Abstract
Background:
Ulnar nerve blockade as a component of wrist block is a promising technique for adequate anesthesia and analgesia for different surgeries of the hand. Due to anatomical variations in the location of ulnar nerve under the flexor carpi ulnaris (FCU) a technique with good results and minimal complications are required.
Aim:
The aim of the following study is to compare the three techniques (volar, transtendinous volar [TTV] and ulnar) for ulnar nerve block at the wrist in human cadaveric wrists.
Materials and Methods:
Our study was conducted using 40 cadaver wrists. After inserting standard hypodermic needles by three techniques for ulnar nerve blockade at the wrist, a detailed dissection of FCU was done. The mean distance from the tip of the needle to ulnar artery/nerve and number of instances in which the ulnar artery/nerve pierced were observed.
Results:
Inter-group statistical significance was observed in measurement of the mean distance (mm) from the tip of the needle to the ulnar artery (volar [0.92 ± 0.11], TTV [3.96 ± 0.14] and ulnar [7.14 ± 0.08] approaches) and ulnar nerve (volar/TTV/ulnar approaches were 0.71 ± 0.12/3.61 ± 0.10/6.31 ± 0.49, respectively) (P = 0.001). Inadvertent intra-arterial/intraneural injections was seen with volar approach in 14 (35%) and 16 (40%) of the cadaveric wrists respectively, statistically significant with transtendinous and ulnar techniques of ulnar nerve block.
Conclusion:
TTV approach could be a better technique of choice for ulnar nerve blockade at the wrist because of its ease to practice, safer profile and minimum chances of inadvertent intra-arterial/intraneural injection with adequate anesthesia/analgesia.
Keywords: Ulnar nerve, ulnar nerve block, wrist block
INTRODUCTION
Ulnar nerve is a branch of medial cord of brachial plexus with a root value of C8-T1.[1] This nerve passes superficially to the flexor retinaculum and enters the palm of the hand through the Guyon's canal. In the hand, it gives motor (hypothenar, 3rd/4th lumbricals, palmar/dorsal interossei muscles) and sensory (fifth digit and the medial half of the fourth digit) innervations.[2]
Ulnar nerve blockade provides anesthesia and analgesia to the operative procedures of the little finger and also acts as a component of wrist block for the surgeries of the hand. It is also used to supplement a brachial plexus block and spares the patient from the complications of general anesthesia with excellent post-operative analgesia.[3] Brachial plexus block is associated with more motor anesthesia and particularly useful for long duration procedures where tourniquet anesthesia is also required. However, ulnar nerve block is advocated in procedures that do not require a tourniquet or last approximately <20 min.[4]
Because of variability in the location of ulnar nerve under the flexor carpi ulnaris (FCU),[5,6] a definite technique with promising results is a debatable issue. Classically, two approaches (volar/ulnar) had been described in the literature.[7] The deposition of anesthetic agent in the volar approach is between the tendon of FCU and the distal end of the ulna, while during ulnar approach the placement of the drug is posterior to the tendon of FCU.[7] However, none of the techniques completely eliminates the risk of intra-arterial/intraneural piercing.[8] Extensive Medline search revealed limited literature (an abstract) regarding the third approach (transtendinous volar, [TTV]) for ulnar nerve blockade.[9]
The aim behind our study is to compare the three above mentioned techniques for ulnar nerve block at the wrist in human cadavers. Such results could be applied judiciously on the patients posted for various operative procedures involving ulnar nerve block at the wrist with minimum inadvertent injections.
MATERIALS AND METHODS
We conducted our study using 40 cadaver wrists (22 males and 18 females). Identification of FCU was done proximal to the wrist crease and a standard hypodermic needle of 1.5 inch, 25 gauge was inserted into the right and left wrists of the non-dissected cadaver hands using the following standard techniques:
Volar technique
The needle was inserted perpendicular to the long axis of the arm at the proximal wrist crease along the lateral border of FCU.
TTV injection
The needle was inserted in the same axis as described in volar technique, but through the mid-portion of the FCU and we identified the traversing of the tendon by loss of resistance to the needle.
Ulnar injection
The needle was inserted parallel to the proximal wrist crease, just dorsal to the FCU and perpendicular to the long axis of the arm.
A detailed dissection was carried out for better visualization, in which FCU was separated and reflected back from its insertion. After visualizing the anatomical structures [Figure 1] following parameters were assessed in all techniques:
Figure 1.

Hypodermic needles showing techniques for ulnar nerve block on dissected wrists. Volar approach (1), transtendinous approach (2), ulnar approach (3), flexor carpi ulnaris (4), ulnar nerve (5), ulnar artery (6) are demonstrated
The mean distance from the tip of the needle to the ulnar nerve and artery.
Number of occasions in which the ulnar nerve or artery were pierced.
The measurements were taken with double tipped compass and then transferred to Vernier calipers (least count 0.01 mm) to measure the distances. The dimensions were taken three times by the same person and the mean was taken, thus increasing the accuracy of the data.
Statistical analysis
Data analysis was done using Statistical Package for Social Sciences version 19 (SPSS Inc., Chicago, IL, USA). The parametric data was analyzed by ANOVA while Chi-square/Fisher's test was applied on non-parametric data. Unless otherwise stated, data were presented as mean (standard deviation) and P < 0.05 was considered to be statistically significant.
RESULTS
Measurements were taken from all 40 carefully dissected cadaveric wrists. During dissection of soft tissues, different anatomical structures were easily identified.
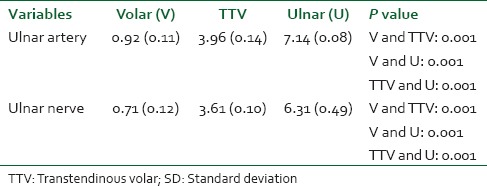
The mean distance (mm) from the tip of the needle to the ulnar artery in volar (0.92 ± 0.11), TTV (3.96 ± 0.14) and ulnar (7.14 ± 0.08) approaches were statistically significant between them (P = 0.001) [Table 1]. The mean dimensions (mm) between the tip of the needle to the ulnar nerve among volar/TTV/ulnar approaches were 0.71 ± 0.12/3.61 ± 0.10/6.31 ± 0.49 respectively (P = 0.001) [Table 1]. The mean values from the needle tip to the ulnar artery in all approaches were greater than ulnar nerve, implying that ulnar nerve was medial to the ulnar artery in most of the cases.
Table 1.
Mean distance (in mm) from the tip of the needle to ulnar artery/nerve (mean [SD])
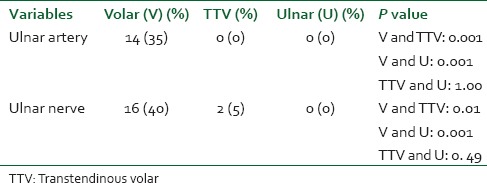
On passing the needle through volar approach, ulnar artery was punctured in 14 (35%) of the cadaveric wrists. No intra-arterial penetration was found in TTV or ulnar approaches. Statistical significance was observed between volar and TTV and volar and ulnar techniques (P = 0.001) [Figure 2 and Table 2]. Instances of intra-neural punctures in volar and TTV approaches were 16 (40%) and 2 (5%) of the cadaveric wrists respectively (P = 0.01) [Figure 2 and Table 2]. However, no needle penetration to the ulnar nerve was seen with ulnar approach.
Figure 2.
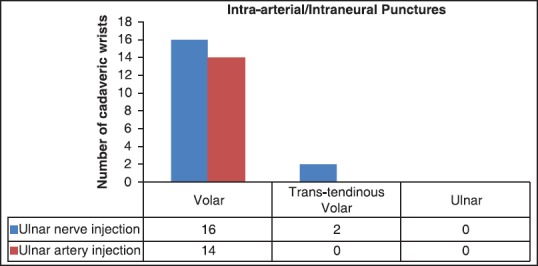
Number of occasions of intra-arterial/intraneural puntures
Table 2.
Instances (n/40) of ulnar artery/nerve puncture
DISCUSSION
Our study reveals that the mean distances between the tip of the needle to the medial aspect of ulnar nerve was smaller than the distance to the ulnar artery in different techniques of ulnar nerve blockade. This supports the established fact that ulnar nerve is lateral to the tendon of FCU and medial to the ulnar artery at the wrist.[10,11] The dimension from the needle tip to the ulnar nerve was significantly large in ulnar approach (6.31 ± 0.49 mms) compared to volar (0.71 ± 0.12 mms) and TTV (3.61 ± 0.10 mms) techniques (P = 0.001). This implies that the chance of the ulnar artery perforation was negligible with the ulnar approach provided the needle tip behind the lateral side of the tendon of FCU should not penetrate beyond 6-7 mms medially. However, TTV injection is a better alternative than other approaches as its closer proximity to the ulnar nerve warrants adequate anesthesia and analgesia and less inadvertent intra-arterial injection risk.
A minimal amount of bleeding at Guyon's canal can increase its pressure and finally resulting in compartment syndrome, so an appropriate approach for ulnar nerve block having minimal arterial puncture threat is essential. In our study, ulnar artery was injured in 14 (35%) wrists via volar technique which was significantly higher than ulnar/TTV approaches (P = 0.001). TTV and ulnar techniques provides significant safeguard against intra-arterial injection (P = 1.00). The higher incidences of the ulnar artery puncture, while a volar approach compared with other techniques could be attributed due to the close association of the ulnar artery with ulnar nerve.[12]
The possibility of inadvertent intraneural injection during volar technique was encountered in 16 (40%) wrists, which was statistically significant than other approaches (P = 0.001). Although the risk of neural injury was 5% via TTV approach, but it is statistically insignificant on comparing with ulnar technique (P = 0. 49). The uniqueness of our study was an assessment of the risk of intraneural injection via different techniques for ulnar nerve blockade. The above data could direct an anesthetist for eliminating the risk of ulnar nerve injury, particularly when the patient is under general anesthesia and culminating the possibility of eliciting paraesthesia. However, the medical professionals have to be prudent enough, while applying ulnar block by either of the techniques on a patient asleep, as anatomical variations are always possible.
Now-a-days, nerve stimulators and ultrasonography are being used for the application of ulnar nerve blockade. Nerve stimulators had been claimed to reduce the incidence of nerve damage by avoiding the need to elicit paraesthesia, although this is controversial.[13] Most practitioners do not electro-locate the ulnar nerve with such a low intensity (<0.5 mA) and it also carries a risk of neural puncture.[13] Macaire et al.[14] in their study found a higher incidence of intraneural injection in the neurostimulation group and supported the use of ultrasound for ulnar nerve blockade. Although, ultrasound guidance for regional blocks provides direct vision of neurovascular structures and reduces the incidence of direct needle trauma to nerves and vessels, but it carries the disadvantages of expertise, availability, and cost issues.[15]
A limitation of our cadaveric study is that an important landmark, which is used under clinical settings, palpable pulsating ulnar artery could not be used. Anesthetists use this landmark for locating the ulnar nerve lying medial to the ulnar artery. Our findings would be helpful for successful ulnar nerve block in patients where ulnar artery is difficult to palpate like in obese and chronic smokers.[16]
Lizamore et al.[8] witnessed the use of ulnar approach for nerve blockade in peripheral set-ups, due to the fact that TTV approach was not included in their study. We highlight TTV approach for ulnar nerve anesthesia/analgesia at wrist a preferred technique under rural settings as it could be easily applied and skilled by the medical professionals.
CONCLUSION
This study advocates the use of TTV approach a better technique for ulnar nerve blockade compared to ulnar and volar methods. TTV approach carries a safer profile by decreasing intra-arterial/intraneural injections, its ease of applicability and learning by residents advocates the use of such approach for adequate ulnar nerve anesthesia/analgesia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bekler H, Wolfe VM, Rosenwasser MP. A cadaveric study of ulnar nerve innervation of the medial head of triceps brachii. Clin Orthop Relat Res. 2009;467:235–8. doi: 10.1007/s11999-008-0535-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Polatsch DB, Melone CP, Jr, Beldner S, Incorvaia A. Ulnar nerve anatomy. Hand Clin. 2007;23:283–9. doi: 10.1016/j.hcl.2007.05.001. v. [DOI] [PubMed] [Google Scholar]
- 3.Brown AR. Anesthesia for procedures of the hand and elbow. Best Pract Res Clin Anaesthesiol. 2002;16:227–46. doi: 10.1053/bean.2002.0235. [DOI] [PubMed] [Google Scholar]
- 4.Delaunay L, Chelly JE. Blocks at the wrist provide effective anesthesia for carpal tunnel release. Can J Anaesth. 2001;48:656–60. doi: 10.1007/BF03016199. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan EB. Variation of the ulnar nerve at the wrist. Bull Hosp Joint Dis. 1963;24:85–8. [PubMed] [Google Scholar]
- 6.König PS, Hage JJ, Bloem JJ, Prosé LP. Variations of the ulnar nerve and ulnar artery in Guyon's canal: A cadaveric study. J Hand Surg Am. 1994;19:617–22. doi: 10.1016/0363-5023(94)90270-4. [DOI] [PubMed] [Google Scholar]
- 7.Leversee JH, Bergman JJ. Wrist and digital nerve blocks. J Fam Pract. 1981;13:415–21. [PubMed] [Google Scholar]
- 8.Lizamore N, Venter E, Boon JM. Alternative approaches for regional ulnar nerve blockade: A cadaveric study. Clin Anat. 2004;17:373–7. doi: 10.1002/ca.10247. [DOI] [PubMed] [Google Scholar]
- 9.Moon ES, Iannuzzi N, Hanel DP. Comparison of three injection techniques for ulnar nerve blocks at the wrist: A cadaveric study. Abstract for American Academy for Orthopaedic Surgery Annual Meeting. 2012;2:795–6. [Google Scholar]
- 10.Mauldin CC, Brooks DW. Arm, forearm and hand blocks. In: Lennard TA, editor. Pain Procedures in Clinical Practice. 2nd ed. Philadelphia: Hanley & Belfus; 2000. pp. 96–107. [Google Scholar]
- 11.EEllis H, Feldman S. 6th ed. Oxford: Blackwell Science; 1993. Anatomy for Anaesthetists; pp. 170–1. [Google Scholar]
- 12.Williams PL, Warwick R, Dyson M, Bannister LH. 37th ed. Edinburgh: Churchill Livingstone; 1989. Gray's Anatomy; pp. 762–3. [Google Scholar]
- 13.Moore DC, Mulroy MF, Thompson GE. Peripheral nerve damage and regional anesthesia. Br J Anaesth. 1994;73:435–6. doi: 10.1093/bja/73.4.435. [DOI] [PubMed] [Google Scholar]
- 14.Macaire P, Singelyn F, Narchi P, Paqueron X. Ultrasound-or nerve stimulation-guided wrist blocks for carpal tunnel release: A randomized prospective comparative study. Reg Anesth Pain Med. 2008;33:363–8. doi: 10.1016/j.rapm.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Jayakumar A, Egeler C. Ultrasound-guided peripheral upper limb nerve blocks for day-case surgery. Contin Educ Anaesth Crit Care Pain. 2011;11:172–6. [Google Scholar]
- 16.Ali SN, Srivastava S. Study of ulnar and radial arteries at wrist level in smokers. Scand J Plast Reconstr Surg Hand Surg. 2008;42:320–4. doi: 10.1080/02844310802299742. [DOI] [PubMed] [Google Scholar]


