Abstract
Nutrition therapy as part of lifestyle care is recommended for people with type 2 diabetes. However, most people with diabetes do not follow this guideline. Changing eating habits involves obtaining knowledge and building practical skills such as shopping, meal preparation, and food storage. Just as fitness coaches use their specific knowledge base in fitness to enhance the effectiveness of their coaching, credentialed chefs trained as health coaches might combine their culinary expertise with coaching in order to improve clients' food choices and lifestyles.
This report documents the case of a 55-year-old white male physician, single and living alone, who was recently diagnosed with type 2 diabetes and reported chronic stress, sedentary behavior, and unhealthy eating habits. He participated in a chef coaching program of 8 weekly one-on-one 30-minute coaching sessions via Skype delivered by a chef trained as a health coach. During the first five meetings, the patient's goals were primarily culinary; however, with his success in accomplishing these goals, the patient progressed and expanded his goals to include other lifestyle domains, specifically exercise and work-life balance. At the end of the program, the patient had improved both his nutritional and exercise habits, his confidence in further self-care improvement, and his health parameters such as HgA1c (8.8% to 6.7%; normal <6.5%).
We conclude that chef coaching has the potential to help people with diabetes improve their practical culinary skills and implement them so that they eat better and, further, has the potential to help them improve their overall self-care. We intend to further develop chef coaching and assess its potential as we learn from its implementation.
Key Words: Coaching, cooking, lifestyle, diabetes, self-care
摘要
作为生活护理的一部分,营养疗法 是 2 型糖尿病患者的推荐疗法。 然而,大多数糖尿病患者并不遵守 此疗法准则。改变饮食习惯涉及到 获得知识以及掌握实践技能,如购 物、做饭和储藏食物。就像健身教 练利用自己的特殊健身知识提高教 导的有效性,受过健康教练培训的 认证厨师或许可将烹饪知识与教练 结合起来,以改善客户的食物选择 和生活方式。
本报告记录了一名 55 岁的单 身独居白人男性医生的病例,该 病例最近被诊断为 2 型糖尿病, 有慢性压力、久坐行为及不良饮 食习惯。患者参加了为期 8 周的 厨师教练计划,由受过健康教练 培训的厨师通过 Skype 提供一对 一的 30 分钟教练课程。在前五节 课时,患者的目标主要是烹饪技 巧;不过,在成功实现这些目标 后,患者更进一步地将目标扩展 到其他生活领域,特别是运动和 劳逸结合。计划结束时,患者改 善了营养和运动习惯,增强了进 一步改善自我护理的信心,并改 善了 HbA1c(从 8.8% 降低至 6.7% ;正常值为 <6.5%)等健康参数。
我们的结论是,厨师教练有可 能帮助糖尿病患者改善其实际烹 饪技巧并通过实际应用改善其饮 食,此外,有可能帮助他们整体 改善自我护理。我们打算进一步 发展厨师教练,并根据其实施结 果评估其应用潜力。
RESUMEN
Se recomienda un tratamiento nutricional como parte de un estilo de vida saludable para las personas con diabetes de tipo 2. No obstante, la mayoría de las personas con diabetes no siguen esta pauta. Cambiar los hábitos de alimentación implica obtener conocimientos y desarrollar habilidades prácticas, como ir de compras, preparar comidas y almacenar los alimentos. De la misma forma que los entrenadores personales usan sus conocimientos específicos del mantenimiento físico, para mejorar la efectividad de los entrenamientos, los acreditados chefs, que se han formado como entrenadores de la salud, podrían combinar su experiencia culinaria con el entrenamiento especializado en la salud, para mejorar las elecciones alimentarias y los estilos de vida de sus clientes.
Este informe documenta el caso de un médico de 55 años, blanco, soltero y que vive solo, a quien se le diagnosticó recientemente diabetes de tipo 2 y que presentaba estrés crónico, comportamiento sedentario y hábitos dietéticos insanos. Participó en un programa de entrenamiento con un chef durante 8 sesiones individuales de 30 minutos por semana a través de Skype, impartido por un chef con formación específica en la salud. Durante las primeras cinco reuniones, los objetivos del paciente fueron principalmente culinarios; no obstante, al haber conseguido con éxito estos objetivos, el paciente avanzó y amplió los objetivos e incluyó otros ámbitos respecto al estilo de vida, en concreto, el equilibrio entre el ejercicio y el trabajo. Al final del programa, el paciente había mejorado los hábitos alimenticios y los hábitos de ejercicio, la confianza en sí mismo para seguir mejorando el cuidado personal y los parámetros médicos, como la HbA1c (de 8,8 % a 6,7 %; normal <6,5 %).
La conclusión es que el entrenamiento con chef ayuda potencialmente a las personas con diabetes a la hora de mejorar sus habilidades culinarias y de ponerlas en práctica para comer mejor. Además, tiene potencial para ayudarles a mejorar el cuidado personal en general. Tenemos intención de desarrollar el entrenamiento con chef y valorar su potencial, al mismo tiempo que vamos aprendiendo de su implementación.
INTRODUCTION
Nutrition therapy as part of lifestyle care is a recommended component of the overall treatment plan for people with type 2 diabetes mellitus (T2DM).1 However, most people with diabetes do not follow these guidelines.2 Barriers to adherence include lack of understanding of dietary recommendations, limited budget, food preferences (which are at odds with the recommendations), and underdeveloped cooking skills.3,4
Recent literature suggests that nutritional counseling should move from micro- and macronutrients into food-oriented education.5 Part of the proposed solution is supplementing standard knowledge counseling about healthy nutrition with skills like shopping, meal preparation and food storage.6,7 Educational programs delivered by chefs aimed at improving culinary skills have recently emerged as one way to improve adherence to nutritional guidelines. Some of these programs have been empirically evaluated,8 and one program was reported to improve nutrient pattern intake of people with T2DM.9
Health and wellness coaches are health professionals who help patients change their behavior through strategies such as patient-directed goal-setting, content education, guided self-discovery, and accountability.10 Health and wellness coaching has been applied to help people with diabetes manage their illness and has been shown to increase medication adherence and to improve lifestyle behaviors.11
Fitness coaches are credentialed exercise professionals who use coaching skills to enhance exercise training to improve fitness outcomes. They wear two hats—training and coaching—in order to help clients develop healthy lifestyles.12 Like exercise, cooking is more than just a set of skills; it is a validation of life patterns of active engagement and self-care.13 Moreover, cooking healthful food extends from self-care to the care of others, especially families.
We suggest that credentialed chefs who are also trained as health and wellness coaches might similarly don two hats in order to improve clients' food choices and lifestyles. This case study describes an innovative form of health and wellness coaching—chef coaching (CC)—and demonstrates how it was applied to help a newly diagnosed diabetes patient improve his dietary behavior and clinical outcomes.
PRESENTING CONCERNS
The patient was a 55-year-old white male physician, single and living alone. He reported chronic high stress in both his professional and personal life, eating “on the run” (primarily high-carbohydrate, high-fat food), a low level of physical activity and no drinking or smoking.
In December 2013, during routine examination after years of infrequent medical follow-up, the patient was diagnosed with T2DM. This diagnosis of diabetes frightened him, and he was eager to find education and support for changing his eating and exercise patterns. CC was suggested as a potential support. He was referred in April 2014 to the Institute of Lifestyle Medicine at the Joslin Diabetes Center, Harvard Medical School, Boston, to participate in a pilot CC program with the goal of improving his food consumption.
CLINICAL FINDINGS
The patient reported eating high-fat, high-carbohydrate foods starting in childhood, where healthy eating was “never a focus.” He reported having been a small and slender child and adolescent (5 ft 8 in and 95 lb at age 15) who ran high school track until late adolescence, when he stopped athletic training. During young adulthood, his weight fluctuated from 180 to 230 lb, depending on whether or not he was regularly running for exercise. After age 30, with no regular exercise program, his weight increased and was maintained at 270 lb, with the exception of 3 years during which he was on the South Beach Diet, when he reduced his weight to 225 lb.
He also reported a lifelong struggle with stress, beginning with a physically abusive home environment and continued high anxiety since leaving home at age 18. During the past 10 years, he has made determined efforts to manage stress more effectively, primarily through reducing his obligations and improving his assertiveness skills.
The patient's past medical history was remarkable for gastroesophageal reflux disease treated with omeprazole (40 mg, 1/day), cervical disk herniation and carpal tunnel syndrome treated with cyclobenzaprine (10 mg, 1/day) and celecoxib (400 mg, 2/day), hypertriglyceridemia treated with fish oil (1000 mg, 1/day), and posttraumatic stress disorder. His family history was positive for T1DM (maternal grandmother). His diabetic medication included metformin (1000 mg, 2/day), and insulin glargine 40 unit/day.
On examination, the patient was obese (weight: 255 lb; height: 76 in; body mass index [BMI]: 31) with normal blood pressure (130/74) and no evidence of diabetes end organ complication. His laboratory results were remarkable for elevated triglycerides, low-density lipoprotein (LDL) cholesterol, and hemoglobin A1c (HgA1c), and low high-density lipoprotein (HDL) cholesterol; liver enzymes were normal. Clinical and laboratory data before and after participating in the CC program are summarized in Table 1.
Table 1.
Subjective Laboratory and Anthropometric Measurements, Diabetes Medication, and Narratives Before and After Chef Coaching
| Before Chef Coaching Programa | After Chef Coaching Programb | |
|---|---|---|
| Objectives | ||
| Weight, lb | 255 | 259 |
| BMI | 31 | 31.5 |
| Blood pressure | 130/74 | 130/75 |
| HgA1c | 8.8% | 6.7% |
| Total cholesterol | 199 | 158 |
| HDL cholesterol | 28 | 25 |
| LDL cholesterol | 108 | 100 |
| Triglycerides | 563 | 320 |
| ALT | 36 | 43 |
| AST | 22 | 21 |
| Diabetic medicationb | Metformin 1000 mg, 2/day Insulin glargine 40 unit/day | Metformin 1000 mg, 2/day Liraglutide 1.2 mg, 1/day |
| Narrativec | ||
| Chef coach's “coaching hat” | “I did some nutritional changes such as changing sodas to diet sodas … but I don't feel I changed much … I have a very low confidence level to have the ability to prepare my own meal.” | “I understand it is just the starting point of the process. I have confidence that I can continue myself. I need more information, which I plan to get … I feel happier about my success.” |
| Chef coach's “training hat” | “I am eating two lunches a day in my office … the first is prepared ravioli and the second is a 1/2 Subway club … I am keeping the other half for dinner” | “I bought a wide variety of vegetables for the whole week. Now I understand how to store [them] in order to keep them fresh so I will bring some to my office …. I bought a multigrain bread and I froze it. I did not know it is possible to freeze bread. Now I have a healthy bread every day without the need to buy it.” |
Laboratory and anthropometric measurements were collected 1 month prior to the first coaching session (03.11.14); narrative statements were taken during the first session.
Laboratory and anthropometric measurements were collected 3 days after the last coaching session (06.26.14); narrative statements were taken during the last two sessions.
Medications were taken for 3 months prior to “before CC program” and “after CC program.”
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; HDL, high-density lipoprotein; HgA1c, hemoglobin A1c; LDL, low-density lipoprotein.
Assessment
Before beginning CC, the patient completed an online lifestyle questionnaire (LQ) developed by Wellcoaches14 (Wellesley, Massachusetts) and a food preparation behavior questionnaire (FPBQ) developed and pre-piloted by the manuscript authors. On these, the patient reported consuming mostly processed food and food from fast-food restaurants, including mostly refined grain, one or no servings of fruit and vegetables per day, and predominantly high-fat food. He did not exercise at all. As discussed below and presented in Table 2, he also rated the importance of change in various health behaviors and rated his confidence in accomplishing those changes.
Table 2.
Patient's Self-assessment Prior to Chef Coaching
| Importancea | Confidenceb | Readiness for a changec | |
|---|---|---|---|
| Lifestyle questionnaire | |||
| Life satisfaction | 4 | 4 | Plan to change this month |
| Energy | 8 | 7 | Plan to change this month |
| Mental and emotional fitness | 10 | 5 | Plan to change this month |
| Exercise | 5 | 4 | Plan to change this month |
| Nutrition | 9 | 6 | Plan to change this month |
| Weight | 9 | 6 | Plan to change this month |
| Health | 9 | 6 | Plan to change this month |
| Food Preparation Behavior Questionnaire | |||
| Healthy meal preparation | 4 | 2 | Plan to change this month |
Importance of having a high level of … (1, not important at all; 10, most important in my life now).
Confidence level in ability to reach and sustain a high level of … (1, lowest confidence; 10, highest confidence).
Readiness to make changes or improvements in … (no present interest in making a change; plan a change in the next 6 mo; plan to change this month; recently started working on this; already doing this consistently (6 mo+).
Some of the patient's narratives describing his approach to eating before the CC program are presented in Table 1.
COACHING INTERVENTION
Overview
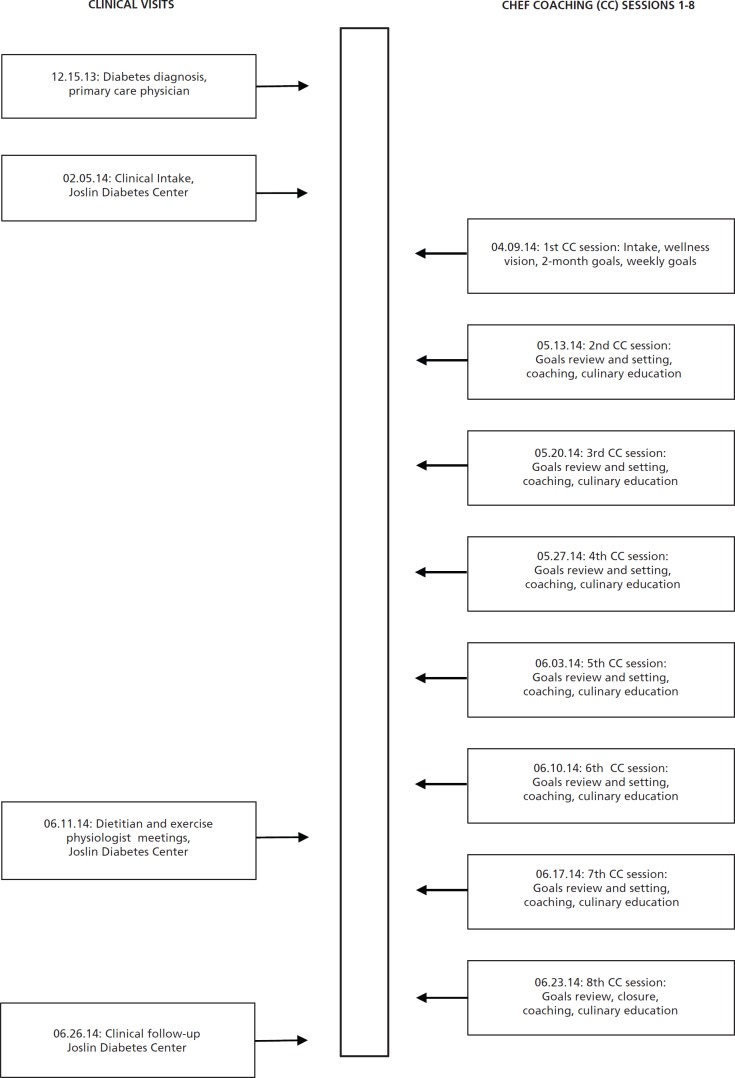
The patient participated in a CC program comprised of 8 weekly one-on-one 30-minute coaching sessions via Skype (Figure 1). During the first session, the patient identified his Wellness Vision14 and goals for the course of his participation in the CC program (see below). During each subsequent meeting, the patient reviewed his progress toward the prior week's goals and identified his goals for the coming week, using the Wellcoaches Structured Coaching Checklist.14 Coaching relied on reinforcing behaviors that the patient reported as helping him work toward achieving his goals and problem-solving when goals were not achieved, with the coach facilitating a self-discovery process.12 Practical culinary skills such as meal planning, food purchasing and storage, and healthy food preparation techniques were taught when requested. Any other requested advice, including nutritional information, was referred to active learning. No “hands on” or other cooking demonstrations were involved. A detailed description of the CC program principles10 is presented in Table 3.
Figure 1.
Timeline.
Table 3.
Determining Principles10 of the Chef Coaching Program
| Approaches, Practices, Strategies, and Methodologies | |
| Patient centeredness | Coaching is tailored to the individual's specific needs, concerns, circumstances, and readiness to change. |
| Patient-determined goals | Goals for the course of coaching: Patient is encouraged to set his own goals in the area of food preparation, then encouraged to set additional goals in other wellness areas. |
| Weekly goals: Goals in the area of food preparation and other wellness areas that build toward the longer term or more complex goals for the course of coaching. | |
| Use of self-discovery process | When patient asks for culinary advice, he is asked if he would like an answer or to do active learning. |
| Accountability | Progress toward both weekly goals and long-terms goals are discussed weekly with the patient. |
| Content education | Expert education regarding culinary skills is provided as requested after receiving permission from the patient. |
| Coaching “dose” | 8 sessions |
| Consistent coaching relationship | Ongoing relationship with the same coach |
| Background of coach | |
| Profession | Chef coach |
| Background profession | Cuisine de Base degree via Le Cordon Bleu Paris School in Sidney, Australia 8 y of experience in healthy cooking education |
| Training received by the coach | 3 mo of basic coach training via Wellcoaches Corp, Wellesley, Massachusetts (36 h) Behavioral change skills: This coach training uses a client-centered approach that, among other strategies, emphasizes relationship building, motivational interviewing, development of self-efficacy, and goal setting/achievement14 |
| Health information briefing: Medical background | |
| Job training: Weekly meeting with a mentor coach | |
Coaching Course
During the first session, using appreciative inquiry techniques,12 the coach encouraged the patient to acknowledge the gap between his decision to participate in CC and both his perceived confidence in preparing healthy food (2/10) and the importance he attributed to healthy food preparation (4/10) (Table 2). He was then guided to define a compelling Wellness Vision,12 ie, to “improve intake of healthy food through increasing time spent cooking,” and concrete realistic goals to guide his work over the course of chef coaching, such as “improving my snacking habits in the office to include just healthy snacks every day” (Table 2).
During the following four meetings, the patient's goals were primarily culinary, with a 20% to 100% completion rate, eg, “buying lean meat on Saturday and cooking it using a recipe I plan to find on the internet”; “buying healthy choices such as hummus and carrots on Saturday and bringing them to my office to be used as snacks”; “choosing a healthy cheese on Saturday while shopping.” From the sixth meeting forward, the patient included goals from other lifestyle domains, specifically exercise and work-life balance.
Coach's Reflection With a Mentor Coach
Throughout the CC program, the coach (RP) met with a mentor coach (DD) weekly who was a “silent listener” to the CC session and subsequently guided the coach in a session debriefing. Debriefing focused on two key issues we confronted in developing this new model of coaching. First, the mentor coach reinforced the coach's fidelity to the CC program standards of coaching described above. Second, the mentor coach helped the coach resolve when and how to proceed when “switching hats” from the coach/facilitator role in which the patient's expertise is elicited and the chef/expert role, in which the chef provides technical instruction.
OUTCOMES
During the final CC session, the patient reported having improved his nutritional habits in terms of buying healthful food and making healthy choices available, with the result that he ate healthful food for lunch and dinner more frequently. “I drove to Whole Foods and bought carrots and celery and hummus, tomatoes, broccoli, and cheese sauce. I brought it to the office, and ate it instead of the terrible food I usually eat. I feel better—no sugar rush and crash.” (See Table 1 for additional narratives.)
In addition to having improved his nutritional habits, he increased his exercise substantially—walking 1 mile at least two times per week “I walked 4 loops (1 mile) … I walked slowly, but it was easy so I picked it up … I felt very good to do it … I plan to do this twice a week, once [on] the weekend and once during the week after work.”
His confidence that he could change his lifestyle behaviors increased (see narrative in table 1). As a result of success in goal attainment, the patient felt inspired to continue better self-care: “This process was a good jump start … I got pointed in the right direction and got momentum. Now I want to do it for myself.”
Tests conducted during the week following the last CC session showed remarkable improvement in the patient's HgA1c and triglycerides, as shown in Table 1. There was no change in weight, BMI, LDL and HDL cholesterol, or blood pressure. The patient attributed the change in HgA1c to a combination of medication and change in his eating and exercise habits. He credited the reinforcing nature of the CC for his success in changing his lifestyle behaviors: “[It was] a nice pace and support. The gentle approach helped me give myself credit for the good things I do, and not for the bad things.”
From the point of view of the mentor coach, the coaching style was key to the patient's success in making changes: “The coach, while drawing on his expertise as a chef, nevertheless consistently encouraged the patient's self-direction via goal-setting, reflection, and exploration. The patient was strongly motivated by his accountability to his coach and by anticipating his pleasure in the changes he would be able to make.”
The patient, himself a clinician, also reported that his CC experience led him to talk more empathically to his own patients and to use “change talk”12 more often with them: “I got nicer in 8 weeks. I talk more about changing behaviors and what's holding [my patients] back. My coach did a lot of that talk to me and I find myself using it now.”
DISCUSSION
This case report introduces CC as a potential strategy for helping people with diabetes apply the nutrition education they receive so that they make healthier nutritional choices. We demonstrated that it is possible to help a patient improve his eating behavior and his confidence to improve his lifestyle over 8 30-minute weekly coaching sessions conducted by Skype with a health and wellness coach who is also a professional chef. These results align with those of other studies, which show that health and wellness coaching can improve participants' lifestyle behaviors, confidence, and motivation,11,15 and they also align with additional studies that show that cooking interventions can improve participants' time spent cooking, cooking confidence, and the nutritional quality of their diets.8
Although definitive support of a relationship between teaching culinary skills and long-term cooking behavior or health outcome is lacking, cooking initiatives have been promoted recently. Many programs that promote cooking as a necessary and appropriate response to unhealthy nutrition exist on the national, state, and community levels.8 However, the feasibility of “hands on” cooking programs in a large-scale community setting has been questioned.16 We have shown that our approach—chef coaching via phone or Skype without hands-on demonstration—has the potential to be a viable response to the need for effective and feasible programming.
Although the patient's preliminary confidence about healthy food preparation was low, he chose CC as his path. As has been seen in other coaching programs,15 his success with accomplishing goals further empowered him and was translated to interest in pursuing future goals in healthy food preparation as well as in other health behaviors. This supports the idea, also shown with fitness coaching, that focus on changing one lifestyle behavior can generalize to changes in other lifestyle behaviors.12
This particular patient enjoyed a positive change in HgA1c and triglycerides levels over the course of his coaching experience. He attributed the change to effective medication and to changes in lifestyle supported by CC. The patient's weight did not change significantly, and his evaluation did not include body composition to further discern if he had any reduction in his fat mass. Until the patient demonstrates a further decrease in cardiometabolic risk factors, additional medication targeting his dyslipidemia might be considered.
One of the patient's first goals was to schedule appointments for counseling with a dietitian and an exercise physiologist. This happened after the sixth coaching session (Figure 1). Although lack of nutritional knowledge was not a barrier in this case, a preliminary nutritional education might be consider as a prerequisite for CC. Coaching as one component of the diabetes care team was proven feasible in a primary care setting.17 As we move forward to develop the CC program, we will work to integrate CC with nutritional education and to structure it within the diabetic care team.
The potential for CC to help other patients accomplish change in health outcomes requires further testing. It is our intention to further develop the various aspects of CC as we continue to learn from its implementation. Next steps will include formal assessment of CC—ie, a randomized controlled trial comparing CC to treatment as usual (education without coaching to assist implementation) and estimates of effect size. We will also explore whether we can train certified chefs who are not health professionals to serve as CC program coaches.
INFORMED CONSENT
This case report was approved for publication by the Joslin Diabetes Center Committee on Human Studies. The patient contributed to the case report, read it in full, and gave written permission for its publication.
Disclosures The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest, and Dr Polak disclosed receipt of grants from Maccabi Health Service, Harvard Medical School, the Israeli Cancer Association, and Wellcoaches Corp. The other authors had no relevant conflicts to disclose.
Contributor Information
Rani Polak, Institute of Lifestyle Medicine, Department of Physical Medicine & Rehabilitation, Harvard Medical School, Joslin Diabetes Center, Boston, Massachusetts (Dr Polak), United States.
Diana Dill, Working Together for Health, Belmont, Massachusetts (Ms Dill), United States.
Martin J. Abrahamson, Center For Integrative Health and Wellness, Joslin Diabetes Center (Dr Abrahamson), United States.
Rachele M. Pojednic, Institute of Lifestyle Medicine, Department of Physical Medicine & Rehabilitation, Harvard Medical School, Joslin Diabetes Center, Boston, Massachusetts (Dr Pojednic), United States.
Edward M. Phillips, Institute of Lifestyle Medicine, Department of Physical Medicine & Rehabilitation, Harvard Medical School, Joslin Diabetes Center, Boston, Massachusetts (Dr Phillips), United States.
REFERENCES
- 1.American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care. 2014; 37Suppl 1: S14–80. [DOI] [PubMed] [Google Scholar]
- 2.Oza-Frank R, Cheng YJ, Narayan KM, Gregg EW. Trends in nutrient intake among adults with diabetes in the United States: 1988-2004. J Am Diet Assoc. 2009;109(7):1173–8. [DOI] [PubMed] [Google Scholar]
- 3.Albarran NB, Ballesteros MN, Morales GG, Ortega MI. Dietary behavior and type 2 diabetes care. Patient Educ Couns. 2006;61(2):191–9. [DOI] [PubMed] [Google Scholar]
- 4.Nagelkerk J, Reick K, Meengs L. Perceived barriers and effective strategies to diabetes self-management. J Adv Nurs. 2006;54(2):151–8. [DOI] [PubMed] [Google Scholar]
- 5.Lichtenstein AH, Ludwig DS. Bring back home economics education. JAMA. 2010;303(18):1857–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hartmann C, Dohle S, Siegrist M. Importance of cooking skills for balanced food choices. Appetite. 2013 Jun;65:125–31. [DOI] [PubMed] [Google Scholar]
- 7.Soliah LA, Walter JM, Jones SA. Benefits and barriers to healthful eating: what are the consequences of decreased food preparation ability? Am J Lifestyle Med. 2012;6(2):152–8. [Google Scholar]
- 8.Reicks M, Trofholz AC, Stang JS, Laska MN. Impact of cooking and home food preparation interventions among adults: outcomes and implications for future programs. J Nutr Educ Behav. 2014;46(4):259–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Archuleta M, Vanleeuwen D, Halderson K, et al. Cooking schools improve nutrient intake patterns of people with type 2 diabetes. J Nutr Educ Behav. 2012;44(4):319–25. [DOI] [PubMed] [Google Scholar]
- 10.Wolever RQ, Simmons LA, Sforzo GA, et al. A systematic review of the literature on health and wellness coaching: defining a key behavioral intervention in healthcare. Glob Adv Health Med 2013;2(4):38–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolever RQ, Dreusicke M, Fikkan J, et al. Integrative health coaching for patients with type 2 diabetes: a randomized clinical trial. Diabetes Educ. 2010;36(4):629–39. [DOI] [PubMed] [Google Scholar]
- 12.Moore M, Tschannen-Moran B. Coaching psychology manual. Philadelphia, PA: Williams and Wilkins; 2010. [Google Scholar]
- 13.Erlich R, Yngve A, Wahlqvist ML. Cooking as a healthy behaviour. Public Health Nutr. 2012;15(7):1139–40. [DOI] [PubMed] [Google Scholar]
- 14.well-coaches. https://wellcoaches.customerhub.net/my-account AccessedAugust1, 2014.
- 15.Frates EP, Moore MA, Lopez CN, McMahon GT. Coaching for behavior change in physiatry. Am J Phys Med Rehabil. 2011;90(12):1074–82. [DOI] [PubMed] [Google Scholar]
- 16.Polak R, Constantini WN, Verbov G, et al. Public health nurses promote healthy lifestyles (PHeeL-PHiNe): methodology and feasibility. J Ambul Care Manage. In press. [DOI] [PubMed] [Google Scholar]
- 17.Liddy C, Johnston S, Nash K, Ward N, Irving H. Health coaching in primary care: a feasibility model for diabetes care. BMC Fam Pract. 2014April3;15:60. [DOI] [PMC free article] [PubMed] [Google Scholar]