Abstract
Aims:
The aim was to assess the effectiveness of adding either dexamethasone or midazolam in comparison with epinephrine addition to 0.5% bupivacaine in supraclavicular brachial plexus block.
Settings and Design:
This is a prospective randomized controlled observer-blinded study.
Subjects and Methods:
This study was carried out in Tanta University Hospital on 60 patients of both sexes; American Society of Anesthesiologists physical Status I and II, age range from 18 to 45 years undergo elective surgery to upper limb. All patients were anesthetized with ultrasound guided supraclavicular brachial plexus block and randomly divided into three groups (each group 20 patients) Group E (epinephrine): 30 mL bupivacaine 0.5%with 1:200,000 epinephrine (5 μg/mL). Group D (dexamethasone): 30 mL bupivacaine 0.5% and dexamethasone 8 mg. Group M (midazolam): 30 ml bupivacaine 0.5% and midazolam 50 μg/kg. The primary outcome measures were onset and duration of sensory and motor block and time to first analgesic request.
Statistical Analysis Used:
The windows version of SPSS 11.0.1 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Data were presented in form of mean ± standard deviation multiple analysis of variance (ANOVA) was used to compare the three groups and Scheffe test was used after ANOVA. Power of significance P < 0.05 was considered to be statistically significant.
Results:
Onset of sensory and motor block was significantly rapid (P < 0.05) in Groups D and M in comparison with Group E. Time of administration of rescue analgesic, duration of sensory and motor block showed significant increase (P < 0.05) in Group D in comparison with Group M which showed significant increase (P < 0.05) in comparison with Group E.
Conclusions:
In comparison with epinephrine and midazolam addition of dexamethasone to bupivacaine had rapid onset of block and longer time to first analgesic request with fewer side-effects.
Keywords: Brachial plexus block, bupivacaine, dexamethasone, midazolam, supraclavicular block
INTRODUCTION
Supraclavicular nerve block is good alternative to general anesthesia for upper limb surgery. This avoids the untoward effects of general anesthetic drugs and upper airway instrumentation. It achieves complete muscle relaxation, intraoperative hemodynamic stability, and postoperative analgesia.[1]
There are many approaches to the brachial plexus block have been described, but the supraclavicular approach is the easiest and appropriate method for anesthesia and management of perioperative pain in surgery below the shoulder joint.[2]
Bupivacaine used frequently for supraclavicular nerve block as it has long duration of action from 3 to 6 h. Adjuncts to local anesthetics for brachial plexus block may enhance the quality and duration of analgesia.[3]
Brachial plexus blockade reduces pain, but still with short duration and the challenge remains to increase the duration of analgesia with decreasing side-effects.[4]
Different additives have been used to prolong regional blockade and shorten the onset times of blocks. Vasoconstrictor was used to constrict vessels, thereby reducing vascular absorption of the local anesthetic. Additives such as opioids, clonidine, verapamil, etc., were added to local anesthetics, but the results are either inconclusive or associated with side-effects.[5]
Steroids have powerful antiinflammatory as well as analgesic property and were used intrathecally with no evidence suggesting neuritis when given in low concentration.[6]
Also midazolam, a water-soluble benzodiazepine, is known to produce antinociception and enhance the effect of local anesthetics when given epidurally or intrathecally.[7]
The purpose of this study was to assess the effectiveness of adding either dexamethasone or midazolam in comparison with epinephrine addition to 0.5% bupivacaine in supraclavicular brachial plexus block.
SUBJECTS AND METHODS
This is a prospective randomized controlled observer-blinded study conducted at Tanta University Hospital and carried out on 60 adult patients of both sexes during the period from April 2010 to February 2012 after approval by the Hospital Ethical Committee.
Inclusion criteria are American Society of Anesthesiologists physical Status I-II and age between 18 and 45 years.
Exclusion criteria are known allergy to local anesthetic agents or narcotics, coagulation disorders, ASA physical status of more than II, history of a major psychiatric disorder, chronic pain syndrome, diabetic patient, pregnancy, history of substance abuse, and current opioid use. Patients were provided with complete information about the techniques of anesthesia and analgesia. All included participants were asked to take part in the study by the study personnel soon after admission to the ward and a written informed consent was obtained from each patient. Patients were randomly allocated to three groups of 20 patients each.
Patients were connected to the monitor include pulse oximeter, electrocardiogram and noninvasive blood pressure (BP). Patients were connected to nasal prong at 3 L/min. Intravenous access was secured, lactated ringer started at rate 10 mL/kg intravenous (IV).
Patient in semi-sitting position (the head of the bed raised about 45°) with head tilted to the opposite side of injection site. The skin was cleaned with chlorhexidine solution. The ultrasound transducer (high frequency linear 13-6 MHz, 38 mm broadband linear array [SonoScape SSI 6000 China]) was inserted into a sterile sheath. A thin layer of sterile gel was placed between the draped ultrasound transducer and the skin. Probe is applied parallel to the clavicle in the supraclavicular fossa. At this location, the subclavian artery is seen beating above the first rib; it cannot be compressed as opposed to the vein. The rib is bright and pleura are seen on each side of the rib. The brachial plexus is lateral to the subclavian artery with honeycomb appearance. A volume of 2 mL lignocaine 2% was infiltrated subcutaneous before the block (24-G needle Masco Mid Co., Cairo, Egypt). An 18-G tuohy needle (Perifix, B Braun, Melsungen AG, Germany) is advanced in plane under direct visualization toward the plexus sheath till its puncture and start injection. The injected volume gently expands the connective tissue surrounding the nerves, which is called hydro dissection. This allows a clear path for the needle, decreasing the chance of nerve damage by the needle. Another injection site is at the angle between the first rib and the subclavian artery. Aspiration done every 3-5 mL during injection to prevent vascular injection the end of the injection was considered time 0.
Patients were randomly divided into three groups (each group 20 patients) using closed sealed envelope, according to drugs injected into:
Group E (epinepherine): 30 mL bupivacaine 0.5%with 1:200,000 epinepherine (5 μg/mL).
Group D (dexamethasone): 30 mL bupivacaine 0.5% + dexamethasone 8 mg.
Group M (midazolam): 30 mL bupivacaine 0.5% + midazolam 50 μg/kg.
The following parameters were measured
Onset of sensory block
It was defined as the time taken from the end of the injection to the first dull response to pinprick in the distribution of any of the three sensory nerves in the hand.
After injection, patients were assessed for sensory blockade by using pinprick. The palmar surfaces of the index and little finger were used to test the median and ulnar nerve in the hand, respectively. The dorsal surface of the thumb was used to test the radial nerve. Sensory characteristics of the block were assessed using response to pinprick to 23-G hypodermic needle.[17]
Sensory score
0 normal sensations to pin prick.
1 dull response to pin prick.
2 no response to pin prick.[7]
Onset of motor block
from end of injection until onset of complete loss of the motor power.
Patients with inadequate blockade requiring supplementation were excluded from the study.
The end of the injection was considered time 0 to be successful if it occurred within <30 min.
Motor block was assessed by asking the patient to adduct the shoulder and flex the fore-arm and hand against gravity. Motor characteristics of block were assessed using Bromage 3-point scale.[8]
Motor score
0 normal motor functions with full flexion and extension elbow, wrist, and fingers.
1 decreased motor strength with ability to move fingers only.
2 complete motor blockade with inability to move fingers.
Duration of sensory block (the time taken between injection of the drug and appearance of pain requiring analgesia) duration of motor block (time taken between injection to complete return of motor power) were recorded.
Sedation score was assessed by using the sedation score.[8]
Awake and alert;
Sedated, responding to verbal stimulus.
Sedated, responding to mild physical stimulus.
Sedated, responding to moderate or severe physical stimulus.
Pain was assessed using the visual analog scale (VAS) where zero (0) represented no pain and 10 meant the worst possible pain.[3] Postoperative rescue analgesic in form of paracetamol 30 mg/kg IV if VAS (4-6) or pethidine 30 mg IV if VAS >6.
Hemodynamic variables (heart rate [HR], mean arterial pressure [MAP], and oxygen saturation).
Neurologic assessment (sensory and motor), hemodynamic variables (HR, MAP, and SaO2), analgesia with VAS and sedation scores were recorded at 1, 3, 5, 10, 15, 20, 30 and 45 min, then hourly up to 6 h, 2 hourly up to 16 h and 4 hourly until 24 h.
Any adverse effects such as nausea, vomiting, dizziness…etc. Specific questions were asked about any residual numbness, discomfort, and pain.
In addition, overall patient satisfaction with analgesia was assessed by a second anesthesiologist on postoperative day 1 by the use of a 4-point verbal scale ranging from very satisfied to very dissatisfied (1: Very dissatisfied, 2: Dissatisfied, 3: Satisfied, 4: Very satisfied).[9]
Statistical analysis used
Sample size calculation was performed before patient recruitment. Based on a previous study.[1,2]
The windows version of SPSS 11.0.1 (SPSS Inc., Chicago, IL) was used for statistical analysis. Data were presented in form of mean ± standard deviation multiple analysis of variance (ANOVA) was used to compare the three groups and Scheffe test was used after ANOVA. Power of significance P < 0.05 was considered to be statistically significant.
RESULTS
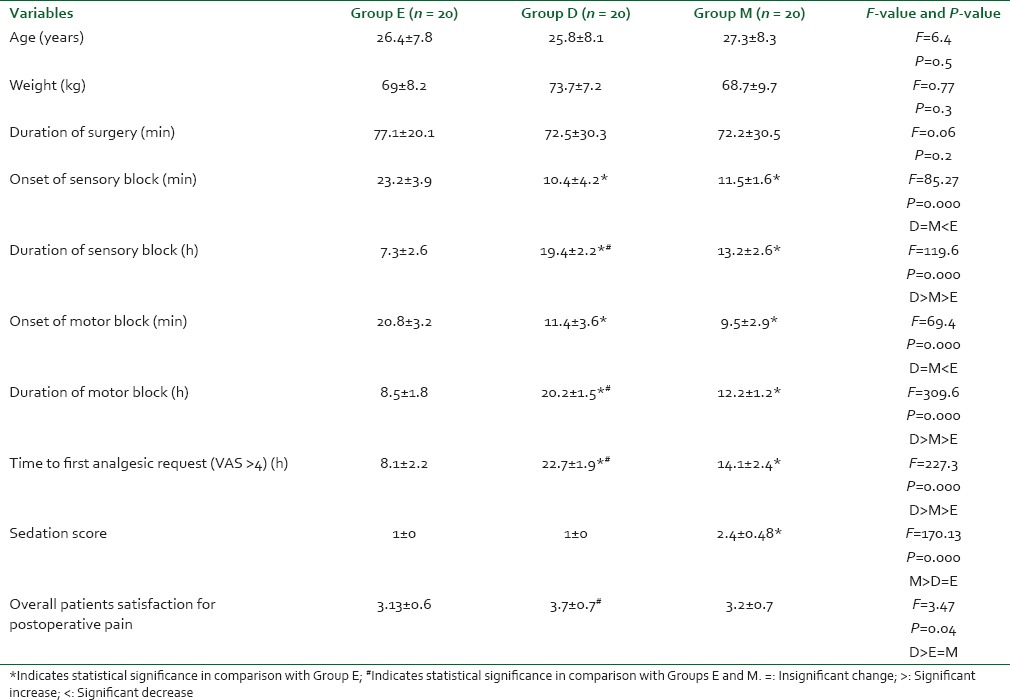
The demographic data showed insignificant differences (P > 0.05) between the three groups. Onset of sensory and motor block were significantly rapid (P < 0.05) in Groups D and M in comparison with Group E. Time of administration of rescue analgesic, duration of sensory and motor block showed significant increase (P < 0.05) in Group D in comparison with Group M which showed significant increase (P < 0.05) in comparison with Group E [Table 1].
Table 1.
Demographic data, onset and duration of sensory and motor block, sedation score, overall patient satisfaction with analgesia
Sedation scores were higher in Group M compared to Groups E and D (P < 0.05) as patients in Groups E and D were all awake (score 1) throughout the procedure time, while in Group M, five patients at 10 min, seven patients at 20 min and eight patients at 30 min were sedated and responded to verbal stimulation (score 2). Score 2 was the highest sedation in Group M and no patient had sedation score of 3 or more that required airway assistance.
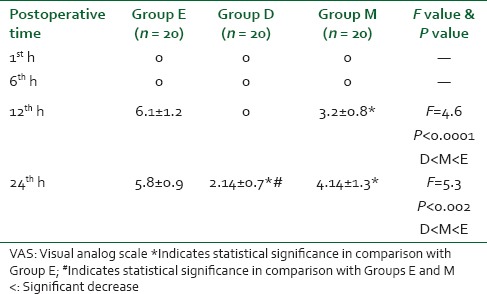
In comparison with groups E and M, Group D showed significant decrease (P < 0.05) in postoperative VAS pain scores 12 and 24 hours postoperatively [Table 2].
Table 2.
Postoperative pain VAS
Hemodynamic variables that is, HR, mean BP, and oxygen saturation were comparable between groups and did not change significantly in the perioperative period. No adverse event was encountered in the three groups of patients.
VAS: Visual analog scale *Indicates statistical significance in comparison with Group E; #Indicates statistical significance in comparison with Groups E and M.
DISCUSSION
Significant decrease
Ultrasound guided supraclavicular brachial plexus block is a safe reliable anesthetic technique for upper limb surgery with less complication. It provides ideal surgical condition with stable hemodynamic, decreases vasospasm, edema, postoperative pain, and help early ambulation.[10]
A mixture of bupivacaine and lignocaine provides better surgical condition, but the analgesic time is rarely longer than 6 h.
In this study, we assess the effectiveness of adding either dexamethasone or midazolam in comparison with epinephrine addition to 0.5% bupivacaine in supraclavicular brachial plexus anesthesia for management of the postoperative pain.
The major findings of this study is that onset of sensory and motor block was significantly rapid (P < 0.05) in Groups D and M in comparison with Group E. Time of administration of rescue analgesic, duration of sensory and motor block showed significant increase (P < 0.05) in Group D in comparison with Group M which showed significant increase (P < 0.05) in comparison with Group E.
Steroids are very potent antiinflammatory and immunosuppressive agents. Perineural injection was found to be safe, devoid of potential adverse effects and may affect postoperative analgesia. Dexamethasone is a synthetic glucocorticoid, preferred because it is highly potent antiinflammatory, about 30 times as potent as hydrocortisone and without any mineralocorticoid activity.[11]
Dexamethasone is also known to reduce postoperative nausea and vomiting through its antiinflammatory effect.[12]
Dexamethasone prolonged duration of block through local action mediated through glucocorticoid receptors. When steroid alone is used in regional blocks, the blockade is not produced. Steroids might exert this effect by altering the function of potassium channels in the excitable cells; bind to intracellular receptors and modulate nuclear transcription.[13,14]
Movafegh et al. in their study they found that addition of dexamethasone to lignocaine prolongs duration of analgesia significantly without any change in onset time.[15]
While in study of Shrestha et al. found that addition of dexamethasone as adjuvant to mixture of local anesthetics in supraclavicular block had significant early onset and longer duration of analgesia.[16]
Dexamethasone had safety profile in spite of sample sizes in most studies are insufficient to detect rare outcomes and most studies did not follow patients for weeks after surgery. No trial has reported neurotoxicity. In the study of Cummings et al. on 108 patients given dexamethasone for interscalene nerve block without any adverse effect.[17]
Animal studies demonstrate no long-term changes in nerve structure or function after local steroid administration. Toxicity attributed to corticosteroids may be due to the particulate nature or vehicle used in different steroid preparations – neither of which applies to the formulation of dexamethasone (dexamethasone sodium phosphate) used in this study and many other studies.[18]
Researchers showed axonal gamma-aminobutyric acid (GABA-A) receptors in brachial plexus and peripheral nerve trunks. Various studies in animals and human have demonstrated the antinociceptive action of benzodiazepines when used intrathecally mediated by GABA receptor, opioid receptor, and benzodiazepines receptor in spinal cord.[19]
Administration of opioid antagonist naltrindole acts on d-receptors and suppresses the antinociceptive effect of intrathecal midazolam, suggesting that intrathecal midazolam is responsible for the release of an endogenous opioid acting at spinal d-receptors.[20]
Animal studies have shown midazolam had no damage to the spinal cord, nerve roots, or meninges.[21]
Mahajan et al. observed that in bupivacaine midazolam group there were clinically and statistically prolonged postoperative analgesic effects in caudal block.[22]
Güleç et al. found that bupivacaine midazolam providing prolonged postoperative analgesia in comparison with bupivacaine-morphine combination in caudal block.[23]
In this study, sedation scores were higher in Group M compared to Groups E and D, this could be due to systemic absorption of the drug (midazolam) and its effect on central nervous system to produce sedation.[24] Though mean sedation score in Group M was higher as compared to Groups E and D, patients, sedation in Group M was not clinically significant. The highest sedation score was 2 that is, the patient was sedated and responding to verbal stimulus. No patient had airway compromise or required airway support.
In this study, BP, HR and oxygen saturation remained stable throughout the procedure and postoperatively as they did not differ significantly during the study period. These results are in agreement with those obtained by Laiq et al.[3]
CONCLUSION
In comparison with epinephrine and midazolam addition of dexamethasone to bupivacaine had rapid onset of block and longer time to first analgesic request with fewer side-effects.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Jarbo K, Batra YK, Panda NB. Brachial plexus block with midazolam and bupivacaine improves analgesia. Can J Anesth. 2005;52:822–6. doi: 10.1007/BF03021776. [DOI] [PubMed] [Google Scholar]
- 2.Shrestha BR, Maharjan SK, Tabedar S. Supraclavicular brachial plexus block with and without dexamethasone – A comparative study. Kathmandu Univ Med J (KUMJ) 2003;1:158–60. [PubMed] [Google Scholar]
- 3.Laiq N, Khan MN, Arif M, Khan S. Midazolam with bupivacaine for improving analgesia quality in brachial plexus block for upper limb surgeries. J Coll Physicians Surg Pak. 2008;18:674–8. [PubMed] [Google Scholar]
- 4.Parrington SJ, O’Donnell D, Chan VW, Brown-Shreves D, Subramanyam R, Qu M, et al. Dexamethasone added to mepivacaine prolongs the duration of analgesia after supraclavicular brachial plexus blockade. Reg Anesth Pain Med. 2010;35:422–6. doi: 10.1097/AAP.0b013e3181e85eb9. [DOI] [PubMed] [Google Scholar]
- 5.Islam SM, Hossain MH, Maruf AA. Effect of addition of dexamethasone to local anesthetics in supraclavicular brachial plexus block. J Armed Forces Med Coll Bangladesh. 2011;7:11–4. [Google Scholar]
- 6.Benzon HT. Epidural steroids. In: Raj PP, editor. Pain Medicine. A Comprehensive Review. UK: Mosby Publications; 1999. pp. 259–63. [Google Scholar]
- 7.Ravi NA, Ritesh MK, Parmila SJ, Dipsheekha C. Role of midazolam as an adjuvant to local anesthetic in supraclavicular brachial plexus block. Asian J Med Res. 2012;1:103–7. [Google Scholar]
- 8.Culebras X, Van Gessel E, Hoffmeyer P, Gamulin Z. Clonidine combined with along acting local anesthetic does not prolong postoperative analgesia after brachial plexus block but does induce hemodynamic changes. Anesth Analg. 2001;92:199–204. doi: 10.1097/00000539-200101000-00038. [DOI] [PubMed] [Google Scholar]
- 9.Wang F, Shen X, Guo X, Peng Y, Gu X. Labor Analgesia Examining Group. Epidural analgesia in the latent phase of labor and the risk of cesarean delivery: A five-year randomized controlled trial. Anesthesiology. 2009;111:871–80. doi: 10.1097/ALN.0b013e3181b55e65. [DOI] [PubMed] [Google Scholar]
- 10.Paul FW, Alejandro RF. Elsevier Churchill Livingstone. 6th ed. 2005. Regional anesthesia: Ambulatory (Outpatient) anesthesia. In Miller's; p. 2608. [Google Scholar]
- 11.Golwala MP, Swadia VN, Dhimar AA, Sridhar NV. Pain relief by dexamethasone as an adjuvant to local anesthetics in supraclavicular brachial plexus block. J Anesth Clin Pharmacol. 2009;25:285–8. [Google Scholar]
- 12.Elhakim M, Ali NM, Rashed I, Riad MK, Refat M. Dexamethasone reduces postoperative vomiting and pain after pediatric tonsillectomy. Can J Anesth. 2003;50:392–7. doi: 10.1007/BF03021038. [DOI] [PubMed] [Google Scholar]
- 13.Castillo J, Curley J, Hotz J, Uezono M, Tigner J, Chasin M, et al. Glucocorticoids prolong rat sciatic nerve blockade in vivo from bupivacaine microspheres. Anesthesiology. 1996;85:1157–66. doi: 10.1097/00000542-199611000-00025. [DOI] [PubMed] [Google Scholar]
- 14.Biradar PA, Kaimar P, Gopalakrishna K. Effect of dexamethasone added to lidocaine in supraclavicular brachial plexus block: A prospective, randomised, double-blind study. Indian J Anesth. 2013;57:180–4. doi: 10.4103/0019-5049.111850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Movafegh A, Razazian M, Hajimaohamadi F, Meysamie A. Dexamethasone added to lidocaine prolongs axillary brachial plexus blockade. Anesth Analg. 2006;102:263–7. doi: 10.1213/01.ane.0000189055.06729.0a. [DOI] [PubMed] [Google Scholar]
- 16.Shrestha BR, Maharjan SK, Shrestha S, Gautam B, Thapa C, Thapa PB, et al. Comparative study between tramadol and dexamethasone as an admixture to bupivacaine in supraclavicular brachial plexus block. JNMA J Nepal Med Assoc. 2007;46:158–64. [PubMed] [Google Scholar]
- 17.Cummings KC, 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, et al. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Br J Anesth. 2011;107:446–53. doi: 10.1093/bja/aer159. [DOI] [PubMed] [Google Scholar]
- 18.Benzon HT, Chew TL, McCarthy RJ, Benzon HA, Walega DR. Comparison of the particle sizes of different steroids and the effect of dilution: A review of the relative neurotoxicities of the steroids. Anesthesiology. 2007;106:331–8. doi: 10.1097/00000542-200702000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Kohno T, Kumamoto E, Baba H, Ataka T, Okamoto M, Shimoji K, et al. Actions of midazolam on GABAergic transmission in substantia gelatinosa neurons of adult rat spinal cord slices. Anesthesiology. 2000;92:507–15. doi: 10.1097/00000542-200002000-00034. [DOI] [PubMed] [Google Scholar]
- 20.Goodchild CS, Guo Z, Musgreave A, Gent JP. Antinociception by intrathecal midazolam involves endogenous neurotransmitters acting at spinal cord delta opioid receptors. Br J Anesth. 1996;77:758–63. doi: 10.1093/bja/77.6.758. [DOI] [PubMed] [Google Scholar]
- 21.Serrao JM, MacKenzie JM, Goodchild CS, Gent JP. Intrathecal midazolam in the rat: An investigation of possible neurotoxic effects. Eur J Anesthesiol. 1990;7:115–22. [Google Scholar]
- 22.Mahajan R, Batra YK, Grover VK, Kajal J. A comparative study of caudal bupivacaine and midazolam-bupivacaine mixture for post-operative analgesia in children undergoing genitourinary surgery. Int J Clin Pharmacol Ther. 2001;39:116–20. doi: 10.5414/cpp39116. [DOI] [PubMed] [Google Scholar]
- 23.Güleç S, Büyükkidan B, Oral N, Ozcan N, Tanriverdi B. Comparison of caudal bupivacaine, bupivacaine-morphine and bupivacaine-midazolam mixtures for post-operative analgesia in children. Eur J Anesthesiol. 1998;15:161–5. [PubMed] [Google Scholar]
- 24.Reves JG, Fragen RJ, Vinik HR, Greenblatt DJ. Midazolam: Pharmacology and uses. Anesthesiology. 1985;62:310–24. [PubMed] [Google Scholar]


