Abstract
Aim of the study
We determined the expression of beclin-1 in gallbladder carcinoma, analyzed the association of beclin-1 expression with clinicopathologic parameters and prognosis, and investigated the relationship between microvessel density and beclin-1 expression.
Material and methods
Tissue microarray blocks containing 118 primary gallbladder tumor sites were used. Clinical parameters and prognostic data were collected. Expression of beclin-1 in these specimens was analyzed by immunohistochemical studies and confirmed by Western blotting. Microvessel density was counted using immunohistochemical staining.
Results
The overall rate of over-expression of beclin-1 was 68.1% (80 of 118). Over-expression of beclin-1 was significantly associated with TNM stage and liver metastasis. Over-expression of beclin-1 has no significant relationship with age, sex, lymphatic metastasis, or tumor differentiation. Based on the Kaplan-Meier method, over-expression of beclin-1 showed no significant difference for the overall survival rate in patients with gallbladder cancer. The multivariate Cox regression analysis demonstrated that beclin-1 was not an independent prognostic factor for gallbladder cancer.
Conclusions
Beclin-1 might play roles in the development of gallbladder cancer. However, beclin-1 may not be an effective prognostic factor for gallbladder cancer.
Keywords: autophagy, beclin-1, angiogenesis, gallbladder cancer
Introduction
Autophagy is a ubiquitous process conserved among all eukaryotes ranging from yeast to mammals [1]. Autophagy is considered to be involved in programmed cell death and plays roles in tumorigenesis and tumor progression [2]. In recent years, autophagy has been attracting increasing attention and it is becoming an important area in tumor research. Accumulated evidence suggests that autophagic activity is related to occurrence and development of several tumors, such as hepatocellular carcinoma, cervical squamous carcinoma, esophageal squamous carcinoma and colon carcinoma [3–6]. Therefore, autophagy has been regarded as a potential cancer-promoting factor [7–9].
In 1998, Liang identified a novel 60-KDa coiled-coil protein, beclin-1, which was confirmed to interact with Bcl-2 in mammalian cells, using fluorescence resonance energy transfer microscopy [10]. Beclin-1 was the first identified mammalian gene with a role in mediating autophagy [11]. The complete cDNA sequence of beclin-1 encodes a 2098-bp transcript, with a 120-bp 5′ UTR, 1353-bp coding region, and 625-bp 3′ UTR. Hybridization screening of a human genomic PAC library identified PAC 452O8, which contains the complete beclin-1 gene [12]. Beclin-1 is mapped to a region approximately 150 kb centromeric to BRCA1 on chromosome 17q21 that is commonly deleted in breast, ovary, and prostate cancer [5]. Beclin-1 has been considered as an autophagy-related protein and tumor suppressor gene [13, 14].
Carcinoma of the gallbladder accounts for 1.5% of digestive tract tumors and is the fifth common gastrointestinal tract cancer [15]. Gallbladder carcinoma was considered as a disease with poor prognosis, for it usually was diagnosed at an advanced stage when metastases had formed [16, 17]. A previous study indicated that autophagy protein may play a role in regulating carcinoma growth, especially in the early stage of tumorigenesis [18]. Autophagy also affects angiogenesis, because it serves as a response to stress when limited angiogenesis leads to nutrient deprivation and hypoxia [2]. Evaluation of angiogenesis by measurement of microvessel density (MVD) is a useful parameter for estimating gallbladder cancer metastatic risk [19, 20], but its relationship with autophagy is unknown. In the study described herein, we evaluated the expression of beclin-1 in gallbladder carcinoma, analyzed the association of beclin-1 expression with clinicopathologic parameters and prognosis, and investigated the relationship between MVD and beclin-1 expression.
Material and methods
Patient specimens and tissue microarray blocks
Tissue samples from 118 patients with gallbladder carcinoma who underwent curative surgery at the Sixth People's Hospital in Shanghai, People's Republic of China, from 2004 to 2007, were enrolled in this study. Hematoxylin and eosin-stained sections of these blocks were prepared and reviewed by two pathologists to ensure the quality of tissue blocks. Twenty clinically normal adjacent specimens were also collected from parts of these patients. The patients’ medical records were reviewed to obtain data including age at diagnosis, sex, liver metastasis, lymph metastasis, and American Joint Committee on Cancer stage (AJCC). Mean age of patients at tumor resection was 63.7 years; 42 (36%) were male and 76 (64%) were female. Clinical and pathological records of all patients in the study were reviewed periodically. According to place of birth, the patients were classified as being either from (n = 72) or not from (n = = 46) the Shanghai area. Clinical follow-up results were available only for the patients from the Shanghai area [mean follow-up duration, 18.26 months (range, 1–67.3 months)]. The tissue microarray consisted of 118 primary tumor sites, in which 20 sites had one 1.5-mm core of non-neoplastic mucosal tissue and one 1.5-mm core of primary tumor tissue. Patient characteristics are listed in Table 1. Experiments were performed in compliance with the Chinese laws and guidelines concerning the patients’ informed consent. The use of the human specimens was approved by the Sixth People's Hospital Institutional Review Board.
Table 1.
Correlation between beclin-1/MVD and various clinicopathological features
| Variables | n | Beclin-1 (+) | p | MVD | p |
|---|---|---|---|---|---|
| Age (years) | |||||
| < 60 | 42 | 24 | 0.066 | 56.19 ±1.81 | 0.216 |
| ≥ 60 | 76 | 56 | 50.92 ±2.05 | ||
| Sex | |||||
| Male | 42 | 26 | 0.309 | 54.57 ±1.83 | 0.419 |
| female | 76 | 54 | 51.82 ±2.07 | ||
| Differentiation | |||||
| good | 46 | 28 | 0.373 | 57.17 ±2.86 | 0.082 |
| Moderate | 40 | 30 | 54.65 ±3.24 | ||
| Poor | 32 | 32 | 44.19 ±2.92 | ||
| Liver metastasis | |||||
| Positive | 26 | 22 | 0.038 | 74.15 ±1.15 | 0.000 |
| Negative | 92 | 58 | 46.76 ±1.72 | ||
| Lymphatic metastasis | |||||
| Positive | 54 | 40 | 0.180 | 57.89 ±1.85 | 0.063 |
| Negative | 64 | 40 | 48.50 ±2.00 | ||
| TNM stage | |||||
| 0 | 12 | 8 | 0.000 | 43.67 ±1.73 | 0.000 |
| I | 16 | 2 | 32.25 ±1.15 | ||
| II | 42 | 32 | 51.19 ±1.86 | ||
| III | 14 | 10 | 44.86 ±1.04 | ||
| IV | 34 | 28 | 70.94 ±1.28 |
Immunohistochemistry
Tissue sections were deparaffinized in xylene, and then rehydrated in graded concentrations of ethyl alcohol (100%, 95%, 75%, then water). Tissue microarray sections were microwave-treated twice in citrate buffer (PH 6.0) at 99°C for 6 min. The sections were placed in 3% H2 O2 for 10 min to inhibit endogenous peroxide activity, washed three times with phosphate-buffered saline (PBS) buffer for 5 min and placed in normal mouse serum as blocking antibody at room temperature for 10 min. The sections were evaluated by antibody for beclin-1 (1: 80 dilution; Abcam, Cambridge, UK) and CD34 (1: 100 dilution; Dako Cytomation, Glostrup, Denmark). After incubation at 4°C for 24 h, sections were washed three times with PBS buffer for 10 min. Biotinylated anti-mouse/rabbit immunoglobulin was used as the second antibody. 3,3-Diaminobenzidine tetrahydrochloride (DAB) was used as a chromogen. The sections were counter-stained with hematoxylin. All slices were evaluated without knowledge of the clinical outcome. Beclin-1 and CD34 protein expression in the 118 cases was evaluated by two individuals (Y.C. and H.D.) under an Olympus CX31 microscope (Olympus, Center Valley, PA). Staining was scored independently by the two individuals who were blinded to each other's findings.
Evaluation of immunohistochemical staining
Evaluation of beclin-1 staining was performed as suggested by Kyu et al. The expression of beclin-1 was determined by immunohistochemical staining, which appeared as fine granular and diffuse cytoplasmic staining with occasional nuclear staining. Immunohistochemical staining for beclin-1 was evaluated according to intensity and proportion. The intensity score was determined as 0 (no staining), 1 (weak staining), 2 (moderate staining), and 3 (strong staining). The proportion score was determined as 1 (30% of tumor cells) and 2 (30% of tumor cells). The intensity score and proportion score were multiplied together for a total score. Total scores were as follows: 0 to 1 (under-expression) and 2 to 6 (over-expression) [21].
Qualification of microvessel density
Quantification of angiogenesis, using microvessel density (MVD) as a parameter, is considered to be a valuable prognostic indicator of gallbladder cancer aggressiveness.[20] Determination of MVD (assessed by immunostaining for CD34) was performed as suggested by Weidner in ref. [22]. After scanning the immunostained section at low magnification, the area of tissue with the highest density of microvessels (hot spots) was selected. Hot spots were determined by two independent investigators (Song Yu and Xiaohu Wang), who were blinded to patients’ clinical parameters. Microvessels were counted in three hot spots (200×), and the mean MVD was used for the later analysis (any endothelial cell or endothelial cluster close to tumor cells and connective tissue around tumor cells which stained brownish yellow were considered as a single, countable micro-vessel).
Western blot analysis
Whole-cell lysates were prepared from human gallbladder cancer and normal gallbladder tissue specimens. Standard Western blotting was done using rabbit polyclonal antibodies against human beclin-1 and an anti-rabbit IgG antibody, which was a horseradish peroxidase-linked F (ab’)2 fragment obtained from a donkey (Amersham, Arlington Height, IL, USA). Equal protein sample loading was monitored by probing the same membrane filter with an anti-β-actin antibody. The probe proteins were detected using the Amersham enhanced chemiluminescence system according to the manufacturer's instructions.
Statistical analysis
Analyses were performed using the SPSS statistical software program for Windows (SPSS Inc., Chicago, IL). Categorical data were analyzed using χ2 tests. Within-group correlations of continuous and ordinal variables were assessed using Pearson's correlation coefficient or Spearman's rank correlation coefficient when appropriate. The Kaplan-Meier method was used to estimate survival rates, and the log-rank and the Wilcoxon rank sum tests were used to assess survival duration differences among groups. In all of the tests, a two-sided p < 0.05 was considered statistically significant.
Results
Over-expression of beclin-1 in patients with gallbladder cancer
Immunostaining revealed over-expression of beclin-1 in primary tumor tissue compared with under-expression in normal gallbladder tissue (p < 0.05) (Fig. 1). The results were confirmed by Western blotting using gallbladder tumor tissues and normal gallbladder tissue (Fig. 2). The overall rate of over-expression of beclin-1 was 68.1%. We also detected that the mean MVD was 52.80 ±1.94 microvessels/field and the median MVD was 51.13 (range 20–92.3) microvessels/field. The mean MVD of gallbladder cancer was significantly higher than normal gallbladder tissue (p < 0.05).
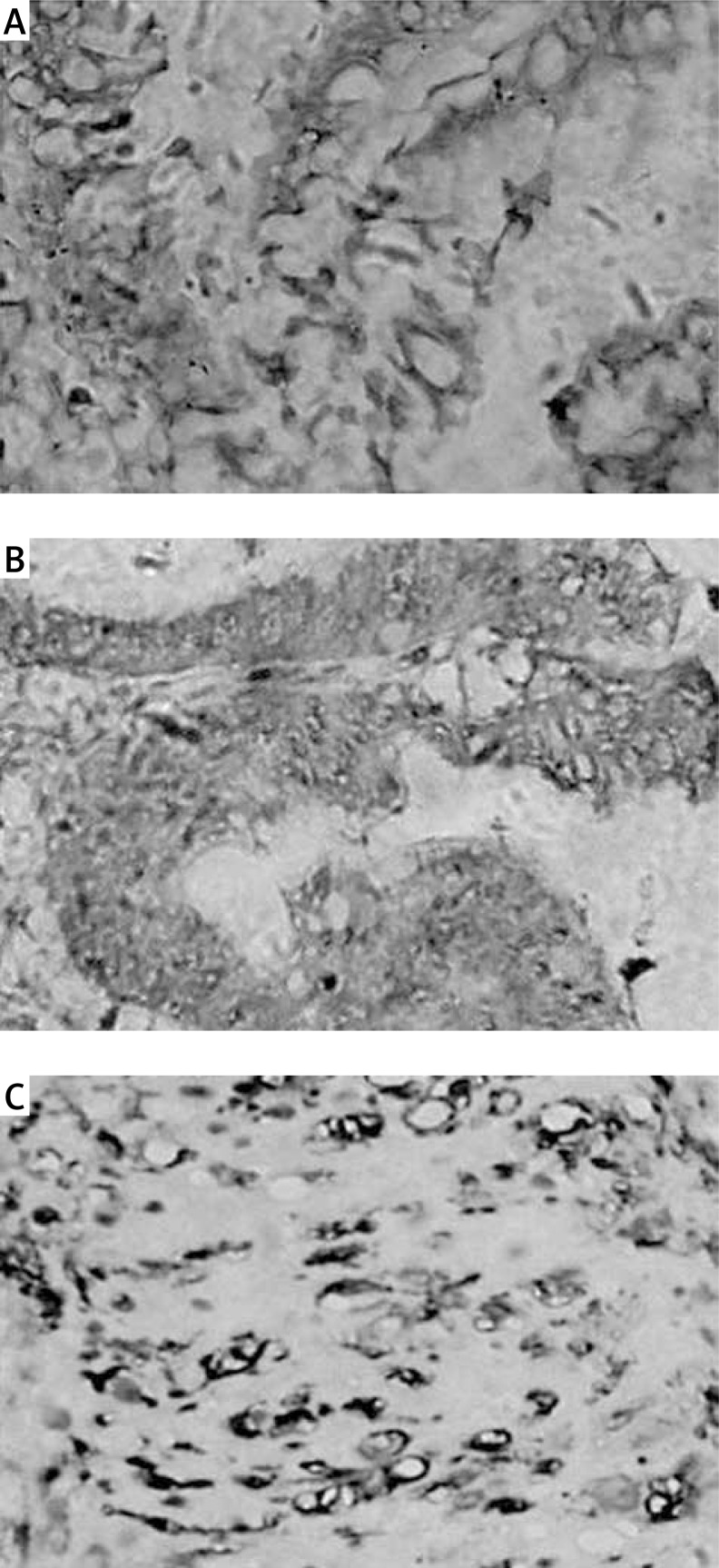
Fig. 1.
Analysis of beclin-1 and MVD in human gallbladder cancer. A) A sample of normal gallbladder tissue with under-expression of beclin-1; B) A sample of gallbladder cancer with over-expression of beclin-1; C) A sample of gallbladder cancer with high MVD. Original magnification 200×
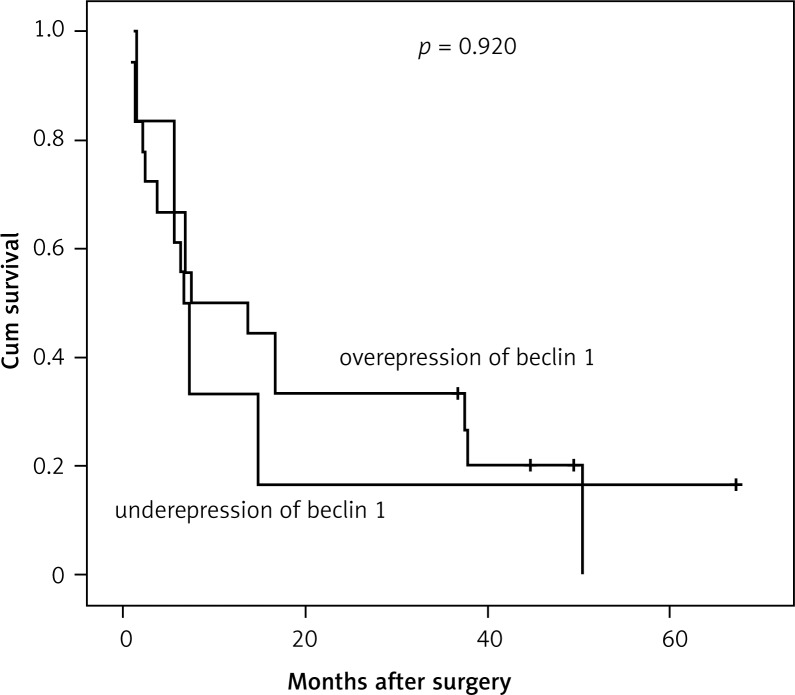
Fig. 2.
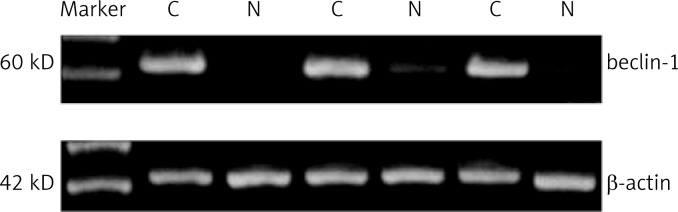
Western blot analysis of the expression of beclin-1 in normal gallbladder tissue and gallbladder cancer
Association of beclin-1 over-expression with clinicopathologic factors in patients with gastric cancer
The correlations between the over-expression of beclin-1 and clinicopathologic factors (Table 1) were analyzed. The over-expression of beclin-1 was significantly associated with TNM stage (p < 0.01) and liver metastasis (p < 0.05). The over-expression of beclin-1 showed no significant relationship with age, sex, lymphatic metastasis, or tumor differentiation. The results of our analysis also revealed that high MVD was associated with TNM stage (p < 0.01, respectively) and liver metastasis (p < 0.01).
Correlations between beclin-1 and microvessel density
We analyzed the relationship between beclin-1 and MVD expression using Spearman rank correlation analysis and the χ2 test. Spearman correlation analysis suggested a very weak relationship between beclin-1 and MVD (r = 0.296, p < 0.05). The χ2 test revealed that numerous tumor specimens with beclin-1 over-expression also had high MVD expression (p < 0.05, Table 2).
Table 2.
Correlation between beclin-1 and MVD expression in 118 cases of gallbladder cancer
| MVD | Total | P | |||
|---|---|---|---|---|---|
| negative | positive | ||||
| beclin-1 | under-expression | 26 (68.4%) | 12 (31.6%) | 38 | 0.03 |
| over-expression | 38 (47.5%) | 42 (52.5%) | 80 | ||
| total | 64 | 54 | 118 | ||
Survival analysis
The cohort consisted of 27 male (37.5%) and 45 female (62.5%) patients with a median age of 62.7 years (range 36–84 years). The median cumulative survival duration in patients with resection of gallbladder carcinoma was 7.35 months. Over-expression of beclin-1 showed no significant difference for the overall survival rate in patients with gallbladder cancer (p = 0.920, Fig. 3). Beclin-1 expression was not determined as an independent prognostic factor for gallbladder cancer (Table 3).
Fig. 3.
Kaplan-Meier curves of survival durations in patients with gallbladder cancer treated with curative surgery (p = 0.920)
Table 3.
Multivariate survival analysis: Cox proportional hazard analysis of 72 cases of gallbladder cancer
| Parameter | B | SE | Wald | Sig. | Exp(B) | 95.0% CI for Exp(B) | |
|---|---|---|---|---|---|---|---|
| lower | upper | ||||||
| age | 0.677 | 0.464 | 2.127 | 0.145 | 1.968 | 0.792 | 4.890 |
| sex | 0.311 | 0.396 | 0.616 | 0.433 | 1.364 | 0.628 | 2.963 |
| differentiation | –0.140 | 0.241 | 0.340 | 0.560 | 0.869 | 0.542 | 1.393 |
| liver metastasis | –0.750 | 0.533 | 1.981 | 0.159 | 0.472 | 0.166 | 1.342 |
| lymph metastasis | –0.072 | 0.422 | 0.029 | 0.864 | 0.930 | 0.407 | 2.125 |
| TNM stage | 0.670 | 0.255 | 6.876 | 0.009 | 1.954 | 1.184 | 3.224 |
| beclin-1 | –0.629 | 0.466 | 1.823 | 0.177 | 0.533 | 0.214 | 1.328 |
Discussion
Autophagy is a catabolic process in which cytosol and organelles are sequestered within double-membrane vesicles that deliver the contents to the lysosome/vacuole for degradation and recycling of the resulting macromolecules [1]. Additionally, autophagy may play a critical role in the cellular response to stress such as nutrient limitation, and be involved in various development pathways and functions in tumor suppression [1, 14]. Accumulating evidence favors the ideal that autophagy can promote tumor development and protect tumor cells from cell death stimuli. Chang et al. stated that beclin-1, an autophagy-related protein, may play a role in both colorectal and gastric tumorigenesis [23]. Chen et al. found that beclin-1 protein correlated with the progression of human esophageal squamous cell carcinoma [3]. Miracco et al. showed that beclin-1 expression is related to the aggressiveness of brain tumor [24]. However, there are some different opinions, according to which autophagy can suppress tumor development. Kyu et al. suggest that beclin-1 might play a role in the inhibition of the development of breast cancer and that inhibition might be due to an interaction with bcl-2 protein [21]. So, more studies on different cancers will be necessary to analyze the relationship between autophagy and tumors.
In the present study, we detected expression of beclin-1 in gallbladder cancer cases for the first time. We found, compared with the expression in normal gallbladder tissue, that beclin-1 was over-expressed in primary tumor tissue. Moreover, the over-expression of beclin-1 in gallbladder cancer was significantly associated with TNM stage and liver metastasis. These findings may suggest that beclin-1 plays an important role in development and progression of gallbladder cancer. However, we did not find any correlation between beclin-1 expression and cumulative survival. Moreover, multivariate Cox regression analysis demonstrated that beclin-1 expression was not an independent prognostic factor for gallbladder cancer. All of those data may indicate that over-expression of beclin-1 is an important event in gallbladder tumorigenesis, but it is not a valuable prognostic factor.
The process of forming new blood vessels from existing vascular networks known as angiogenesis is a crucial event which is essential for growth and persistence of tumors and their metastases [25–27]. A number of tumor therapeutic strategies are being developed to inhibit pathological angiogenesis [28]. The relationship between autophagy and angiogenesis is a new hot topic. It was considered that autophagy keeps tumor cells alive when limited angiogenesis leads to nutrient deprivation and hypoxia [2]. Sundaram et al. found that when the increase in beclin-1 levels was suppressed by shRNA, endothelial cells activated the caspase-dependent intrinsic pathway of programmed cell death [29]. To our knowledge, there have been no reports on the association between MVD and beclin-1 expression. We observed a weak relationship between beclin-1 and MVD. Most gallbladder tumors with beclin-1 over-expression also had high MVD expression in these specimens. Then, we guess, in gallbladder cancer, that beclin-1 protein might contribute to angiogenesis, which supports tumor cells in the poor nutrition or hypoxic environment.
In conclusion, we have characterized the expression of beclin-1 in human gallbladder cancer and found a weak relationship between beclin-1 and angiogenesis. Our study suggests that beclin-1 might play a role in the development of gallbladder cancer. But we also observed that beclin-1 may not be a suitable prognostic factor for gallbladder cancer. A further study on a larger scale will be necessary to clarity the prognostic value of beclin-1 in the process of tumorigenesis and the relationship between beclin-1 and angiogenesis.
The authors declare no conflict of interest.
References
- 1.Klionsky DJ. The molecular machinery of autophagy: unanswered questions. J Cell Sci. 2005;118:7–18. doi: 10.1242/jcs.01620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jaskólski D, Papierz T, Liberski PP, Sikorska B. Ultrastructure of meningiomas: autophagy is involved in the pathogenesis of “intranuclear vacuoles”. Folia Neuropathol. 2012;50:187–93. [PubMed] [Google Scholar]
- 3.Chen Y, Lu Y, Lu C. Beclin-1 expression is a predictor of clinical outcome in patients with esophageal squamous cell carcinoma and correlated to hypoxia-inducible factor (HIF)-1alpha expression. Pathol Oncol Res. 2009;15:487–93. doi: 10.1007/s12253-008-9143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi YH, Ding ZB, Zhou J, Qiu SJ, Fan J. Prognostic significance of Beclin 1-dependent apoptotic activity in hepatocellular carcinoma. Autophagy. 2009;5:380–82. doi: 10.4161/auto.5.3.7658. [DOI] [PubMed] [Google Scholar]
- 5.Kondo Y, Kondo S. Autophagy and cancer therapy. Autophagy. 2006;2:85–90. doi: 10.4161/auto.2.2.2463. [DOI] [PubMed] [Google Scholar]
- 6.Wang ZH, Peng ZL, Duan ZL, Liu H. Expression and clinical significance of autophagy gene Beclin 1 in cervical squamous cell carcinoma. Sichuan Da Xue Xue Bao Yi Xue Ban. 2006;37:860–3. [PubMed] [Google Scholar]
- 7.Baehrecke EH. Autophagy: dual roles in life and death? Nat Rev Mol Cell Biol. 2005;6:505–10. doi: 10.1038/nrm1666. [DOI] [PubMed] [Google Scholar]
- 8.Levine B. Cell biology: autophagy and cancer. Nature. 2007;446:745–7. doi: 10.1038/446745a. [DOI] [PubMed] [Google Scholar]
- 9.Hait WN, Jin S, Yang JM. A matter of life or death (or both): Understanding autophagy in cancer. Clin Cancer Res. 2006;12:1961–5. doi: 10.1158/1078-0432.CCR-06-0011. [DOI] [PubMed] [Google Scholar]
- 10.Liang XH, Kleeman LK, Jiang HH, Gordon G, Goldman JE, Berry G, Herman B, Levine B. Protection against fetal Sindbis virus encephalitis by Beclin, a novel Bcl-2-interacting protein. J Virol. 1998;72:8586–96. doi: 10.1128/jvi.72.11.8586-8596.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liang XH, Jackson S, Seaman M, Brown K, Kempkes B, Hibshoosh H, Levine B. Induction of autophagy and inhibition of tumorigenesis by beclin 1. Nature. 1999;40:672–76. doi: 10.1038/45257. [DOI] [PubMed] [Google Scholar]
- 12.Aita VM, Liang XH, Murty VV, et al. Cloning and genomic organization of beclin 1, a candidata tumor suppressor gene on chromosome 17q21. Genomics. 1999;59:59–65. doi: 10.1006/geno.1999.5851. [DOI] [PubMed] [Google Scholar]
- 13.Liang XH, Yu J, Brown K, Levine B. Beclin 1 contains a leucine-rich nuclear export signal that is required for its autophagy and tumor suppressor. J Cancer Res. 2001;61:3443–9. [PubMed] [Google Scholar]
- 14.Gozuacik D, Kimhi A. Autophagy as a cell death and tumor suppression mechanism. Oncogene. 2004;23:2891–906. doi: 10.1038/sj.onc.1207521. [DOI] [PubMed] [Google Scholar]
- 15.Ishikawa T, Horimi T, Shima Y, et al. Evaluation of aggressive surgical treatment for advanced carcinoma of the gallbladder. J Hepatobiliary Pancreat Surg. 2003;10:233–8. doi: 10.1007/s00534-003-0848-5. [DOI] [PubMed] [Google Scholar]
- 16.Misra S, Chaturvedi A, Misra NC, Sharma ID. Carcinoma of the gallbladder. Lancet Oncol. 2003;4:167–76. doi: 10.1016/s1470-2045(03)01021-0. [DOI] [PubMed] [Google Scholar]
- 17.Ito H, Matros E, Brooks DC, Osteen RT, Zinner MJ, Swanson RS, Ashley SW, Whang EE. Treatment outcomes associated with surgery for gallbladder cancer: a 20-year experience. J Gastrointest Surg. 2004;8:183–90. doi: 10.1016/j.gassur.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 18.Mikami T, Yanagisawa N, Baba H, Koike M, Okayasu I. Association of Bcl-2 protein expression with gallbladder carcinoma differentiation and progression and its relation to apoptosis. Cancer. 1999;85:318–25. [PubMed] [Google Scholar]
- 19.Nathanson SD. Insights into the mechanisms of lymph node metastasis. Cancer. 2003;98:413–23. doi: 10.1002/cncr.11464. [DOI] [PubMed] [Google Scholar]
- 20.Artico M, Bronzetti E, Alicino V, et al. Human gallbladder carcinoma: Role of neurotrophins, MIB-1, CD34 and CA15-3. Eur J Histochem. 2010;54:e10. doi: 10.4081/ejh.2010.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Won KY, Kim GY, Kim YW, Song JY, Lim SJ. Clinicopathologic correlation of beclin-1 and bcl-2 expression in human breast cancer. Hum Pathol. 2010;41:107–12. doi: 10.1016/j.humpath.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 22.Weidner N. Current pathologic methods for measuring intratumoral microvessel density within breast carcinoma and other solid tumors. Breast Cancer Res Treat. 1995;36:169–80. doi: 10.1007/BF00666038. [DOI] [PubMed] [Google Scholar]
- 23.Ahn CH, Jeong EG, Lee JW, Kim MS, Kim SH, Kim SS, Yoo NJ, Lee SH. Expression of beclin-1, an autophagy-related protein, in gastric and colorectal cancers. APMIS. 2007;115:1344–9. doi: 10.1111/j.1600-0463.2007.00858.x. [DOI] [PubMed] [Google Scholar]
- 24.Miracco C, Cosci E, Oliveri G, et al. Protein and mRNA expression of autophagy gene Beclin 1 in human brain tumors. Int J Oncol. 2007;30:429–36. [PubMed] [Google Scholar]
- 25.Zhou D, Cheng SQ, Ji HF, Wang JS, Xu HT, Zhang GQ, Pang D. Evaluation of protein pigment epithelium-derived factor (PEDF) and microvessel density (MVD) as prognostic indicators in breast cancer. J Cancer Res Clin Oncol. 2010;136:1719–27. doi: 10.1007/s00432-010-0830-y. [DOI] [PubMed] [Google Scholar]
- 26.Jiménez B, Volpert OV. Mechanistic insights on the inhibition of tumor angiogenesis. J Mol Med (Berl) 2001;78:663–72. doi: 10.1007/s001090000178. [DOI] [PubMed] [Google Scholar]
- 27.Giatromanolaki A, Sivridis E, Koukourakis MI. Angiogenesis in colorectal cancer: prognostic and therapeutic implications. Am J Clin Oncol. 2006;29:408–17. doi: 10.1097/01.coc.0000221317.56731.4e. [DOI] [PubMed] [Google Scholar]
- 28.Koh YJ, Kim HZ, Hwang SI, et al. Double antiangiogenic protein, DAAP, targeting VEGF-A and angiopoietins in tumor angiogenesis, metastasis, and vascular leakage. Cancer Cell. 2010;18:171–84. doi: 10.1016/j.ccr.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 29.Ramakrishnan S, Nguyen TM, Subramanian I, Kelekar A. Autophagy and angiogenesis inhibition. Autophagy. 2007;3:512–15. doi: 10.4161/auto.4734. [DOI] [PubMed] [Google Scholar]