Abstract
Background: The number of older jail inmates in poor health is increasing rapidly. Among older adults, pain is common and leads to greater acute care use. In jail, pain management is complicated by concerns about misuse and diversion. A lack of data about the prevalence and management of pain in older jail inmates limits our ability to develop optimal palliative care strategies for this population.
Objective: To describe the prevalence of and factors associated with pain and analgesic use in a population of older jail inmates.
Design: Cross-sectional study. χ2 tests assessed association between characteristics, pain, and analgesic use.
Setting/Subjects: Two hundred ten jail inmates age 55 or older.
Measurements: “Severe frequent pain” defined as “severe or very severe” pain experienced “frequently or constantly” using the validated Memorial Symptom Assessment Scale. Medical conditions, substance use, and analgesic treatment determined through self-report and jail medical records.
Results: Participants' mean age was 59 years; 69% had multimorbidity; 75% reported any pain; 39% reported severe frequent pain. Report of severe frequent pain was associated with multimorbidity, functional impairment, and pre-jail acute care use (p<0.05), but not with substance use (57% versus 56%, p=0.89). Within a week of their interview, most participants with severe frequent pain had received an analgesic (87%) and many received an opioid (70%).
Conclusion: High rates of pain in a rapidly growing population of older jail inmates with multimorbidity and functional impairment suggest that jails are an important site for assessing symptom burden and developing appropriate palliative care interventions.
Introduction
Palliative medicine experts have called for the integration of palliative medicine into care delivery systems that serve the needs of persons with serious illness and multimorbidity well before the final months of life.1,2 Jail has become one such health care system. Approximately 13 million Americans pass through jails annually. In contrast to prisons, which generally house persons convicted of a crime and sentenced to incarceration for more than 1 year, jails house inmates who are awaiting trial or serving short sentences. The average length of stay in jails is 30 days.3 Between 1996 and 2008, the number of older jail inmates increased 278% compared to a 53% increase in the jail population.4,5 Annually, more than 550,000 older adults are arrested6 and detained in jails where they have, by far, the highest in-jail mortality rates.7,8 Nearly all jail inmates (95%) return to our communities within 6 months, where they experience a high risk for poor health outcomes, acute care use, and mortality.7,9 Accordingly, jail detention provides a unique opportunity to address palliative care needs in medically complex older adults and to link them to appropriate community health and social services after release.10–12
While provision of palliative care to those with advanced and chronic illness can improve patient outcomes and reduce acute care use,13,14 little is known about the palliative care needs of older jail inmates. At a very basic level, little is known about the epidemiology of pain in older jail inmates. Undertreated pain increases distress, worsens health and function, and increases acute care utilization and health care costs.15,16 Among older adults, pain is common and often underreported and undertreated,17,18 particularly for those of minority race or ethnicity.19,20 Factors commonly associated with pain in older adults, including functional impairment and multimorbidity,15,16 are also associated with acute care use21 and are disproportionately prevalent in older prisoners.22,23 Clinician misperceptions that pain is a normal part of aging and a lack of consensus regarding the optimal treatment of nonmalignant chronic pain in older adults mean that pain is often poorly managed in older adults.24,25 In jail, pain management is further complicated by concerns about misuse, diversion, and overdose in patients with substance use and/or mental health disorders.26 Additionally, concurrent heart failure, renal insufficiency or liver disease—all common in prisoners—may leave clinicians with few nonopioid treatment options.
Therefore, we conducted a study to describe the prevalence of, and factors associated with, pain and the treatment of pain in older jail inmates. This basic epidemiologic knowledge is needed to inform the development of evidence-based palliative care treatment strategies for this medically complex and rapidly growing population of patients with serious and chronic illness.
Methods
Participants and design
This study was conducted in a county jail, where inmates are typically held while awaiting trial or serving short sentences for relatively minor offenses. Jail inmates are considered “older” at age 55 due to high rates of premature functional impairment and multimorbidity.27 Therefore, this cross-sectional study included 210 inmates aged 55 or older incarcerated in a county jail between May and November 2012. Through consecutive sampling we enrolled inmates who had spent at least 48 hours in the jail, because inmates are often in transit or in court after arrest and not able to participate in interviews during their first 2 days in jail. Inmates were ineligible for this study if they did not speak English, Spanish, or Cantonese or were deemed a safety risk by the sheriff's deputy on duty. Research staff confirmed the eligibility of those who expressed interest in the study to the jail nurse and conducted the questionnaire with those who consented to participate using a teach-to-goal method. Teach-to-goal has been used to verify consent comprehension in low literacy older adults and is endorsed by the National Institutes of Health.28,29 Participants who did not remain in custody for 1 week after their interview and/or did not grant study staff access to their jail medical records were excluded from these analyses so that all participants had jail-based medication treatment records for the week after their interview.
Study questionnaires were read to participants in English, Spanish, or Cantonese by native-speaking interviewers and answers were transcribed by the interviewer. Jail medical records were reviewed and abstracted. Consistent with ethical standards and federal regulations governing human subjects research involving prisoners,30 participants were credited $10 to their jail accounts for use at the jail canteen or to be given to them in cash upon release as compensation for their time. This study was approved by the Human Research Protection Program at the University of California, San Francisco.
Main measures: Pain and analgesic treatment
Pain assessment was based on self-report using items from the validated Memorial Symptom Assessment Scale (MSAS), which is commonly used to assess pain and other symptoms.31 The MSAS was chosen because it has been used with older adults and medically vulnerable populations, including those with HIV, substance dependence, and mental illness.32,33 Participants who answered “yes” to “In the past week, did you experience any pain?” were categorized as experiencing pain and were asked follow-up questions regarding frequency and severity. All others were categorized as having “no pain” or “less than severe pain” in the past week. Participants reporting “severe or very severe” pain experienced “frequently or constantly” were categorized as having “severe frequent pain.” Because participants were new to the jail and were asked about pain in the prior week, pain reported in this study may have occurred in the jail, out of the jail, or both in and out of the jail.
We abstracted patient medical charts to determine analgesic use. Analgesics were classified using practice guidelines from the American Society of Anesthesiologists Task Force on Chronic Pain Management34 and analgesics from all recommended classes are available for clinicians to prescribe at the county jail in this study including nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, neuropathic pain relievers such as gabapentin (all categorized as nonopioid analgesics), and/or opioid analgesics. All medications given to inmates are listed in the jail medical record, including nonopioid analgesics available over the counter in the community. Participants were categorized as receiving analgesics if they received one or more analgesic in jail in the week following their participation in the study. Analgesics were then categorized according to whether they were opioids. Opioid replacement therapy for opioid dependence was excluded from analyses. Only analgesics received during the stay in jail were included.
Other measures: Sociodemographics and health
Other collected measures included demographic characteristics and annual income (less than $15,000 versus $15,000 or more based on national Medicaid income eligibility criteria). Medical and mental health conditions were assessed by self-report using validated questions from the Health and Retirement Study (HRS).35 Serious mental illness was defined using the Bureau of Justice Statistics' definition, which includes a diagnosis of major depression or mania or any psychotic disorder.36 Self-report was used because medical diagnoses might not be included in all jail medical records because not all inmates are seen in the jail clinic within 48 hours of arrest. Self-report of medical conditions is well-validated in older adults,37 including in medically vulnerable populations.38 To minimize underrepresentation of medical diagnoses for inmates who were unaware of their medical diagnoses, we also abstracted medical conditions from jail medical records. We defined multimorbidity as having two or more chronic conditions.
Geriatric health factors commonly associated with pain in older adults were collected, including falls in the last 3 months and functional impairment (difficulty with one or more activity of daily living [ADL]—bathing, feeding, dressing, transferring, or toileting—in the prior 2 weeks).15,16 Social and behavioral health risk factors assessed included predetainment homelessness, medication insecurity (not having enough money for medications39), drug use, and problem alcohol use. Homelessness was defined as spending 1 or more nights outside or in a homeless shelter within 30 days of arrest.40 Drug use was determined by jail medical record documentation of drug dependence or an answer of “no” to a validated Drug Abuse Screening Test41 item, “In the last year, could you get through the week without using drugs?” Problem alcohol use was defined as medical record documentation of current alcohol dependence or a positive screen on the three-item AUDIT-C.42 We also collected information on a validated question about self-reported arrest related to alcohol or drug-related charges.43
Acute care use prior to incarceration was assessed because undertreated pain is a common cause of acute care use in older adults.21 Acute care use was assessed by asking “In the 3 months before jail, did you ever visit an emergency department?” and “In the 3 months before jail, did you ever stay overnight in a hospital?”
Statistical analysis
Participant characteristics were analyzed using descriptive statistics. Bivariate analyses using χ2 tests were conducted to determine the sociodemographic, health, and health-related factors and health care utilization patterns associated with pain in older jail inmates. Bivariate analyses using χ2 tests were also conducted to assess the relationship between pharmacologic pain management and prevalence of severe frequent pain, sociodemographics, and behavioral health risk factors. All analyses were conducted using Stata, version 12 software (StataCorp, College Station, TX). Study data were collected and managed using REDCap electronic data capture.44
Results
Sample characteristics
During the study period, 319 adults aged 55 or older spent at least 48 hours in the county jail. Overall, 23 (7%) did not meet inclusion criteria: 7 (2%) did not speak English, Spanish, or Cantonese and 16 (5%) were deemed a safety risk to interviewers by the sheriff's department. Of the 296 inmates who met inclusion criteria, 44 (15%) declined to participate and 252 (85%) were enrolled in the study. Two participants (<1%) subsequently withdrew, 22 (9%) did not grant access to jail medical records, and 18 (7%) did not remain in jail for 1 week after their interview, resulting in a final sample of 210 older inmates. Participants who were excluded from analyses because they did not grant access to their jail medical records or because they did not remain in jail for at least 1 week did not differ significantly from the remaining sample of 210 participants by sociodemographic status including age, gender, race/ethnicity, education level, or income, or by the study's primary outcomes, any pain and severe frequent pain (all p>0.1).
Participants' average age was 59 years (range, 55–75). They were predominantly male (95%) and black (60%). Most reported at least a high school or GED degree (74%) and an annual income below the 2013 Medicaid eligibility cutoff of approximately $15,000 (80%; Table 1).
Table 1.
Characteristics of Older Jail Inmates, n=210
| Characteristic | n (%) |
|---|---|
| Mean age (SD) | 59.4 (3.8) |
| Age 55–64, n (%) | 186 (89) |
| Race/ethnicity, n (%) | |
| Black | 125 (60) |
| White/non-Latino | 47 (22) |
| Latino | 21 (10) |
| Asian/Pacific Islander | 12 (6) |
| Female, n (%) | 10 (5) |
| Annual income <$15,000, n (%) | 168 (80) |
| High school, GED or more, n (%) | 155 (74) |
| Self-rated health, n (%) | |
| Poor or fair | 111 (53) |
| Good | 54 (26) |
| Very good or excellent | 45 (21) |
| Multimorbidity, n (%)a | 145 (69) |
| Serious mental illness, n (%)b | 104 (50) |
| ADL impairment, n (%)c | 70 (33) |
| Recent Fall(s), n (%)d | 66 (31) |
| Drug-/alcohol-related arrest, n (%) | 55 (26) |
| Drug use, n (%)e | 118 (56) |
| Problem alcohol use, n (%)f | 127 (60) |
| Homelessness, n (%)g | 98 (47) |
| Medication insecurity, n (%)h | 82 (39) |
| Recent acute care use, n (%)i | 106 (50) |
| Any pain, n (%) | 157 (75) |
Health conditions determined through self-report and/or documentation in the jail medical record. “Multimorbidity” includes two or more of the physical health conditions: hypertension, diabetes, cancer (not skin), chronic lung disease, heart disease (heart attack, coronary heart disease, or angina), congestive heart failure, stroke, HIV/AIDS, hepatitis C, or arthritis/rheumatism.
Includes any major depressive, manic or psychotic disorder as determined through self-report and/or documentation in the jail medical record.
Defined as having difficulty with ≥1 ADL (bathing, eating, transferring, toileting or dressing).
Defined as any self-reported fall to the ground within the last 3 months.
Defined as documentation of current drug use in the jail medical record and/or answering “no” to “In the last year, could you get through the week without using drugs?”
Defined as documentation of current alcohol use disorder in jail medical record or a positive screen on the validated, three-item AUDIT-C.
Defined as needing to spend 1 or more nights outside in a homeless shelter in the 30 days prior to jail.
Defined as “yes” to “Was there a time in the last year when you did not have enough money for medications?”
Based on self-report of emergency department use or hospitalization in the 3 months prior to jail.
ADL, activity of daily living.
Prevalence of pain and associated factors
Overall, 157 (75%) participants reported having any pain and 81 (39%) reported severe frequent pain. Those with severe frequent pain were more likely to be female (9% versus 2%, p=0.05), have poor or fair self-rated health (72% versus 41%, p<0.001), have 2 or more chronic medical conditions (85% versus 59%, p<0.001), have one or more ADL difficulty (59% versus 18%, p<0.001), report a fall in the past 3 months (61% versus 13%, p<0.001), and have serious mental illness (59% versus 43%, p=0.03; Table 2). Participants with severe frequent pain were also more likely to report predetainment community acute care use (66% versus 42%, p=0.001). Chronic medical conditions associated with reports of severe frequent pain included hepatitis C, arthritis, chronic lung disease, and heart disease (Table 2).
Table 2.
Severe Frequent Pain and Associated Factors among Older Jail Inmates, n=210
| Characteristic | Less or no pain (n=129, 61%) | Severe frequent pain (N=81, 39%) | p value |
|---|---|---|---|
| Mean age (SD) | 59.5 (4.3) | 59.4 (3.8) | 0.91 |
| Age 55–64, n (%) | 114 (88.4) | 72 (88.9%) | 0.90 |
| Race/ethnicity, n (%) | |||
| Black | 77 (59.7) | 48 (59.3) | 0.37 |
| White/non-Latino | 25 (19.4) | 22 (27.2) | |
| Latino | 13 (10.1) | 8 (9.9) | |
| Asian/Pacific Islander | 10 (7.8) | 2 (2.5) | |
| Female, n (%) | 3 (2.3) | 7 (8.6) | 0.05 |
| Annual income <$15,000, n (%) | 100 (80) | 68 (86.1) | 0.27 |
| High school, GED or more, n (%) | 99 (76.7) | 56 (69.1) | 0.22 |
| Self-rated health, n (%) | |||
| Poor or fair | 53 (41.1) | 58 (71.6) | |
| Good | 39 (30.2) | 15 (18.5) | <0.001 |
| Very good or excellent | 37 (28.7) | 8 (9.9) | |
| Hypertension, n (%) | 77 (59.7) | 58 (71.6) | 0.08 |
| Diabetes, n (%) | 24 (18.6) | 14 (17.3) | 0.81 |
| Heart attack or coronary disease, N (%) | 20 (15.5) | 26 (32.1) | 0.01 |
| Congestive heart failure, n (%) | 7 (5.4) | 10 (12.3) | 0.07 |
| Stroke, n (%) | 11 (8.5) | 13 (16) | 0.10 |
| Cancer, n (%)a | 7 (5.4) | 10 (12.3) | 0.70 |
| Chronic lung disease, n (%) | 14 (10.9) | 21 (25.9) | 0.004 |
| HIV/AIDS, n (%) | 5 (3.9) | 6 (7.4) | 0.26 |
| Hepatitis C, n (%) | 55 (42.6) | 53 (65.4) | 0.001 |
| Arthritis or rheumatism, n (%) | 50 (38.8) | 53 (65.4) | <0.001 |
| Multimorbidity, n (%)b | 76 (58.9) | 69 (85.2) | <0.001 |
| Serious mental illness, n (%)c | 56 (43.4) | 48 (59.3) | 0.03 |
| ADL impairment, n (%)d | 23 (18) | 57 (58.8) | <0.001 |
| Bathing | 11 (7.9) | 31 (35.6) | <0.001 |
| Dressing | 7 (5) | 21 (24.1) | <0.001 |
| Toileting | 5 (3.6) | 25 (28.7) | <0.001 |
| Transferring | 17 (12.2) | 39 (45.9) | <0.001 |
| Eating | 6 (4.3) | 27 (31) | <0.001 |
| Needing a cane, wheelchair, or walker | 27 (19.3) | 46 (52.3) | <0.001 |
| Recent Fall(s), n (%)e | 17 (13.4) | 49 (60.5) | <0.001 |
| Drug-/alcohol-related arrest, n (%) | 28 (22.6) | 27 (34.2) | 0.07 |
| Drug use, n (%)f | 72 (55.8) | 46 (56.8) | 0.89 |
| Problem alcohol use, n (%)g | 80 (62) | 47 (58) | 0.57 |
| Homelessness, n (%)h | 62 (48.4) | 36 (45) | 0.63 |
| Medication insecurity, n (%)i | 45 (36.9) | 37 (48.1) | 0.12 |
| Recent acute care use, n (%)j | 54 (42.2) | 52 (65.8) | 0.001 |
Excluding minor skin cancers.
Health conditions determined through self-report and/or documentation in the jail medical record.
Includes any major depressive, manic, or psychotic disorder and was determined through self-report and/or documentation in the jail medical record.
Defined as having difficulty with one or more ADL (bathing, eating, transferring, toileting or dressing)30 and/or needing a cane, wheelchair, walker, or other aid to help with daily activities.
Defined as any self-reported fall to the ground within the last 3 months.
Defined as documentation of current drug use in the jail medical record and/or answering “no” to “In the last year, could you get through the week without using drugs?”
Defined as documentation of current alcohol use disorder in jail medical record or a positive screen on the validated, three-item AUDIT-C.
Defined as needing to spend 1 or more nights outside in a homeless shelter in the 30 days prior to jail.
Defined as answering “yes” to “Was there a time in the last year when you did not have enough money for medications?”
Based on self-report of emergency department use or hospitalization in the 3 months prior to jail.
ADL, activities of daily living.
Participants who reported severe frequent pain had similar rates of drug use (57% versus 56%, p=0.89) and problem alcohol use (58% versus 62%, p=0.57) as those reporting less or no pain and the two groups were equally likely to report being in jail for a drug- or alcohol-related arrest (34% versus 23%, p=0.07; Table 2).
Use of pharmacologic analgesics according to level of pain
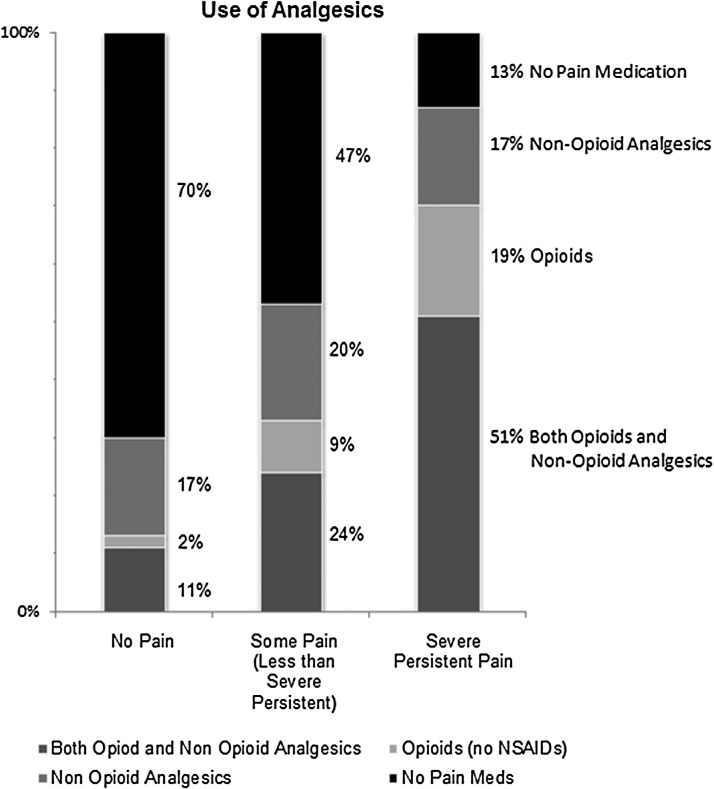
In the week after the interview, 126 (60%) of all participants received one or more analgesic medication; 23 (11%) received opioid therapy alone, 38 (18%) received one or more nonopioid analgesic(s) alone, and 65 (31%) received both opioid therapy and one or more nonopioid analgesic. Analgesic medications were received by 30% of those with no pain, 53% with less than severe frequent pain, and 87% with severe frequent pain (p<0.001; Fig. 1). Of 11 participants with severe frequent pain who did not receive any analgesics within a week, 9 (82%) were evaluated by a jail clinician.
FIG. 1.
One-week use of analgesics according to level of self-reported pain, n=210. During the week after the study interview, analgesic medications were received by 30% of those who reported no pain, 53% of those reporting less than severe frequent pain, and by 87% of those who reported severe frequent pain.
Factors associated with analgesic use
Participants who received any analgesic(s) were more likely to report any pain (87% versus 56%, p<0.001), severe frequent pain (56% versus 13%, p<0.001), multimorbidity (79% versus 55%, p=0.006), and poor or fair self-rated health (62% versus 39%, p=0.003). Those who received opioids were also more likely to report any pain (92% versus 62%, p<0.001), severe frequent pain (64% versus 21%, p<0.001), multimorbidity (77% versus 63%, p=0.02), and poor or fair self-rated health (65% versus 44%, p=0.01). No sociodemographic or behavioral health factors were associated with pharmacologic treatment of pain with any analgesics. Those who received opioids were no more likely to report that their incarceration was due to a drug- or alcohol-related offense (32% versus 23%, p=0.16); the groups did not differ according to drug use (60% versus 53%, p=0.32) or problem alcohol use (57% versus 63%, p=0.36).
Discussion
We found that in older jail inmates, severe frequent pain is common and is associated with multimorbidity, functional impairment, and recent community acute care use. In this study, rates of severe pain, chronic disease, disability, and acute care use in older jail inmates with a mean age of 59 were comparable to rates reported in community-dwelling adults with a median age of 75.45 While reports of recent falls among those without severe pain (13%) were on par with national averages in their age group, falls among older inmates with severe frequent pain (61%) were notably high. Similarly, participants with severe frequent pain were significantly more likely to report difficulties in each of the traditional activities of daily living (bathing, dressing, toileting, transferring, and eating), suggesting that untreated pain in this population may significantly limit independence, and negatively affect transitions back to the community for older former jail inmates after release. Participants who reported severe pain were also more likely to rate their health poor or fair or to suffer from multiple chronic conditions compared to those with less or no pain. These findings echo those of studies linking severe frequent pain to disproportionate acute care use in medically complex older adults46 and suggest that older inmates with severe frequent pain may be at particularly high risk for post-release acute care use.
Palliative care has been shown to improve health outcomes and lower cost for older adults with nonterminal, chronic illness by reducing symptom burden, improving transitions between care settings, and reducing acute care use.1,2,13,14,47 Yet in the nation's approximately 3000 jails, the adaptation and targeting of palliative care to chronically or seriously ill older adults has been largely overlooked. In prisons (which house those convicted of a crime serving sentences of 1 year or longer), health services guidelines created by the National Commission on Correctional Health Care include the provision of palliative care.48 Efforts to expand correctional palliative care have focused mainly on dying prisoners, successfully leading to the creation of prison-based hospice units in approximately 70 facilities nationwide.49 However, prison-based hospices face unique challenges, including restrictions on inmate movements and providers' access to patients, restricted pharmaceutical formularies, and a dearth of trained medical personnel.50 Moreover, the health care needs of prison inmates (generally serving long sentences) and jail inmates (generally awaiting trial or serving short sentences for relatively minor offenses) likely differ considerably, as jail inmates cycle between incarceration and community health systems far more rapidly and in greater number. A profound lack of data about the health care needs of seriously or chronically ill jail inmates limits the development and targeting of appropriate palliative care for the jail population. More research is also needed to better understand the palliative care needs of long-term prisoners with severe frequent pain and/or serious illness who are not at the end of life.
A first critical step to filling this gap in palliative care knowledge and programming is to develop an evidence base that describes the prevalence and treatment of pain and other symptoms in inmates because the optimal approach to treatment for these patients is uniquely complicated. Treatment of chronic pain in older adults is complex because aging is associated with increasing variance in both sensitivity to pain and responsiveness to treatment, more often requiring highly individualized approaches to pain management.51 Additionally, provider concerns about opioid analgesic prescribing to medically and socially vulnerable populations are well-documented, including the potential need for higher doses to achieve symptom relief, lower tolerance for discomfort, and the high risk of diversion and/or misuse-related mortality.26,52 However, reports of severe frequent pain in this study were not significantly associated with substance abuse or drug or alcohol related arrests, suggesting that the apparent unmet need for palliative care in this population cannot be primarily attributed to drug-seeking or other behaviors associated with criminal justice involved populations. In addition, this study found variability in the treatment of pain for older jail inmates, underscoring the need for evidence-based treatment guidelines that address the needs of this unique population.
To address this challenge, some have called for higher quality opioid prescribing guidelines53 while other care delivery systems have taken measures to restrict opioid analgesic prescriptions for chronic pain. For example, New York's I-STOP program aims to reduce overprescribing of opioids by requiring that practitioners use an electronic prescribing service that reports data to the state for review.54 While in this study, neither participants who reported severe frequent pain nor those who received opioid therapy were more likely to have self-reported or documented evidence of drug or problem alcohol use or to report that their current incarceration was due to a drug or alcohol-related offense, participants overall had high rates of drug and problem alcohol use. Future studies should also focus on developing an evidence-based approach to pain management in this population that carefully evaluates nonpharmacologic interventions to treat pain.
Several limitations should be considered when interpreting our results. The relatively small number of women in this study limits the result showing that women were more likely to report severe frequent pain. However, these underpowered findings are consistent with studies showing that women use more correctional health care services and experience greater morbidity and health care needs than incarcerated men,55 and with studies reporting that community-dwelling women report pain at higher rates than men.56 Additionally, this study was conducted in one urban jail system and did not explore whether analgesic prescriptions were initiated in the jail or in the community. However, while pain management policy and practice may differ in other jails and communities, criminal justice populations are rapidly aging nationwide and this study constitutes a critical first step in understanding the prevalence of pain and the associated challenges of pain treatment in this population. Future studies should also investigate whether older prisoner populations have similarly high rates of pain, and the prevalence of other palliative care needs including symptoms and psychological distress related to advanced illness among older jail and prison inmates.
In this study, older jail inmates with severe frequent pain constituted a medically complex population with significantly higher rates of multimorbidity, functional impairment, recent fall(s), recent community acute care use and serious mental illness compared to those with less or no pain. Because pain is a leading chief complaint in emergency department visits,46 a robust, evidence-based approach to providing jail-based palliative care to seriously or chronically ill older inmates that includes linkages to community-based palliative care could have a positive impact on patients' quality of life while simultaneously helping community safety-net systems reduce acute care use.27,57–60 Yet aside from the development of prison-based hospice units, palliative medicine has been largely absent from standards of care for incarcerated populations. The first step toward adapting community-based palliative care to the jail setting is to recognize the health care implications of an aging inmate population. With this knowledge, we can develop evidence-based palliative care models that can account for the treatment concerns providers face when caring for this complex population,3 including integration of nonpharmacologic therapies for symptom management, and development of population-focused risk evaluation and mitigation strategies to increase treatment compliance, minimize misuse, improve pain control, and reduce acute care use after release.
Acknowledgments
All authors listed here meet the criteria of authorship for this manuscript and no others contributed to this manuscript sufficiently to warrant inclusion as an author.
B.A.W received support from the National Institute of Aging (K23AG033102), The Jacob & Valeria Langeloth Foundation, and The UCSF Program for the Aging Century. This project was also supported in part by a Pilot and Exploratory Project Support Grant from the National Palliative Care Research Center (NPCRC). Sponsors played no role in the design, methods, subject recruitment, data collection, analysis, or preparation of this manuscript.
This paper was accepted for oral presentation at the 2014 American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association Annual Assembly in San Diego, California held in March, 2014.
Author Disclosure Statement
B.A.W. has served as an expert witness and as a court consultant in legal cases related to prison conditions of confinement. These relationships have included: the ACLU National Prison Project; the Disability Rights Legal Center; Hunton and Williams LLP; Holland and Knight LLP; The University of Denver Student Law Office; and The Office of the Independent Medical Monitor, MI. These relationships had no role in the decision to write this manuscript and did not influence the data analyses.
B.A.W., A.K.S., and C.S.R. are employees of the Department of Veterans Affairs. The opinions expressed in this manuscript may not represent those of the VA. J.G. is an employee of the San Francisco Department of Public Health. The views expressed herein do not necessarily reflect the official policies of the City and County of San Francisco; nor does mention of the San Francisco Department of Public Health imply its endorsement.
No other competing financial interests exist.
References
- 1.Kelley AS, Meier DE: Palliative care—A shifting paradigm. N Engl J Med 2010;363:781–782 [DOI] [PubMed] [Google Scholar]
- 2.Meier DE, Thar W, Jordan A, et al. : Integrating case management and palliative care. J Palliat Med 2004;7:119–134 [DOI] [PubMed] [Google Scholar]
- 3.Beck AJ. The Importance of Successful Reentry to Jail Population Growth. Bureau of Justice Statistics, Department of Justice. Presented to the The Urban Institute Jail Reentry Roundtable, Washington D.C., 2006 [Google Scholar]
- 4.Bureau of Justice Statistics: Profile of Jail Inmates 2002. Department of Justice. Office of Justice Programs, Bureau of Justice Statistics; Washington, D.C: http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=1118 (Last accessed September17, 2012) [Google Scholar]
- 5.Beck AJ, Berzofsky M: Sexual Victimization in Prison and Jails Reported by Inmates, 2008–2009 [Table T6]. NCJ 231169. Washington, D.C.: Department of Justice. Office of Justice Programs, Bureau of Justice Statistics, 2010, p. 91 [Google Scholar]
- 6.Snyder HN: Arrest in the United States, 1990–2010. NCJ 239423. Washington, D.C.: Department of Justice. Office of Justice Programs, Bureau of Justice Statistics, 2012, p. 26 [Google Scholar]
- 7.Binswanger IA, Stern MF, Deyo RA, et al. : Release from prison—A high risk of death for former inmates. N Engl J Med 2007;356:157–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bureau of Justice Statistics: Mortality in Local Jails, 2000–2007. Washington, D.C.: Department of Justice. Office of Justice Programs, Bureau of Justice Statistics; http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=2197 (Last accessed September17, 2012) [Google Scholar]
- 9.Williams BA, McGuire J, Lindsay RG, et al. : Coming home: Health status and homelessness risk of older pre-release prisoners. J Gen Intern Med 2010;25:1038–1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freudenberg N: Jails, prisons, and the health of urban populations: A review of the impact of the correctional system on community health. J Urban Health 2001;78:214–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hammett T, Roberts C, Kennedy S: Health-related issues in prisoner reentry. Crime Delinq 2001;47:290–409 [Google Scholar]
- 12.Lincoln T, Kennedy S, Tuthill R, et al. : Facilitators and barriers to continuing healthcare after jail: A community-integrated program. J Ambul Care Manage 2006;29:2–16 [DOI] [PubMed] [Google Scholar]
- 13.Meier D: Palliative care as a quality improvement strategy for advanced, chronic illness. J Healthc Qual 2005;27:33–39 [DOI] [PubMed] [Google Scholar]
- 14.Rabow MW, Dibble SL, Pantilat SZ, McPhee SJ: The comprehensive care team: A controlled trial of outpatient palliative medicine consultation. Arch Intern Med 2004;164:83–91 [DOI] [PubMed] [Google Scholar]
- 15.Chai E, Horton JR: Managing pain in the elderly population: Pearls and pitfalls. Curr Pain Headache Rep 2010;14:409–417 [DOI] [PubMed] [Google Scholar]
- 16.Herr K: Pain in the older adult: An imperative across all health care settings. Pain Manag Nurs 2010;11(2 Suppl):S1–10 [DOI] [PubMed] [Google Scholar]
- 17.Pergolizzi J, Boger RH, Budd K, et al. : Opioids and the management of chronic severe pain in the elderly: Consensus statement of an International Expert Panel with focus on the six clinically most often used World Health Organization Step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract 2008;8:287–313 [DOI] [PubMed] [Google Scholar]
- 18.The management of persistent pain in older persons. J Am Geriatr Soc 2002;50(6 Suppl):S205–224 [DOI] [PubMed] [Google Scholar]
- 19.Chen I, Kurz J, Pasanen M, et al. : Racial differences in opioid use for chronic nonmalignant pain. J Gen Intern Med 2005;20:593–598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joynt M, Train MK, Robbins BW, et al. : The impact of neighborhood socioeconomic status and race on the prescribing of opioids in emergency departments throughout the United States. J Gen Intern Med 2013;28:1604–1610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gruneir A, Silver MJ, Rochon PA: Emergency department use by older adults: A literature review on trends, appropriateness, and consequences of unmet health care needs. Med Care Res Rev 2011;68:131–155 [DOI] [PubMed] [Google Scholar]
- 22.Loeb SJ, Steffensmeier D, Lawrence F: Comparing incarcerated and community-dwelling older men's health. West J Nurs Res Mar 2008;30:234–249; discussion 250–238 [DOI] [PubMed] [Google Scholar]
- 23.Williams BA, Lindquist K, Hill T, et al. : Caregiving behind bars: Correctional officer reports of disability in geriatric prisoners. J Am Geriatr Soc 2009;57:1286–1292 [DOI] [PubMed] [Google Scholar]
- 24.Abdulla A, Adams N, Bone M, et al. : Guidance on the management of pain in older people. Age Ageing 2013;42(Suppl 1):i1–57 [DOI] [PubMed] [Google Scholar]
- 25.Arnstein P: Balancing analgesic efficacy with safety concerns in the older patient. Pain Manag Nurs 2010;11(2 Suppl):S11–22 [DOI] [PubMed] [Google Scholar]
- 26.Rich JD, Boutwell AE, Shield DC, et al. : Attitudes and practices regarding the use of methadone in US state and federal prisons. J Urban Health 2005;82:411–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williams BA, Stern MF, Mellow J, et al. : Aging in correctional custody: Setting a policy agenda for older prisoner health care. Am J Public Health 2012;102:1475–1481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Office of Disease Prevention and Health Promotion: Quick Guide to Health Literacy. U.S. Department of Health and Human Services. October, 2013. www.health.gov/communication/literacy/quickguide/quickguide.pdf (Last accessed September17, 2012)
- 29.Sudore RL, Landefeld CS, Williams BA, et al. : Use of a modified informed consent process among vulnerable patients: A descriptive study. J Gen Intern Med 2006;21:867–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hanson RK, Letourneau EJ, Olver ME, Miner MH: Incentives for offender research participation are both ethical and practical. Crim Justice Behav 2012;39 [Google Scholar]
- 31.Portenoy RK, Thaler HT, Kornblith AB, et al. : The Memorial Symptom Assessment Scale: An instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer 1994;30A:1326–1336 [DOI] [PubMed] [Google Scholar]
- 32.Aouizerat BE, Miaskowski CA, Gay C, et al. : Risk factors and symptoms associated with pain in HIV-infected adults. J Assoc Nurses AIDS Care 2010;21:125–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ritchie C, Dunn LB, Paul SM, et al. : Differences in the symptom experience of older oncology outpatients. J Pain Symptom Manage 2014;47:697–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology 2010;112:810–833 [DOI] [PubMed] [Google Scholar]
- 35.Growing Older in America: The Health & Retirement Study. National Institute on Aging, National Institutes of Health, U.S. Department of Health and Human Services. 2012Participant Lifestyle Questionnaire. http://hrsonline.isr.umich.edu/modules/meta/2012/core/qnaire/online/HRS2012_SAQ_Final.pdf (Last accessed June4, 2013)
- 36.James DJ, Glaze LE: Mental Health Problems of Prison and Jail Inmates. NCJ 213600. Washington, D.C.: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, 2006 [Google Scholar]
- 37.Bush TL, Miller SR, Golden AL, Hale WE: Self-report and medical record report agreement of selected medical conditions in the elderly. Am J Public Health 1989;79:1554–1556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brown RT, Kiely DK, Bharel M, Mitchell SL: Geriatric syndromes in older homeless adults. J Gen Intern Med 2012;27:16–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Recommended Sociodemographic Measures. University of California, San Francisco, Center for Aging in Diverse Communities, Measurement and Methods Core; http://dgim.ucsf.edu/cadc/mm/msesenglish.pdf (Last accessed June24, 2013) [Google Scholar]
- 40.Homeless Emergency Assistance and Rapid Transition to Housing: Defining “Homeless” (24 CFR Parts 91, 582, and 283 [Docket No. FR-5333-F-02] RIN 2506-AC26)(2010)
- 41.Skinner HA: The drug abuse screening test. Addict Behav 1982;7:363–371 [DOI] [PubMed] [Google Scholar]
- 42.Bush K, Kivlahan DR, McDonell MB, et al. : The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 1998;158:1789–1795 [DOI] [PubMed] [Google Scholar]
- 43.Maisto SA, Sobell LC, Sobell MB: Corroboration of drug abusers' self-reports through the use of multiple data sources. Am J Drug Alcohol Abuse 1982;9:301–308 [DOI] [PubMed] [Google Scholar]
- 44.Harris PA, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sawyer P, Bodner EV, Ritchie CS, Allman RM: Pain and pain medication use in community-dwelling older adults. Am J Geriatr Pharmacother 2006;4:316–324 [DOI] [PubMed] [Google Scholar]
- 46.Samaras N, Chevalley T, Samaras D, Gold G: Older patients in the emergency department: A review. Ann Emerg Med 2010;56:261–269 [DOI] [PubMed] [Google Scholar]
- 47.Kelly B, McClement S, Chochinov HM: Measurement of psychological distress in palliative care. Palliat Med 2006;20:779–789 [DOI] [PubMed] [Google Scholar]
- 48.National Commission for Correctional Health Care: Standards for Health Services in Prisons. Chicago, IL: National Commission for Correctional Health Care, 2008 [Google Scholar]
- 49.Stone K, Papadopoulos I, Kelly D: Establishing hospice care for prison populations: An integrative review assessing the UK and USA perspective. Palliat Med 2012;26:969–978 [DOI] [PubMed] [Google Scholar]
- 50.Linder JF, Meyers FJ: Palliative care for prison inmates: “Don't let me die in prison.” JAMA 2007;298:894–901 [DOI] [PubMed] [Google Scholar]
- 51.Fine PG: Chronic pain management in older adults: Special considerations. J Pain Symptom Manage 2009;38(2 Suppl):S4–S14 [DOI] [PubMed] [Google Scholar]
- 52.Gomes T, Mamdani MM, Dhalla IA, et al. : Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med 2011;171:686–691 [DOI] [PubMed] [Google Scholar]
- 53.Nuckols TK, Anderson L, Popescu I, et al. : Opioid prescribing: A systematic review and critical appraisal of guidelines for chronic pain. Ann Intern Med 2014;160:38–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Part 80 (10 NYCRR). Electronic Prescribing, Dispensing, and Recordkeeping of Controlled Substances. Amendment to Article 2-A and Article 33 of the Public Health in New York State. Last Updated March27, 2013. www.health.ny.gov/regulations/recently_adopted/docs/2013-02-13_electronic_prescribing_dispensing_and_recordkeeping_of_controlled_substances.pdf (Last accessed June4, 2013)
- 55.Lindquist CH, Lindquist CA: Health behind bars: Utilization and evaluation of medical care among jail inmates. J Community Health 1999;24:285–303 [DOI] [PubMed] [Google Scholar]
- 56.Ruau D, Liu LY, Clark JD, et al. : Sex differences in reported pain across 11,000 patients captured in electronic medical records. J Pain Mar 2012;13:228–234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Human Rights Watch: Old Behind Bars: The Aging Prison Population in the United States. New York: Human Rights Watch, 2012 [Google Scholar]
- 58.American Civil Liberties Union. At America's Expense: The Mass Incarceration of the Elderly. New York: American Civil Liberties Union, 2012 [Google Scholar]
- 59.Williams BA, Abraldes RM. Growing older: Challenges of prison and re-entry for the elderly. In: Greifinger RB. (ed): Public Health Behind Bars: From Prisons to Communities: Springer, 2007, pp. 56–72 [Google Scholar]
- 60.Williams BA, Goodwin JS, Baillargeon J, et al. : Addressing the aging crisis in U.S. criminal justice health care. J Am Geriatr Soc 2012;60:1150–1156 [DOI] [PMC free article] [PubMed] [Google Scholar]