Abstract
Background
The standard recommendation to date has been that acute hypoproliferative thrombocytopenia should be treated with a prophylactic platelet transfusion if the morning platelet count is less than 10 000/µL, or less than 20 000/µL if there are additional risk factors. For chronic thrombocytopenia, transfusion has been recommended if the platelet count is less than 5000/µL. In Germany, half a million platelet transfusions are now being given every year, and the number is rising. New studies indicate, however, that a more restrictive transfusion strategy is justified.
Method
A selective literature search was carried out in PubMed, with additional attention to recommendations from Germany and abroad, and to the guidelines of medical specialty societies.
Results
Prophylactic platelet transfusions should be given when clinically indicated in consideration of the individual hemorrhagic risk. To prevent severe hemorrhage, it is more important to respond to the first signs of bleeding than to pay exclusive attention to morning platelet counts below 10 000/µL. This threshold value remains standard for patients with acute leukemia. According to recent studies, however, clinically stable patients who are at low risk for bleeding—e.g., patients who have undergone autologous hematopoietic stem-cell transplantation—may be well served by a therapeutic, rather than prophylactic, platelet transfusion strategy, in which platelets are transfused only when evidence of bleeding has been observed. For cancer patients, intensive-care patients, and patients with other risk factors, a clinically oriented transfusion strategy is recommended, in addition to close attention to threshold platelet values.
Conclusion
The number of platelet transfusions could be safely lowered by a more restrictive transfusion strategy that takes account of the risk of bleeding, as recommended in the hemotherapy guidelines.
In the 1960s, according to the publication by Gaydos et al. (1), the prophylactic transfusion of platelets became the standard procedure to reduce the risk of bleeding in patients with thrombocytopenia and a morning platelet count of 20 000 platelets/µL or less. In patients with acute leukemia, it was first shown in 1991 that setting the platelet count threshold to 10 000/µL is safe to prevent bleeding in day-to-day clinical practice (2). This trigger for prophylactic platelet transfusion was confirmed to be safe in several consecutive studies and became the standard for clinical routine (3– 6). However, experts have long agreed that the indication for prophylactic transfusion should be based on clinical aspects and the patient’s individual risk situation. With the platelet counts fluctuating throughout the day, the indication should not solely rely on the morning count (7– 10).
In patients with chronic thrombocytopenia, e.g. along with myelodysplastic syndromes (MDS), severe bleeding events are rare, even with platelet counts <10 000/µL. Therefore, the question whether routine prophylactic platelet transfusion is necessary at all becomes increasingly important (11). Most recently, two large randomized controlled studies and one clinical observational study have addressed this issue (12– 14). These studies included patients with acute leukemia as well as patients after autologous stem cell transplantation. One patient group was treated using a therapeutic transfusion strategy, i.e., platelet concentrates were only transfused when clinical bleeding was observed. The other patient group received prophylactic transfusions at platelet counts <10 000/µL.
In Germany, approximately 75% of transfused platelet concentrates are administered to hematology and oncology patients. The remaining 25% are mainly used along with surgical treatments (Dr. Margarethe Heiden, Paul Ehrlich Institute, personal communication). Spot audits in selected hospitals have shown that, in- and outside of Germany, the actual number of platelet concentrate transfusions exceeds the recommendations in the current hemotherapy guidelines by approximately 30 to 40% (6, 15). Blood products are a precious good and voluntary donors dedicate their time and take the risk of adverse events to provide them. Moreover, platelet transfusions expose patients to risks and may very rarely result in fatal outcomes. Thus, they should always be used with caution and proper restraint (10, 16). In addition, recent data indicate that platelet transfusions may have an effect on both inflammatory reactions and the immune system and potentially have a negative impact on the prognosis of malignant diseases (16, 17).
Methods
For this review, a selective literature search in the PubMed database was performed. To this end, the following key words were used: prophylactic and therapeutic platelet transfusion, platelet transfusion and hematological and oncological patients. The level of evidence was reported as follows:
high: sufficiently large and methodological sound, randomized, controlled studies; large prospective studies
moderate: large retrospective and several smaller prospective studies
low: case series; expert opinion based on clinical experience.
This paper provides an overview of new publications on platelet transfusion against the background of the 2008 Cross-Sectional Guidelines of the German Medical Association, as well as international guidelines (5, 6, 18). Particular attention shall be paid to the discussion in recent years about the prophylactic transfusion strategy. Based on this, the authors will develop recommendations for future changes in day-to-day transfusion practice.
Hematology patients
Chronic thrombocytopenia
For chronic thrombocytopenia, e.g. in aplastic anemia or MDS, the hemotherapy guidelines recommend restraint. However, this has so far been confirmed by only one study (11). Provided that the patient has no temperature above 38°C, no apparent bleeding and is not scheduled to undergo surgery, platelets should only be transfused when the platelet count is found to have dropped below 5000/µL in one of the weekly checks (5, 6, 18, 19).
In idiopathic thrombocytopenic purpura (ITP), strictly no prophylactic platelet transfusions should be given. Here, causative treatment has priority (6, 19, 20). Patients with ITP rarely start bleeding despite severe thrombocytopenia. In case of severe bleeding, however, platelet concentrate should be transfused (level of evidence: low to moderate).
Acute thrombocytopenia
Severe thrombocytopenia is observed especially after intensive therapy for acute leukemia and lymphoma. In these cases, national and international guidelines recommend prophylactic platelet transfusions for clinically stable patients only for a morning platelet threshold <10 000/µL (5, 6, 18, 19) (evidence level: high).
Clinically unstable patients are defined as patients with a temperature >38 °C, signs of bleeding, infections, leukocytosis, a plasmatic coagulation disorder, a steep drop in platelets, or existing areas of necrosis. In these cases, transfusions should already be started when the platelet count falls below the threshold of 20 000/µL (6) (evidence level: low).
Newer studies with no risk modification of the trigger have shown that the trigger of 10 000/µL can generally be maintained with clinically unstable patients (12, 13, 21). However, in pediatric and debilitated patients it is recommended to consider concomitant risks, such as an urge to move around and a risk of falling which would justify a higher platelet count as a trigger (evidence level: high).
Prophylactic and therapeutic transfusion strategies
Provided that platelet concentrates are readily available, the question arises whether a therapeutic transfusion strategy would be sufficient in clinical stable patients and thus could replace the current standard of giving a prophylactic transfusion. In the hope of preventing severe and life-threatening hemorrhages, transfusions are given prophylactically, i.e. in the absence of any signs of bleeding. The therapeutic strategy is to immediately transfuse platelet concentrates in the moment when first signs of bleeding become apparent (more than a few isolated petechiae), but not earlier. On this strategy, two large randomized studies have been published in recent years (12, 13, 22). Consistently these studies showed the following results (Table):
Table. Bleeding in two randomized controlled studies.
| WHO Bleeding Scale*1 |
Wandt et al. (12) | p-value | Stanworth et al. (13,22) | p-value | ||
|---|---|---|---|---|---|---|
| prophylactic | therapeutic | prophylactic | therapeutic | |||
| All patients Grade 2 and higher Grade 3 Grade 4 |
65/343 (19)*2 3 (1) 4 (1) |
127/301 (42) 7 (2) 13 (5) |
<0.001 ns 0.016 |
128/299 (43) 1(<1) 0 |
151/301 (50) 4 (1) 2 (1) |
0.04 ns ns |
| Autologous HSCT Grade 2 and higher Grade 3 Grade 4 |
8/98 (8) 0 0 |
29/103 (28) 1 (1) 0 |
0.0005 |
95/210 (45) 0 0 |
99/211 (47) 1 (0.5) 2 (1) |
ns |
| Acute leukemia Grade 2 and higher Grade 3 Grade 4 |
57/245 (24) 3 (1) 4 (2) |
98/198 (51) 6 (3) 13 (7) |
<0.0001 ns 0.0095 |
33/89 (37) 1 (1) 0 |
52/90 (58) 3 (3) 0 |
<0.05 ns |
*1WHO Grade 2: mild bleeding (more than isolated petechiae); no erythrocyte transfusion required; WHO Grade 3: bleeding requiring red cell transfusion; WHO Grade 4: symptomatic retinal or CNS bleeding; any life-threatening or fatal bleeding
*2absolute numbers (%)
WHO. World Health Organization; ns. non-significant; HSCT. hematopoietic stem cell transplantation
Prophylactic transfusions significantly lower the bleeding rate by at least 7%. This was especially shown by the study conducted by Stanworth et al. where bleeding was the primary endpoint (13, 22). A significantly increased bleeding risk with regard to the therapeutic transfusion strategy was found in patients with acute leukemia (52 of 90 affected (58%) vs. 33 of 89 patients (37%) with prophylactic transfusions), but not in patients after autologous stem cell transplantation (99 of 211 affected (47%) vs. 95 of 210 patients (45%) with prophylactic transfusion).
Severe and life-threatening hemorrhages occurred despite prophylactic transfusion. For these, no significant differences were found between the two transfusion strategies in this study (13). In patients with acute leukemia, Wandt et al. observed significantly more episodes of severe bleeding when platelets were only therapeutically transfused (12). In both studies the majority of episodes of severe bleeding occurred with platelet counts >10 000/µL and almost all of these were related to clinical risks.
In both studies, the bleeding risk following autologous hematopoietic stem cell transplantation (comparatively short duration of thrombocytopenia and remission of underlying disease) was significantly lower compared with acute leukemia. In both studies, patients after autologous transplantation did not experience more episodes of severe bleeding when treated according to the therapeutic transfusion strategy. One study found a comparable risk for milder bleeding too (22). These data confirm the results of a previously published observational study (14).
In both studies, the use of platelet concentrates was at least one third lower with the therapeutic strategy. This difference was statically significant. However, both studies reported a tendency to an increased number of red cell transfusions in these patients.
Both randomized studies confirmed the insight already gained in earlier retrospective studies and meta-analyses that severe and life-threatening bleeding is neither primarily due to the degree of thrombocytopenia nor can it be prevented by prophylactic transfusion. These are rather dependent on the clinical risk constellation, such as uncontrolled underlying diseases, comorbidities and additional plasmatic coagulation disorders (7– 9, 12, 13, 21, 22).
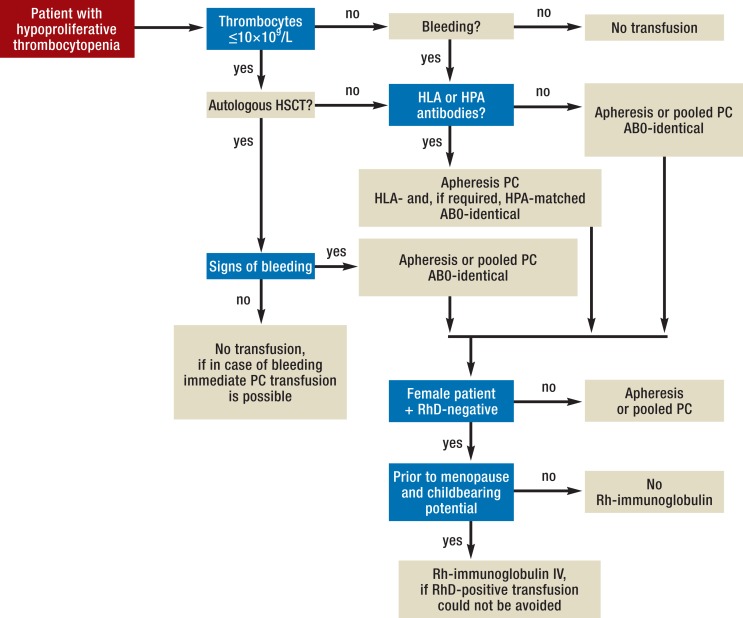
Based on the data currently available, the prophylactic strategy with a platelet transfusion trigger of 10 000/µL should be maintained in patients with acute leukemia. In contrast, the authors and other experts consider the available data convincing enough to also pursue a therapeutic strategy in adult and clinically stable patients after autologous stem cell transplantation while they are monitored on an inpatient basis (Figure). However, it has to be ensured that platelet concentrates are readily available at the first signs of bleeding (10, 12– 14, 22). The increased rate of mild bleeding has to be accepted by both the patient and the treating physician and be balanced against a relevant reduction of platelet transfusions by 30 to 40%. The increased incidence of mild bleeding found in one study (12) and the slightly increased number of days with bleeding in the other study (13, 22) are the direct result of the therapeutic transfusion strategy where the transfusion is only initiated after the first signs of bleeding have become apparent (evidence level: high).
Figure.
Example of an algorithm for platelet concentrate (PC) transfusion in patients with hypoproliferative thrombocytopenia (HLA, human leukocyte antigen; HPA, human platelet antigen; HSCT, hematopoietic stem cell transplantation, Rh, Rhesus factor)
Whether the therapeutic strategy can be extended to other patients with a low bleeding risk, such as e.g. patients with acute leukemia under post-remission therapy, is currently investigated in a study in Germany.
Oncology patients
In oncology patients, treatment-induced thrombocytopenia is less pronounced and persistent compared with leukemia patients. Prophylactic transfusion should usually only be initiated with platelet levels of <10 000/µL (6, 19). The hemotherapy guidelines describe exemptions for brain tumors and brain metastases as well as other tumors associated with an increased bleeding risk. Only in these patients, platelet counts >50 000/µL should be maintained (Box 1).
Box 1. Score for a risk-adapted approach in oncology patients (23).
Any prior bleeding episode
Receiving anti-platelet therapy
Bone marrow metastases
Baseline platelet count <75 000/µL
Genitourinary or gynecologic neoplasm
Performance status >2
Chemotherapy regimen with high bone marrow toxicity
Each risk factor from 1 to 6 counts 2 points and risk factor 7 one point. The bleeding risk of patients with ≥4 points is high. In the study of Elting et al. this applied to 14% of patients. The recommendation for these patients is to transfuse platelets if platelet counts are <20 000/µL and in all other patients if platelets counts are 5000–10 000/µL or less.
Evidence level: moderate
It is not uncommon for oncology patients to present with acute thrombosis (Box 2). Increasingly, oncology patients on anti-platelet therapy after coronary stent placement experience bleeding, e.g. along with gastrointestinal tumors. Thrombocytopenia alone does not reliably prevent in-stent thrombosis. Therefore, according to expert opinion, the platelet count should be above 30 000/µL and at the same time the patient should at least receive aspirin or clopidogrel (e2, e3, 26).
Box 2. Recommendations of the International Society on Thrombosis and Haemostasis and the American Society of Clinical Oncology (24, 25, e1).
During the first four weeks after diagnosis of a deep vein thrombosis, patients should receive anticoagulation with low–molecular weight heparin in therapeutic doses:
Platelet counts should be controlled to be >50 000/µL.
After four weeks, the dose of the low–molecular weight heparin should be reduced in patients with platelet counts <50 000/µL to 50% of the therapeutic dose.
Patients with platelet counts <20 000/µL should not receive anticoagulation.
Especially patients with metastatic cancer can develop thrombocytopenia as the result of tumor-induced activation of coagulation. This, often in combination with concomitant hyperfibrinolysis, aggravates the tendency to bleed (e4). Typically, D-dimer levels are very high. In these cases, antithrombotic treatment with low-molecular-weight heparin is superior to platelet transfusion as long as platelet counts are >20 000/µL; based on the authors’ experience, high doses of heparin are often required. Response to treatment is reflected by rising platelet counts and falling D-dimer levels. Platelets should only be transfused to treat acute bleeding (27) (evidence level: low).
Invasive procedures
Compared with the guidelines of the German Medical Association (Bundesärztekammer) (6), only little new information has become available. The recommendation remains unchanged that prior to minor surgery platelet counts of >20 000/µL should be achieved by means of transfusion, while for procedures with a higher risk of bleeding platelet counts >50 000/µL are recommended. However, it is often not possible to achieve the platelet counts between 70 000 and 100 000/µL stated in the guidelines before neurosurgical procedures. Here, based on the authors’ experience, the surgical procedure can be started with platelet counts of 50 000/µL. For immunized patients, sufficiently compatible platelet concentrates must be made available.
Central venous catheterization (CVC) does not necessarily require prophylactic transfusion, even if marked thrombocytopenia is present (28, 29). Before spinal taps, the guidelines recommend platelet levels of at least 20 000/µL. In 66 patients with acute leukemia, 195 spinal taps were analyzed. Despite platelet counts <20 000/µL, no significant bleeding was observed in this study (30). The physician’s level of experience in performing spinal taps and CVC placements has a greater impact on bleeding complications than the absolute platelet counts (evidence level: low to moderate).
Intensive care patients
Prophylactic transfusion versus therapeutic transfusion
Between 5 and 10% of intensive care patients develop thrombocytopenia with platelet counts <50 000/µL (31). Since there often is uncertainty as to how these patients should be managed, this specific situation is discussed here in greater detail. Currently, between 9 and 30% of intensive care patients receive platelet transfusions, primarily as bleeding prophylaxis (32, 33). This trend was accelerated by an expert recommendation in the 2012 Sepsis Surviving Campaign Guidelines to prophylactically transfuse platelets concentrates in septic patients once a transfusion trigger of 20 000/µL is reached (34).
Recently, a systematic review of the literature on the effect of platelet transfusion in adult intensive care patients was published (35). Platelet counts after administration of a concentrate rose by 15 000/µL on average. Whether the platelet transfusion actually prevents bleeding has not been studied so far. The mortality among these patients is not reduced by the administration of platelets. Therefore, the authors have arrived at the conclusion that it is not possible to issue an evidence-based recommendation given the limited data currently available.
Numerous studies have shown that thrombocytopenia is associated with increased mortality. However, it has not been conclusively determined whether the increased platelet counts resulting from the transfusion have an impact of the survival of these patients. Often, the causes are multifactorial, ranging from reduced production of platelets to increased platelet consumption combined with other complex organ injuries.
In summary, the evidence currently available does not justify to deviate from the recommendation of the hemotherapy guidelines for intensive care patients and only transfuse platelets in case of bleeding or prior to invasive procedures (6) (evidence level: low).
Management of patients refractory to platelet transfusion
In between 10 and 20% of patients, the platelet count rises by less than 5000/µL approximately one hour after transfusion of at least two fresh AB0-compatible platelet concentrate units. The clinical management of this patient is difficult. The increased consumption of transfused platelets is usually the result of non-immunological factors, e.g. bleeding, sepsis or an enlarged spleen. Less frequently (between 1 and 3%), it is related to immunological factors, such as antibodies against human leukocytes (HLA) or platelet antigens (HPA) (36). Before platelet refractoriness is diagnosed, it should be taken into consideration that patients with platelet counts of <5000/µL typically respond to the administration of one platelet concentrate unit with a short temporary increase. The transfused platelets are immediately utilized to seal the endothelium and consumed in the process. In most cases of non-immunological etiology, an increase in platelet counts—and, above all, hemostasis—can be achieved with the transfusion of several blood group-identical platelet concentrate units.
Refractoriness to platelet transfusions due to immunological factors is typically the result of previous pregnancies and frequent transfusions which triggered the production of corresponding antibodies. An immunological cause is suspected when after at least two AB0-compatible transfusions the platelet count has not improved or the bleeding has not been stopped. In this case, HLA-A and -B typing should be initiated urgently. It is advisable to perform this typing prior to any intensive treatment, because in case transfusion-relevant antibodies are detected and the patient starts bleeding, transfusion of HLA-/HPA-compatible platelets is urgently required (6).
Generally, it is recommended to pursue a therapeutic transfusion strategy in immune refractory patients, i.e. to transfuse platelets only if the patient develops severe bleeding or prior to any invasive procedure required. This will help to reduce the risk of induction of additional antibodies (6, 19). In these patients, hemostasis is the key criterion for a successful treatment outcome.
Severe bleeding can be treated by mass transfusion of 8 to 10 AB0-compatible platelet concentrate units in patients refractory to other therapy (6, 19). Furthermore, recent evidence suggests that intravenous administration of tranexamic acid may reduce the tendency to bleed in patients with thrombocytopenia (e5, 37) (evidence level: low to moderate).
Selection of the platelet concentrate
In non-immunized patients, the Cross-Sectional Guidelines of the German Medical Association equally recommend the transfusion of platelet concentrates prepared by apheresis (APC) from a single donor and of pooled platelet concentrate (PPC) which is usually prepared from 4 whole-blood donations. However, immunized patients should only receive APCs (6).
PPCs offer the advantage that the platelets can be harvested from regular whole-blood donations (38). Because of the different production methods used, a direct comparison is not easily possible. The donor population, the intervals between donations and the amount and type of the blood products prepared are different. Taking into consideration all available position statements, there is still no advantag e or disadvantage of the various platelet preparations that has been proven in non-immunized patients (38– 40, e6, e7). To ensure timely treatment of patients with platelet concentrates, both preparation methods are required and to be kept ready nationwide. The treating physician’s decision for or against APC or PPC should be guided by medical criteria. In addition, the availability of the platelet concentrates has to be ensured. When no PPC is available for prompt therapeutic transfusion, the treating physician has to transfuse APC. This has to be paid by the funding organizations. Not indication-related incentives to use one or the other of the various concentrates and transfusion quantities, which currently exist because of the DRG (diagnosis related groups)-based billing system, should be removed immediately (evidence level: moderate to high).
Key Messages.
Not the morning platelet count alone but rather the overall clinical situation determines the risk of severe bleeding in thrombocytopenic patients.
Prophylactic platelet transfusion below a threshold of 10 000/µL, especially in acute leukemia, remains the standard in clinical routine, even though it often cannot prevent severe bleeding. To daily check the patient for first signs of bleeding (more than petechiae or minimal mucosal bleeding) and to administer the therapeutic platelet transfusion required in these cases is crucial in this situation. At the same time, local hemostasis should be attempted whenever possible.
Recent studies, however, have questioned the value of general prophylactic platelet transfusion in patients with a low risk of bleeding, e.g. after autologous stem cell transplantation. Here, a therapeutic strategy may be taken into consideration. By stringent adherence to the transfusion strategy recommended in the guidelines, the number of platelet transfusions could be significantly reduced in some hospitals.
If a prophylactic platelet transfusion is given before a surgical procedure, the transfusion amount required will depend on the bleeding risk associated with the procedure.
Hematology and oncology patients with high coronary risk, e.g. stent, and patients with deep venous thrombosis require adequate anti-platelet therapy or anticoagulation even in the presence of thrombocytopenia. In these cases, additional platelet transfusions may be required.
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Footnotes
Conflict of interest statement
Prof. Greinacher is head of the Institute of Immunology and Transfusion Medicine, Ernst-Moritz-Arndt-University of Greifswald, where platelet concentrates are prepared. He has received congress fees and travel cost reimbursement as well as lecture fees from Maco-Pharma. Prof. Greinacher argues in scientific discussions that pooled platelet concentrates are not inferior to apheresis platelet concentrates.
Prof. Wandt and Dr. Schäfer-Eckart declare that no conflict of interest exists.
References
- 1.Gaydos LA, Freirecht EJ, Mantel N. The quantitative relation between platelet count and hemorrhage in patients with acute leukemia. N Engl J Med. 1962;266:905–909. doi: 10.1056/NEJM196205032661802. [DOI] [PubMed] [Google Scholar]
- 2.Gmür J, Burger J, Schanz U, Fehr J, Schaffner A. Safety of stringent prophylactis platelet transfusion policy for patients with acute leukemia. Lancet. 1991;338:1223–1226. doi: 10.1016/0140-6736(91)92098-m. [DOI] [PubMed] [Google Scholar]
- 3.Rebulla P, Finanzzi G, Marangoni F, et al. The threshold for prophylactic platelet transfusions in adults with acute myeloid leukemia. Gruppo Italiano Malattie Ematologiche Maligne dell’Adulto. N Engl J Med. 1997;337:1870–1875. doi: 10.1056/NEJM199712253372602. [DOI] [PubMed] [Google Scholar]
- 4.Wandt H, Frank M, Ehninger G, et al. Safety and cost effectiveness of a 10x10(9)/L trigger for prophylactic platelet transfusions compared with the traditional 20x10(9)/L trigger: a prospective comparative trial in 105 patients with acute myeloid leukemia. Blood. 1998;91:3601–3606. [PubMed] [Google Scholar]
- 5.Schiffer CA, Anderson KC, Bennet CL, et al. Platelet transfusion for patients with cancer: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol. 2001;19:1519–1538. doi: 10.1200/JCO.2001.19.5.1519. [DOI] [PubMed] [Google Scholar]
- 6.Bundesärztekammer. 4th edition. Kön: Deutscher Ärzte-Verlag; 2009. Querschnitts-Leitlinien zur Therapie mit Blutkomponenten und Plasmaderivaten. [Google Scholar]
- 7.Friedmann AM, Sengul H, Lehmann H, Schwartz C, Goodman S. Do basic laboratoy test of clinical observations predict bleeding in thrombocytopenic oncology patients? A re-evaluation of prophylactic platelet transfusions. Transfus Med Rev. 2002;16:34–45. doi: 10.1053/tmrv.2002.29403. [DOI] [PubMed] [Google Scholar]
- 8.Slichter SJ. Relationship between platelet count and bleeding risk in thrombocytopenic patients. Transfus Med Rev. 2004;18:153–167. doi: 10.1016/j.tmrv.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Estcourt L, Stanworth S, Doree C, et al. Prpophylactic platelet transfusion for prevention of bleeding in patients with haematological disorders after chemotherapy and stem cell transplantation. Cochrane Database Syst Rev. 2012 doi: 10.1002/14651858.CD004269.pub3. CD004269. [DOI] [PubMed] [Google Scholar]
- 10.Schiffer CA. Prophylactic platelet transfusion is frequently not necessary. Nat Rev Clin Oncol. 2013;10:431–432. doi: 10.1038/nrclinonc.2013.113. [DOI] [PubMed] [Google Scholar]
- 11.Sagemeister M, Oec L, Gmür J. A restrictive platelet transfusion policy allowing long-term support of outpatients with severe aplastic anemia. Blood. 1999;93:3124–3126. [PubMed] [Google Scholar]
- 12.Wandt H, Schaefer-Eckart K, Wendelin K, et al. Therapeutic platelet transfusion versus routine prophylactic transfusion in patients with haematological malignancies: an open-label, multicentre, randomized study. Lancet. 2012;380:1309–1316. doi: 10.1016/S0140-6736(12)60689-8. [DOI] [PubMed] [Google Scholar]
- 13.Stanworth SJ, Estcourt LJ, Powter G, et al. A no-prophylaxis platelet-transfusion strategy for hematologic cancers. N Engl J Med. 2013;368:1771–1780. doi: 10.1056/NEJMoa1212772. [DOI] [PubMed] [Google Scholar]
- 14.Wandt H, Schaefer-Eckart K, Frank M, Birkmann J, Wilhelm M. A therapeutic platelet transfusion strategy is safe and feasible in patients after autologous peripheral blood stem cell transplantation. Bone Marrow Transplant. 2006;37:387–392. doi: 10.1038/sj.bmt.1705246. [DOI] [PubMed] [Google Scholar]
- 15.Estcourt LJ. Why has demand for platelet component increased? Areview. Transfus Med. 2014 doi: 10.1111/tme.12155. in press. [DOI] [PubMed] [Google Scholar]
- 16.Blumberg N, Heal JM, Phillips GL, Phipps RP. Platelets - to transfuse or not to transfuse. Lancet. 2012;380:1287–1289. doi: 10.1016/S0140-6736(12)60983-0. [DOI] [PubMed] [Google Scholar]
- 17.Refaai MA, Phipps RP, Spinelli SL, Blumberg N. Platelet transfusions: impact on hemostasis, thrombosis, inflammation and clinical outcomes. Thromb Res. 2011;127:287–291. doi: 10.1016/j.thromres.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.British Committee for Standards in Haematology, Blood Transfusion Task Force. Guidelines for the use of platelet transfusions. Br J Haemat. 2003;122:10–23. [Google Scholar]
- 19.Greinacher A, Kiefel V, Klüter H, Kroll H, Pötzsch B, Riess H. Empfehlung zur Thrombozytentransfusion der Thrombozyten-Arbeitsgruppe der DGTI, GTH und DGHO. Transfus Med Hemother. 2006;33:528–543. doi: 10.1055/s-2006-956275. [DOI] [PubMed] [Google Scholar]
- 20.Neunert C, Lim W, Crowther M, Cohen A, Solberg L, Jr, Crowther MA. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117:4190–4207. doi: 10.1182/blood-2010-08-302984. [DOI] [PubMed] [Google Scholar]
- 21.Slichter SJ, Kaufman RM, Assmann SF, et al. Dose of prophylactic platelet transfusions and prevention of hemorrhage. N Engl J Med. 2010;362:600–613. doi: 10.1056/NEJMoa0904084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stanworth SJ, Estcourt LJ, Llewelyn CA, Murphy MF, Wood EM. Impact of prophylactic platelet transfusions on bleeding events in patients with hematologic malignancies: a subgroup analysis of a randomized trial. Transfusion. 2014 doi: 10.1111/trf.12646. doi: 10.1111/trf.12646. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.Elting LS, Martin CG, Kurtin DJ, et al. The bleeding risk index: a clinical prediction rule to guide the prophylactic use of platelet transfusions in patients with lymphoma or solid tumors. Cancer. 2002;94:3252–3262. doi: 10.1002/cncr.10603. [DOI] [PubMed] [Google Scholar]
- 24.Carrier M, Khorana AA, Zwicker J, Noble S, Lee AY. Subcommittee on haemostasis and malignancy for the SSC of the ISTH: Management of challenging cases of patients with cancer-associated thrombosis including recurrent thrombosis and bleeding: guidance from the SSC of the ISTH. J Thromb Haemost. 2013;11:1760–1765. doi: 10.1111/jth.12338. [DOI] [PubMed] [Google Scholar]
- 25.Lyman GH, Khorana AA, Kuderer NM, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline udate. J Clin Oncol. 2013;31:2189–2204. doi: 10.1200/JCO.2013.49.1118. [DOI] [PubMed] [Google Scholar]
- 26.Matzdorff A, Beer JH. Immun thrombocytopenia patients requiring anticoagulation - maneuvering between Scylla and Charybdis. Sem Hematol. 2013;50:83–88. doi: 10.1053/j.seminhematol.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 27.Wada H, Matsumoto T, Yamashita Y. Diagnosis and treatment of disseminated intravascular coagulation (DIC) according to four guidelines. J Intensive Care. 2014;2 doi: 10.1186/2052-0492-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duffy SM, Coyle TE. Platelet transfusions and bleeding complications associated with plasma exchange catheter placement in patients with presumed thrombotic thrombocytopenic purpura. J Clin Apher. 2013;28:356–358. doi: 10.1002/jca.21279. [DOI] [PubMed] [Google Scholar]
- 29.Zeidler K, Arn K, Senn O, Schanz U, Stussi G. Optimal preprocedural platelet transfusion threshold for central venous catheter insertions in patients with thrombocytopenia. Transfusion. 2011;51:2269–2276. doi: 10.1111/j.1537-2995.2011.03147.x. [DOI] [PubMed] [Google Scholar]
- 30.Avricka SR, Walter RB, Irani S, Halter J, Schanz U. Safety of lumbarpuncture for adults with acute leukemia and restrictive prophylacticplatelet transfusion. Ann Hematol. 2003;82:570–573. doi: 10.1007/s00277-003-0707-0. [DOI] [PubMed] [Google Scholar]
- 31.Stanworth SJ, Walsh TS, Prescott RJ, Lee RJ, Watson DM, Wyncoll DL. Intensive care study of coagulopathy investigators. Thrombocytopenia and platelet transfusion in UK critical care:a multicenter observational study. Transfusion. 2013;53:1050–1058. doi: 10.1111/j.1537-2995.2012.03866.x. [DOI] [PubMed] [Google Scholar]
- 32.McIntyre L, Tinmouth AT, Fergusson DA. Blood component transfusion in critically ill patients. Curr Opin Crit Care. 2013;19:326–333. doi: 10.1097/MCC.0b013e3283632e56. [DOI] [PubMed] [Google Scholar]
- 33.Arnold DM, Crowther MA, Cook RJ, et al. Utilization of platelet transfusions in the intensive care unit: indications, transfusion triggers, and platelet count responses. Transfusion. 2006;46:1286–1291. doi: 10.1111/j.1537-2995.2006.00892.x. [DOI] [PubMed] [Google Scholar]
- 34.Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39:165–228. doi: 10.1007/s00134-012-2769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lieberman L, Bercovitz RS, Sholapur NS, Heddle NM, Stanworth SJ, Arnold DM. Platelet transfusions for critically ill patients with thrombocytopenia. Blood. 2014;123:1146–1151. doi: 10.1182/blood-2013-02-435693. [DOI] [PubMed] [Google Scholar]
- 36.Slichter SJ, Davis K, Enright H, et al. Factors affecting posttransfusion platelet increments, platelet refractoriness, and platelet transfusion intervals in thrombocytopenic patients. Blood. 2005;105:4106–4114. doi: 10.1182/blood-2003-08-2724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wardrop D, Estcourt LJ, Brunskill SJ, et al. Antifibrinolytics (lysine analogues) for the prevention of bleeding in patients with haematological disorders. Cochrane Database Syst Rev. 2013;7 doi: 10.1002/14651858.CD009733.pub2. CD009733. [DOI] [PubMed] [Google Scholar]
- 38.Schrezenmeier H, Seifried E. Buffy-coat-derived pooled platelet concentrates and apheresis platelet concentrates: which product type should be preferred? Vox Sang. 2010;99:1–15. doi: 10.1111/j.1423-0410.2009.01295.x. [DOI] [PubMed] [Google Scholar]
- 39.Hitzler WE. Single-donor (apheresis) platelets and pooled whole-blood-derived platelets - significance and assessment of both blood products. Clin Lab. 2014;60:1–39. doi: 10.7754/clin.lab.2014.140210. [DOI] [PubMed] [Google Scholar]
- 40.Thiele T, Heddle NM, Greinacher A. Donor exposures in recipients of pooled platelet concentrates. N Engl J Med. 2013;368:487–489. doi: 10.1056/NEJMc1213383. [DOI] [PubMed] [Google Scholar]
- e1.Lee AY. Anticoagulation in the treatment of established venous thromboembolism in patients with cancer. J Clin Oncol. 2009;27:4695–4901. doi: 10.1200/JCO.2009.22.3958. [DOI] [PubMed] [Google Scholar]
- e2.Russo A, Cannizzo M, Ghetti G, et al. Idiopathic thrombocytopenia purpura and coronary artery disease: comparision between coronary artery bypass grafting and percutaneous coronary intervention. Interact Cardiovasc Thorac Surg. 2011;13:153–157. doi: 10.1510/icvts.2011.271296. [DOI] [PubMed] [Google Scholar]
- e3.Oliveira W, Meireles GC, Pimenta J. Elective coronary stent implantation in a patient with unstable angina and thrombocytopenia. J Invasive Cardiol. 2005;17:393–394. [PubMed] [Google Scholar]
- e4.Eklund EA. Thrombocytopenia and cancer. Cancer Treat Res. 2009;148:279–293. doi: 10.1007/978-0-387-79962-9_16. [DOI] [PubMed] [Google Scholar]
- e5.Antun AG, Gleason S, Arellano M, et al. Epsilon aminocaproic acid prevents bleeding in severely thrombocytopenic patients with hematological malignancies. Cancer. 2013;119:3784–3787. doi: 10.1002/cncr.28253. [DOI] [PubMed] [Google Scholar]
- e6.Dumont LJ, Szczepiorkowski ZM. Pooled platelet concentrates or apheresis platelets? N Engl J Med. 2013;368:1848–1849. doi: 10.1056/NEJMc1302634. [DOI] [PubMed] [Google Scholar]
- e7.Triulzi DJ, Assmann SF, Strauss RG, et al. The impact of platelet transfusion characteristics on posttransfusion platelet increments and clinical bleeding in patients with hypoproliferative thrombocytopenia. Blood. 2012;119:5553–5562. doi: 10.1182/blood-2011-11-393165. [DOI] [PMC free article] [PubMed] [Google Scholar]