Abstract
The present study examined whether pretreatment mindfulness exerts an indirect effect on outcomes following cognitive-behavioral therapy (CBT). Cognitive processes of probability and cost bias (i.e., overestimations of the likelihood that negative social events will occur, and that these events will have negative consequences when they do occur) were explored as potential mediators of the relation between mindfulness and social anxiety symptom change. People with higher levels of mindfulness may be better able to benefit from treatments that reduce biases because mindfulness may aid in regulation of attention. Sixty-seven individuals with a primary diagnosis of social phobia identifying public speaking as their greatest fear received eight sessions of one of two types of exposure-based CBT delivered according to treatment manuals. Participants completed self-report measures of mindfulness, probability bias, cost bias, and social anxiety symptoms. Mediation hypotheses were assessed by a bootstrapped regression using treatment outcome data. Pretreatment mindfulness was not related to change in social anxiety symptoms from pre- to posttreatment. However, mindfulness had an indirect effect on treatment outcome via its association with probability bias, but not cost bias, at midtreatment. These findings were consistent across three metrics of social anxiety symptoms. Mindfulness may play a role in response to CBT among individuals with social phobia through its relation with probability bias – even when the treatment does not target mindfulness.
Keywords: mindfulness, mediation, cognitive biases, social phobia, cognitive-behavioral therapy
Introduction
Mindfulness is a concept originating in ancient Hindu and Buddhist philosophies (Kang & Whittingham, 2010) that has been empirically studied in recent years. Although current definitions of mindfulness vary, all identify mindfulness as a process of sustained attention and awareness of the present moment in daily life (e.g., Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006; Brown & Ryan, 2003). Thus, the present study defines mindfulness as sustained attention toward present-moment experience. Mindfulness has been linked to a number of positive psychosocial outcomes, such as higher self-esteem and lower neuroticism (Brown & Ryan, 2003). Mindfulness-based interventions show promise in the treatment of a number of psychological difficulties (e.g., Kabat-Zinn et al., 1992; Miller, Fletcher, & Kabat-Zinn, 1995; Safer, Telch, & Agras, 2001; Telch, Agras, & Linehan, 2001), including social phobia. In particular, treatments which combine cognitive-behavioral therapy (CBT) with mindfulness, as well as mindfulness meditation training alone, show preliminary efficacy in the reduction of social anxiety symptoms, with authors reporting large effect sizes in recent open trials and controlled trials (i.e., Cohen’s d > 1.00) (Dalrymple & Herbert, 2007; Goldin & Gross, 2010; Goldin, Ramel, & Gross, 2009; Kocovski, Fleming, & Rector, 2009). The manner in which mindfulness may have a positive impact on exposure therapy for anxiety disorders has been described (Treanor, 2011); a recent study, however, found that mindfulness did not moderate response to traditional CBT (Burton, Schmertz, Price, Masuda, & Anderson, 2013). The current study examines whether or not mindfulness has an indirect influence on treatment response to traditional CBT via its relation to cognitive processes – specifically cognitive biases.
Two types of cognitive biases figure prominently in social phobia: probability bias and cost bias. Probability bias is defined as an individual’s tendency to exaggerate the likelihood of negative social events, and cost bias occurs when individuals exaggerate the potential consequences of negative social events. Research consistently shows that people with social phobia report greater probability and cost biases than healthy controls (Foa, Franklin, Perry, & Herbert, 1996; Foa, Huppert, & Cahill, 2006; McManus, Clark, & Hackmann, 2000). These biases have been proposed as a target of CBT for social anxiety disorder (SAD) for decades (Foa & Kozak, 1986). Numerous studies show that successful treatment for SAD is associated with reductions in probability and cost estimates (Franklin, Huppert, Langner, Leiberg, & Foa, 2005; Lucock & Salkovskis, 1988; Poulton & Andrews, 1996) and that reductions in such biases mediate treatment outcome (e.g., Smits, Rosenfield, McDonald, & Telch, 2006).
Attentional allocation, a central feature of mindfulness, has been identified in theoretical models of social phobia as central for developing cognitive biases. For example, Clark and Wells (1995) argue that self-focused attention prevents individuals with social phobia from processing external cues about social situations, which can lead to judgmental biases because individuals use information from self-focused attention (e.g., my heart is racing) rather than potentially positive external cues (e.g., most people are smiling) to evaluate social performance. Heinrichs and Hofmann (2001) also suggest that biased attentional allocation leads to cognitive biases. Research shows that individuals with social phobia direct more attention to the self than to environmental cues (Jostes, Pook, & Florin, 1999), and self-focused attention is associated with more negative thinking (Hope & Heimberg, 1988). Thus, biased attentional allocation appears to be linked to problematic cognitions within social phobia.
Mindfulness, by definition, consists of attentional allocation to the present moment rather than to cognitions about the self, the past, and the future (e.g., Kabat-Zinn, 1994, p. 4; Marlatt & Kristeller, 1999, p. 68). The impact of mindfulness on attentional processes has been well researched. Mindfulness is negatively related to self-focused attention in healthy populations (Beitel, Ferrer, & Cecero, 2005; Brown & Ryan, 2003). In addition, mindfulness-based interventions appear to reduce activity in brain regions associated with narrative self-reference (Farb et al., 2007), increase brain activity in areas associated with attention regulation, and decrease activity in brain regions associated with narrative self-view (i.e., cognitions about the self rather than the present moment) (Goldin et al., 2009). Mindfulness may have an indirect effect on CBT for SAD via its impact on cognitive biases through attentional processes.
People with higher levels of mindfulness may be better able to benefit from interventions designed to reduce self-focused attention and biased cognitive appraisals. Indeed, one study found that probability and cost biases partially mediated the relation between mindfulness and social anxiety among individuals with social phobia using a cross-sectional design (Schmertz, Masuda, & Anderson, 2012). That is, the relation between mindfulness and social anxiety was explained through relations to cognitive biases. However, this hypothesis has not yet been tested longitudinally in a clinical sample receiving treatment.
The current study uses a longitudinal design to examine the relation between mindfulness, cognitive biases, and change in social phobia symptoms following CBT. The present study is a secondary data analysis from a randomized clinical trial comparing two types of CBT, virtual reality exposure therapy and cognitive-behavioral group therapy, neither of which target mindfulness, but both of which target self-focused attention and probability and cost biases. We predict that pretreatment mindfulness will be positively related to reductions in social anxiety symptoms following treatment via its relation to probability bias and cost biases.
Method
Participants
The initial sample consisted of 88 participants who completed the procedures of this study as part of a randomized controlled trial comparing two types of CBT (Anderson et al., 2013). Professionals referred participants, and participants self-referred in response to advertising. Participants were included if they were literate in English and had a primary diagnosis of social phobia with a predominant fear of public speaking as determined by the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID-IV; First, Spitzer, Gibbon, &Williams, 2002). Participants were excluded if they had a history of seizure disorder, mania, schizophrenia, or other psychoses, as well as prominent suicidal ideation, or current alcohol or drug abuse or dependence. Past experience with meditation or mindfulness was not necessary to participate in this study. All participants who met inclusion criteria, completed the pre-, mid-, and posttreatment assessments, and had valid data for all study-relevant measures (N = 67) were included in the current study; 21 participants were excluded from our analyses because they dropped out of treatment during the initial phase. No significant differences between dropouts and nondropouts were found in age (t (86) = 1.83, p = ns) or gender (χ2 (2, N = 88) = 0.59, p = ns), nor were differences found at baseline on any of the measures used in the present analysis (Personal Report of Communication Apprehension (PRCA): t (86) = 0.73, p = ns; Personal Report of Confidence as a Speaker (PRCS): t (86) = −1.26, p = ns; Brief Fear of Negative Evaluation (BFNE): t (86) = −1.07, p = ns; Mindful Attention Awareness Scale (MAAS): t (86) = −0.10, p = ns; Outcome Cost Questionnaire (OCQ): t (86) = −1.59, p = ns; Outcome Probability Questionnaire (OPQ): t (86) = −1.82, p = ns).
The sample had more women (60%) than men, with a mean age of 39.09 (SD = 11.27; range = 19–69). Most participants self-identified as either Caucasian (47%) or African-American (36%); among the rest of the sample, four self-identified as Hispanic, two as Asian American, two as Asian, one as African, one as Ethiopian, and two as biracial. Most of the sample was college educated; sixty-six percent of the sample reported completing college. Forty-five percent of the sample met criteria for the generalized subtype of social phobia. The majority of the participants did not have a comorbid diagnosis (N = 59, 88%).
Measures
The Brief Fear of Negative Evaluation – Brief Form
The BFNE is a 12-item self-report measure that assesses fear of negative judgment by others. Items are on a 5-point scale, and scores range from 12 to 60. Higher scores indicate increased evaluative concerns. In two studies of social anxiety with clinical samples, the BFNE showed excellent psychometric properties, including test–retest reliability (r = .94), internal consistency (α = .89–.97), convergent validity, and discriminant validity (Collins, Westra, Dozois, & Stewert, 2005; Weeks et al., 2005). Internal consistency for the BFNE was also good in the present sample (α = .80 at both pretreatment and posttreatment) (Leary, 1983).
Personal Report of Communication Apprehension
The PRCA is a self-report measure of apprehension about public speaking. Each of its 10 items are scored on a 5-point Likert scale ranging from 1 (Strongly Agree) to 5 (Strongly Disagree). Scores range from 0 to 46, with higher scores indicating higher publicspeaking anxiety. The scoring algorithm utilized to compute the PRCA total score prevents valid measurement of its internal consistency; however, 5-week test–retest reliability was good (r = .74) (McCroskey, 1978).
Personal Report of Confidence as a Speaker
The PRCS is a 30-item self-report measure of behaviors and cognitions related to public speaking. Each item is rated as true or false, and a scoring algorithm computes a total score of public speaking confidence based on these responses. Scores range from 0 to 30; higher scores indicate lower confidence in public-speaking situations. For the present sample, PRCS internal consistency scores were questionable at pretreatment (α = .69), good for midtreatment (α = .83), and good for posttreatment (α = .82) (Paul, 1966).
Mindful Attention Awareness Scale Brown & Ryan, 2003
The MAAS is a 15-item self-report measure assessing the degree to which individuals are mindful (i.e., attentive and aware) in everyday life (Brown & Ryan, 2003). The MAAS assesses aspects of mindfulness specifically related to attention and awareness of the present moment; this measure does not measure aspects of mindfulness outside of attention to the present, such as nonjudgment and non-reactivity toward present-moment experience. Participants indicate the extent to which they function without awareness in their daily activities (e.g., “I rush through activities without being really attentive to them” and “I drive places on automatic pilot and then wonder why I went there”). Participants report how often they have the experiences of each item using a 6-point Likert-type scale, from 1 (almost always) to 6 (almost never) and total scores range from 1 to 6 (average item score), with higher scores indicating greater mindfulness. The MAAS has shown good temporal stability over a period of 4 weeks (ICC = 0.81) and high internal consistency (α = .82; Brown & Ryan, 2003). The MAAS also showed excellent internal consistency in the present sample (α = .90 at both pretreatment and posttreatment). In addition, the MAAS has shown convergence with the personality factor of openness to experience (on the NEO-PI), the mental engagement subscale of the Mindfulness-Mindlessness Scale, and emotional intelligence; discriminant validity has been shown through non-associations with measures of self-consciousness, self-monitoring, and cognitive flexibility (Brown & Ryan, 2003). Items on the MAAS have also correlated with other facets of mindfulness, such as nonjudgment and nonreactivity (Baer et al., 2006).
The Outcome Probability Questionnaire and Outcome Cost Questionnaire
The OPQ and OCQ consist of 12 items measuring cognitive biases related to the feared outcomes of social situations. They were developed from a set of items used by Butler and Mathews (1983) and Foa et al. (1996). For the OPQ, participants rate how likely it is that a given outcome would occur in a public-speaking situation, and for the OCQ, participants rate how distressing the outcome would be if it happened. Participants rate the items on a 9-point Likert scale (0 = not at all likely/distressing, 8 = extremely likely/distressing), with summary scores ranging from 0 to 96. For the current study, internal consistency was excellent (OPQ; α = .92–.94; OCQ; α = .89–.90). The OPQ and OCQ have been shown to have good convergent validity and individuals with social anxiety score higher on the OPQ and OCQ than non-anxious controls (Uren, Szabo, & Lovibond, 2004).
Procedure
The study was completed at a clinic in the southeastern United States. Investigators determined potential participants’ eligibility for the study with a brief telephone screening and an in-person diagnostic interview. Four doctoral candidates in clinical psychology conducted all assessment procedures. For training in administration of the diagnostic interview, doctoral students watched training tapes and practiced interviews. A licensed clinical psychologist reviewed all training videotapes and supervised student assessors weekly.
During the initial phone screen, potential participants were asked questions to rule out obvious exclusion criteria (e.g., prior seizures). The people who were eligible and interested in participating were scheduled for a face-to-face interview. After receiving informed consent from participants, the anxiety, mood, and substance abuse modules of the SCID were administered to establish a diagnosis of social phobia that included a fear of public speaking and to rule out current substance dependence. Blind reviewers reexamined videotaped SCID administrations for 12 randomly selected participants; interrater reliability revealed 100% agreement amongst reviewers. Participants also completed a self-report battery that included the previously described measures. Data utilized for the current study were collected at three different occasions: pre-, mid-, and posttreatment.
Both treatments were administered according to a treatment manual (Anderson, Zimand, Hodges, & Rothbaum, 2005; Hofmann, 2004) by five study therapists: two senior therapists were licensed psychologists with prior experience implementing manualized CBT, and three junior therapists were doctoral students supervised by the last author. All therapists administered both treatments, each of which included eight sessions of CBT designed to target several processes shown to maintain social anxiety, including self-focused attention, negative perceptions of self and others, perceptions of lack of emotional control, and realistic goal-setting for social situations. The primary difference between the two therapies was the modality of exposure, delivered either in a group setting, using other group members for exposure (N = 34), or, individually, using virtual reality for exposure (N = 33). Ratings of adherence and competence were provided by experts in both treatments (Dr Stefan Hofmann for EGT, and Dr Barbara Rothbaum for VRE) for a randomly selected subset of videotaped sessions (14%). Adherence was quite good, with over 90% of the essential elements of the protocol being completed for both treatments, and one infraction for each treatment group across all sessions reviewed. The skill with which therapists delivered treatments was rated using a 7-point scale (1 – very poor to 7 – excellent), with a mean quality rating of 6.1 for VRE and 5.4 for EGT, which were not significantly different from one another (p = .90).
Data analytic plan
The mediation hypotheses were assessed within a framework consistent with that of Cole and Maxwell (2003). Mediation posits that the association between an independent variable (X) and a dependent variable (Y) is better explained through an indirect effect via a mediating variable (M). That is, the relation between X and Y (C-path) is better explained by the relation of X to M (A-path) and M to Y (B-path). For the present study, pre- to posttreatment change measures of social anxiety including the BFNE, PRCA, and PRCS were identified as the Y variables, the pretreatment MAAS was identified as the X variable, and pretreatment to midtreatment measures of OCQ and OPQ were identified as Ms. Mediation was assessed with a panel model that included pretreatment MAAS scores (X), midtreatment OPQ and OCQ scores (M) after controlling for pretreatment OPQ and OCQ scores, respectively, and posttreatment BFNE, PRCA, and PRCS scores (Y) controlling for pretreatment scores, respectively. The indirect effect was estimated through bootstrapping methods based on 1000 samples to obtain the 95% bias-corrected confidence intervals (Mackinnon, Lockwood, Hoffman, West, & Sheets, 2002; MacKinnon, Lockwood, & Williams, 2004). Prior work on mediation has suggested that a significant C-path is not necessary to meet criteria for mediation; rather, the significance of the indirect path is of most importance (Mackinnon et al., 2002). Such an approach has been used to assess longitudinal mediation in prior work (McLaughlin & Nolen-Hoeksema, 2011). Analyses were performed using Mplus 6.11 (Muthén & Muthén, 2004). Model fit for the mediation was evaluated by an RMSEA < 0.06, a CFI > 0.95, and a nonsignificant chi-square test (Hu & Bentler, 1999).
Results
Primary results from this outcome trial are reported elsewhere (Anderson et al., 2013) and suggested that there were no differences on treatment response across the two treatment conditions for the dependent variables used in the current study. Additional analyses of variance suggested that there were no differences in mindfulness (F(1, 65) = 0.29, p = .59), pretreatment outcome cost (F(1, 65) = 0.1.46, p = .23), midtreatment outcome cost (F(1, 65) = 0.02, p = .88), pretreatment outcome probability (F(1, 65) = 0.43, p = .52), and posttreatment outcome probability (F(1, 65) = 0.14, p = .71) across the treatment conditions. Thus, the treatment groups were collapsed for the present analysis. Descriptive statistics for the measures are presented in Table 1. Data were inspected for normalcy, excessive missing cases, and outliers, defined as scores greater or less than three standard deviations from the mean (Field, 2005). A BFNE score of 11 that fell 3.17 standard deviations below the mean was removed from the relevant analyses. Relations among variables are presented in Table 2.
Table 1.
Descriptive statistics.
| Measure | Mean | SD | Min | Max |
|---|---|---|---|---|
| MAAS pretreatment | 60.68 | 15.69 | 21.00 | 89.00 |
| OPQ pretreatment | 52.42 | 18.77 | 9.00 | 89.00 |
| OPQ midtreatment | 37.83 | 19.85 | 5.00 | 77.00 |
| OCQ pretreatment | 64.94 | 15.92 | 9.00 | 90.00 |
| OCQ midtreatment | 52.46 | 20.65 | 3.00 | 86.00 |
| BFNE pretreatment | 42.66 | 9.25 | 21.00 | 60.00 |
| BFNE posttreatment | 41.01 | 9.30 | 23.00 | 56.00 |
| PRCS pretreatment | 25.36 | 2.76 | 19.00 | 30.00 |
| PRCS posttreatment | 13.36 | 7.40 | 3.00 | 29.00 |
| PRCA pretreatment | 38.76 | 6.22 | 26.00 | 50.00 |
| PRCA posttreatment | 28.62 | 7.07 | 15.00 | 45.00 |
Note: MAAS = Mindful Attention Awareness Scale; OPQ = Outcome Probability Questionnaire; OCQ = Outcome Cost Questionnaire; BFNE = Brief Fear of Negative Evaluation; PRCS = Personal Report of Confidence as a Speaker; PRCA = Personal Report of Communication Apprehension.
Table 2.
Correlation matrix of all variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 – MAAS pretreatment | 1.00 | ||||||||||
| 2 – OPQ pretreatment | −0.46** | 1.00 | |||||||||
| 3 – OPQ midtreatment | −0.48** | 0.64** | 1.00 | ||||||||
| 4 – OCQ pretreatment | −0.31* | 0.57* | 0.21 | 1.00 | |||||||
| 5 – OCQ midtreatment | −0.22 | 0.46** | 0.63** | 0.37** | 1.00 | ||||||
| 6 – BFNE pretreatment | −0.032** | 0.044** | 0.42** | 0.47** | 0.40** | 1.00 | |||||
| 7 – BFNE posttreatment | −0.30* | 0.42** | 0.64** | 0.28* | 0.49** | 0.51** | 1.00 | ||||
| 8 – PRCS pretreatment | 0.00 | 0.16 | 0.13 | 0.30* | 0.15 | 0.23 | 0.06 | 1.00 | |||
| 9 – PRCS posttreatment | 0.02 | 0.12 | 0.43** | 0.19 | 0.49** | 0.10 | 0.58** | 0.03 | 1.00 | ||
| 10 – PRCA pretreatment | −0.01 | 0.13 | 0.11 | 0.27* | 0.15 | 0.31* | 0.17 | 0.44** | 0.11 | 1.00 | |
| 11 – PRCA posttreatment | −0.05 | 0.19 | 0.40** | 0.21 | 0.50** | 0.10 | 0.50** | 0.17 | 0.76** | 0.43** | 1.00 |
Note: MAAS = Mindful Awareness Acceptance Scale; OPQ = Outcome Probability Questionnaire; OCQ = Outcome Cost Questionnaire; BFNE = Brief Fear of Negative Evaluation; PRCS = Personal Report of Confidence as a Speaker; PRCA = Personal Report of Communication Apprehension.
p < .05.
p < .01.
Outcome probability as a mediator of mindfulness and social phobia symptoms
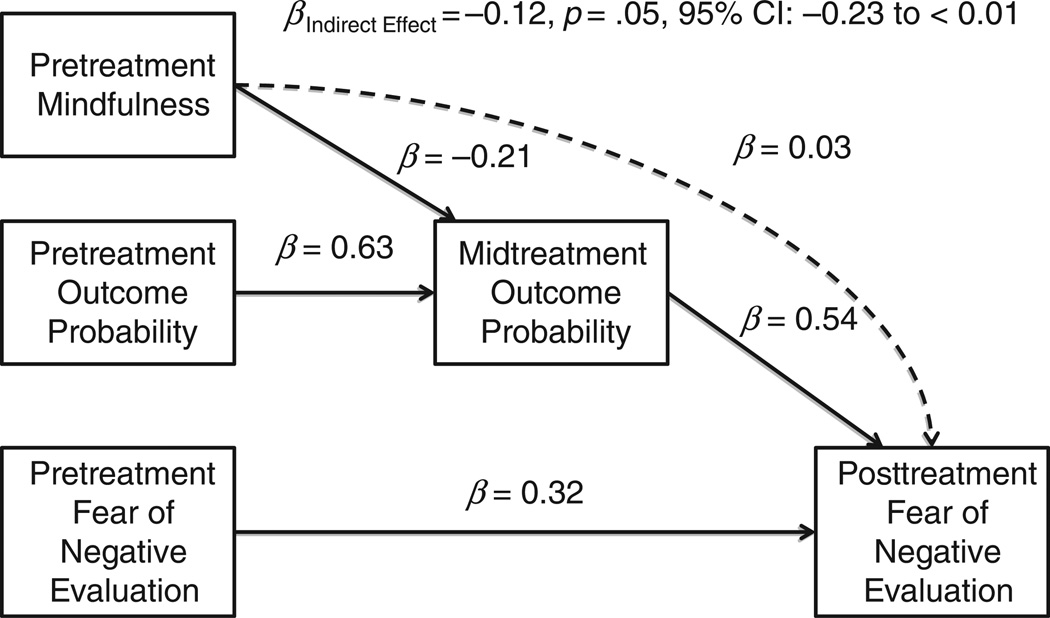
First, the A-path was evaluated to determine the association between pretreatment MAAS scores and change in OPQ scores from pre- to midtreatment. There was a significant A-path in that pretreatment MAAS scores were negatively associated with midtreatment OPQ scores controlling for pretreatment OPQ scores (β = −0.22, p = .03). The first model assessed the indirect effect of MAAS scores on BFNE scores via OPQ scores. Controlling for pretreatment BFNE scores, the association between pretreatment MAAS scores on posttreatment BFNE (C-path) approached significance (β = −0.17, p = .08). There was support for a significant B-path as midtreatment OPQ scores were associated with posttreatment BFNE scores while controlling for the respective pretreatment measures (β = 0.53, p < .01). Finally, the indirect effect of MAAS scores on BFNE scores via OPQ scores was significant (β = −0.12, p = .05, 95% CI: −0.23 to <0.01). The final mediational model approximated the data well, χ2 (2) = 1.41, p = .49; RMSEA < 0.01, 95% CI: <0.01 to 0.22; CFI = 0.99; SRMR = 0.02. The total model explained 52% of the variance in posttreatment BFNE scores (Figure 1).
Figure 1.
Mediation model of cognitive biases predicting post-treatment social anxiety symptoms.
A similar pattern of findings was obtained for the measures of public speaking as outcome variables (PRCA, PRCS). The association between pretreatment MAAS scores on posttreatment PRCA (C-path) was not significant (β = −0.03, p = .81) after controlling for pretreatment PRCA scores. However, the association between midtreatment OPQ scores and posttreatment PRCA scores (B-path) was significant after controlling for the respective pretreatment variables (β = 0.39, p < .01). Finally, the indirect effect of MAAS scores on PRCA scores via OPQ scores was significant (β = −0.11, p = .05, 95% CI: −0.22 to <0.01). The final mediation model approximated the data well, χ2 (2) = 1.43, p = .49; RMSEA < 0.01, 95% CI: <0.01 to 0.23; CFI = 0.99; SRMR = 0.02. The final model accounted for 56% of posttreatment PRCA scores.
The association between pretreatment MAAS scores on posttreatment PRCS (C-path) was not significant (β = −0.01, p = .94) after controlling for pretreatment PRCS scores. The B-path association, between midtreatment OPQ scores and posttreatment PRCS scores, was significant after controlling for the respective pretreatment variables (β = 0.46, p < .01). Finally, the indirect effect of MAAS scores on PRCS scores via OPQ scores was significant (β = −0.13, p = .04, 95% CI: −0.22 to <0.01). The final mediation model approximated the data well, χ2 (2) = 2.48, p = .29; RMSEA = 0.06, 95% CI: <0.01 to 0.27; CFI = 0.99; SRMR = 0.03. The final model accounted for 26% of posttreatment PRCS scores.
Outcome cost as a mediator of mindfulness and social phobia symptoms
The same approach was used to evaluate OCQ scores as a mediator of the relation between MAAS and social phobia scores. However, there was not an association between pretreatment MAAS scores and midtreatment OCQ scores controlling for pretreatment OCQ scores (β = −0.10, p = .32). Although mediation could no longer be established, an additional model was fitted to the data to fully evaluate the associations between OCQ, MAAS, and treatment response. This model approximated the data well for the BFNE, χ2 (2) = 1.55, p = .46; RMSEA < 0.01, 95% CI: <0.01 to 0.23; CFI = 0.99; SRMR = 0.03 (see Figure 1 for a parallel model). There was support for a significant association between midtreatment OCQ scores and posttreatment BFNE after controlling for pretreatment values (β = 0.33, p < .01). However, MAAS scores were unrelated to posttreatment BFNE scores (β = −0.14, p = .15). The total model explained 41% of the variance in posttreatment BFNE scores.
For measures of public-speaking fear, the comprehensive model approximated the data well for the PRCA (χ2 (2) = 1.05, p = .59; RMSEA = 0.01, 95% CI: <0.01 to 0.21; CFI = 0.99; SRMR = 0.02) and the PRCS (χ2 (2) = 0.39, p = .82; RMSEA = 0.01, 95% CI: <0.01 to 0.15; CFI = 0.99; SRMR = 0.01). Midtreatment OCQ scores were positively related to posttreatment PRCA scores (β = 0.49, p < .01), whereas pretreatment MAAS scores were not (β = −0.10, p = .34). Midtreatment OCQ scores were also positively associated with posttreatment PRCS scores (β = 0.52, p < .01), whereas pretreatment MAAS scores were not (β = 0.09, p = .48).
Taken together, the findings of the current study suggest that there is a significant indirect effect of MAAS scores on the BFNE, PRCA, and PRCS through OPQ scores. However, there was no support for an indirect effect via OCQ scores despite a consistent positive relation between OCQ scores and scores on the BFNE, PRCA, and PRCS.
Discussion
The current study examined cognitive biases as mediators of the relation between mindfulness and changes in social phobia symptoms following CBT. As predicted, mindfulness was negatively related to probability and cost bias measured at a later time point, with higher pretreatment mindfulness predicting less cognitive bias at midtreatment after controlling for pretreatment biases. Also as expected, lower probability and cost biases at midtreatment predicted greater change in social anxiety symptoms following treatment. Although there was no significant C-path (i.e., a direct relationship from X to Y) between mindfulness and social anxiety symptom change on any measure, contemporary guidelines suggest that the significance of the indirect path is of most importance in identifying mediation (Mackinnon et al., 2002). Indeed, tests of mediation in the present study showed that mindfulness exerts an indirect effect on symptom change following CBT via its relation to probability bias, but not cost bias. These findings were consistent across three separate indices of social anxiety symptoms (i.e., BFNE, PRCA, and PRCS).
It is worth noting that the treatment did not target mindfulness in any way; instead, the pretreatment mindfulness was measured and identified individuals’ tendency to be mindful (i.e., attentive toward the present moment) in daily life before they received treatment. Thus, our findings suggest that individuals who entered CBT with higher levels of mindfulness appeared to experience more symptom reduction following treatment due to lower levels of probability bias at midtreatment. Because mindfulness is presumed to reflect attention to moment-to-moment experience (Kabat-Zinn, 2003), individuals with higher levels of mindfulness may have been better able to disengage from excessive self-focused attention (which was explicitly targeted in this treatment). In addition, it is also possible that mindfulness facilitated attention to external cues in the environment that help disconfirm the probability of a negative outcome and develop new information to compete with existing fear memories (see Amir et al., 2009).
One interesting and unexpected finding was that probability bias, but not cost bias, mediated the relation between mindfulness and symptom change. This finding suggests that mindfulness may be more relevant to probability bias; that is, noticing what comes up in the present may help individuals identify the actual, in-the-moment frequency of negative social events (probability bias). Given that our measure of mindfulness specifically assessed the present-moment attention aspect of mindfulness, aspects of mindfulness that are related to attentional allocation in particular may be especially relevant to probability bias. For example, a clinically anxious individual who is attentive in his/her daily activities may still be likely to think negative social events will be terrible (i.e., costly) if they do occur. After learning about cognitive biases, this individual may be better attuned to the environment and thus may more quickly notice that it is unlikely that others will ridicule them if they give a speech in public. However, this individual’s higher level of present-moment attention may not help her/him in better evaluating how costly this negative event would be if it did occur. Cost estimates require the formation of judgments based on evaluative categories (i.e., good versus bad); more accurate cost evaluations may require aspects of mindfulness over and above attentional allocation. These aspects of mindfulness are not measured by the MAAS. It is possible that measures of mindfulness which assess other aspects of mindfulness, such as nonjudgment and nonreactivity to present-moment experience, would have yielded different results.
The mixed findings for probability and cost bias echo mixed findings in the literature about their relative importance for social phobia treatment. Foa and Kozak (1986) argued that cost bias was more important than probability bias for social phobia because negative social interactions are so common, and studies show that decreases in cost biases mediate improvement following treatment (Foa et al., 1996; Hofmann, 2004). However, other research shows that reductions in both cost and probability bias are associated with better treatment response (McManus et al., 2000). Finally, in a methodologically rigorous study designed to test the relative roles of these biases, Smits and colleagues (2006) found that whereas changes in both probability bias and cost bias accounted for fear reduction, the cause of fear reduction could be attributed to reductions in probability bias, while changes in cost bias were a consequence of fear reduction. Examining the role of probability and cost biases clearly is an area of active research, and results from the current study support the notion that probability and cost biases function differently in the treatment of SAD.
It should be noted that the relation between mindfulness, cognitive biases, and symptom change may be different for a treatment that explicitly targets mindfulness. Thus far, none of the studies showing a positive effect of mindfulness-based interventions on social phobia (e.g., Dalrymple & Herbert, 2007; Kocovski et al., 2009; Koszycki, Benger, Shlik, & Bradwejn, 2007) have examined the roles of probability and cost bias in relation to outcomes of mindfulness-based treatment. Exploratory research examining the efficacy of this treatment has theoretically linked mindfulness and current models of social anxiety (Koszycki et al., 2007), but have not directly explored how cognitive biases may factor in response to mindfulness-based interventions. Some mindfulness-based interventions are based on theoretical models that have, at their root, differing philosophical assumptions than cognitive-behavioral models of psychopathology and treatment (i.e., contextual behavioral models; Hayes et al, 2013). However, linking well-researched constructs from cognitive-behavioral models of social phobia to newer forms of treatment may shed light on the relative roles of these biases across treatment type. Specifically, future work should examine the degree to which change in mindfulness affects change in cognitive biases in the context of a mindfulness intervention.
There are several methodological limitations of note. First, the current study did not examine true longitudinal temporal mediation. True temporal mediation is most rigorously established when the effects on independent variables are isolated. It is possible that treatment differentially affected any or all of these variables over time, and it is unclear which variables in this study may have been affected by treatment. Thus, our data must be interpreted as they apply to individuals with social phobia undergoing CBT. Also, although the MAAS is widely used as a measure of mindfulness and has been shown to have sound psychometric properties (Brown & Ryan, 2003), others suggest that it is a measure of general inattentiveness (Grossman, 2011; Van Dam, Earleywine, & Borders, 2010), as the MAAS is related to exaggerated lapses of attention on behavioral tasks (Schmertz, Robins, & Anderson, 2009). The MAAS also has been criticized as a limited measure as it does not assess the purposeful regulation of attention (e.g., “nonjudgmentally”, Kabat-Zinn, 1994, p. 4) found in many definitions (e.g., Baer, Smith, & Allen, 2004). However, nonjudgmental awareness has been correlated with items from the MAAS in other studies (Baer et al., 2006). There are several limitations of generalizability. The high level of education is not typical of socially anxious samples. Individuals with higher levels of education may be more prepared to learn complex verbal concepts that are taught in psychotherapy. It is unknown if similar results would apply to populations with lower levels of education. Although the rate of comorbidity in the current study is comparable to recent studies utilizing Internet-based or virtual reality exposure therapy for public-speaking fears (7–12.5%; Andersson et al., 2006; Botella et al., 2008), it is lower than that found in other socially anxiety samples. Another limitation is that the internal consistency of the PRCS at pretreatment was questionable (α = .69), which is lower than has been found in other studies utilizing the PRCS (Paul, 1966). It is possible that, at pretreatment, the items of the PRCS did not represent a unitary construct for participants. Finally, the inclusion criteria for the study specified that fear of public speaking must be the primary social fear, and others have argued that public-speaking anxiety may be a specific subtype of social phobia (Blöte, Kint, Miers, & Westenberg, 2009). The results of this study, therefore, may not extend to more severe, comorbid samples of socially anxious individuals.
Despite these limitations, our findings are the first to show that mindfulness exerts a positive influence on treatment for social phobia via its relation to probability biases, even when mindfulness is not explicitly targeted during treatment. This intriguing finding urges further research for how mindfulness may be incorporated into existing CBTs to maximize treatment response. More research is also needed to understand how, when, and for whom mindfulness impacts change in social anxiety symptoms following CBT.
Acknowledgments
This research described in this paper was supported in part by R42MH60506 awarded to Page L. Anderson. Matthew Price is supported by T32MH018869.
References
- Amir N, Beard C, Burns M, Bomyea J. Attention modification program in individuals with generalized anxiety disorder. Journal of Abnormal Psychology. 2009;118(1):28–33. doi: 10.1037/a0012589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson PL, Price M, Edwards SM, Obasaju MA, Schmertz SK, Zimand E, Calamaras MR. Virtual reality exposure therapy for social phobia: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2013 doi: 10.1037/a0033559. [DOI] [PubMed] [Google Scholar]
- Anderson PL, Zimand E, Hodges LF, Rothbaum BO. Cognitive behavioral therapy for public speaking anxiety using virtual reality for exposure. Depression and Anxiety. 2005;22:156–158. doi: 10.1002/da.20090. [DOI] [PubMed] [Google Scholar]
- Andersson G, Carlbring P, Holmström A, Sparthan E, Furmark T, Nilsson-Ihrfelt E, Ekselius L. Internet-based self-help with therapist feedback and in vivo group exposure for social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:677–686. doi: 10.1037/0022-006X.74.4.677. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: The Kentucky inventory of mindfulness skills. Assessment. 2004;11:191–206. doi: 10.1177/1073191104268029. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Beitel M, Ferrer E, Cecero JJ. Psychological mindedness and awareness of self and others. Journal of Clinical Psychology. 2005;61:739–750. doi: 10.1002/jclp.20095. [DOI] [PubMed] [Google Scholar]
- Blöte AW, Kint MJW, Miers AC, Westenberg PM. The relation between public speaking anxiety and social anxiety: A review. Journal of Anxiety Disorders. 2009;23:305–313. doi: 10.1016/j.janxdis.2008.11.007. [DOI] [PubMed] [Google Scholar]
- Botella C, Gallego MJ, Garcia-Palacios A, Baños RM, Quero S, Guillen V. An internet-based self-help program for the treatment of fear of public speaking: A case study. Journal of Technology in Human Services. 2008;26:182–202. [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Burton M, Schmertz SK, Price M, Masuda A, Anderson PL. The relation between mindfulness and fear of negative evaluation over the course of cognitive behavioral therapy for social phobia. Journal of Clinical Psychology. 2013;69(3):222–228. doi: 10.1002/jclp.21929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler G, Mathews A. Cognitive processes in anxiety. Advances in Behaviour Research & Therapy. 1983;5(1):51–62. [Google Scholar]
- Clark DM, Wells A. A cognitive model of social phobia. In: Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, editors. Social phobia: Diagnosis, assessment, and treatment. New York, NY: Guilford Press; 1995. pp. 69–93. [Google Scholar]
- Cole DA, Maxwell SE. Testing meditational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Collins KA, Westra HA, Dozois DA, Stewart SH. The validity of the brief version of the fear of negative evaluation scale. Journal Of Anxiety Disorders. 2005;19(3):345–359. doi: 10.1016/j.janxdis.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Dalrymple KL, Herbert JD. Acceptance and commitment therapy for generalized social anxiety disorder: A pilot study. Behavior Modification. 2007;31:543–568. doi: 10.1177/0145445507302037. [DOI] [PubMed] [Google Scholar]
- Farb NAS, Segal ZV, Mayberg H, Bean J, McKeon D, Fatima Z, Anderson AK. Attending to the present: Mindfulness meditation reveals distinct neural modes of self-reference. Social Cognitive and Affective Neuroscience. 2007;2:313–322. doi: 10.1093/scan/nsm030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A. Discovering statistics using IBM SPSS statistics. 2nd ed. Thousand Oaks, CA: Sage; 2005. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, research version, non-patient edition (SCID-I/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Foa EB, Franklin ME, Perry KJ, Herbert JD. Cognitive biases in generalized social phobia. Journal of Abnormal Psychology. 1996;105:433–439. [PubMed] [Google Scholar]
- Foa EB, Huppert JD, Cahill SP. Emotional processing theory: An update. In: Rothbaum BO, editor. Pathological anxiety: Emotional processing in etiology and treatment. New York, NY: Guilford Press; 2006. pp. 3–24. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99(1):20–35. [PubMed] [Google Scholar]
- Franklin ME, Huppert J, Langner R, Leiberg S, Foa EB. Interpretation bias: A comparison of treated social phobics, untreated social phobics, and controls. Cognitive Therapy and Research. 2005;29:289–300. [Google Scholar]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10(1):83–91. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin P, Ramel W, Gross J. Mindfulness meditation training and self-referential processing in social anxiety disorder: Behavioral and neural effects. Journal of Cognitive Psychotherapy. 2009;23:242–257. doi: 10.1891/0889-8391.23.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P. Defining mindfulness by"how poorly I think I pay attention during everyday awareness” and other intractable problems for psychology’s (re) invention of mindfulness. Psychological Assessment. 2011;23:1034–1040. doi: 10.1037/a0022713. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Levin ME, Plumb-Vilardaga J, Villatte JL, Pistorello J. Acceptance and commitment therapy and contextual behavioral science: Examining the progress of a distinctive model of behavioral and cognitive therapy. Behavior Therapy. 2013;44(2):180–198. doi: 10.1016/j.beth.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrichs N, Hofmann SG. Information processing in social phobia: A critical review. Clinical Psychology Review. 2001;21:751–770. doi: 10.1016/s0272-7358(00)00067-2. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Cognitive mediation of treatment change in social phobia. Journal of Consulting and Clinical Psychology. 2004;72:392–399. doi: 10.1037/0022-006X.72.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope DA, Heimberg RG. Public and private self-consciousness and social phobia. Journal of Personality Assessment. 1988;52:626–639. doi: 10.1207/s15327752jpa5204_3. [DOI] [PubMed] [Google Scholar]
- Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- Jostes A, Pook M, Florin I. Public and private self-consciousness as specific psychopathological features. Personality and Individual Differences. 1999;27:1285–1295. [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are: Mindfulness meditation in everyday life. New York, NY: Hyperion; 1994. [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice. 2003;10(2):144–156. [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher K, Pbert L, Santorelli SF. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149:936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Kang C, Whittingham K. Mindfulness: A dialogue between Buddism and clinical psychology. Mindfulness. 2010;1(3):161–173. [Google Scholar]
- Kocovski NL, Fleming JE, Rector NA. Mindfulness and acceptance-based group therapy for social anxiety disorder: An open trial. Cognitive and Behavioral Practice. 2009;16:276–289. [Google Scholar]
- Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behaviour Research and Therapy. 2007;45:2518–2526. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Leary MR. A brief version of the Fear of Negative Evaluation Scale. Personality and Social Psychology Bulletin. 1983;9:371–375. [Google Scholar]
- Lucock MP, Salkovskis PM. Cognitive factors in social anxiety and its treatment. Behaviour Research and Therapy. 1988;26:297–302. doi: 10.1016/0005-7967(88)90081-2. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt G, Kristeller JL. Mindfulness and meditation. In: Miller WR, editor. Integrating spirituality into treatment: Resources for practitioners. Washington, DC: American Psychological Association; 1999. pp. 67–84. [Google Scholar]
- McCroskey JC. Validity of the PRCA as an index of oral communication apprehension. Communication Monographs. 1978;45(3):192–203. [Google Scholar]
- McLaughlin KA, Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behaviour Research and Therapy. 2011;49(3):186–193. doi: 10.1016/j.brat.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus F, Clark DM, Hackmann A. Specificity of cognitive biases in social phobia and their role in recovery. Behavioural and Cognitive Psychotherapy. 2000;28:201–209. [Google Scholar]
- Miller J, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness-based stress reduction intervention in the treatment of anxiety disorders. General Hospital Psychiatry. 1995;17(3):192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus 3.0: User’s guide. Los Angeles, CA: Author; 2004. [Google Scholar]
- Paul GL. Insight versus systematic desensitization in psychotherapy: An experiment in anxiety reduction. Redwood City, CA: Stanford University Press; 1966. [Google Scholar]
- Poulton RG, Andrews G. Change in danger cognitions in agoraphobia and social phobia during treatment. Behaviour Research and Therapy. 1996;34:413–421. doi: 10.1016/0005-7967(96)00009-5. [DOI] [PubMed] [Google Scholar]
- Safer DL, Telch CF, Agras WS. Dialectical behavior therapy for bulimia nervosa. American Journal of Psychiatry. 2001;158:632–634. doi: 10.1176/appi.ajp.158.4.632. [DOI] [PubMed] [Google Scholar]
- Schmertz SK, Anderson PL, Robins DL. The relation between self-report mindfulness and performance on tasks of sustained attention. Journal of Psychopathology and Behavioral Assessment. 2009;31(1):60–66. [Google Scholar]
- Schmertz SK, Masuda A, Anderson PL. Cognitive processes mediate the relation between mindfulness and social anxiety within a clinical sample. Journal of Clinical Psychology. 2012;68:362–371. doi: 10.1002/jclp.20861. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Rosenfield D, McDonald R, Telch MJ. Cognitive mechanisms of social anxiety reduction: An examination of specificity and temporality. Journal of Consulting and Clinical Psychology. 2006;74:1203–1212. doi: 10.1037/0022-006X.74.6.1203. [DOI] [PubMed] [Google Scholar]
- Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69:1061–1065. doi: 10.1037//0022-006x.69.6.1061. [DOI] [PubMed] [Google Scholar]
- Treanor M. The potential impact of mindfulness on exposure and extinction learning in anxiety disorders. Clinical Psychology Review. 2011;31:617–625. doi: 10.1016/j.cpr.2011.02.003. [DOI] [PubMed] [Google Scholar]
- Uren TH, Szabó M, Lovibond PF. Probability and cost estimates for social and physical outcomes in social phobia and panic disorder. Journal of Anxiety Disorders. 2004;18:481–498. doi: 10.1016/S0887-6185(03)00028-8. [DOI] [PubMed] [Google Scholar]
- Van Dam NT, Earleywine M, Borders A. Measuring mindfulness? An item response theory analysis of the Mindful Attention Awareness Scale. Personality and Individual Differences. 2010;49:805–810. [Google Scholar]
- Weeks JW, Heimberg RG, Fresco DM, Hart TA, Turk CL, Schneier FR, Liebowitz MR. Empirical validation and psychometric evaluation of the brief fear of negative evaluation scale in patients with social anxiety disorder. Psychological Assessment. 2005;17(2):179–190. doi: 10.1037/1040-3590.17.2.179. [DOI] [PubMed] [Google Scholar]