Abstract
Given the importance of public information environment in cancer control, it is theoretically and practically important to explore how people's media use to acquire health information influences their beliefs about cancer prevention. In the current research, we focus on the role of the Internet in shaping fatalistic beliefs about cancer prevention (cancer fatalism). To be more specific, we examine the effect of Internet use for health information on changes in cancer fatalism using a 2-wave nationally representative survey. We then investigate whether the effect of Internet use on cancer fatalism is moderated by education and health knowledge. Health-related Internet use reduced cancer fatalism only among those with average and lower than the average levels of education and health knowledge.
Fatalism is an outlook that events are controlled by external forces and humans are powerless to influence them. Fatalistic beliefs about cancer prevention are a situational manifestation of fatalism and thus can be understood as beliefs that cancer prevention is beyond human control and getting cancer is a matter of fate or luck (Freeman, 1991; Powe & Finnie, 2003). These beliefs are further characterized by a sense of pessimism, helplessness, and confusion (Niederdeppe & Gurmankin Levy, 2007). Although a sizeable proportion of cancer incidence is preventable, many Americans still hold fatalistic beliefs about cancer prevention (cancer fatalism; e.g., “everything causes cancer”; “there's not much I can do to lower my risk of cancer”; Jensen et al., 2011; Niederdeppe, Fowler, Goldstein, & Pribble, 2010). People who hold these beliefs have lower rates of cancer screening, engage less frequently in healthy behaviors such as fruit and vegetable consumption, and engage more often in health-threatening behaviors like smoking (Freeman, 1991). This phenomenon is particularly worrisome because these beliefs are more prevalent among those with low socioeconomic status (SES) relative to those with high SES (Freeman, 1991; Powe & Finnie, 2003). As populations with lower SES shoulder a greater burden of cancer than those with higher SES, reducing cancer fatalism should be an important public health goal, particularly among low-SES groups (Viswanath & Emmons, 2006).
Little empirical research has been conducted regarding why individuals with low SES have higher cancer fatalism than those with high SES. However, scholars suggest that differences in access to health-related information are among several underlying mechanisms (Berkman, Davis, & McCormack, 2010; Viswanath & Emmons, 2006). Public health educators have focused recent attention on relaying useful, accurate information to the general public through diverse media channels (Slater, Hayes, Reineke, Long, & Bettinghaus, 2009). Despite the importance of information and knowledge conveyed through media in cancer control, previous research suggests that some forms of news coverage may increase cancer fatalism over time (Jensen et al., 2011; Lee & Niederdeppe, 2011). To our knowledge, only three studies (Jensen et al., 2011; Lee & Niederdeppe, 2011; Niederdeppe et al., 2010) have examined the effect of specific channels of media use on cancer fatalism. All three show that exposure to cancer news, particularly via local television, may cultivate fatalistic beliefs about cancer prevention.
Given the importance of the Internet as an emerging and crucial source of cancer information, we examine the role of the Internet in shaping cancer fatalism over time among those with both low and high levels of SES. Previous studies (Lee & Niederdeppe, 2011; Niederdeppe et al., 2010) have not accurately captured the influences that Internet use may have on cancer fatalism because Internet use in these studies has been captured using global measures of time spent on the web (e.g., how often did you use the Internet?) instead of health-specific Internet-use items. Because Internet use is not a monolithic concept, measures of time spent with the Internet do not say anything about the specific content to which Internet users are exposed. Also, it has been consistently found that content-specific media exposure measures perform better than general media exposure measures in predicting health outcomes (Romantan, Hornik, Price, Cappella, & Viswanath, 2008; Slater, 2004). Thus, we examine whether Internet use specifically to acquire health information may influence fatalistic beliefs about cancer prevention.
Moreover, we explore whether the Internet functions as a source of further social stratification or as a possible solution to bridge gaps in cancer fatalism by education. Considerable resources have been invested in recent years to develop and market Internet-based programs for cancer education, particularly among low-SES groups. For instance, the National Cancer Institute recently awarded nearly 1 million dollars to the Digital Divide Pilot Projects to develop new strategies to reach underprivileged populations through the Internet (Gustafson et al., 2008; Kreps et al., 2007). A few intervention programs sponsored by these projects, such as the Comprehensive Health Enhancement Support System (CHESS) program, CancerInforNet, and the Low-Literacy User Cancer Information Interface (LUCI) program, show that there exist only minimal SES differences in motivations and skills to use the Internet for health information. Emerging information and communication technologies could thus empower low-SES cancer patients by increasing knowledge and social support (for an overview, see Kreps et al., 2007).
Here, we examine whether health information-related Internet use may influence fatalistic beliefs about cancer prevention over time using a two-wave nationally representative survey. Considering that perceptions of cancer fatalism develop over time (Freeman, 1991; Powe & Finnie, 2003), longitudinal data are well suited for this study. We then test whether education and health knowledge moderate the effect of Internet use on cancer fatalism. We use education as a single indicator of SES because income has not been consistently associated with cancer fatalism in studies employing nationally representative survey data (Lee & Niederdeppe, 2011; Niederdeppe & Gurmankin Levy, 2007) and because education is the most widely used indicator of SES in this area of research (Gaziano, 1997; Lee, 2009). We also employ health knowledge as a moderator because it has been regarded as one subdimension or a proxy for health literacy, defined as “the degree to which individuals can obtain, process, understand, and communicate about health-related information needed to make informed health decisions” (Berkman et al., 2010, p. 16). To isolate the independent effect of Internet use on cancer fatalism, we control for sociodemographic factors, health-related variables, and other media use behaviors that predicted Internet use and/or cancer fatalism in previous studies (Freeman, 1991; Niederdeppe & Gurmankin Levy, 2007). We seek to inform recent debates about communication inequality in the context of the Internet and public health, and hope to catalyze further research on the role of the Internet in health disparities.
Possible effects of Internet use on cancer fatalism
One perspective argues that exposure to online health information is likely to increase confusion and fatalism about health issues (Hungerford, 2009). Several scholars point out that online health information has many shortcomings—it contains inaccurate and incomplete information, and may not follow ethical publication guidelines (Benigeri & Pluye, 2003). Also, because anyone can post content on the Internet without going through the editorial review process associated with other media (e.g., print, television), people may be exposed to research findings that have not undergone scientific peer review and have not been replicated. Furthermore, many traditional news sites offer opportunities for the general public to comment on stories about cancer, which may convey a sense of controversy about even well-established and scientifically vetted findings. Thus, consumers of online health information may be exposed to information that is consistent with the fatalistic beliefs that “everything causes cancer” or that “there's nothing a person can do to reduce their chances of getting cancer.”
Other scholars have argued that attributes of the Internet itself may also afford negative consequences for health-related beliefs, including beliefs about cancer prevention. The Internet is characterized by high levels of user control and interactivity, which in part results from “hypertextuality” or the ability to follow one link to another (Kim & Stout, 2010; Lowrey & Kim, 2009). Eveland and Dunwoody (2001) found that hypertext can cause disorientation and cognitive overload by providing users with more freedom—too many choices—to select what type of content they read or watch. Rather than following content in a linear manner, users may become lost on the Web, jumping from one small snippet of information to another based on their link patterns, and in the process may develop a sense of cognitive, information overload. Disorientation and cognitive overload interfere with learning, which may impair the ability to discern credible and noncredible online sources or may lead to a failure to notice or process information (e.g., inclusion of caveats or limitations) that could offset fatalistic beliefs about cancer (Jensen et al., 2011).
We adopt a different perspective. Many studies report that online health information is usually factually true, although limited in other aspects like readability, accountability, and completeness (Berland et al., 2001). Even studies reporting inaccurate and inappropriate health information on the Internet tend to find that this information is incorrect because it is outdated rather than completely factually wrong (Eysenbach, Powell, Kuss, & Sa, 2002). Moreover, according to Eysenbach et al. (2002), the incompleteness should not be a valid criterion on which to evaluate the quality of online health information because the Internet is a huge network of information. Thus, if a particular source is not complete, one can look to the abundant additional sources available online to fill in any gaps. Finally, the aforementioned problems of online health information such as readability and accountability are less severe when compared to similar presentation styles in other media (Eysenbach et al., 2002).
Hypertextuality can promote learning too. Although hypertextuality may lead to overload and disorientation, it may also promote elaboration and rehearsal, which in turn promote learning and integration (Eveland & Dunwoody, 2001; Lowrey & Kim, 2009). While several studies report less recall following online news exposure with in-text links than print versions of the same information without such links, some studies also find that hypertext is more advantageous in learning structural knowledge and higher-order knowledge (Eveland, Marton, & Seo, 2004; Lowrey & Kim, 2009). Because knowledge related to cancer prevention includes complex structural information (e.g., probabilistic, relative risk estimates; technical medical terminology) as well as simple factual knowledge, Internet use may actually promote the integration of new information (“here are the things we already know reduce cancer risk, here are things that increase it, and here is where this new information fits in with my existing knowledge”) and thus reduce fatalistic beliefs about cancer prevention. We thus hypothesize that health-related Internet use will diminish fatalistic beliefs about cancer prevention by facilitating integration and assimilation of new information about cancer prevention in ways that do not lead to cognitive overload (H1).
Theorizing about the role of the Internet in cancer fatalism disparities: The moderating roles of education and health knowledge
Inequalities in Internet use and its effects have been of great interest in the field of communication and related disciplines. First, the digital divide—gaps in access to computers and the Internet by SES and race/ethnicity—has been heavily debated among both scholars and policymakers (Selwyn, 2004; Viswanath & Kreuter, 2007). Even if gaps in physical access to computers and the Internet were to be solved, however, another layer of inequality may exist. The knowledge-gap hypothesis argues that, even with equal access, low-SES groups tend to acquire mediated information and integrate this knowledge at a slower rate than high-SES groups, which in turn widens knowledge gaps (Slater et al., 2009; Tichenor, Donohue, & Olien, 1970). Recently, knowledge gaps have been detected on the Internet in the context of health information (Lee, 2009). The Internet is characterized as an active medium which requires higher levels of skill and literacy for its users to navigate the web efficiently and to learn from it, compared to passive, traditional mass media channels (Bonfadelli, 2002; DiMaggio, Hargittai, Celeste, & Shafer, 2004; Selwyn, 2004).
More recently, scholars have expanded the concept of the digital divide and the knowledge-gap hypothesis to include more diverse aspects of Internet use. DiMaggio et al. (2004), for instance, proposed the concept of digital inequality, which refers to inequalities in five specific areas of Internet use (i.e., inequalities in equipment, autonomy, skills, support, and purposes). The digital inequality model attempts to capture the complex relationship that individuals have developed with the Internet by redressing the limitations of “the conventional dichotomous notion of the digital divide” (Selwyn, 2004, p. 341). Similarly, Radmanadhan & Viswanath (2006, p. 132) proposed the concept of communication inequality, which was defined as “inequalities in communication characterized by differences in access to communication sources, processing and retention of information, and the ability to act on it.” These scholars contend that low-SES groups stand to benefit less from their Internet use than high-SES groups. Difficulty in processing and retaining complex and sometimes conflicting information about cancer could lead to increased fatalistic beliefs about cancer prevention.
Other theoretical perspectives, however, support the opposite prediction. People with higher levels of education tend to be more knowledgeable about health in general, and cancer in particular, than those with lower levels of education (Viswanath & Emmons, 2006). Because human beings are “cognitive misers” (Eagly & Chaiken, 1993), highly educated people may not seek and process health or medical information from the Internet if they already hold enough information in these areas. In contrast, those with low levels of education who have Internet access at all may benefit more from their Internet use than their more educated counterparts to compensate for a lack of prior health or medical knowledge. That is, since active information processing tends to increase persuasion (Briñol & Petty, 2006), and less educated individuals may have greater reason to actively process and successfully integrate new cancer-related information from the Internet, Internet use to acquire health information could decrease cancer fatalism more among less educated people than among more educated people. In light of strong arguments in each direction, we propose a research question (rather than hypothesis) to examine whether the effect of Internet use for health information on reducing cancer fatalism is larger for those with low levels of education than those with high levels of education (RQ1).
Education may not be an ideal indicator of the skills necessary to benefit from online health information. Controlling for educational attainment, there may be substantial differences in other factors that predict integration of cancer knowledge and fatalism (Berkman et al., 2010). Thus, we focus on health knowledge as a second potential moderator.
On the one hand, those who have greater health knowledge may be better suited to learn from online health information than less knowledgeable people. Online health information may be so difficult and full of uncertainties that those with low levels of health knowledge may have hard time in comprehending and putting it into use (Lee, 2009; Viswanath & Kreuter, 2007). According to this perspective, one would expect that those with high health knowledge would be likely to learn more than those with low health knowledge from online health information. This learning, in turn, should consequently reduce their fatalistic beliefs about cancer prevention.
On the other hand, however, different theoretical arguments support the prediction that the effect of Internet use on cancer fatalism should be greater for people with low levels of health knowledge. This alternative expectation is based the concept of “information sufficiency,” which posits that “people will exert whatever effort is required to attain a ‘sufficient’ degree of confidence that they have satisfactorily accomplished their processing goals” (Eagly & Chaiken, 1993, p. 330; Griffin, Dunwoody, & Neuwirth, 1999). Active information seeking and processing is partly determined by the gap between one's desired level of information and one's current level of information. Thus, those who already have high health knowledge should be “information sufficient” and less likely to seek and actively process online health information. To conserve cognitive resources, they may rely on heuristics like “everything causes cancer” or “there are too many recommendations” when integrating new cancer information. Thus, we also explore whether the effect of Internet use for health information on reducing cancer fatalism is larger or smaller for those with low health knowledge than those with high health knowledge (RQ2).
Methods
We employed a nationally representative survey of adults between the ages of 40 and 70 and conducted a longitudinal follow-up survey 1 year later. Because cancer risk accelerates rapidly between the ages of 40 and 70 (Freeman, 1991), we focus on adults within this age group. Data were collected by Knowledge Networks (KN), a research firm that administers surveys via the Internet in respondents' homes. Respondents were chosen from a previously recruited KN panel of respondents and restricted to individuals who had been in the KN panel for fewer than 2 years. KN first selected participating households using a random-digit-dialing (RDD) sampling of U.S. households. If sampled households did not have Internet access, KN provided these households with free web television hardware and Internet access. The monthly recruitment rate for KN panel participation ranged from 18 to 25%, with an overall recruitment rate of 22%.
In total, 2,489 cases were collected from October 21, 2005 to October 25, 2006 for the first-round survey. Sampled panel members (including a proportion who were recruited into the panel specifically for this survey) received an e-mail invitation and follow-up reminders to complete the survey. The survey instrument was pretested by 211 respondents in September, 2005. The weekly participation rates ranged from 61 to 84%, with an overall participation rate of 73%. Thus, the response rate for the Wave 1 survey was 16%, the product of the overall panel recruitment rate (22) and the cooperation rate (73). The second round of data collection took place approximately 1 year later, in the same calendar month. The final sample size for the longitudinal analyses was 1,812 and consisted of participants who completed both waves of data collection. Seventy percent of the Wave 1 respondents were retained at Wave 2.1 The product of the original panel recruitment rate (22), the first-wave cooperation rate (73), and the second-wave cooperation rate (70) produced an overall response rate for the two-wave survey of 12%. Using data from the Current Population Survey (CPS), poststratification weights were used to adjust for sample under- or overrepresentation of groups that occurred either from patterned nonresponse or from purely stochastic factors. Weights accounted for discrepancies between national population estimates and our sample by sociodemographic variables that included age, gender, race/ethnicity, education, census region (Northeast, Midwest, South, and West), metropolitan area, and having Internet access. All analyses used these population weights in STATA.
Dependent variable: fatalistic beliefs about cancer prevention
Participants were asked to rate each of three statements about cancer fatalism (“it seems that everything causes cancer,” “there's not much I can do to lower my chances of getting cancer,” and “there are so many different recommendations about preventing cancer, I don't know which ones to follow”) on a 5-point scale (1 = strongly disagree, 2 = somewhat disagree, 3 = no opinion, 4 = somewhat agree, 5 = strongly agree). We averaged the three items to create a scale (Wave 1 α = .63, M = 2.94, SE = .02; Wave 2 α = .61, M = 3.00, SE = .03).2
Although the reliability of the cancer fatalism scale is low, this is consistent with previous studies using similar measures (Lee & Niederdeppe, 2011; Niederdeppe & Gurmankin Levy, 2007; Niederdeppe et al., 2010). Nevertheless, previous studies have also found that each individual scale item is associated with a lower likelihood of engaging in healthy behaviors (indicating that the items have predictive validity; Niederdeppe & Gurmankin Levy, 2007) and the three items share considerable variance. In addition, the substantive pattern of results was highly consistent when testing each item as a dependent variable separately. Thus, we examine the three-item scale rather than assessing Internet use effects on each item individually.
Independent variable: Internet use for health information
Internet use for health information was assessed with the two questions, designed to capture both scanned (information obtained through routine use of a medium) and sought information exposure (information obtained through active searching within a medium; Shim, Kelly, & Hornik, 2006): “How often have you read health information on the Internet in the past 30 days?; response categories 1 = not at all, 2=less than once per week, 3 = once per week, and 4 =two or more times a week,” and “Thinking about the past 12 months, how much have you actively looked for information about a specific health concern or medical problem that you or a family member had from the Internet?; response categories 1 = not at all, 2 = 1–2 times, 3 = 3–4 times, 4 = 5–12 times, and 5 = more than 12 times.” Since both scanned and sought information exposure are associated with cancer prevention behaviors (evidence of predictive validity; Shim et al., 2006) and these items were strongly correlated (Wave 1 r = .56, Wave 2 r = .54), we combined them into a single scale. After z-standardizing each item (because they were measured with different response options), we calculated their mean (Wave 1 M = −.01, SE =.02; Wave 2 M = −.08, SE = .02).
Moderating variables: Education and health knowledge
The first moderating variable is formal education. Respondents were asked about the highest level of school they had completed. We assigned each category the number of years that are typically required to finish each degree to create a ratio-level measure (e.g., high school graduates assigned a value of 12; Wave 1 M = 13.76, SE = .06; Wave 2 M = 13.73, SE =.08).
The second moderating variable is health knowledge, operationalized as an additive index of seven dichotomous items. Respondents were asked to indicate if the following statements were correct: (a) doctors say that both types of cholesterol (called LDL and HDL) should be kept as low as possible; (b) if a person has a gene for a disorder, that person will always get the disorder; (c) the Human Papilloma Virus is associated with an increased risk of cervical cancer; (d) the body mass index (BMI), used to measure obesity, is based on waist size and percent body fat; (e) there is currently a cure for cancer but the medical industry won't tell the public about it because they make too much money treating cancer patients; (f) men are more likely to die because of prostate cancer than because of heart disease; and (g) treating cancer with surgery can cause it to spread throughout the body (Wave 1 KR-20 = .64, M =3.19, SE =.04; Wave 2 KR-20=.61, M =3.52, SE =.06).
Scale reliability is low due in part to the dichotomous nature of these scaled items. Unlike political knowledge, there is no established measure of health knowledge commonly used in health communication research. Thus, in order to measure health knowledge for this age group (40–70), we adopted some items from previous studies on cancer (i.e., Gansler et al., 2005; Radosevich et al., 2004) and developed the other items. The above items were finally selected based on their distribution, face validity, nomological validity, and internal reliability in the pretest. Additional evidence of validity comes from a positive association with a measure of health information seeking that was not specific to the Internet (Wave 1 r = .20, Wave 2 r = .24).
Control variables: sociodemographic, health, and behavioral factors
We controlled for a variety of sociodemographic factors, health-related variables, and other media use behaviors that were found to predict Internet use for health information and/or cancer fatalism in previous work (Freeman, 1991; Niederdeppe & Gurmankin Levy, 2007) and thus could confound our interpretation of an association between Internet use and cancer fatalism. Among sociodemographic variables, we included age (Wave 1 M = 52.59, SE = .18; Wave 2 M = 52.79, SE = .24), gender (Wave 1 51.2% female, Wave 2 51.5% female), income (Wave 1 M =$55,350, SE = 940; Wave 2 M = $54,270, SE = 1,190), race/ethnicity (Wave 1 75% White, 10.9% African American, 8.8% Hispanic, 4.7% Other; Wave 2 72.9% White, 10.9% African American, 10.2% Hispanic, 5% Other), marital status (Wave 1 59% married, Wave 2 58% married), household size (Wave 1 M = 2.33, SE = .03; Wave 2 M = 2.29, SE = .04), frequency of religious events attendance (times per year; Wave 1 M = 23.21, SE = .64; Wave 2 M = 23.23, SE = .81), and employment status (Wave 1 62.5% employed, Wave 2 61% employed).
We also controlled for a variety of health-related variables. We calculated BMI (a measure of overweight) by dividing self-reported weight (in kg) by height (in m2; Wave 1 M = 28.69, SE = .16; Wave 2 M = 28.64, SE = .20). Health status was assessed using a single item that inquired, “In general, would you say that your health is …” Participants were offered five ordinal response options that ranged from “poor” (1) to “excellent” (5; Wave 1 M = 3.34, SE = .02; Wave 2 M = 3.37, SE = .03). Frequency of doctor visits was measured by asking respondents on a 5-point scale (1 = never, 2 = once or twice a month, 3 = three to six times, 4 = about once a month or so, 5 = more than once a month) the following question: “Over the past 12 months, how many times have you consulted a doctor about your health?” (Wave 1 M = 3.82, SE = .10; Wave 2 M = 3.70, SE = .12). Personal cancer history was measured by asking respondents whether or not they had been diagnosed with cancer by a doctor (Wave 1 12% yes, Wave 2 12.6% yes). Significant others' cancer history was measured by asking respondents whether any of their close family members or close friends had been diagnosed with cancer by a doctor (Wave 1 86.3% yes, Wave 2 87.3% yes). We accounted for smoking behavior by asking whether respondents had smoked a cigarette in the past 30 days (Wave 1 27.7% yes, Wave 2 26.7% yes).
In addition, our regression models included health information acquisition from other sources as controls to isolate independent effects of Internet use. We asked respondents how often they read about health issues in newspapers or general magazines, read special health or medical magazines or newsletters, watched special health segments of television newscasts, watched television programs (other than news) which address health issues or focus on doctors or hospitals, and talked with family or friends about health issues using a 4-point scale (1 = not at all, 2 = less than once per week, 3 = once per week, 4 = two or more times a week). We used these items to construct averaged scales of print media use for health (combining general newspapers/magazines with special health newsletters/magazines; Wave 1 r = .52, M = .69, SE = .01; Wave 2 r = .53, M = .65, SE = .02), television use for health (combining special health segments of television newscasts and television programs addressing health issues; Wave 1 r = .54, M = .73, SE = .01; Wave 2 r = .53, M = .69, SE = .02), and a one-item measure of interpersonal communication with family and friends (Wave 1 M = 1.05, SE = .02; Wave 2 M = .97, SE = .02). Finally, based on effects of local television news watching reported in previous studies (Lee & Niederdeppe, 2011; Niederdeppe et al., 2010), we measured local television news viewing by asking, “In the past 7 days, on how many days did you watch the local news on television?” (Wave 1 M = 4.98, SE = .06; Wave 2 M = 4.75, SE = .07).
Analytic procedures
To account for causal ordering, we employed a series of ordinary least squares (OLS) lagged dependent variable regression models (Campbell & Kwak, 2011; Finkel, 1995). We tested H1 by examining the lagged association between Internet use for health information at Wave 1 and fatalistic beliefs about cancer prevention at Wave 2, controlling for fatalistic beliefs about cancer prevention at Wave 1 and measured potential confounding factors. An effect of Internet use at Wave 1 on cancer fatalism at Wave 2, controlling for fatalism at Wave 1, can be interpreted as an effect of Internet use on the change in cancer fatalism over time.
To address RQ1 and RQ2, we constructed two hierarchical OLS regression models which included the control variables outlined above and the main-effect variable (i.e., Internet use for health information), followed by the interaction terms between (a) Internet use for health information and education and (b) Internet use for health information and health knowledge, respectively. To reduce multicollinearity associated with interaction terms, we z-standardized each variable (i.e., Internet use for health information, education, health knowledge) before forming the multiplicative terms (Aiken & West, 1991) and tested the interactive effects of education and health knowledge in separate models. We predicted fatalistic beliefs about cancer prevention at Wave 2 as a function of fatalistic beliefs about cancer prevention at Wave 1, Wave 1 independent and control variables, and Wave 1 interaction terms.
Results
We regressed Wave 2 fatalistic beliefs about cancer prevention on fatalistic beliefs about cancer prevention and potential confounders at Wave 1 (see Table 1, Model 1). As one might expect, Wave 1 fatalistic beliefs about cancer prevention was the strongest predictor of fatalistic beliefs about cancer prevention at Wave 2. Supporting H1, higher levels of Internet use for health information at Wave 1 predicted reductions in fatalistic beliefs about cancer prevention at Wave 2 (β = −.07, p < .05) after controlling for possible confounders.
Table 1. Testing the Effects of Internet Use, Education, and Health Knowledge at Wave 1 on Cancer Fatalism at Wave 2 (Two-Wave Panel Design).
| Predictors | Model 1: Main Effect | Model 2: Education × Internet | Model 3: Knowledge × Internet |
|---|---|---|---|
| Step 1 | |||
| Age | −.03 | −.03 | −.03 |
| Gender (male = 0, female = 1) | −.04 | −.04 | −.04 |
| Education | −.11** | −.11** | −.11** |
| Income | −.00 | −.01 | −.00 |
| Being African American | −.00 | −.00 | −.00 |
| Being Hispanic | .03 | .03 | .03 |
| Being other race | .03 | .04 | .03 |
| Marital status | .02 | .02 | .02 |
| Employment status | .00 | .01 | .01 |
| Religious events attendance | −.00 | −.00 | −.00 |
| Household size | .01 | .01 | .01 |
| Health status | −.03 | −.03 | −.03 |
| Body mass index | .02 | .02 | .02 |
| Current smoker | .11** | .11** | .11** |
| Personal cancer experience | −.03 | −.03 | −.03 |
| Significant others' cancer experience | −.06 | −.06 | −.05 |
| Frequency of doctor visits | .05 | .05 | .05 |
| Health knowledge | −.09** | −.09** | −.09** |
| Cancer fatalism (Wave 1) | .41*** | .41*** | .41*** |
| Local television news viewing | .01 | .01 | .01 |
| Print media use for health | .06 | .06 | .06 |
| Television use for health | −.04 | −.04 | −.04 |
| Interpersonal health communication | .03 | .03 | .03 |
| Incremental R2 (%) | 29.9*** | — | — |
| Step 2 | |||
| Internet use for health information | −.07* | −.07* | −.08* |
| Incremental R2 (%) | .3* | — | — |
| Step 3 | |||
| Internet × Education | — | .06* | — |
| Internet × Knowledge | — | — | .05* |
| Incremental R2 (%) | — | .4* | .3* |
| Total R2 (%) | 30.2*** | 30.6*** | 30.5*** |
| N | 1,646 | 1,646 | 1,646 |
Notes:
p < .05;
p < .01;
p < .001.
Displayed values are weighted standardized regression coefficients and explained variances.
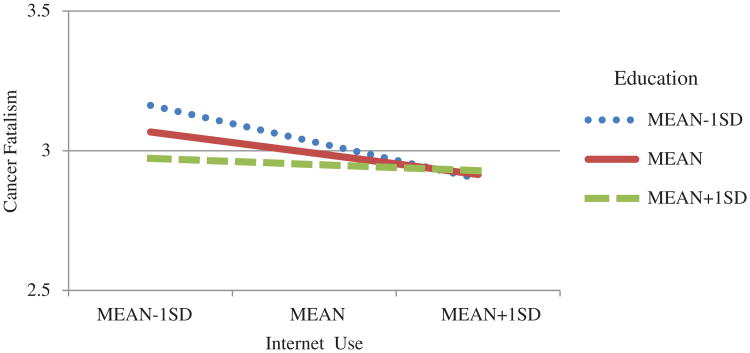
Next, we tested whether education moderated the effect of Internet use for health information on fatalistic beliefs about cancer prevention (see Table 1, Model 2). The effect of Internet use on cancer fatalism was substantially stronger among less educated than more educated respondents (interaction term β = .06, p < .05). To gain a clearer understanding of the interaction, OLS regression model parameter estimates (i.e., unstandardized regression coefficients after controlling for all confounders) were used to predict fatalistic beliefs about cancer prevention by education and Internet use for health information (see Figure 1). According to the recommendations by Hayes & Matthes (2009), we computed the effects of Wave 1 Internet use on Wave 2 cancer fatalism at one standard deviation below the mean years of education, at the mean years of education, and at 1 standard deviation above the mean years of education. A negative relationship between Internet use at Wave 1 and cancer fatalism at Wave 2 was apparent only among respondents with the average or lower than the average level of education. Among respondents with above-average levels of education, the relationship between Internet use and cancer fatalism was generally flat.
Figure 1.
Relationships between Internet use and education at Wave 1 and cancer fatalism at Wave 2. To show the interactive effect of Internet use and education, we assigned mean values to all the continuous control variables that were not used in constructing the interaction term. This figure shows White, married, employed, nonsmoking males, who have not had cancer but know someone with cancer. Cancer fatalism was measured on a 5-point scale (1 = “strongly disagree” to 5 = “strongly agree”).
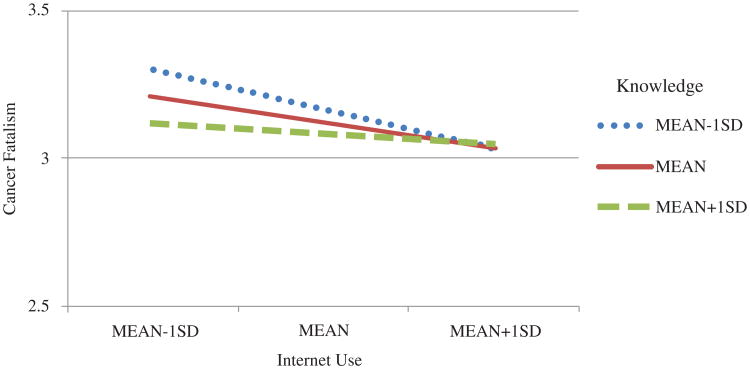
Model 3 in Table 1 reveals the same pattern of interaction between Internet use and health knowledge. The relationship between Internet use and cancer fatalism was substantially stronger among individuals with the average and lower than the average levels of health knowledge (interaction term β = .05, p < .05). Following the same procedure with education, we convey the form of the moderating effect of health knowledge in Figure 2. A negative relationship between Internet use at Wave 1 and cancer fatalism at Wave 2 was apparent only among those with the average or lower than the average level of health knowledge. Respondents with high levels of health knowledge did not appear to reduce their fatalistic beliefs about cancer prevention with increased health-related Internet use.
Figure 2.
Relationships between Internet use and health knowledge at Wave 1 and cancer fatalism at Wave 2. To show the interactive effect of Internet use and health knowledge, we assigned mean values to all the continuous control variables that were not used in constructing the interaction term. This figure shows White, married, employed, nonsmoking males, who have not had cancer but know someone with cancer. Cancer fatalism was measured on a 5-point scale (1 = “strongly disagree” to 5 = “strongly agree”).
Discussion
Study findings are consistent with the argument that Internet use to acquire health information has potential to reduce fatalistic beliefs about cancer prevention among some subsets of the population. Evidence consistent with beneficial effects of the Internet on cancer fatalism was only apparent among those with the average or lower than the average levels of education and health knowledge. Considering that cancer fatalism is associated with negative cognitive and behavioral consequences, this finding shows potential for the Internet as a valuable health communication channel for low-SES groups.
Notably, there is no evidence that this result occurred because respondents with high education and health knowledge had reached the lower bound of our measure of cancer fatalism (a score of “1” indicating strong disagreement with all three items). As Figures 1 and 2 show, cancer fatalism ranged from 2.9 to 3.2 among those with high education and health knowledge, values which are not close to the lower bound of the measure. We note, however, that health-related Internet use did not decrease cancer fatalism among highly educated and health-knowledgeable people. This suggests that the incremental effect of health-related information obtained via the Internet on cancer fatalism may decrease at higher levels of exposure. It may be that there is a particular threshold of health knowledge at which cancer fatalism will not decrease further. Alternatively, it may take longer time for health-related Internet use to reduce cancer fatalism of those with high levels of education and health knowledge. Thus, the time lag that we adopted in this study (i.e., 1 year) might not have been long enough to fully capture Internet effects on highly educated and health-knowledgeable populations.
Study limitations: Measurement
Several study limitations are worth noting before moving to a larger discussion of the study's implications. Most notably, measurement reliability for several variables (cancer fatalism, Internet use for health information, and health knowledge) was low by traditional standards. The low Cronbach's alpha for cancer fatalism, while observed in previous studies, suggests that “cancer fatalism” as described here may have multiple correlated but distinct dimensions. While our results were similar when examining each of these items separately, and each item predicts unhealthy behaviors, one recent study differentiated the items that comprise our cancer fatalism measure into three distinct constructs: confusion, fatalism, and overload (Jensen, Brown, Lynam, Jones, & Christy, 2010). Better measurement of these constructs may yield new insights into the role of the Internet in shaping specific types of cancer prevention beliefs.
Our measure of Internet use for health information is similarly limited in both its scope (two items) and characterization of the current (and future) online information environment. While the two items we measured were highly correlated and likely reflect important dimensions of health information exposure via the Internet, it is likely that they did not capture other important aspects of health-related exposure online. For instance, social network sites have rapidly proliferated in recent years. We suspect that many people acquire (purposefully or not) health-related information through these channels. This could include links to traditional health information, news stories, or even casual information about the health and well-being of people in one's social network. Do people catalog this type of information as health-related information, and would they report it as such on a survey? Different types of information acquisition may have different direction and magnitude of impact on cancer-related beliefs and behaviors.
Health knowledge is also an imperfect proxy measure for health literacy, gauging only one dimension of the concept (Berkman et al., 2010). Although many scholars have long noted the importance of health literacy and health knowledge in media effects on health outcomes (Viswanath & Emmons, 2006), there has not been a widely shared definition of what they are, nor is their operationalization well-established. Further work is clearly needed to clarify what it means to be fatalistic about cancer prevention, to use the Internet for health-related information, and to have health knowledge, as well as how to measure these constructs in practice.
Study limitations: Population and survey
Although we recognize that cancer fatalism disparities by race/ethnicity are important from both ethical (justice and fairness) and practical points of view (identifying and reaching historically underserved populations who suffer a disproportionate high disease burden from cancer), race and ethnicity were not associated with cancer fatalism. A failure to detect associations between race/ethnicity and cancer fatalism is also consistent with other studies using nationally representative survey data (Lee & Niederdeppe, 2011; Niederdeppe & Gurmankin Levy, 2007; Niederdeppe et al., 2010). In fact, only a group of studies using samples from small geographic locations has reported that fatalistic beliefs about cancer prevention are more prevalent among African Americans and Hispanics than Whites. Also, observed racial and ethnic differences in fatalistic beliefs about cancer prevention may be at least partially attributable to differences in SES, which we would have captured here (Freeman, 1991).
These data were collected on the Internet and the response rate for the sample is fairly low (Wave 1 16%, Wave 2 12%). However, we believe these particular limitations are not critically problematic for the following reasons. First, when we compared the distributions of some important sociodemographic variables (i.e., age, gender, education, income, race/ethnicity, census region) of the unweighted sample with those of the CPS data (which aims to be nationally representative and does not require Internet access), there were no significant differences. Second, we developed poststratification weights using the data from the CPS and poststratified all the results to adjust for under- or overrepresentation of certain segments of the population in our sample. It is nevertheless possible that weighted results may not perfectly represent the U.S. population, because we may have omitted some important variables in creating the poststratification weights. Third, although the sample was recruited through RDD, all respondents were given access to the Internet to be able to participate in the KN panel. This was likely to increase the proportion of the sample that uses the Internet for health information relative to a sample of nonpanel participants. This would not explain, however, why high and low Internet users show different levels of cancer fatalism by levels of education and health knowledge. Fourth, there were virtually no differences in terms of education and income between Wave 1 and Wave 2 samples even before we put on poststratification weights. Thus, the attrition rates between the two waves were not different by SES. Even if attribution rates might have varied according to SES, poststratification weights would have corrected for this.
Implications for future research
The use of a nationally representative sample of adults aged 40–70 allows us to consider both the magnitude of the effect per exposure (as captured by standardized coefficients) and the magnitude of that exposure at the population level (as captured by the proportion of the population using the Internet for health information). In light of the large proportion of adults who currently use the Internet for health information, a number which is likely to increase over time, favorable effects of health-related Internet use on cancer fatalism among lower SES adults appear practically significant even if small by traditional effect size standards.
The current research underscores the need to better understand relationships between unique characteristics of specific media channels (like the Internet) and cancer prevention beliefs. In light of previous findings by Lee & Niederdeppe (2011) and Niederdeppe et al. (2010) about the role of local television in increasing cancer fatalism, the current study's results suggest that the Internet may play a different role than traditional mass media. This study was unable to test why this may have been the case, but numerous explanations are plausible. For instance, functional characteristics of the Internet, like interactivity and user control, may facilitate active information acquisition and assimilation among socioeconomically disadvantaged groups (Gustafson et al., 2008; Lowrey & Kim, 2009). Internet use might make people feel like active agents of change because they are required to engage with the Internet more actively than with other passive media, such as television (Bonfadelli, 2002; DiMaggio et al., 2004). This heightened sense of agency and control could transfer to other domains to increase proactive attitudes toward health and thus reduce cancer fatalism. Internet use might reduce cancer fatalism through cancer-related social norms by conveying a sense that many people are actively involved in cancer prevention, thereby believing that cancer is preventable by adopting some effective measures (Lapinski & Rimal, 2006). Easy accessibility to content from trustworthy sources like the National Cancer Institute (NCI) or American Cancer Society (ACS) could reduce the likelihood of developing fatalistic beliefs by providing clear recommendations about effective preventive behaviors.
These speculative explanations invite future research to test ways that Internet use for health information may influence cancer fatalism, particularly among low-SES groups. Survey designs are well suited for testing relationships at the population level, as we have done here, but may be less useful for identifying mechanisms that explain these relationships. Lab experimental designs that manipulate and assess the possible mediating effects of these or other qualities of the Internet offer one promising approach; in-depth interviews to learn how low-SES populations use the Internet for health-related information and make sense of these issues offer another.
Concluding remarks and caveats
Reducing health disparities is among the nation's top health priorities (U.S. Department of Health and Human Services, 2012). The Internet is likely to play an increasingly important role as a source of cancer-related information. It is thus theoretically and practically important to better understand how people's use of the Internet to acquire health information may influence their beliefs about ways to prevent cancer. Our findings are consistent with the notion that the Internet has potential to empower less educated individuals by reducing their cancer fatalism. However, this study represents only a first step in developing a better understanding of the promises (and potential pitfalls) of the Internet for low-SES groups. We hope this study spurs additional research to better understand these important public health issues.
Acknowledgments
This study was supported under a grant from the NCI Center of Excellence in Cancer Communication (CECCR) at the University of Pennsylvania (P50 CA101404). We thank Malcolm Parks and three anonymous reviewers for their insightful comments on earlier versions of this article.
Footnotes
We examined whether there were any statistically significant differences in terms of the descriptive statistics of our key variables between Wave 1 and Wave 2 data. The only significant difference was for health knowledge. However, this difference disappeared when we looked at only the respondents who were included in our tests of hypotheses.
Weighted descriptive statistics are presented throughout this article. As such, standard errors (rather than standard deviations) are the appropriate measure of population-level variation around a parameter estimate.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Benigeri M, Pluye P. Shortcomings of health information on the Internet. Health Promotion International. 2003;18:381–386. doi: 10.1093/heapro/dag409. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Davis TC, McCormack L. Health literacy: What is it? Journal of Health Communication. 2010;15:9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- Berland GK, Elliott MN, Morales LS, Algazy JI, Kravitz RL, Broder MS, et al. Health information on the Internet: Accessibility, quality, and readability in English and Spanish. Journal of the American Medical Association. 2001;285:2612–2621. doi: 10.1001/jama.285.20.2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonfadelli H. The Internet and knowledge gaps: A theoretical and empirical investigation. European Journal of Communication. 2002;17:65–84. doi: 10.1177/0267323102017001607. [DOI] [Google Scholar]
- Briñol P, Petty RE. Fundamental processes leading to attitude change: Implications for cancer prevention communications. Journal of Communication. 2006;56:S81–S104. doi: 10.1111/j.1460-2466.2006.00284.x. [DOI] [Google Scholar]
- Campbell SW, Kwak N. Mobile communication and civil society: Linking patterns and places of use to engagement with others in public. Human Communication Research. 2011;37:207–222. doi: 10.1111/j.1468-2958.2010.01399.x. [DOI] [Google Scholar]
- DiMaggio P, Hargittai E, Celeste C, Shafer S. From unequal access to differentiated use: A literature review and agenda for research on digital inequality. In: Neckerman K, editor. Social inequality. New York, NY: Russell Sage Foundation; 2004. pp. 355–400. [Google Scholar]
- Eagly AH, Chaiken S. The psychology of attitude. Belmont, CA: Wadsworth; 1993. [Google Scholar]
- Eveland WP, Dunwoody S. User control and structural isomorphism or disorientation and cognitive load? Communication Research. 2001;28:48–78. doi: 10.1177/009365001028001002. [DOI] [Google Scholar]
- Eveland WP, Marton K, Seo M. Moving beyond “just the facts”: The influence of online news on the content and structure of public affairs knowledge. Communication Research. 2004;31:82–108. doi: 10.1177/0093650203260203. [DOI] [Google Scholar]
- Eysenbach G, Powell J, Kuss O, Sa E. Empirical studies assessing the quality of health information for consumers on the World Wide Web: A systematic review. Journal of the American Medical Association. 2002;287:2691–2700. doi: 10.1001/jama.287.20.2691. [DOI] [PubMed] [Google Scholar]
- Finkel SE. Causal analysis with panel data. Thousand Oaks, CA: Sage; 1995. (Sage University Paper Series on Quantitative Applications in the Social Sciences, 07 – 105). [Google Scholar]
- Freeman HP. Race, poverty, and cancer. Journal of the National Cancer Institute. 1991;83:526–527. doi: 10.1093/jnci/83.8.526. [DOI] [PubMed] [Google Scholar]
- Gansler T, Henley SJ, Stein K, Nehl EJ, Smigal C, Slaughter E. Sociodemographic determinants of cancer treatment health literacy. Cancer. 2005;104:653–660. doi: 10.1002/cncr.21194. [DOI] [PubMed] [Google Scholar]
- Gaziano C. Forecast 2000: Widening knowledge gap. Journalism & Mass Communication Quarterly. 1997;74:237–264. doi: 10.1177/107769909707400202. [DOI] [Google Scholar]
- Griffin RJ, Dunwoody S, Neuwirth K. Proposed model of the relationship of risk information seeking and processing to the development of preventive behaviors. Environmental Research. 1999;80:S230–S245. doi: 10.1006/enrs.1998.3940. [DOI] [PubMed] [Google Scholar]
- Gustafson DH, Hawkins R, McTavish F, Pingree S, Chen WC, Volrathongchai K, et al. Internet-based interactive support for cancer patients: Are integrated systems better? Journal of Communication. 2008;58:238–257. doi: 10.1111/j.1460-2466.2008.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior Research Methods. 2009;41:924–936. doi: 10.3758/brm.41.3.924. [DOI] [PubMed] [Google Scholar]
- Hungerford DS. Internet access produces misinformed patients: Managing the confusion. Orthopedics. 2009;32:658. doi: 10.3928/01477447-20090728-04. [DOI] [PubMed] [Google Scholar]
- Jensen JD, Brown N, Lynam C, Jones C, Christy K. Are cancer fatalism and cancer information overload unique constructs?; Poster presented at the International Breast Cancer and Nutrition Conference in West Lafayette, IN; 2010, October 9–11.2010. [Google Scholar]
- Jensen JD, Carcioppolo N, King AJ, Bernat JK, Davis LA, Yale R, Smith J. Including limitations in news coverage of cancer research: Effects of news hedging on fatalism, medical skepticism, patient trust, and backlash. Journal of Health Communication. 2011;16:486–503. doi: 10.1080/10810730.2010.546491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Stout PA. The effects of interactivity on information processing and attitude change: Implications for mental health stigma. Health Communication. 2010;25:142–154. doi: 10.1080/10410230903544936. [DOI] [PubMed] [Google Scholar]
- Kreps GL, Gustafson D, Salovey P, Perocchia RS, Wilbright W, Bright MA, et al. The NCI Digital Divide Pilot Projects: Implications for cancer education. Journal of Cancer Education. 2007;22:S56–S60. doi: 10.1080/08858190701348414. [DOI] [PubMed] [Google Scholar]
- Lapinski MK, Rimal RN. An explication of social norms. Communication Theory. 2006;15:127–147. doi: 10.1111/j.1468-2885.2005.tb00329.x. [DOI] [Google Scholar]
- Lee CJ. The role of Internet engagement in the health-knowledge gap. Journal of Broadcasting & Electronic Media. 2009;53:365–382. doi: 10.1080/08838150903102758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CJ, Niederdeppe J. Genre-specific cultivation effects: Lagged associations between overall TV viewing, local TV news viewing, and fatalistic beliefs about cancer prevention. Communication Research. 2011;38:731–753. doi: 10.1177/0093650210384990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowrey W, Kim S. Online news media and advanced learning: A test of cognitive flexibility theory. Journal of Broadcasting & Electronic Media. 2009;53:547–566. doi: 10.1080/08838150903323388. [DOI] [Google Scholar]
- Niederdeppe J, Gurmankin Levy A. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiology, Biomarkers & Prevention. 2007;16:998–1003. doi: 10.1158/1055-9965.epi-06-0608. [DOI] [PubMed] [Google Scholar]
- Niederdeppe J, Fowler EF, Goldstein K, Pribble J. Does local television news coverage cultivate fatalistic beliefs about cancer prevention? Journal of Communication. 2010;60:230–253. doi: 10.1111/j.1460-2466.2009.01474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powe BD, Finnie R. Cancer fatalism: The state of the science. Cancer Nursing. 2003;26:454–467. doi: 10.1097/00002820-200312000-00005. Retrieved from http://journals.lww.com/cancernursingonline. [DOI] [PubMed] [Google Scholar]
- Radmanadhan S, Viswanath K. Health and the information nonseeker: A profile. Health Communication. 2006;20:131–139. doi: 10.1207/s15327027hc2002_4. [DOI] [PubMed] [Google Scholar]
- Radosevich DM, Partin MR, Nugent S, Nelson D, Flood AB, Holtzman J, et al. Measuring patient knowledge of the risks and benefits of prostate cancer screening. Patient Education and Counseling. 2004;54:143–152. doi: 10.1016/S0738-3991(03)00207-6. [DOI] [PubMed] [Google Scholar]
- Romantan A, Hornik R, Price V, Cappella J, Viswanath K. A comparative analysis of the performance of alternate measures of exposure. Communication Methods and Measures. 2008;2:80–99. doi: 10.1080/19312450802062539. [DOI] [Google Scholar]
- Selwyn N. Reconsidering political and popular understanding of the digital divide. New Media and Society. 2004;6:341–362. doi: 10.1177/1461444804042519. [DOI] [Google Scholar]
- Shim M, Kelly B, Hornik R. Cancer information scanning and seeking behaviour is associated with knowledge, lifestyle choices, and screening. Journal of Health Communication. 2006;11:S157–S172. doi: 10.1080/10810730600637475. [DOI] [PubMed] [Google Scholar]
- Slater MD. Operationalizing and analyzing exposure: The foundation of media effects research. Journalism & Mass Communication Quarterly. 2004;81:168–183. doi: 10.1177/107769900408100112. [DOI] [Google Scholar]
- Slater MD, Hayes AF, Reineke JB, Long M, Bettinghaus EP. Newspaper coverage of cancer prevention: Multilevel evidence for knowledge-gap effects. Journal of Communication. 2009;59:514–533. doi: 10.1111/j.1460-2466.2009.01433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tichenor PJ, Donohue GA, Olien CN. Mass media flow and differential growth in knowledge. Public Opinion Quarterly. 1970;34:159–170. doi: 10.1086/267786. [DOI] [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Healthy People 2020. Washington, DC: USDHHS; 2012. Retrieved from http://www.healthypeople.gov/2020/default.aspx. [Google Scholar]
- Viswanath K, Emmons KM. Message effects and social determinants of health: Its application to cancer disparities. Journal of Communication. 2006;56:S238–S264. doi: 10.1111/j.1460-2466.2006.00292.x. [DOI] [Google Scholar]
- Viswanath K, Kreuter MW. Health disparities, communication inequalities, and e-health: A commentary. American Journal of Preventive Medicine. 2007;32:S131–S133. doi: 10.1016/j.amepre.2007.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]