Summary
Background
Ulnar neuropathy is the second most common peripheral nerve neuropathy after median neuropathy, with an incidence of 25 cases per 100 000 men and 19 cases per 100 000 women each year. Skipping (snapping) elbow syndrome is an uncommon cause of pain in the posterior-medial elbow area, sometimes complicated by injury of the ulnar nerve. One of the reason is the dislocation of the abnormal insertion of the medial triceps head over the medial epicondyle during flexion and extension movements. Others are: lack of the Osboune fascia leading to ulnar nerve instability and focal soft tissue tumors (fibromas, lipomas, etc). Recurrent subluxation of the nerve at the elbow results in a tractional and frictional neuritis with classical symptoms of peripheral neuralgia. As far as we know snapping triceps syndrome had never been evaluated in sonoelastography.
Case Report
A 28yo semi-professional left handed tennis player was complaining about pain in posterior-medial elbow area. Initial US examination suggest golfers elbow syndrome which occurs quite commonly and has a prevalence of 0.3–0.6% in males and 0–3–1.1% in women and may be associated (approx. 50% of cases) with ulnar neuropathy. However subsequently made MRI revealed unusual distal triceps anatomy, moderate ulnar nerve swelling and lack of medial epicondylitis symptoms. Followed (second) US examination and sonoelastography have detected slipping of the both ulnar nerve and the additional band of the medial triceps head.
Discussion
Snapping elbow syndrome is a poorly known medical condition, sometimes misdiagnosed as the medial epicondylitis. It describes a broad range of pathologies and anatomical abnormalities. One of the most often reasons is the slipping of the ulnar nerve as the result of the Osborne fascia/anconeus epitrochlearis muscle absence. Simultaneously presence of two or more “snapping reasons” is rare but should be always taken under consideration.
Conclusions
There are no sonoelastography studies describing golfers elbow syndrome, additional triceps band and ulnar neuritis. Our data suggest that the sonoelastography signs are similar to those seen in well described lateral epicondylitis syndrome, Achilles tendinitis and medial nerve neuralgia.
MeSH Keywords: Elasticity Imaging Techniques, Elbow Joint, Ulnar Nerve Compression Syndromes
Background
Ulnar neuropathy is the second most common peripheral nerve neuropathy after median neuropathy, with an incidence of 25 cases per 100 000 men and 19 cases per 100 000 women each year [1]. Skipping (snapping) elbow syndrome is an uncommon cause of pain in the posterior-medial elbow area, sometimes complicated by an injury of the ulnar nerve. One of the reasons is a dislocation of an abnormal insertion of the medial triceps head over the medial epicondyle during flexion and extension movements. Others are: lack of the Osboune’s fascia leading to ulnar nerve instability and focal soft tissue tumors (fibromas, lipomas, etc.). Recurrent subluxation of the nerve at the elbow results in tractional and frictional neuritis with classic symptoms of peripheral neuralgia. As far as we know, snapping triceps syndrome has never been evaluated with sonoelastography before.
Case Report
A 28-year-old semi-professional left-handed tennis player complained of recurrent pain in the posteromedial elbow area. Tenderness over the medial humeral epicondyle was noted two months prior to the examination of the patient. Golfer’s elbow syndrome was suspected, which occurs quite commonly and has a prevalence of 0.3–0.6% in males and 0.3–1.1% in women [2] and may be associated (approx. 50% of cases) with ulnar neuropathy [3]. However, the golfer’s test was negative and the patient was directed to the radiodiagnostic unit where he underwent an elbow X-ray and US in a private clinic. The X-ray was normal. The US revealed a small amount of fluid around the medial epicondyle. The image of soft tissues was described as “without any abnormalities”. The patient was prescribed anti-inflammatory drugs (diclofenac) and advised to spare the affected limb. After 6 weeks of rest, the patient returned to playing tennis, which caused all symptoms to recur within the following three weeks. Due to long-lasting pain that impeded his tennis play, the patient underwent a commercial MRI scan at our department. When golfer’s elbow is suspected, it is a good decision to introduce MRI after a negative US result. In a study by Miller et al. [4] the sensitivity of US in detecting medial epicondylitis ranged from 64 to 82%, while the sensitivity of MRI was between 90 and 100%. The study was performed on 1.5 T (Siemens) device using an examination protocol proposed by the ESSR Sports Subcommittee (PD TSE axial/coronal/sagittal and T2 TSE axial/coronal) with additional T1 sequences (axial/coronal). The scan showed tiny fluid collections near to the medial epicondyle (Figure 1). An unusual presence of the distal tendon of the medial triceps head was reported as an additional finding. The ulnar nerve was also slightly enlarged (7.5×3.1 mm). The described changes did not match the golfer’s elbow. Consequently, the snapping elbow syndrome was suspected. Unfortunately, this syndrome can be confirmed only in a dynamic examination. We contacted the patient and advised him to get another US examination, as it was possible that the previous US was conducted without dynamic evaluation of the anatomical relationships in the posterior-medial elbow. Our suspicion was not confirmed by the patient who claimed that the procedure had been carried out correctly. Before the procedure, the Golfer’s elbow test was performed and gave a negative result. However, we noticed a positive Froment’s sign. As far as we know, snapping triceps syndrome has never been evaluated in sonoelastography before.
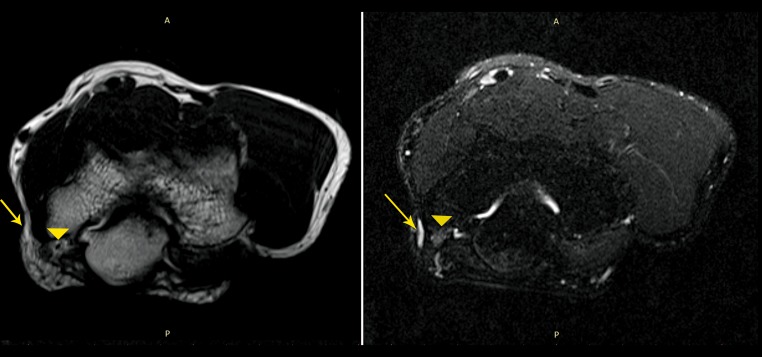
Figure 1.
T2 image (left) and T2 FS presents small fluid collection in the medial epicondyle area (arrow). The ulnar nerve is moderately enlarged (arrowhead).
The examination (US and sonoelastography) was carried out using Toshiba (UIMV-A500A) 12 and 18MHz linear probes. Apart from the fluid, the only abnormality noticed in the classic elbow US protocol (ESSR protocol) was enlargement of the ulnar nerve to 19 mm2 with mild hyperemia inside (Figure 2). A normal ulnar nerve in the cubital tunnel should be less than 9–10 mm2 in size [5,6]. The immage suggested moderate neuralgia [6] which coincided with the McGowan [7] score of ulnar neuropathy. In the sonoelastographic examination, the nerve trunk was also stiffer than the one in the opposite hand. The common flexor tendon had a normal appearance. The additional band of the medial triceps head was less stiff as well (Figure 3). These two different pictures might be easily explained. The nerve trunk underwent an active inflammation leading to an increase in the intra- and extracellular pressure, causing the nerve to be stiffer. Although the muscle band had no signs of hyperemia, it included hypoechoic areas slightly hyperintense in T2-w images on MRI, suggesting a mucoid/lipoid degenerative process. It was unclear whether this was caused by a simple ulnar nerve sliding or a movement-dependent dislocation of the abnormal muscle band, although the second case seemed more probable. Determining the cause of such changes was crucial for introducing appropriate treatment. Failure to recognize dislocation of the ulnar nerve and/or the medial head of the triceps can result in persistent, symptomatic snapping after an otherwise successful operation [8]. We introduced dynamic evaluation. A simple study merely revealed slipping of the nerve. When the study was repeated and counter-resistance was applied to the forearm, it revealed an almost simultaneous slipping of the ulnar nerve and muscle band over the medial epicondyle, with compression of the nerve by the medial epicondyle during that process (Figure 4). Snapping sound, if present, was associated only with the dislocation of the muscle band. No other abnormalities were detected. The patient was instructed to visit a neurologist and orthopedic surgeon for further treatment.
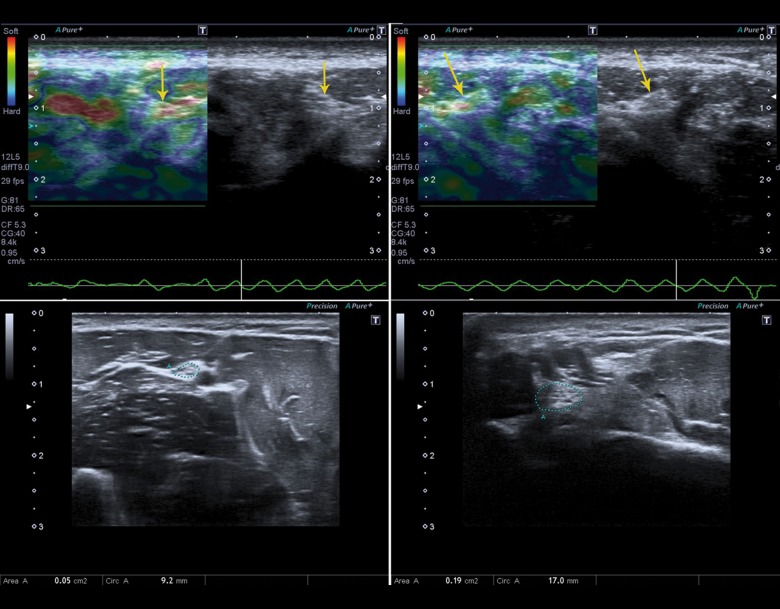
Figure 2.
Enlargement of the ulnar nerve to 0.19 cm2 compared to a normal right nerve (0.05 cm2). The left ulnar nerve is stiffer (green-red color) than the right one (arrow).
Figure 3.
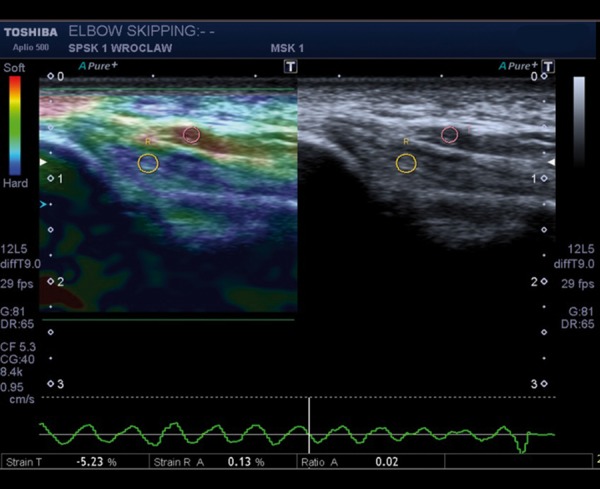
Bifurcated medial triceps head. The additional muscle band has higher softness than the normal one (red color in sonoelastography).
Figure 4.
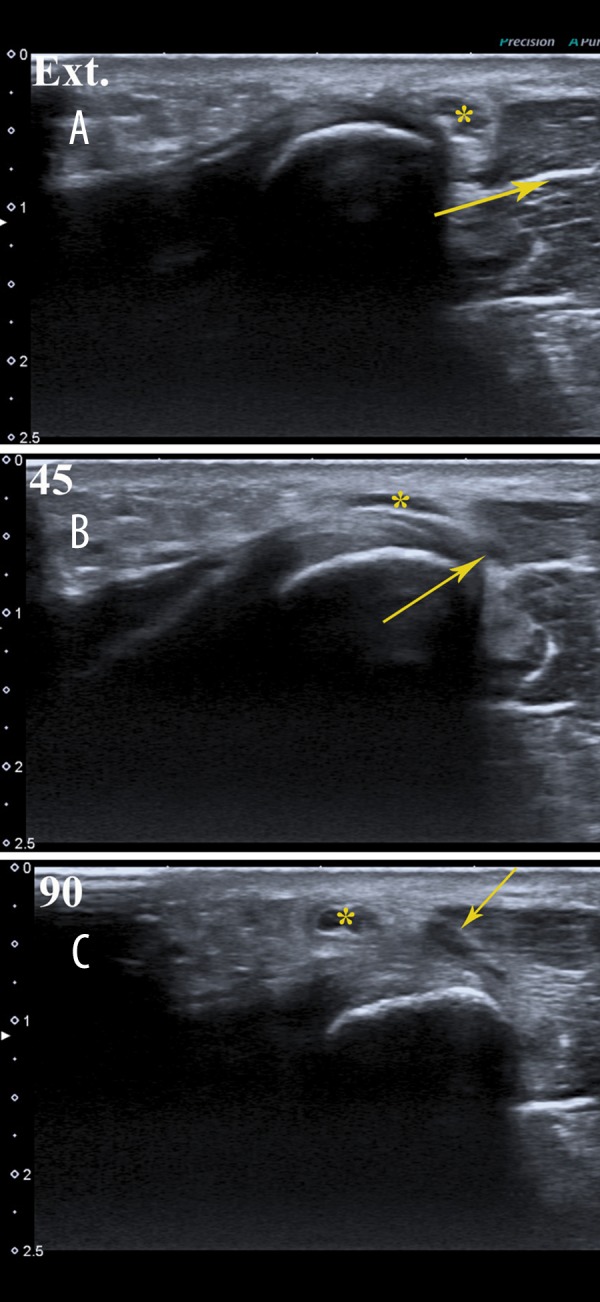
Dislocation of the ulnar nerve (*) and an additional muscle band (arrow) over the medial epicondyle. (A) extended arm, (B) 45-degree flexion, (C) 90-degree flexion.
Discussion
Snapping elbow syndrome is divided into two groups, depending on the cause: intraarticular and extraarticular (Table 1). Skipping triceps syndrome is an example of the extraarticular syndrome and in a healthy population it is an uncommon condition [9]. It may sometimes be confused with other, better known ailments, like the golfer’s elbow [10], present in this case.
Table 1.
| Intraarticular cause | Extraarticular cause | |
|---|---|---|
| Medial localisation | Lateral localisation | |
|
|
|
A rare incidence of this syndrome is one of the reasons of it being under-diagnosed. Moreover, the majority of MRI and US protocols are based on a static limb position. Detection of the abnormality would have been impossible if the data had been collected only at one limb position. Another reason for misdiagnosis of the snapping elbow syndrome may be the lack of counter-resistance exerted on the limb or too high pressure applied by a transducer to the tissues [11].
Ulnar nerve subluxation is another important condition. Following the classification of O’Driscoll [12], cubital tunnel anatomy depends on the type of the cubital tunnel retinaculum. In a normal joint (type Ia and Ib), the roof is formed by Osborne’s fascia. Less commonly, the ligament is replaced by the anconeus epitrochlearis muscle. Both structures stabilize the ulnar nerve position and prevent from subluxation. A complete absence of the retinacular tissue occurs only in a small number of patients (in an original study that was 1/27 patients). In type Ia/b and II elbow flexion it creates a reduction in the volume of the cubital tunnel and increases the extra- and intra-neural tissue pressure. Without them, the growing pressure of an elongating nerve dislocates the nerve over the medial epicondyle edge [13–15]. Repetitive traumatisation results in focal neuritis and clinical symptoms of ulnar neuralgia. Ulnar neuropathy is the second most common peripheral nerve neuropathy, right after median neuropathy, with an incidence of 25 cases per 100 000 men and 19 cases per 100 000 women each year [1]. It is important to distinguish the underlying cause to introduce adequate treatment. Failure to recognize dislocation of the ulnar nerve and/or the medial head of the triceps can result in persistent, symptomatic snapping after an otherwise successful operation [8]. Treatment options are surgical (e.g. anterior submuscular transposition of the ulnar nerve combined with or without minimal/partial epicondylectomy) or conservative (strapping, non-steroidal anti-inflammatory drugs) [16]. Apart from different types of snapping, more typical causes of ulnar nerve traumatisation/compression, such as the arcade of Struthers, anconeus epitrochlearis muscle hypertrophy or deep flexor aponeurosis should always be sought by the ultrasonographer. These conditions are mostly treated by simple surgical decompression [17]. However, if the MR examination does not reveal any of the above mentioned abnormalities, snapping elbow syndrome should be taken into consideration.
There were a few studies establishing usefulness of sonoelastography in upper limb nerve pathologies. The examination was usually performed for the median nerve in CPS (carpal tunnel syndrome) where injured nerve stiffness was significantly increased [18,19]. There have been no studies on ulnar nerves, but the data collected in our study suggest that the ulnar nerve reacts similarly to the median nerve when it comes to mechanical traumatisation. Sonoelastography may be helpful in differential diagnosis of pain in the medial elbow area. Although there are no studies on the golfer’s elbow we assumed that the sonoelastographic image of the common flexor tendon pathology is similar to the image of the common extensor tendon pathology characteristic for the tennis elbow. De Zordo et al. concluded that there is intra-tendinous softening in the common extensor origin in cases of lateral epicondylitis [20]. There were no sonoleatographic studies that focused on the distal triceps tendon and additional triceps band. However, taking into consideration the results of the studies on chronic Achilles tendinosis [20,21] and lateral epicondylitis there is high probability that the image would be similar
Conclusions
Quoting the poet “we need to know what we are looking for when we try to do that” is a great conclusion for this case. The reason why the snapping elbow syndrome was not diagnosed at initial US examination could be poor awareness of its existence or inappropriate technique of examination (application of firm pressure to the skin by the transducer) and lack of neurological symptoms.
Real-time sonoelastography could be valuable in the detection and distinction of medial epicondylitis from an unstable triceps tendon leading to snapping triceps syndrome. If the common flexor tendon origin is normal, but the triceps tendon is hypoechoic and shows intratendinous softening in sonoelastography, the diagnosis of the snapping triceps syndrome should be taken into consideration, even if the previously performed US did not revealed it.
References
- 1.Latinovic R, Gulliford MC, Hughes RA. Incidence of common compressive neuropathies in primary care. J Neurol Neurosurg Psychiatry. 2006;77(2):263–65. doi: 10.1136/jnnp.2005.066696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shiri R, Viikari-Juntura E. Lateral and medial epicondylitis: Role of occupational factors. Best Pract Res Clin Rheumatol. 2011;25:43–57. doi: 10.1016/j.berh.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Gabel GT, Morrey BF. Medial epicondylitis. In: Morrey BF, editor. The Elbow and Its Disorders. 3rd ed. Philadelphia, Pa: WB Saunders Co; 2000. pp. 537–42. [Google Scholar]
- 4.Miller TT, Shapiro MA, Schultz E, Kalish PE. Comparison of sonography and MRI for diagnosing epicondylitis. J Clin Ultrasound. 2002;30(4):193–202. doi: 10.1002/jcu.10063. [DOI] [PubMed] [Google Scholar]
- 5.Ozturk E, Sonmez G, Colak A, et al. Sonographic appearances of the normal ulnar nerve in the cubital tunnel. J Clin Ultrasound. 2008;36(6):325–29. doi: 10.1002/jcu.20486. [DOI] [PubMed] [Google Scholar]
- 6.Volpe A, Rossato G, Bottanelli M, et al. Ultrasound evaluation of ulnar neuropathy at the elbow: correlation with electrophysiological studies. Rheumatology. 2009;48:1098–101. doi: 10.1093/rheumatology/kep167. [DOI] [PubMed] [Google Scholar]
- 7.McGowan AJ. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br. 1950;32:293–30. doi: 10.1302/0301-620X.32B3.293. [DOI] [PubMed] [Google Scholar]
- 8.Spinner RJ, Goldner RD. Snapping of the medial head of the triceps and recurrent dislocation of the ulnar nerve. Anatomical and dynamic factors. J Bone Joint Surg Am. 1998;80(2):239–47. doi: 10.2106/00004623-199802000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Vanhees MKD, Geurts GFAE, van Riet RP. Snapping Triceps Syndrome: A Review of the Literature. Shoulder & Elbow. 2010;2:30–33. [Google Scholar]
- 10.Chan KKW, Wu WK. Snapping elbow syndrome: a case report of two cases. HK Pract. 2011;33:159–68. [Google Scholar]
- 11.Silva HR, Simão MN, Júnior JE, et al. Imaging diagnosis in snapping syndromes. Radiol Bras. 2009;42(1):49–55. [Google Scholar]
- 12.O’Driscoll SW, Horii E, Carmichael SW, et al. The cubital tunnel and ulnar neuropathy. J Bone Joint Surg Br. 1991;73(4):613–17. doi: 10.1302/0301-620X.73B4.2071645. [DOI] [PubMed] [Google Scholar]
- 13.Pechan J, Julius I. The pressure measurement in the ulnar nerve: A contribution to the pathophysiology of the cubital tunnel syndrome. J Biomech. 1975;8:75–79. doi: 10.1016/0021-9290(75)90045-7. [DOI] [PubMed] [Google Scholar]
- 14.Macnicol MF. Extraneural pressures affecting the ulnar nerve at the elbow. Hand. 1982;14:5–11. doi: 10.1016/s0072-968x(82)80030-2. [DOI] [PubMed] [Google Scholar]
- 15.Werner CO, Ohlin P, Elmquist D. Pressures recorded in ulnar neuropathy. Acta Orthop Scand. 1985;56:404–6. doi: 10.3109/17453678508994358. [DOI] [PubMed] [Google Scholar]
- 16.Xarchas KC, Psillakis I, Koukou O, et al. Ulnar Nerve Dislocation at the Elbow: Review of the Literature and Report of Three Cases. Open Orthop J. 2007;1:1–3. doi: 10.2174/1874325000701010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Filippi R, Charalampaki P, Reisch R, et al. Recurrent cubital tunnel syndrome: Etiology and treatment. Minim Invasive Neurosurg. 2001;44:197–201. doi: 10.1055/s-2001-19937. [DOI] [PubMed] [Google Scholar]
- 18.Kantarci F, Ustabasioglu FE, Delil S, et al. Median nerve stiffness measurement by shear wave elastography: a potential sonographic method in the diagnosis of carpal tunnel syndrome. Eur Radiol. 2014;24(2):434–40. doi: 10.1007/s00330-013-3023-7. [DOI] [PubMed] [Google Scholar]
- 19.Miyamoto H, Halpern EJ, Kastlunger M, et al. Carpal tunnel syndrome: diagnosis by means of median nerve elasticity – improved diagnostic accuracy of US with sonoelastography. Radiology. 2014;270(2):481–86. doi: 10.1148/radiol.13122901. [DOI] [PubMed] [Google Scholar]
- 20.De Zordo T, Lill SR, Fink C, et al. Real-time sonoelastography of lateral epicondylitis: comparison of findings between patients and healthy volunteers. Am J Roentgenol. 2009;193(1):180–85. doi: 10.2214/AJR.08.2020. [DOI] [PubMed] [Google Scholar]
- 21.De Zordo T, Chhem R, Smekal V, et al. Real-time sonoelastography: findings in patients with symptomatic achilles tendons and comparison to healthy volunteers. Ultraschall Med. 2010;31(4):394–400. doi: 10.1055/s-0028-1109809. [DOI] [PubMed] [Google Scholar]
- 22.Huang GS, Lee CH, Lee HS, Chen CY. A meniscus causing painful snapping of the elbow joint: MR imaging with arthroscopic and histologic correlation. Eur Radiol Eur Radiol. 2005;15(12):2411–14. doi: 10.1007/s00330-005-2685-1. [DOI] [PubMed] [Google Scholar]