Abstract
Background:
Post-operative nausea and vomiting (PONV) is commonly seen after modified radical mastectomy (MRM). In this randomized double-blind prospective study we compared the efficacy of ondansetron, granisetron and granisetron and dexamethasone combination for prevention of PONV following MRM in female patients.
Materials and Methods:
A total of 75 patients (20-60 years of age) undergoing elective MRM were randomly allocated to one of the three groups of 25 patients each. Group O received ondansetron 4 mg, Group G received granisetron 40 mcg/kg and group granisetron and dexamethasone (G + D) received granisetron 40 mcg/kg + dexamethasone 8 mg prior to induction. All episodes of PONV within 24 h after induction of anesthesia were recorded.
Statistical Analysis:
Statistical analysis was done using Kruskal-Wallis test (nonparametric ANOVA).
Results:
The incidence of complete response (no PONV, no rescue medication) was 96% with G+D, as compared with 86% with granisetron and 4% with ondansetron during 0-3h after surgery which was clinically significant (P < 0.05). Similarly clinically significant response was seen during 3-6, 6-9, 9-12 and 12-24 h of surgery.
Conclusion:
Granisetron and dexamethasone combination is more effective for prevention of PONV in comparison to individual ondansetron and granisetron in MRM.
Keywords: Dexamethasone, granisetron, modified radical mastectomy, ondansetron, postoperative nausea and vomiting
INTRODUCTION
Postoperative nausea and vomiting (PONV) is described as “The Big Little Problem”[1] and from the patients perspective PONV is among the most distressing complication of anesthesia and surgery.[2] Nausea, vomiting and retching are among the most common post-operative complaints and can occur in general, regional and local anesthesia. The reported incidence of PONV in patients undergoing breast surgery with axillary dissection is about 60-80%.[3] Hence, there is a continued interest in methods to reduce the incidence and severity of PONV.
Patients report that avoidance of PONV is of greater concern than avoidance of postoperative pain.[4] Among high-risk patients, the incidence of PONV can be as frequent as 70-80%.[5] Patients with PONV may develop medical complications, consume more resources, increased pain at the surgical site and delayed discharge from hospital.
There are a number of other contributing factors.[6] These include patient related factors, surgical and post-operative condition. Patient related factors include increased body weight,[7] female gender[8,9] history of motion sickness or previous PONV,[10] perioperative opioid use[11] and non-smoking status.[12,13]
Current medical practice entails the use of a combination of antiemetic acting on multiple receptor sites to reduce the risk of PONV in high-risk pts. A recent meta-analysis on prevention of PONV[14] suggested that a combination of dexamethasone with the 5-HT3 receptor antagonists is likely to be the best antiemetic prophylactic regimen among the drugs currently available.
It has been postulated that antiemetic and antinauseant effect of ondansetron is exerted by blockade of serotonin induced depolarization of vagal afferent nerves. It may also involve 5-HT3 binding sites in the chemoreceptor trigger zone and nucleus tractus solitarii in the brain stem. Emetogenic action of chemotherapeutic agents and radiotherapy as well as PONV may involve activation of 5-HT3 receptors in vagal afferents in the small intestine as well as central neurons in the area postrema near the fourth ventricles. These actions are effectively blocked by ondansetron. It has a half-life of 3 h.
Granisetron is a new 5-HT3 receptor antagonist more selective than ondansetron. It is effective orally as well as intravenous (i.v.). It blocks the 5-HT3 receptors at both the central and the peripheral sites. It acts on the vagal efferent nerves of the gut and produces blockade of 5-HT3 receptors. It has a half-life of 8-9 h.[15] Hence, it has longer duration of action than ondansetron.
Dexamethasone is a 21 carbon compound having a cyclopentanoperhydro-phenanthrene (steroid) nucleus. It is very potent and highly selective long-acting glucocorticoid. It has a long half-life of 36-48 h after a single dose of 8 mg i.v. given before induction of anesthesia.[16] The precise mechanism of action is not well understood, but may be due to prostaglandin antagonism, serotonin inhibition in the gut and the release of endorphins that elevate mood and stimulate appetite.[16] It augment the efficacy of other primary antiemetic drugs like metoclopramide, ondansetron and granisetron. It also serves to reduce certain side effects of the primary antiemetics.
We designed this prospective randomized double-blind study to compare the efficacy of ondansetron, granisetron and combination of granisetron and dexamethasone to prevent PONV in patients undergoing modified radical mastectomy (MRM).
MATERIALS AND METHODS
The study protocol was approved by Instituitional Ethical Committee and informed consent was taken by every patient. Seventy-five female patients of American Society of Anesthesiologists (ASA) Grade 1 and 2 with carcinoma breast Stages 1-3 going for elective MRM with or without chemotherapy were included in the study. Patients with history of motion sickness and previous history of PONV, history of smoking, full stomach, gastroesophageal disease, pregnant and menstruating women and those who had taken antiemetic medication within 24 h were excluded from the study.
All the patients were kept fasting 6-8 h and premedicated with tablet alprazolam 0.25 mg at night and in the morning of surgery. In the operation theater, i.v. line was started in the hand opposite to the side to be operated. Basic monitors in the form of electocardiogram, non-invasive blood pressure and pulse oximetry were connected to the patient. Baseline pulse, BP and SpO2 were recorded. In a double-blind manner, patients were randomly divided into three groups (25 patients each), received either:
Group O: Ondansetron 4 mg
Group G: Granisetron 40 mcg/kg
Group G + D: Combination of granisetron 40 mcg/kg plus dexamethasone 8 mg.
All drugs were delivered in equivalent volume in 5 ml syringe with a coded label. The anesthesiologist who anesthetized the patient and all involved nurses were unaware of the content of the syringe. The study drug was administered just before the induction of anesthesia. Pulse, BP and SpO2 were recorded 5 min after administration of study drugs.
The anesthesia regimen and surgery were standardized for all patients. After preoxygenation, induction of anesthesia was done with injection- fentanyl 2 mcg/kg and injection thiopentone 5 mg/kg intravenously. Tracheal intubation was facilitated with injection vecuronium 0.1 mg/kg. Intermittent positive pressure ventilation was maintained by nitrous oxide and oxygen (50:50). Anesthesia was maintained by isoflurane and supplemental doses of vecuronium (0.04 mg/kg) and fentanyl as and when required. Injection ketorolac 30 mg intravenously was given 15 min. prior to completion of surgery. At the end of surgical procedure, residual neuromuscular block was adequately reversed using i.v. glycopyrrolate (0.4 mg) and neostigmine (2.5 mg). Patient was extubated after adequate respiration and head lift and shifted to post anesthesia care unit. Postoperative analgesia was provided with injection- tramadol 100 mg i.v. 6 hourly in drip and injection- ketorolac 30 mg i.v. if required. All the patients were observed for hemodynamics, nausea, retching and emetic episodes and any adverse events for 0-3, 3-6, 6-9, 9-12, 12-24 h of surgery. Pulse, BP and SpO2 were recorded every 30 min during surgery and at 3, 6, 9, 12, and 24 h of surgery.
Severity of nausea and vomiting was assessed by visual analogue scoring as:[17]
Score 0 (no nausea or vomiting),
Score 1 (nausea),
Score 2 (retching or mild vomiting),
Score 3 (two or more vomitings in 30 min duration).
Patients who had two or more vomitings post-operatively received a rescue dose of injection-metoclopramide 10 mg i.v. adverse effects such as headache, dizziness, hypotension, and extra-pyramidal effects were also noted.
Nausea is defined as a subjectively unpleasant sensation associated with an urge to vomit.[18] Retching is defined as the labored, spasmodic, rhythmic contraction of the respiratory muscles, including the diaphragm, chest wall and abdominal wall muscles without expulsion of gastric contents. Vomiting is defined as the forceful expulsion of gastric contents from the mouth[19] brought about by the powerful sustained contraction of the abdominal muscles, descent of the diaphragm and opening of gastric cardia.
Statistical analysis
The results were analyzed using SPSS version 14 (SPSS Inc., Chicago, IL, USA). Power analysis indicated that 25 patients are required per each group based on 85% incidence of PONV in MRM surgery if no prophylaxis given with an anticipated reduction in the incidence of emesis up to 25%, which was the therapeutic outcome for dexamethasone when given as a sole prophylactic agent. The alpha error was set at 0.05 and Type 2 error was set at 0.20. Statistical analysis was done using Kruskal-Wallis test (nonparametric ANOVA). If Kruskal-Wallis test was significant, Dunn's multiple comparisons test was used to compare different groups. For all tests P < 0.05 was considered to be significant. Data were presented as a mean and standard deviation or number and percentages.
RESULTS
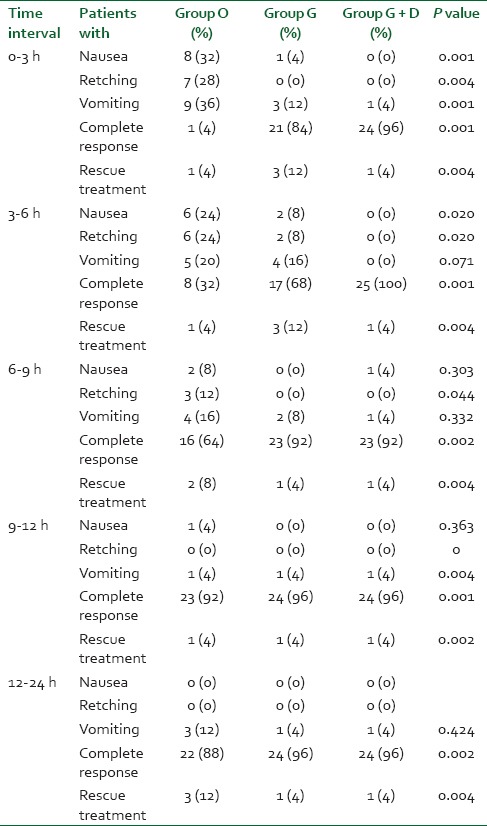
The groups were comparable with respect to age and weight [Table 1] and the vitals remained stable throughout the surgery in all the three groups except in ondansetron group where 1 patient had hypotension which is insignificant. The incidence of complete response [Table 2] (no nausea, no rescue medication) during 0-3 h in postoperative period was 4% with ondansetron (Group O), 84% with granisetron (Group G) and 96% with granisetron + dexamethasone (G + D) (Group G + D). Hence, P < 0.05 was considered significant. Similarly, clinically significant response was seen during 3-6, 6-9, 9-12 and 12-24 h following surgery.
Table 1.
The age and weight data is presented as mean and SD
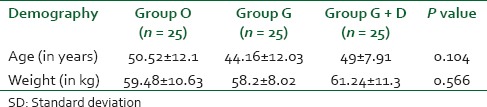
Table 2.
Incidence of nausea, retching and vomiting
In Group O (ondansetron), 8% (2)patients complained of headache, 8% (2) had dizziness and 4% (1) patient had hypotension.[Table 3]
Table 3.
Incidence of adverse complaints in different groups
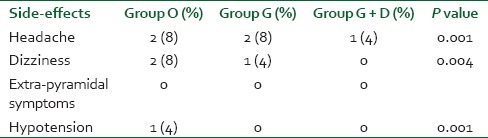
In Group G (granisetron), 8% (2) patients had headache, 4% (1) had dizziness.
In Group G + D, only 4% (1) patient complained of headache.
Fuethermore, we can see those overall 8 patients in ondansetron group, 9 patients in granisetron group and only 5 patients in G + D group required rescue dose, which is clinically highly significant.
DISCUSSION
Postoperative nausea and vomiting is one of the most distressing experiences associated with surgery, and many patients find it troublesome than post-operative pain itself. The occurrence of intractable vomiting can prolong the hospital stay[7] and hence the economic implications also assume greater significance.
The strategies for the prevention of early and late PONV have changed considerably over the last decade, with the focus having moved from single drug therapy to combination antiemetic therapy, or balanced antiemesis. The first evidence that such combination therapy is of superior benefit came in year 1994.[20] Since this time several combinations have been tried, and many of them have proved to be more efficacious than single drug therapy.[21] More recently, multimodal management strategies incorporating changes in anesthetic technique, aggressive fluid management and pain relief strategies have produced even better results.[22]
Fujii et al. (1998): Undertook a study in Japanese females to evaluate the efficacy of granisetron-dexamethasone combination for prevention of PONV in patients undergoing general anesthesia for breast surgery. 135 ASA 1 patients aged between 40 and 65 years were assigned to receive placebo (saline), granisetron 40 mcg/kg i.v. or granisetron 40 mcg/kg + dexamethasone 8 mg i.v. immediately before the induction of anesthesia. A complete response during 0-3 h after anesthesia was 51%, 82% and 96% in patients who had received placebo, granisetron and G + D combination, respectively. The corresponding incidence during 3-24 h after anesthesia was 56%, 84% and 96%, respectively. It was concluded that prophylactic use G + D combination is more effective than granisetron alone for the prevention of PONV after breast surgery.
This study is in concordance with the above study. The study is performed in Indian females. We also compared the efficacy of granisetron and dexamethasone combination with granisetron or ondansetron for prevention of PONV in female patients undergoing breast surgery.
Episodes of nausea, retching, and vomiting were recorded for 0-3, 3-6, 6-9, 9-12, and 12-24 h, respectively of the postoperative period in all the three groups.
During 0-3h, 32% (8) patients had nausea in ondansetron group while no patients in G + D group. 28% (7) complained of retching in ondansetron group while none in granisetron and G + D group. 36% (9) had vomiting in Group O, 12% (3) in granisetron group but only 1% (4) in G + D group. P < 0.05 which is statistically significant.
At 3-6 h, 24% (6) in ondansetron group and 8% (2) in granisetron group had nausea and retching. Episodes of vomiting were 20% (5) in ondansetron group and 16% (4) in granisetron group. None of the patients in group G + D complained of nausea, retching or vomiting during this time period. P < 0.05 which is statistically significant.
During 6-9 h, 8% (2) in Group O and 4% (1) in Group G + D had nausea. Retching was seen in 12% (3) in Group O while none of the patients in Group G and G + D. 16% (4) had vomiting in Group O, 8% (2) in Group G while 4% (1) in Group G + D had vomiting. P < 0.05 which is statistically significant.
At 9-12 h, all the three groups were comparable as 4% (1) had nausea in Group O and 4% (1) had vomiting in all the three groups.
During 12-24 h of the postoperative period, none of the patients had nausea and retching. But 12% (3) had vomiting in ondansetron group, 4% (1) in each granisetron and G + D group.
A complete response (no PONV and no need of rescue antiemetic) during 0-3 h after surgery was seen in 4%, 84% and 96% patients who had received ondansetron, granisetron and granisetron plus dexamethasone, respectively (P < 0.05).
The corresponding incidence during 3-24 h was 70%, 88% and 96% in the respective groups. Requirement of rescue antiemetic was comparatively higher in ondansetron group rather than in granisetron and granisetron plus dexamethasone group.
Adverse effects such as headache, hypotension, dizziness, etc., were more common in ondansetron group as compared to granisetron and granisetron plus dexamethasone group.
Hence, we can say that the administration of granisetron and dexamethasone had significantly reduced the incidence of PONV as compared to ondansetron or granisetron alone in patients undergoing MRM.
Thomas R and Jones et al. (BJA 2001) conducted a prospective randomized comparative study of dexamethasone, ondansetron, and ondansetron + dexamethasone as prophylactic antiemetic therapy in patients undergoing day case gynecological surgery. They found that failure of prophylaxis during first 3 h after surgery was recorded in 22%, 28.3%, and 8.6%. The overall incidences for the 24 h postsurgery were 42.4%, 48.3%, and 34.5%, respectively.
Dipasi Bhattacharya and Arnab Banerjee (IJA 2003) conducted a double-blind randomized placebo controlled trial to compare the efficacy of ondansetron and granisetron for prevention of PONV after day care gynecological laparoscopy.
They found that incidences of emetic episodes were 20% in ondansetron group and 7% in granisetron group which is clinically significant (P < 0.05).
Hence, the results of our study are in concordance with the previous studies by different authors, with few differences, which are insignificant. Hence, granisetron and dexamethasone combination is quite effective in preventing and reducing PONV in MRM patients.
CONCLUSION
On the basis of results obtained, it was concluded that Indian females who were undergoing MRM and had prophylactically received granisetron and dexamethasone combination were either free from nausea and emetic episodes or had lesser degree of PONV as compared to ondansetron or granisetron group alone. A complete response of 96% was seen with granisetron and dexamethasone combination.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kapur PA. The big “little problem”. Anesth Analg. 1991;73:243–5. doi: 10.1213/00000539-199109000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Orkin FK. What do patients want? Preference for immediate postoperative recovery. Anesth Analg. 1992;74:S225. [Google Scholar]
- 3.Fujii Y. Prophylaxis of postoperative nausea and vomiting in patients scheduled for breast surgery. Clin Drug Investig. 2006;26:427–37. doi: 10.2165/00044011-200626080-00001. [DOI] [PubMed] [Google Scholar]
- 4.Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg. 1999;89:652–8. doi: 10.1097/00000539-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 5.Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: Conclusions from cross-validations between two centers. Anesthesiology. 1999;91:693–700. doi: 10.1097/00000542-199909000-00022. [DOI] [PubMed] [Google Scholar]
- 6.Leman J. Surgical and patient factors involved in post operative nausea and vomiting. Br J Anaesth. 1992;69(Suppl):524–32. doi: 10.1093/bja/69.supplement_1.24s. [DOI] [PubMed] [Google Scholar]
- 7.Gan TJ, Meyer T, Apfel CC, Chung F, Davis PJ, Eubanks S, et al. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97:62–71. doi: 10.1213/01.ane.0000068580.00245.95. [DOI] [PubMed] [Google Scholar]
- 8.Salmenperä M, Kuoppamäki R, Salmenperä A. Do anticholinergic agents affect the occurrence of postanaesthetic nausea? Acta Anaesthesiol Scand. 1992;36:445–8. doi: 10.1111/j.1399-6576.1992.tb03494.x. [DOI] [PubMed] [Google Scholar]
- 9.Burtles R, Peckett BW. Postoperative vomiting; some factors affecting its incidence. Br J Anaesth. 1957;29:114–23. doi: 10.1093/bja/29.3.114. [DOI] [PubMed] [Google Scholar]
- 10.Kenny GN. Risk factors for postoperative nausea and vomiting. Anesthesia. 1994;9:6–10. doi: 10.1111/j.1365-2044.1994.tb03576.x. [DOI] [PubMed] [Google Scholar]
- 11.Islan S, Jain PN. PONV: A review article. Indian J Anaesth. 2004;48:253–8. [Google Scholar]
- 12.Anonymous (Editorial.) Nausea and vomiting after general anesthesia. Lancet. 1989;337:651. [PubMed] [Google Scholar]
- 13.Tramèr MR. Treatment of postoperative nausea and vomiting. BMJ. 2003;327:762–3. doi: 10.1136/bmj.327.7418.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rowbotham DJ. Recent advances in the non-pharmacological management of postoperative nausea and vomiting. Br J Anaesth. 2005;95:77–81. doi: 10.1093/bja/aei125. [DOI] [PubMed] [Google Scholar]
- 15.Giglio CA, Soares HP, Caparroz C, Castro PC. Granisetron is equivalent to ondansetron for prophylaxis of chemotherapy-induced nausea and vomiting: Results of a meta-analysis of randomized controlled trials. Cancer. 2000;89:2301–8. doi: 10.1002/1097-0142(20001201)89:11<2301::aid-cncr19>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 16.Mansour EE. Postoperative nausea & vomiting prophylaxis: The efficacy of a novel antiemetic drug (palonosetron) combined with dexa methasone. Egypt J Anaesth. 2013;29:1–7. [Google Scholar]
- 17.Pierre S, Benais H, Pouymayou J. Apfel's simplified score may favourably predict the risk of postoperative nausea and vomiting. Can J Anaesth. 2002;49:237–42. doi: 10.1007/BF03020521. [DOI] [PubMed] [Google Scholar]
- 18.Knapp MR, Beecher HK. Postanesthetic nausea, vomiting, and retching; evaluation of the antiemetic drugs dimenhydrinate (dramamine), chlorpromazine, and pentobarbital sodium. J Am Med Assoc. 1956;160:376–85. doi: 10.1001/jama.1956.02960400034009. [DOI] [PubMed] [Google Scholar]
- 19.Rudra A, Ray AK. Post operative nausea and vomiting review article. Indian J Anaesth. 1996;44:226. [Google Scholar]
- 20.Henzi I, Walder B, Tramèr MR. Dexamethasone for the prevention of postoperative nausea and vomiting: A quantitative systematic review. Anesth Analg. 2000;90:186–94. doi: 10.1097/00000539-200001000-00038. [DOI] [PubMed] [Google Scholar]
- 21.Heffeman AM, Rowbotham DJ. Post-operative nausea & vomiting-time for balanced antiemesis? Editorial; Comment. Br J Anaesth. 2000;85:675–7. doi: 10.1093/bja/85.5.675. [DOI] [PubMed] [Google Scholar]
- 22.Habib AS, Gan TJ. Combination therapy for postoperative nausea and vomiting-a more effective prophylaxis? Ambul Surg. 2001;9:59–71. doi: 10.1016/s0966-6532(01)00103-2. [DOI] [PubMed] [Google Scholar]


