an analysis sample of 1502 participants.
Baseline Data
Participants in the 4 study groups generally had similar characteristics at baseline (Table 1). Nearly all participants were from the Luo ethnic group, the largest in the region and one that is traditionally noncircumcising. Participants reported being economically active; mean hours worked in the past week were 47.1 (SD, 19.8) and median daily earnings were US $5.00 (IQR, $3.80–$7.50). Participants’ self-reported sexual behavior and male circumcision attitudes were similar in all study groups (Table 2). The vast majority of participants (68%) reported the possibility of being unable to work temporarily as their greatest concern about getting circumcised, 15% reported fear of pain, and 16% reported other factors.
Table 1.
Baseline Characteristics of Study Participants
| Study Group | Full Sample (n = 1502) |
||||
|---|---|---|---|---|---|
| Control (n = 370) |
US $2.50a (n = 374) |
US $8.75a (n = 381) |
US $15.00a (n = 377) |
||
| Age, mean (SD), y | 34.1 (6.7) | 34.2 (6.7) | 34.8 (6.5) | 34.4 (6.7) | 34.4 (6.7) |
| Wealth based on asset index, mean (SD)b | 3.0 (1.5) | 3.0 (1.5) | 3.1 (1.5) | 3.0 (1.5) | 3.0 (1.5) |
| Hours worked in past week, mean (SD) | 46.9 (20.1) | 46.6 (19.5) | 48.0 (19.4) | 47.1 (19.8) | 47.1 (19.8) |
| Daily earnings, median (IQR), US $a | 5.0 (3.8–7.1) | 5.0 (3.1–7.5) | 6.3 (3.8–7.5) | 5.0 (3.8–7.5) | 5.0 (3.8–7.5) |
| Distance to nearest clinic, median (IQR), km | 5.6 (4.6–7.3) | 5.7 (4.6–7.6) | 5.8 (4.6–7.8) | 6.0 (4.6–7.9) | 5.7 (4.6–7.7) |
| Education, No. (%) | |||||
| Some primary education or none | 113 (31) | 99 (26) | 104 (27) | 99 (26) | 415 (28) |
| Completed primary education | 112 (30) | 125 (33) | 122 (32) | 124 (33) | 483 (32) |
| Some secondary education | 49 (13) | 53 (14) | 46 (12) | 48 (13) | 196 (13) |
| Completed secondary or greater | 96 (26) | 97 (26) | 109 (29) | 106 (28) | 408 (27) |
| Married, No. (%) | 317 (86) | 293 (78) | 332 (87) | 324 (86) | 1266 (84) |
| Luo ethnicity, No. (%) | 370 (100) | 373 (100) | 381 (100) | 375 (99) | 1499 (100) |
Abbreviations: IQR, interquartile range.
Because of varying exchange rates, US dollar conversions (from Kenya shillings) are approximate.
Wealth was measured using an asset index defined as the sum of affirmative responses to questions about ownership of 11 household items.
Table 2.
Attitudes Related to Demand for VMMC and Self-reported Sexual Behavior
| No. (%) | |||||
|---|---|---|---|---|---|
| Study Group | Full Sample | ||||
| Control | US $2.50a | US $8.75a | US $15.00a | ||
| Sexual risk behavior | |||||
| Have a primary sex partner | 343 (93) | 337 (90) | 354 (93) | 352 (93) | 1386 (92) |
| Had any other sex partner besides primary in past year | 54 (15) | 60 (16) | 57 (15) | 58 (15) | 229 (15) |
| Condom used at last intercourse | 94 (25) | 83 (22) | 84 (22) | 92 (25) | 353 (24) |
| No. of lifetime partners, median (IQR) | 5 (3–8) | 5 (3–10) | 6 (3–10) | 5 (3–10) | 5 (3–10) |
| Self-reported chance of having HIV | |||||
| HIV-infected | 19 (5) | 19 (5) | 16 (4) | 11 (3) | 65 (4) |
| High | 83 (22) | 76 (20) | 67 (18) | 76 (20) | 302 (20) |
| Moderate | 168 (45) | 173 (46) | 177 (46) | 178 (47) | 696 (46) |
| Low | 48 (13) | 49 (13) | 53 (14) | 66 (18) | 216 (14) |
| No risk at all | 26 (7) | 21 (6) | 32 (8) | 20 (5) | 99 (7) |
| Circumcision knowledge | |||||
| Chance of HIV reduced with circumcision | 309 (84) | 317 (85) | 328 (86) | 319 (85) | 1273 (85) |
| Circumcised men less likely to get HIV | 301 (88) | 289 (86) | 316 (88) | 329 (93) | 1235 (89) |
| Likelihood of getting circumcised sometime in the future | |||||
| Definitely yes | 94 (26) | 85 (23) | 91 (25) | 89 (24) | 359 (25) |
| Maybe | 221 (61) | 221 (61) | 223 (60) | 221 (61) | 886 (61) |
| Unlikely | 22 (6) | 24 (7) | 24 (6) | 27 (7) | 97 (7) |
| Definitely not | 26 (7) | 32 (9) | 33 (9) | 27 (7) | 118 (8) |
| Likelihood of getting circumcised if given a food voucher for compensation | |||||
| Very likely | 149 (41) | 122 (33) | 127 (34) | 155 (41) | 553 (37) |
| Somewhat likely | 139 (38) | 161 (44) | 168 (45) | 148 (40) | 616 (42) |
| Not very likely | 77 (21) | 85 (23) | 79 (21) | 71 (19) | 312 (21) |
| Minimum amount needed for a food voucher to compensate most men for circumcision costs, median (IQR), US $a | 31 (19–63) | 31 (19–50) | 31 (19–63) | 31 (15–50) | 31 (19–56) |
| Greatest concern about getting circumcised | |||||
| Cost of missed work | 240 (69) | 234 (68) | 239 (68) | 230 (66) | 943 (68) |
| Pain | 48 (14) | 54 (16) | 56 (16) | 56 (16) | 214 (15) |
| Other concern | 61 (17) | 52 (15) | 54 (15) | 59 (17) | 226 (16) |
Abbreviations: HIV, human immunodeficiency virus; IQR, interquartile range; VMMC, voluntary medical male circumcision.
Because of varying exchange rates, US dollar conversions (from Kenya shillings) are approximate.
Effect on VMMC Uptake
Table 3 shows that 2-month VMMC uptake was higher among participants randomized to receive compensation of approximately US $8.75 (6.6%; 95% CI, 4.3%–9.5% [25 of 381]) or approximately US $15.00 (9.0%; 95% CI, 6.3%–12.4% [34 of 377]). The VMMC uptake in the US $2.50 group (1.9%; 95% CI, 0.8%–3.8% [7 of 374]) was similar to uptake in the control group (1.6%; 95% CI, 0.6%–3.5% [6 of 370]). A mean of 26 days elapsed between enrollment in the study and VMMC uptake (SD, 23 days).
Table 3.
Effects of Conditional Economic Compensation on VMMC Uptake Within 2 Months
| Study Group |
P Value for Test of Equalityb |
||||
|---|---|---|---|---|---|
| Control | US $2.50a | US $8.75a | US $15.00a | ||
| No. of participants | 370 | 374 | 381 | 377 | |
| Circumcised | |||||
| No. | 6 | 7 | 25 | 34 | |
| % (95% CI) | 1.6 (0.6–3.5) | 1.9 (0.8–3.8) | 6.6 (4.3–9.5) | 9.0 (6.3–12.4) | |
| Unadjustedc | |||||
| OR (95% CI) | 1 [Reference] | 1.2 (0.4–3.5) | 4.3 (1.7–10.5) | 6.0 (2.5–14.5) | .21 |
| P value | .80 | .002 | <.001 | ||
| Adjustedd | |||||
| OR (95% CI) | 1 [Reference] | 1.1 (0.4–3.3) | 4.3 (1.7–10.7) | 6.2 (2.6–15.0) | .20 |
| P value | .87 | .002 | <.001 | ||
Abbreviations: OR, odds ratio; VMMC, voluntary medical male circumcision.
Because of varying exchange rates, US dollar conversions (from Kenya shillings) are approximate.
P value from Wald test of equality between US $8.75 group and US $15.00 group.
Results from logistic regression model of VMMC uptake with indicators of study group (control group as the reference standard).
Results from logistic regression model with indicators of study group and controls for age, education, wealth, and marital status.
Logistic regression analysis of VMMC uptake (Table 3) indicated that compared with participants in the control group, those in the US $15.00 group were significantly more likely to get circumcised within 2 months (OR, 6.0; 95% CI, 2.5–14.5). Participants in the US $8.75 group were also significantly more likely to uptake VMMC (OR, 4.3; 95% CI, 1.7–10.5). Those enrolled in the US $2.50 group, however, were not significantly more likely to uptake VMMC (OR, 1.2; 95% CI, 0.4–3.5). The effect sizes of the US $8.75 and US $15.00 groups did not differ significantly (P = .21). Results from the adjusted logistic regression analysis were similar, with significant increases in the likelihood of VMMC uptake among those in the US $15.00 and US $8.75 groups (AOR, 6.2; 95% CI, 2.6–15.0 and AOR, 4.3; 95% CI, 1.7–10.7, respectively). There were no adverse events reported in any of the study groups. Examples of adverse events related to the study would have included cases in which participants felt coerced to undergo circumcision or negative rumors about the intervention that would have led to participants suffering social harm.
Subgroup Analyses
The results in Table 3 were used as the basis for combining participants receiving low compensation (control and US $2.50 groups, in which VMMC uptake was similar) or high compensation (US $8.75 and US $15.00 groups, in which VMMC uptake was higher and also similar) and then comparing the effectiveness of providing high compensation in participant subgroups that had different characteristics. Participants offered high compensation were significantly more likely to become circumcised than participants offered low compensation (Table 4; AOR, 5.0; 95% CI, 2.7–9.2). Among all subgroups examined in this study, provision of high compensation significantly increased the likelihood of getting circumcised. This included married participants (AOR, 4.5; 95% CI, 2.3–9.1), participants older than age 33 years (AOR, 7.9; 95% CI, 2.7–22.7), as well as participants who self-reported having any other sex partner besides the primary in the past year at baseline (AOR, 11.8; 95% CI, 1.4–98.7). The intervention also significantly increased the likelihood of circumcision among participants who self-reported a low likelihood of getting circumcised in the near future (AOR 7.8; 95% CI, 3.0–20.2). There were no statistically significant interactions within any of the analyzed subgroups (Table 4).
Table 4.
Comparison of Intervention Effectiveness in Participant Subgroups
| VMMC Uptake (%) | Effect of High Compensationa |
P Value for Interactionc |
|||
|---|---|---|---|---|---|
| Low Compensation (Control or US $2.50)b |
High Compensation (US $8.75 or US $15.00)b |
||||
| No./Total No. (%) | No./Total No. (%) | AOR (95% CI) | P Value | ||
| Circumcised | 13/744 (1.7) | 59/758 (7.8) | 5.0 (2.7–9.2) | <.001 | |
| Marital status | |||||
| Not married | 3/134 (2.2) | 14/102 (13.7) | 7.5 (2.0–28.0) | .003 | .55 |
| Married | 10/610 (1.6) | 45/656 (6.9) | 4.5 (2.3–9.1) | <.001 | |
| Age, y | |||||
| ≤33 | 9/365 (2.5) | 30/355 (8.5) | 3.9 (1.8–8.4) | .001 | .30 |
| >33 | 4/379 (1.1) | 29/403 (7.2) | 7.9 (2.7–22.7) | <.001 | |
| Daily incomeb | |||||
| ≤US $5.00 | 7/394 (1.8) | 37/374 (9.9) | 6.1 (2.7–14.0) | <.001 | .37 |
| >US $5.00 | 6/350 (1.7) | 22/383 (5.7) | 4.0 (1.6–10.1) | .004 | |
| Had any other sex partner besides primary in past year | |||||
| No | 12/628 (1.9) | 49/643 (7.6) | 4.5 (2.3–8.6) | <.001 | .39 |
| Yes | 1/114 (0.9) | 10/115 (8.7) | 11.8 (1.4–98.7) | .023 | |
| Self-reported chance of having HIV/AIDS | |||||
| Low/no risk | 9/500 (1.8) | 36/536 (6.7) | 4.3 (2.0–9.0) | <.001 | .70 |
| Moderate/high | 4/197 (2.0) | 16/170 (9.4) | 6.6 (2.0–21.3) | .002 | |
| Likelihood of getting circumcised sometime in the future | |||||
| Definitely not/probably not/maybe | 5/546 (0.9) | 35/555 (6.3) | 7.8 (3.0–20.2) | <.001 | .16 |
| Definitely yes | 8/179 (4.5) | 23/180 (12.8) | 3.3 (1.4–7.7) | .006 | |
| Likelihood of getting circumcised if given a food voucher for compensation | |||||
| Not/somewhat likely | 5/462 (1.1) | 26/466 (5.6) | 5.1 (1.9–13.6) | .001 | .71 |
| Very likely | 8/271 (3.0) | 33/282 (11.7) | 4.7 (2.1–10.5) | <.001 | |
Abbreviations: AOR, adjusted odds ratio; VMMC, voluntary medical male circumcision.
Results are from logistic regression model of VMMC uptake with indicator of the high-compensation group (low-compensation group as the reference standard) and controls for age, wealth, education, and marital status. Each AOR is for the high-compensation group when sample is restricted to the specific subgroup defined in the first column.
Because of varying exchange rates, US dollar conversions (from Kenya shillings) are approximate.
P value is for interaction between subgroup and the high-compensation group in logistic regression model, which includes all observations within each group and indicator of the high-compensation group (low-compensation group as the reference standard) as well as controls for age, wealth, education, and marital status.
Discussion
This study demonstrates that incentives were effective in increasing VMMC uptake because participants offered compensation in the form of food vouchers worth approximately US $15.00 and approximately US $8.75 were significantly more likely to become circumcised within 2 months than participants in the control group. There was also a significant increase in VMMC uptake among married and older participants, groups that have been harder to reach previously. The interventions also significantly increased the likelihood of circumcision uptake among participants at higher risk of acquiring HIV. This latter result is especially promising from an HIV-prevention standpoint. The overall increase in VMMC uptake within 2 months, as a result of providing compensation, was modest, with an increase of at most 7.4% in the US $15.00 group. This increased uptake was in a population with an estimated circumcision prevalence of 35.6%. Evaluation of scaled-up implementation of the intervention is needed to determine whether it will help achieve higher circumcision coverage over longer periods of time.
This study adds to an as yet small evidence base on effective strategies to create demand for male circumcision. Although a number of qualitative studies and a few quantitative studies have examined stated barriers to and facilitators of VMMC demand in sub-Saharan Africa,11,17,18 none have tested specific individual-level interventions to create demand. While one study has shown that prices for VMMC services may influence demand,19 the study reported herein is unique in testing the effect of economic incentives on demand for VMMC. In light of the fact that VMMC services are already provided free of charge in many priority countries in sub-Saharan Africa and that economic factors continue to be reported as a barrier to VMMC uptake, the intervention tested here is one that has considerable relevance and applicability for countries and programs seeking ways to increase circumcision prevalence. The study also strengthens our broader understanding of how economic incentives can promote HIV-related health behaviors by addressing economic barriers and decision-making errors identified in behavioral economics. Incentives have previously been used to promote various health and education behaviors in low-income countries,14,15,20 and recently their use has also been shown to reduce HIV and sexually transmitted infection prevalence.21 However, despite growing interest in using incentives to promote HIV-related behaviors such as HIV testing uptake, linkage to HIV care, and retention in care, evidence from randomized trials has been limited.22–26 This study illustrates the strengths and limitations of using incentives as a strategy for modifying such behaviors and preventing new HIV infections.
From a policy standpoint, an appealing feature of the intervention implemented in this study is that most of the costs (the compensation amounts) would be incurred only if circumcision uptake occurs. While a cost-effectiveness analysis was beyond the scope of this study, the intervention is likely to be highly cost effective given estimates that 1 HIV infection can be averted for every 5 to 15 VMMCs performed and given lifetime HIV treatment costs.27–29 The sustainability of the intervention is also enhanced because it is for a 1-time behavior rather than a recurring health behavior. The 1-time compensation amounts in the study, which equated to roughly 1 to 3 days of wages in the case of the US $8.75 and US $15.00 vouchers as well as transportation costs, compare favorably to the amounts used in other studies of incentives to modify health behavior. In high-income countries, comparable amounts, adjusting for relative income levels, have been used to promote behaviors such as smoking cessation (≈US $750 over 12 months).30 In low- and middle-income countries, considerably larger amounts of transfers have been used to incentivize children’s school attendance and health behaviors in conditional cash transfer programs, ranging from approximately 25% to 44% of poor households’ incomes in rural areas of Mexico (Progresa and Oportunidades programs) to approximately US $10.00 per household on a monthly basis in Malawi.21,31,32 Although it is difficult to draw comparisons across behaviors and settings, these examples provide context for the compensation amounts used in this study. Finally, there are multiple reasons why offering compensation amounts of approximately US $8.75 or approximately US $15.00 on a wider scale may result in larger effects on VMMC uptake than observed here. First, because this study aimed to rapidly ascertain whether the intervention was acceptable, feasible, and effective, a short VMMC uptake period of 2 months during which compensation was provided was intentionally chosen. It is plausible that a higher proportion of men would become circumcised if a scaled-up intervention offered compensation over a prolonged duration. Second, a scaled-up version of this intervention would presumably also include more promotion of it using mass media, which could in turn increase its effectiveness.
Despite these arguments, it remains possible that participants did not become circumcised because they faced other barriers to circumcision or found the compensation amounts to be inadequate in comparison to their costs associated with circumcision. The results provide some support for such explanations. At enrollment, barriers such as fear of pain or concern about female partners’ perceptions were stated by some participants. Moreover, the interventions were less effective among participants with above-median income and many participants initially recommended larger incentive amounts than US $15.00 for adequate compensation of costs associated with circumcision.
This study had several limitations. First, some men initially sampled as potential participants were not found at their homes or had migrated out of the study area. This was likely due to household listing of study sublocations occurring 3 to 8 months before enrollment, which means that our results may not apply to highly mobile men. Second, because of smaller sample sizes and limited statistical power, our comparisons of the interventions’ effect in different subgroups should be considered as exploratory. Third, the study did not examine whether alternative forms of conditional economic compensation (whether cash or noncash) could be equally or more effective in increasing VMMC uptake. Behavioral economics, for example, points to the potential for other forms of incentives—such as lottery-based rewards—to be more effective than small, fixed incentives.33,34 Additional testing of such strategies is needed. Finally, further testing is necessary to determine the generalizability of our intervention and results to settings outside Kenya. It is important to emphasize, for example, that the intervention would need to be accompanied by adequate supply of VMMC services and that a high background level of general knowledge and acceptability of VMMC, as was the case in our study setting due to prior efforts of the government and VMMC implementing organizations, may be required. To the extent that economic and behavioral barriers to VMMC uptake exist for many men, however, the results from this study should apply in these other settings.
Ethical considerations must also be taken into account when using economic incentives to promote health behaviors such as male circumcision. Although an exhaustive discussion of these issues falls outside the scope of this study, there are several reasons why the intervention in this study is ethically sound. First, based on participants’ reported wages, the modest amounts we used compensated participants for only part of the costs they would likely incur as a result of becoming circumcised. In fact, most men indicated that the appropriate voucher amounts to offset the economic costs associated with male circumcision were even higher than the amounts we offered. Second, in light of the health externality benefits of male circumcision such as secondary HIV prevention, the provision of modest incentives in this case has a more compelling rationale than it would for behaviors with no externality benefits.
Conclusions
Among uncircumcised men in Kenya, compensation in the form of food vouchers worth approximately US $8.75 or approximately US $15.00, compared with lesser or no compensation, resulted in a modest increase in the prevalence of circumcision after 2 months. The effects of more intense promotion or longer implementation require further investigation.
Supplementary Material
Acknowledgments
Funding/Support: The study was funded by the Bill and Melinda Gates Foundation (grant OPP1069673). Dr Thirumurthy reports receipt of support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant K01HD061605).
Role of the Sponsors: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Thirumurthy had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Thirumurthy, Lanham, Evens, Agot.
Acquisition, analysis, or interpretation of data: Thirumurthy, Masters, Rao, Bronson, Lanham, Omanga, Evens, Agot.
Drafting of the manuscript: Thirumurthy.
Critical revision of the manuscript for important intellectual content: Thirumurthy, Masters, Rao, Bronson, Lanham, Omanga, Evens, Agot.
Statistical analysis: Thirumurthy, Masters.
Obtained funding: Thirumurthy, Agot.
Administrative, technical, or material support: Thirumurthy, Rao, Lanham, Omanga, Evens, Agot.
Study supervision: Thirumurthy, Rao, Bronson, Omanga, Agot.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2(11):e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369(9562):657–666. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 3.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369(9562):643–656. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization and Joint United Nations Programme on HIV/AIDS. Geneva, Switzerland: World Health Organization; 2007. New Data on Male Circumcision and HIV Prevention: Policy and Programme Implications. [Google Scholar]
- 5.World Health Organization. Geneva, Switzerland: World Health Organization; 2011. Joint Strategic Action Framework to Accelerate the Scale-Up of Voluntary Medical Male Circumcision for HIV Prevention in Eastern and Southern Africa, 2012–2016. [Google Scholar]
- 6.Sgaier SK, Reed JB, Thomas A, Njeuhmeli E. Achieving the HIV prevention impact of voluntary medical male circumcision: lessons and challenges for managing programs. PLoS Med. 2014;11(5):e1001641. doi: 10.1371/journal.pmed.1001641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galbraith JS, Ochieng A, Mwalili S, et al. KAIS Study Group. Status of voluntary medical male circumcision in Kenya: findings from 2 nationally representative surveys in Kenya, 2007 and 2012. J Acquir Immune Defic Syndr. 2014;66(S1) suppl 1:S37–S45. doi: 10.1097/QAI.0000000000000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gray RH, Wawer MJ, Kigozi G. Programme science research on medical male circumcision scale-up in sub-Saharan Africa. Sex Transm Infect. 2013;89(5):345–349. doi: 10.1136/sextrans-2012-050595. [DOI] [PubMed] [Google Scholar]
- 9.Westercamp N, Bailey RC. Acceptability of male circumcision for prevention of HIV/AIDS in sub-Saharan Africa: a review. AIDS Behav. 2007;11(3):341–355. doi: 10.1007/s10461-006-9169-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herman-Roloff A, Otieno N, Agot K, Ndinya-Achola J, Bailey RC. Acceptability of medical male circumcision among uncircumcised men in Kenya one year after the launch of the national male circumcision program. PLoS One. 2011;6(5):e19814. doi: 10.1371/journal.pone.0019814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evens E, Lanham M, Hart C, Loolpapit M, Oguma I, Obiero W. Identifying and addressing barriers to uptake of voluntary medical male circumcision in Nyanza, Kenya among men 18–35: a qualitative study. PLoS One. 2014;9(6):e98221. doi: 10.1371/journal.pone.0098221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298(20):2415–2417. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- 13.O’Donoghue T, Rabin M. Doing it now or later. Am Econ Rev. 1999;89(1):103–124. [Google Scholar]
- 14.Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA. 2007;298(16):1900–1910. doi: 10.1001/jama.298.16.1900. [DOI] [PubMed] [Google Scholar]
- 15.Sindelar JL. Paying for performance: the power of incentives over habits. Health Econ. 2008;17(4):449–451. doi: 10.1002/hec.1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National AIDS and STI Control Programme. Nairobi, Kenya: Ministry of Health; 2013. Kenya AIDS Indicator Survey 2012: Preliminary Report. [Google Scholar]
- 17.Hatzold K, Mavhu W, Jasi P, et al. Barriers and motivators to voluntary medical male circumcision uptake among different age groups of men in Zimbabwe: results from a mixed methods study. PLoS One. 2014;9(5):e85051. doi: 10.1371/journal.pone.0085051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Macintyre K, Andrinopoulos K, Moses N, et al. Attitudes, perceptions and potential uptake of male circumcision among older men in Turkana County, Kenya using qualitative methods. PLoS One. 2014;9(5):e83998. doi: 10.1371/journal.pone.0083998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chinkhumba J, Godlonton S, Thornton R. The demand for medical male circumcision. American Economic Journal: Applied Economics. 2014;6(2):152–177. [Google Scholar]
- 20.Banerjee AV, Duflo E, Glennerster R, Kothari D. Improving immunisation coverage in rural India: clustered randomised controlled evaluation of immunisation campaigns with and without incentives. BMJ. 2010;340:c2220. doi: 10.1136/bmj.c2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baird SJ, Garfein RS, McIntosh CT, Ozler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379(9823):1320–1329. doi: 10.1016/S0140-6736(11)61709-1. [DOI] [PubMed] [Google Scholar]
- 22.Lee R, Cui RR, Muessig KE, Thirumurthy H, Tucker JD. Incentivizing HIV/STI testing: a systematic review of the literature. AIDS Behav. 2014;18(5):905–912. doi: 10.1007/s10461-013-0588-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thornton RL. The demand for, and impact of, learning HIV status. Am Econ Rev. 2008;98(5):1829–1863. doi: 10.1257/aer.98.5.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bjorkman-Nyqvist M, Corno L, DeWalque D, Svensson J. Evaluating the impact of short term financial incentives on HIV and STI incidence among youth in Lesotho: a randomized trial; Proceedings from the 7th IAS Conference on HIV Pathogenesis, Treatment, and Prevention; June 30-July 3, 2013; Kuala Lumpur, Malaysia. [Google Scholar]
- 25.Operario D, Kuo C, Sosa-Rubí SG, Gálarraga O. Conditional economic incentives for reducing HIV risk behaviors: integration of psychology and behavioral economics. Health Psychol. 2013;32(9):932–940. doi: 10.1037/a0032760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.deWalque D, Dow WH, Nathan R, et al. Incentivising safe sex: a randomised trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ Open. 2012;2:e000747. doi: 10.1136/bmjopen-2011-000747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.UNAIDS/WHO/SACEMA Expert Group on Modelling the Impact and Cost of Male Circumcision for HIV Prevention. Male circumcision for HIV prevention in high HIV prevalence settings: what can mathematical modelling contribute to informed decision making? PLoS Med. 2009;6(9):e1000109. doi: 10.1371/journal.pmed.1000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Njeuhmeli E, Forsythe S, Reed J, et al. Voluntary medical male circumcision: modeling the impact and cost of expanding male circumcision for HIV prevention in eastern and southern Africa. PLoS Med. 2011;8(11):e1001132. doi: 10.1371/journal.pmed.1001132. [published online November 29, 2011]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Auvert B, Marseille E, Korenromp EL, et al. Estimating the resources needed and savings anticipated from roll-out of adult male circumcision in Sub-Saharan Africa. PLoS One. 2008;3(8):e2679. doi: 10.1371/journal.pone.0002679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Volpp KG, Troxel AB, Pauly MV, et al. A randomized, controlled trial of financial incentives for smoking cessation. N Engl J Med. 2009;360(7):699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- 31.Schultz TP. School Subsidies for the Poor: Evaluating the Mexican Progresa Poverty Program. J Dev Econ. 2004;74(1):199–250. [Google Scholar]
- 32.Levy S. Progress Against Poverty: Sustaining Mexico’s Progresa-Oportunidades Program. Washington, DC: Brookings Institution; 2006. [Google Scholar]
- 33.Loewenstein GF, Weber EU, Hsee CK, Welch N. Risk as feelings. Psychol Bull. 2001;127(2):267–286. doi: 10.1037/0033-2909.127.2.267. [DOI] [PubMed] [Google Scholar]
- 34.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA. 2008;300(22):2631–2637. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.