Abstract
Spontaneous coronary artery dissection (SCAD) is a rare cause of acute myocardial infarction (AMI). We are presenting a case of a young woman with a history of untreated dyslipidemia presented with AMI secondary to left anterior descending coronary artery dissection during postpartum period. Physicians should be aware of this rare etiology of AMI which occurs during pregnancy and postpartum, since early diagnosis and treatment play a key role in saving both the mother and the baby. It is important to screen for other possible causes such as collagen vascular diseases, blunt injury to the chest, or cocaine abuse.
Keywords: Acute myocardial infarction, coronary artery dissection, postpartum, pregnancy, women
INTRODUCTION
Spontaneous coronary artery dissection (SCAD) is a rare cause of acute myocardial infarction (AMI), occurs predominantly in young, otherwise healthy people.[1] The predisposing factors of SCAD are pregnancy and postpartum period; vigorous exercise; sexual intercourse; recent chest trauma; cocaine abuse; medications like oral contraceptives, cyclosporine, 5-fluorouracil, and fenfluramine; connective tissue diseases like Marfan and Ehlers-Danlos syndromes; isolated fibromuscular dysplasia; severe hypertension; autoimmune diseases (polyarteritis nodosa, Kawasaki, systemic lupus erythematosus, and rheumatoid arthritis), inflammatory bowel disease, antiphospholipid syndrome, and atherosclerosis.[2,3] We are describing a case of SCAD in a 32-year-old female presented with AMI 2 weeks after delivery.
CASE REPORT
A 32-year-old female gave birth to a baby following a repeat cesarean section. Two weeks later, she presented to the emergency department with acute chest pain. It was associated with nausea, vomiting, palpitations, and dizziness. The patient had a history of untreated dyslipidemia; but no history of hypertension, diabetes, smoking, or oral contraceptive use. Patient had gestational diabetes with most recent HbA1C was 5.5. Family history of early coronary artery disease was negative. Initial troponin and creatine kinase-MB (CK-MB) were normal. Electrocardiogram (ECG) revealed acute ST elevation myocardial infarction [Figure 1]. She underwent emergent coronary angiography (CA), which demonstrated spontaneous distal left anterior descending (LAD) artery dissection [Figure 2] and probable extended intramural hematoma to the distal left main coronary artery (LMCA). TIMI 2 flow was present distally. The right coronary artery (RCA) and left circumflex coronary artery (LCx) appeared normal. The left ventricular function was severely reduced with akinesis of the anterior and apical walls. Coronary CT angiography confirmed the dissection of the posterior LMCA extending into the LAD [Figure 3]. The narrowest true lumen in the distal left main was 1.3 mm in diameter. Given the fragility of the vessel and diffuse nature, no percutaneous intervention was done. She was continued on eptifibatide and heparin. She was discharged on aspirin 81 mg once daily, metoprolol 50 mg twice daily, and lisinopril 2.5 mg once daily. Lipid panel showed cholesterol 249 mg/dl, triglycerides 72 mg/dl, high density lipoprotein (HDL) 52 mg/dl, and low density lipoprotein (LDL) 182 mg/dl; however, patient refused to take statin therapy.
Figure 1.
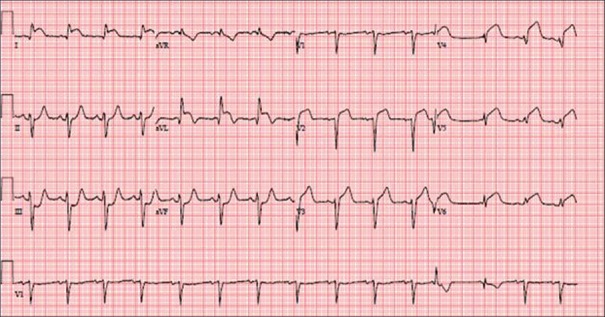
Electrocardiogram showing ST elevation in Lead 1, aVL, V2 through V6
Figure 2.

Coronary angiography. The arrow indicates dissection at the distal left main artery, which is same position as seen in coronary computed tomography angiography
Figure 3.
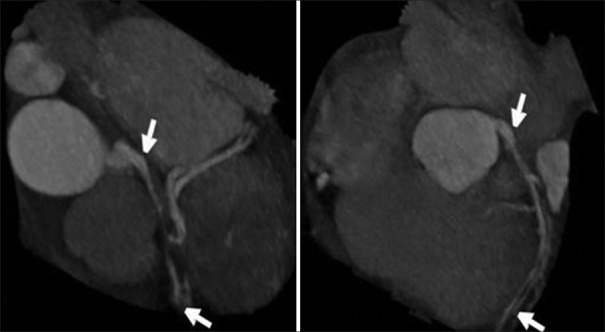
Coronary CT angiography. Arrows indicate the flip of dissection in the proximal and distal sites of left main artery. We can also see the false lumen with blood clot
DISCUSSION
SCAD is an infrequent cause of acute coronary syndrome (ACS) and accounts for 0.2-0.3% of cases in the general population; however, it may account for 25% of cases in pregnant and postpartum women.[3] In two case series involving 83 patients presented with pregnancy-related SCAD, the mean age was 33 years and 72% occurred during the first 2 weeks after the delivery.[4,5] The most often involved artery in women is LAD, and the RCA in men. The most frequent sites of lesion in SCAD are the LAD (78%), the LMCA (24%), the RCA (20%), and the LCx (4%).[4]
According to a study done by James et al., AMI occurs in about 6.2 cases per 100,000 deliveries and the mortality rate was found to be 5.1%, substantially lower than in older studies (7.3-37%) which might be due to improvement in the management of these patients.[3,6] The increased risk of AMI in pregnant women are related to age over 30 years, hypertension, eclampsia and pre-eclampsia, third trimester of pregnancy, multiparity, diabetes, smoking, thrombophilia, need for blood transfusion, and infection following delivery.[3,6] In another study that analyzed 125 pregnant women presented with MI, the main cause was found to be atherosclerosis of coronary arteries. CA was performed in 68 of those patients; they found coronary atherosclerosis in 43%, coronary artery dissection in 16%, thrombus without atherosclerosis in 21%, and normal coronary arteries in 29% of patients.[3]
The clinical presentation of SCAD ranges from asymptomatic to acute coronary syndrome, cardiogenic shock, and sudden death. Some theories attribute these increased rates of SCAD in pregnant and postpartum women to hormonal and hemodynamic changes in pregnancy; such as increase in cardiac output by 50%, excess progesterone and estrogen causing medial necrosis, disruption of the vaso vasorum, relaxin causing severe vasoconstriction, and alterations in the coagulation-fibrinolysis system.[5] Borczuk et al., in their study found that the two SCAD cases had eosinophils along the plane of the dissection and may prepare the tissue in some way for collagenolysis or remove a potential inhibitor of collagenolysis.[7] The diagnosis is usually made by CA, CT angiography, or intravascular ultrasound (IVUS). The angiographic diagnosis of SCAD depends on the visualization of two lumina separated by a radiolucent intimal flap. IVUS delineates the true and false lumen of the vessel, intimal tear length and morphology, and also helps to distinguish atherosclerotic stenosis from intramural hematoma.[8]
The management strategy in SCAD depends on the site of the dissection, number of vessels involved, distal coronary blood flow, hemodynamic status of the patient, and the availability of coronary intervention. In the hemodynamically stable patients with limited dissections, a trial of medical therapy is recommended including beta-blockers to reduce vascular shear forces and antiplatelet agents such as aspirin and clopidogrel to reduce thrombus formation. Calcium channel blockers can be used for coronary vasospasm. Thrombolysis may be useful in arteries where intramural hematoma is compressing the true lumen, allowing the artery to re-expand.[9] A potential complication of thrombolysis includes the propagation of the dissection and expansion of intramural hematoma.[10] Patients with single-vessel SCAD with ongoing signs of ischemia, stenting is the treatment of choice with the disadvantage of extension of intramural thrombus up-or downstream of the stent. Glycoprotein IIb/IIIa inhibitors have been used to treat SCAD in both conservative and adjuvant therapy during stenting. Coronary artery bypass graft (CABG) has been indicated in patients with multivessel dissections, SCAD involving the LMCA and when the PCI failed. The main difficulty with CABG is the risk of grafting the false lumen, with subsequent irreversible myocardial damage or death.
CONCLUSION
Consider the diagnosis of SCAD in any young female patient who presents with acute chest pain during peripartum period without conventional coronary artery disease risk factors. Management of the patient with medical or interventional therapy depends mainly on the extent of the dissection. In young people, especially when lacking typical risk factors and with an infarction, thrombolysis should be avoided until coronary imaging excludes dissection.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Thompson EA, Ferraris S, Gress T, Ferraris V. Gender differences and predictors of mortality in spontaneous coronary artery dissection: A review of reported cases. J Invasive Cardiol. 2005;17:59–61. [PubMed] [Google Scholar]
- 2.Almafragi A, Convens C, Heuvel PV. Spontaneous healing of spontaneous coronary artery dissection. Cardiol J. 2010;17:92–5. [PubMed] [Google Scholar]
- 3.Roth A, Elkayam U. Acute myocardial infarction associated with pregnancy. Ann Intern Med. 1996;125:751–62. doi: 10.7326/0003-4819-125-9-199611010-00009. [DOI] [PubMed] [Google Scholar]
- 4.Koul AK, Hollander G, Moskovits N, Frankel R, Herrera L, Shani J. Coronary artery dissection during pregnancy and the postpartum period: Two case reports and review of literature. Catheter Cardiovasc Interv. 2001;52:88–94. doi: 10.1002/1522-726x(200101)52:1<88::aid-ccd1022>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 5.Appleby CE, Barolet A, Ing D, Ross J, Schwartz L, Seidelin P, et al. Contemporary management of pregnancy-related coronary artery dissection: A single-centre experience and literature review. Exp Clin Cardiol. 2009;14:e8–e16. [PMC free article] [PubMed] [Google Scholar]
- 6.James AH, Jamison MG, Biswas MS, Brancazio LR, Swamy GK, Myers ER. Acute myocardial infarction in pregnancy: A United States population-based study. Circulation. 2006;113:1564–71. doi: 10.1161/CIRCULATIONAHA.105.576751. [DOI] [PubMed] [Google Scholar]
- 7.Borczuk AC, van Hoeven KH, Factor SM. Review and hypothesis: The eosinophil and peripartum heart disease (myocarditis and coronary artery dissection)--coincidence or pathogenetic significance? Cardiovasc Res. 1997;33:527–32. doi: 10.1016/s0008-6363(96)00257-x. [DOI] [PubMed] [Google Scholar]
- 8.Arnold JR, West NE, van Gaal WJ, Karamitsos TD, Banning AP. The role of intravascular ultrasound in the management of spontaneous coronary artery dissection. Cardiovasc Ultrasound. 2008;6:24. doi: 10.1186/1476-7120-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Missouris CG, Ring A, Ward D. A young woman with chest pain. Heart. 2000;84:e12. doi: 10.1136/heart.84.6.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klutstein MW, Tzivoni D, Bitran D, Mendzelevski B, Ilan M, Almagor Y. Treatment of spontaneous coronary artery dissection: report of three cases. Cathet Cardiovasc Diagn. 1997;40:372–6. doi: 10.1002/(sici)1097-0304(199704)40:4<372::aid-ccd11>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]


