Abstract
The pathogenesis of dysfunctional immunoregulation of mesenchymal stem cells (MSCs) in ankylosing spondylitis (AS) is thought to be a complex process that involves multiple genetic alterations. In this study, MSCs derived from both healthy donors and AS patients were cultured in normal media or media mimicking an inflammatory environment. Whole genome expression profiling analysis of 33,351 genes was performed and differentially expressed genes related to AS were analyzed by GO term analysis and KEGG pathway analysis. Our results showed that in normal media 676 genes were differentially expressed in AS, 354 upregulated and 322 downregulated, while in an inflammatory environment 1767 genes were differentially expressed in AS, 1230 upregulated and 537 downregulated. GO analysis showed that these genes were mainly related to cellular processes, physiological processes, biological regulation, regulation of biological processes, and binding. In addition, by KEGG pathway analysis, 14 key genes from the MAPK signaling and 8 key genes from the TLR signaling pathway were identified as differentially regulated. The results of qRT-PCR verified the expression variation of the 9 genes mentioned above. Our study found that in an inflammatory environment ankylosing spondylitis pathogenesis may be related to activation of the MAPK and TLR signaling pathways.
1. Introduction
Ankylosing spondylitis (AS) is a chronic, immune-mediated inflammatory disease characterized by inflammatory back pain and enthesis [1]. To date, several hypotheses have been proposed to describe the pathogenic mechanism behind this disease, including genetic susceptibility of HLA-B27 [2] and ERAP1 [3], infection [4], and environmental factors [5]. However, none of these hypotheses can fully account for the pathogenesis of ankylosing spondylitis. Recent evidence has increasingly suggested that autoimmune disorders may be involved in the onset and development of this disease [6].
It has been recently demonstrated that mesenchymal stem cells (MSCs) possess an immunosuppressive capability to inhibit Th17 cells and induce Treg subpopulations of CD4+ T cells [7, 8]. In 2011, our research showed that compared to healthy donors, the immunomodulatory ability of MSCs was reduced in AS patients. This was manifested by an increase in Th17 cells and a reduction in Treg cells in CD4+ T cell subgroups after a mixed lymphocyte reaction (MLR) [9]. Furthermore, our clinical trial has also suggested that infusion of MSCs is a feasible, safe, and promising treatment for AS patients [10]. Therefore, we believe that the modulatory function of MSCs can play a significant role in improving disease condition or clinical symptoms in AS patients and that immunoregulatory dysfunction of MSCs may play a critical role in the pathogenesis of AS.
Recently, several researchers carried out whole genome expression profiling analyses comparing AS patients to healthy donors [11–13]. These studies found that AS has a strong association with HLA-B27, and other non-HLA susceptibility genes, such as IL23R and ERAP1 [14, 15]. However, these genetic variations could not fully account for the pathogenesis of ankylosing spondylitis. For example, HLA-B27 accounts for only ~45% of the genetic risk for AS. Therefore, in this study we focused mainly on the significant role of MSCs in AS pathogenesis in order to provide a new viewpoint on this inflammatory disease. Our study investigated whether MSCs grown in vitro from AS patients exhibit gene expression differences in normal culture media or in an inflammatory environment, as compared to healthy controls. We found that mimicking an inflammatory environment can activate the MAPK and TLR signaling pathways in MSCs derived from AS patients, thereby upregulating inflammatory gene expression. This data provides suggestive clues in the exploration of the pathogenic mechanism behind ankylosing spondylitis.
2. Materials and Methods
2.1. Patients and Controls
The present study was approved by the Ethics Committee of the Sun Yat-sen Memorial Hospital of Sun Yat-sen University, Guangzhou, China. From June 2012 to December 2012, twelve healthy donors (HD, 9 men and 3 women) with an average age of 22.1 years and twelve AS patients (10 men and 2 women) with an average age of 21.9 years were enrolled in this study (Table 1). The diagnoses of AS patients were all performed according to the ASAS classification criteria [16]. In addition, all patients involved were diagnosed for the first time and remained in active stage (all Bath Ankylosing Spondylitis Disease Activity Index ≥ 4).
Table 1.
Demographic data and disease characteristics of enrolled patients and healthy donors.
| Items | AS | HD |
|---|---|---|
| Numbers | 12 | 12 |
| Sex | ||
| Men | 10 | 9 |
| Women | 2 | 3 |
| Age (years) | 22.9 (20–30) | 23.1 (21–31) |
| Body weight (Kg) | 63.3 (58–65) | 63.5 (60–66) |
| Disease duration from diagnosis (months) | 33.9 (28–39.6) | 0 |
| HLA-B27 | 11 (91.7%) | 0 |
| History of extra-axial involvement (number of patients) | ||
| Uveitis | 0 | 0 |
| Psoriasis | 0 | 0 |
| Dactylitis | 2 (16.7%) | 0 |
| Inflammatory bowel disease | 1 (8.3%) | 0 |
| Enthesitis | 5 (41.7%) | 0 |
2.2. Isolation and Preparation of MSCs
After being informed about scientific significance, possible risks and complications, and the treatment measures for bone marrow aspirations, all donors and patients signed the informed consent and were aspirated by our skilled allied health professionals in strict accordance with the international standardized procedure. Bone marrow MSCs were isolated from the bone marrow aspirates by density gradient centrifugation as previously described by our work and that of others [9, 17]. After identifying MSC immunophenotype markers by flow cytometry, passages three to five were used for the experiments described below. Both HD and AS groups were separated into two subgroups: MSCs cultured in normal media (Norm) and MSCs cultured in an inflammatory environment (Infla) which was created by adding TNF-α (10 ng/mL) and IFN-γ (10 ng/mL) into normal culture media for four hours. Five representatives of cultured MSCs from HD and AS patients were randomly chosen, cultured in both types of media, and further analyzed. Twenty samples were chosen to complete whole genome expression profiles: 5 HD-Norm, 5 HD-Infla, 5 AS-Norm, and 5 AS-Infla samples.
2.3. Total RNA Extraction and Quality Control
1 mL Trizol (Invitrogen, Carlsbad, USA) was added to lyse the collected cells. Total RNA was extracted using the phenol/chloroform method and salt was washed away with 70% alcohol. After air-drying at 15~30°C, the appropriate amount of RNase-free water was added to dissolve RNA. The integrity and concentration of RNA were assessed to ensure accuracy and reliability. Total RNA from each sample was quantified using a NanoDrop 1000, and RNA integrity was assessed by standard denaturing agarose gel electrophoresis. About 5 μg total RNA from each sample was used for labeling and array hybridization following these steps: (1) Reverse transcription by Invitrogen Superscript ds-cDNA synthesis kit; (2) ds-cDNA labeling with NimbleGen one-color DNA labeling kit; (3) array hybridization using the NimbleGen Hybridization System, followed by washing with the NimbleGen wash buffer kit; (4) array scanning using the Axon GenePix 4000B microarray scanner (Molecular Devices Corporation).
2.4. Microarray Scanning and Data Analysis
Scanned images were then imported into NimbleScan software (version 2.5) for grid alignment and expression data analysis. Data were normalized by quantile normalization and the robust multichip average (RMA) algorithm included in the NimbleScan software. Probe level files and gene level files were generated after normalization. The twenty gene level files were imported into Agilent GeneSpring GX software (version 11.5) for further analysis. After GeneSpring quantile normalization, differentially expressed genes were identified using Volcano Plot filtering. KEGG pathway analysis and GO analysis were applied to determine the roles of these differentially expressed genes in biological pathways or GO terms. Finally, the post hoc Bonferroni test was used to correct for multiplicity since a large number of false positive P values were observed. P values <0.01 were considered significant.
2.5. Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR)
After MSCs were cultured in inflammatory environment mentioned above, total RNA was extracted using Trizol reagent (Life Technologies Inc., USA). Synthesis of cDNA (RT-PCR) was carried out using the SuperScriptH III First-Strand Synthesis System (Invitrogen) according to the manufacturer's instructions. The quantitative real-time PCR (qRT-PCR) analyses were performed in a Light Cycler 480 Real-Time PCR System (Roche, Basel) using a SYBR Premix Ex Taq II kit (Takara, Otsu). The program for quantitative-PCR assay was 95°C for 30 s, followed by 40 cycles of 95°C for 5 s and 60°C for 20 s. The mean mRNA levels were calculated from triplicate analyses of each sample and melting curve analysis was performed to confirm the specific amplification of the targets. The relative amount or fold change of the target genes was normalized according to the expression of the housekeeping geneβ-actin. Parts of the primer sequences used in the real-time PCR assay are as follows:
-
β-actin: 5′-CATGTACGTTGCTATCCAGGC-3′ (Forward) and 5′-CTCCTTAATGTCACGCACGAT-3′ (Reverse);
-
GNA12: 5′-CCGCGAGTTCGACCAGAAG-3′ (Forward) and 5′-TGATGCCAGAATCCCTCCAGA-3′ (Reverse);
-
DUSP1: 5′-AGTACCCCACTCTACGATCAGG-3′ (Forward) and 5′-GAAGCGTGATACGCACTGC-3′ (Reverse);
-
MAPK11: 5′-CTGAACAACATCGTCAAGTGCC-3′ (Forward) and 5′-CATAGCCGGTCATCTCCTCG-3′ (Reverse);
-
RAC1: 5′-ATGTCCGTGCAAAGTGGTATC-3′ (Forward) and 5′-CTCGGATCGCTTCGTCAAACA-3′ (Reverse);
-
MAPK3: 5′-CTACACGCAGTTGCAGTACAT-3′ (Forward) and 5′-CAGCAGGATCTGGATCTCCC-3′ (Reverse);
-
TRAF3: 5′-CAGACTAACCCGCCGCTAAAG-3′ (Forward) and 5′-GATGCTCTCTTGACACGCTGT-3′ (Reverse);
-
IFNAR1: 5′-AACAGGAGCGATGAGTCTGTC-3′ (Forward) and 5′-TGCGAAATGGTGTAAATGAGTCA-3′ (Reverse);
-
IL6: 5′-ACTCACCTCTTCAGAACGAATTG-3′ (Forward) and 5′-CCATCTTTGGAAGGTTCAGGTTG-3′ (Reverse);
-
IFNA1: 5′-GCCTCGCCCTTTGCTTTACT-3′ (Forward) and 5′-CTGTGGGTCTCAGGGAGATCA-3′ (Reverse).
3. Results
3.1. Identification of MSC Immunophenotype
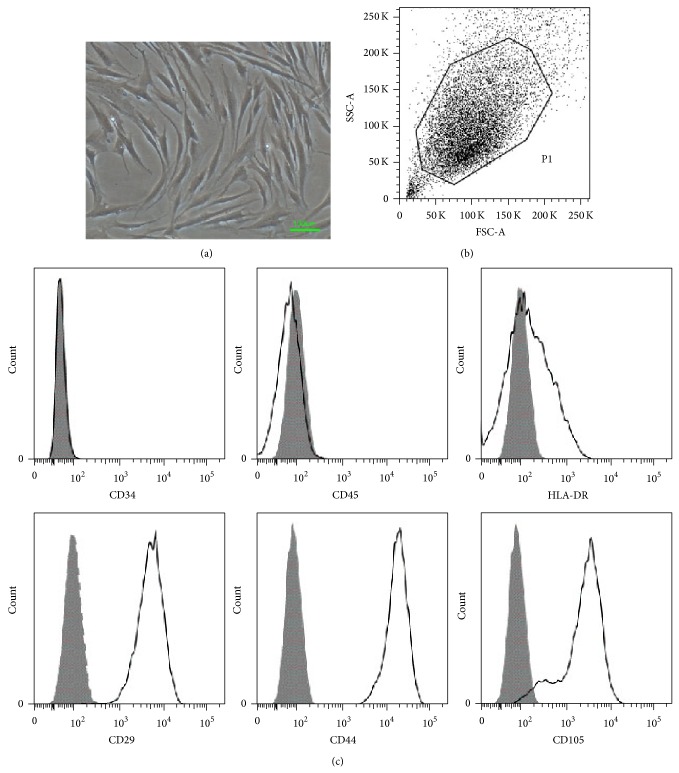
MSCs were obtained from bone marrow aspirates of both healthy volunteers and AS patients. MSCs were cultured and purified to homogeneity according to the culture method described in our previous work [9]. Figure 1(a) shows adherent MSCs growing like intersecting spindle bundles. In addition, immunophenotyping was performed by flow cytometry. Dot plots showing all (ungated) cells as well as gated MSCs are displayed in Figure 1(b). MSCs constitutively expressed CD29, CD44, and CD105 but not CD34, CD45, or HLA-DR (Figure 1(c)).
Figure 1.
Immunophenotype and differentiation of MSCs. (a) Under the 40x microscope, spindle-shaped MSCs grow like intersecting bundles. (b) Dot plot data showing all (nongated) cells as well as gated hMSC (P1). (c) MSCs were harvested, labeled with antibodies against immunophenotype, and analyzed by flow cytometry. MSCs expressed CD29, CD44, and CD105 but not CD34, CD45, and HLA-DR.
3.2. Microarray Hybridization and Data Analysis
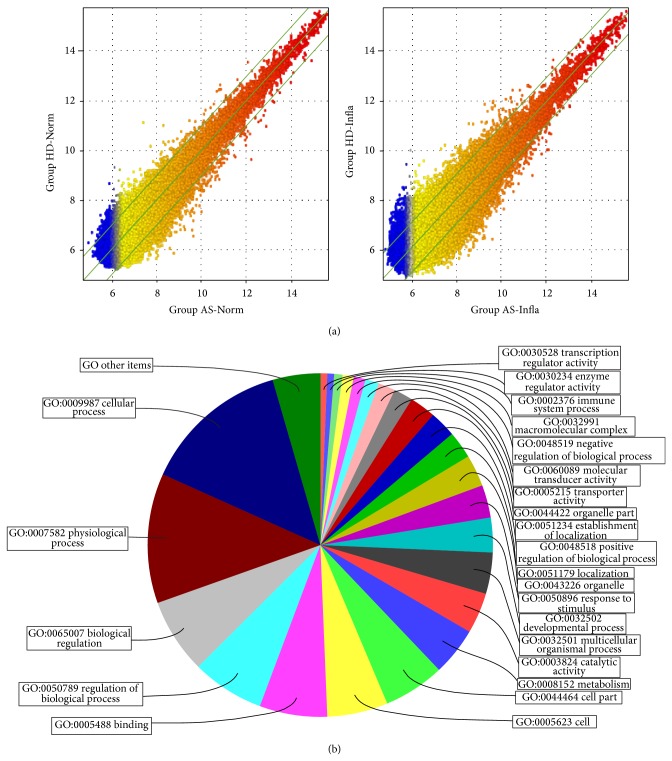
The experimental system was stable and fluorescent signal intensity was strong and homogenous. When cultured under inflammatory conditions, the number of differentially expressed genes in MSCs from AS patients was increased (Figure 2(a)). There were 676 differentially expressed genes in the AS-Norm group, of which 354 were upregulated and 322 were downregulated as compared to the HD-Norm group. 1767 genes were differentially expressed in the AS-Infla group, 1230 upregulated and 537 downregulated, as compared to the HD-Infla group. We used GO (gene ontology) to analyze these differentially expressed genes within three domains (Figure 2(b)).
Figure 2.
Whole genomic expression analysis of MSCs in AS patients. (a) shows the scatter plot of differentially expressed genes of MSCs from both healthy donors and AS patients, respectively, in both normal and inflammatory culture environment. The values of x and y axes in the scatter plot are the normalized signal values of each sample (log2 scaled). The green lines are fold change lines (the default fold change value given is 2.0). Genes above the top green line and below the bottom green line indicated more than 2.0-fold change of genes between two compared arrays. (b) shows the pie chart of gene ontology (GO) analysis of results of the differentially expressed genes of MSCs between group AS-Infla and group HD-Infla. Among the 1590 genes, 892 (56.10%) participated in biological process, 461 (28.99%) played a role in molecular function, and 237 (14.91%) associated with cellular component.
In the biological processes domain, we found 79 significant functional description nodes for group AS-Norm, which were mainly related to intracellular signaling cascades, positive regulation of cellular metabolic processes, regulation of molecular function, positive regulation of macromolecule metabolic processes, positive regulation of cellular biosynthetic processes, and positive regulation of metabolic processes. There were 134 functional description nodes (P < 0.01) in group AS-Infla versus group BD-Infla, which were mainly related to mRNA metabolic processes, nucleobase, nucleoside, nucleotide and nucleic acid metabolic processes, cell cycle, mitotic cell cycle, gene expression, and nitrogen compound metabolic processes (Table 2).
Table 2.
GO analysis of ankylosing spondylitis with different biological processes related to gene.
| Category | GO ID | Term | Count of genes | Percent of count of genes | Fold enrichment | P value |
|---|---|---|---|---|---|---|
| GOTERM_BP | GO:0002376 | Immune system process | 50 | 12.69 | 1.7 | 0.00016 |
| GOTERM_BP | GO:0002520 | Immune system development | 19 | 4.82 | 2.03 | 0.00285 |
| GOTERM_BP | GO:0003006 | Reproductive developmental process | 14 | 3.55 | 2.05 | 0.00898 |
| GOTERM_BP | GO:0006325 | Chromatin organization | 21 | 5.33 | 1.95 | 0.00276 |
| GOTERM_BP | GO:0006816 | Calcium ion transport | 13 | 3.3 | 2.71 | 0.00107 |
| GOTERM_BP | GO:0006950 | Response to stress | 64 | 16.24 | 1.35 | 0.00765 |
| GOTERM_BP | GO:0006996 | Organelle organization | 54 | 13.71 | 1.4 | 0.00669 |
| GOTERM_BP | GO:0007154 | Cell communication | 71 | 18.02 | 1.59 | 0.00005 |
| GOTERM_BP | GO:0007165 | Signal transduction | 108 | 27.41 | 1.24 | 0.00756 |
| GOTERM_BP | GO:0007242 | Intracellular signaling cascade | 73 | 18.53 | 1.7 | 0 |
| GOTERM_BP | GO:0007243 | Protein kinase cascade | 25 | 6.35 | 1.71 | 0.00663 |
| GOTERM_BP | GO:0007275 | Multicellular organismal development | 100 | 25.38 | 1.28 | 0.00422 |
| GOTERM_BP | GO:0009891 | Positive regulation of biosynthetic process | 37 | 9.39 | 2.02 | 0.00004 |
| GOTERM_BP | GO:0009893 | Positive regulation of metabolic process | 46 | 11.68 | 1.87 | 0.00003 |
| GOTERM_BP | GO:0009966 | Regulation of signal transduction | 46 | 11.68 | 1.85 | 0.00004 |
| GOTERM_BP | GO:0009967 | Positive regulation of signal transduction | 20 | 5.08 | 2.32 | 0.00044 |
| GOTERM_BP | GO:0010212 | Response to ionizing radiation | 6 | 1.52 | 3.8 | 0.0048 |
| GOTERM_BP | GO:0010557 | Positive regulation of macromolecule biosynthetic process | 34 | 8.63 | 1.98 | 0.00011 |
| GOTERM_BP | GO:0010604 | Positive regulation of macromolecule metabolic process | 44 | 11.17 | 1.92 | 0.00002 |
| GOTERM_BP | GO:0010627 | Regulation of protein kinase cascade | 15 | 3.81 | 2.07 | 0.00632 |
| GOTERM_BP | GO:0010628 | Positive regulation of gene expression | 32 | 8.12 | 2.11 | 0.00006 |
| GOTERM_BP | GO:0010646 | Regulation of cell communication | 50 | 12.69 | 1.75 | 0.00008 |
| GOTERM_BP | GO:0010647 | Positive regulation of cell communication | 21 | 5.33 | 2.25 | 0.00048 |
| GOTERM_BP | GO:0010740 | Positive regulation of protein kinase cascade | 13 | 3.3 | 2.55 | 0.00185 |
| GOTERM_BP | GO:0015674 | Di-, trivalent inorganic cation transport | 13 | 3.3 | 2.27 | 0.00501 |
| GOTERM_BP | GO:0016568 | Chromatin modification | 18 | 4.57 | 2.26 | 0.00114 |
| GOTERM_BP | GO:0018108 | Peptidyl-tyrosine phosphorylation | 9 | 2.28 | 3.21 | 0.00197 |
| GOTERM_BP | GO:0018212 | Peptidyl-tyrosine modification | 9 | 2.28 | 3.15 | 0.00225 |
Part of GO analysis of biological processes is supplied here; more data can be found in additional files.
In the cellular component domain, 8 significant functional description nodes were found for the AS-Norm group, compared to the BD-Norm group, which were mainly located in the extracellular region, cyclin-dependent protein kinase holoenzyme complex, extracellular region part, keratin filament, neuron projection, cytoplasmic microtubule, extracellular space, and apical plasma membrane. In contrast, compared to group BD-Infla, there were 44 significant functional description nodes for the AS-Infla group, which were mainly located in the intracellular part, intracellular membrane-bounded organelle, membrane-bounded organelle, intracellular organelle lumen, and organelle lumen (Table 3).
Table 3.
GO analysis of differentially expressed genes associated with the cellular location and molecular function.
| Category | GO ID | Term | Count of genes | Percent of count of genes | Fold enrichment | P value |
|---|---|---|---|---|---|---|
| GOTERM_CC | GO:0000307 | Cyclin-dependent protein kinase Holoenzyme complex | 4 | 0.92 | 12.35 | 0.00022 |
| GOTERM_CC | GO:0005576 | Extracellular region | 82 | 18.76 | 1.52 | 0.00006 |
| GOTERM_CC | GO:0005615 | Extracellular space | 29 | 6.64 | 1.6 | 0.00908 |
| GOTERM_CC | GO:0005881 | Cytoplasmic microtubule | 3 | 0.69 | 6.95 | 0.00842 |
| GOTERM_CC | GO:0016324 | Apical plasma membrane | 10 | 2.29 | 2.39 | 0.00945 |
| GOTERM_CC | GO:0043005 | Neuron projection | 18 | 4.12 | 2 | 0.00423 |
| GOTERM_CC | GO:0044421 | Extracellular region part | 41 | 9.38 | 1.61 | 0.00181 |
| GOTERM_CC | GO:0045095 | Keratin filament | 8 | 1.83 | 3.29 | 0.00297 |
| GOTERM_MF | GO:0000287 | Magnesium ion binding | 22 | 5.2 | 1.73 | 0.009 |
| GOTERM_MF | GO:0004725 | Protein tyrosine phosphatase activity | 8 | 1.89 | 2.86 | 0.007 |
| GOTERM_MF | GO:0005057 | Receptor signaling protein activity | 11 | 2.6 | 2.51 | 0.0047 |
| GOTERM_MF | GO:0005102 | Receptor binding | 37 | 8.75 | 1.55 | 0.0055 |
| GOTERM_MF | GO:0005104 | Fibroblast growth factor receptor binding | 4 | 0.95 | 6.95 | 0.0023 |
| GOTERM_MF | GO:0005201 | Extracellular matrix structural constituent | 7 | 1.65 | 3.04 | 0.0082 |
| GOTERM_MF | GO:0005262 | Calcium channel activity | 7 | 1.65 | 3.32 | 0.0051 |
| GOTERM_MF | GO:0008083 | Growth factor activity | 12 | 2.84 | 2.72 | 0.0016 |
| GOTERM_MF | GO:0008138 | Protein tyrosine/serine/threonine phosphatase activity | 6 | 1.42 | 4.86 | 0.0014 |
| GOTERM_MF | GO:0008168 | Methyltransferase activity | 11 | 2.6 | 2.27 | 0.0097 |
| GOTERM_MF | GO:0008276 | Protein methyltransferase activity | 6 | 1.42 | 3.77 | 0.005 |
| GOTERM_MF | GO:0042054 | Histone methyltransferase activity | 5 | 1.18 | 4.05 | 0.0075 |
In the molecular function domain, when compared to group BD-Norm there were 12 significant functional description nodes for the AS-Norm group, such as protein tyrosine/serine/threonine phosphatase activity, growth factor activity, fibroblast growth factor receptor binding, and receptor signaling protein activity. Simultaneously, 20 significant functional description nodes (P < 0.01) were found for group AS-Infla versus group BD-Infla, which included protein binding, nucleic acid binding, structure-specific DNA binding, RNA binding, and hexosaminidase activity (Table 3).
3.3. Screening of Signaling Pathways Related to AS
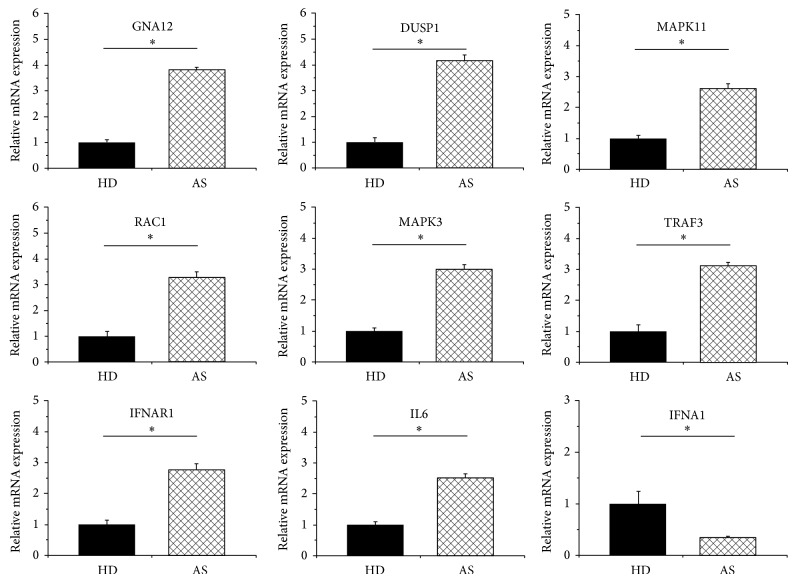
KEGG pathway analysis was used to discover key signaling pathways and relationships between differentially expressed genes. In the inflammatory environment, the two highest scores of indicators in the AS group were hsa04010: mitogen-activated protein kinase (MAPK) signaling pathway, and hsa04620: toll-like receptor (TLR) signaling pathway (Table 4). In the MAPK pathway, there were 14 differentially expressed genes (P < 0.05): DUSP1, GNA12, RAC1, MRAS, ELK1, ATF4, MAPK3, CDC25B, STMN1, MAX, TGFBR2, MAPK11, CACNB3, FGF8, and RASA2 (Table 5). In the TLR pathway, there were 8 key genes with a significant difference in expression (P < 0.05): RAC1, TRAF3, MAPK3, IFNAR1, TICAM1, IL6, MAPK11, and IFNA1 (Table 5). However, there were only two differentially expressed genes (CACNA2D3 and PPM1B) in the MAPK pathway and one key gene (TLR6) in the TLR pathway in the AS group cultured in normal media, both with an insignificant KEGG analysis score (P > 0.05). The results of qRT-PCR verified the expression variation of such genes mentioned above, including GNA12, DUSP1, MAPK11, RAC1, MAPK3, TRAF3, IFNAR1, IL6, and IFNA1 (Figure 3).
Table 4.
Ankylosing spondylitis KEGG pathway analysis result.
| Group compared | KEGG pathway ID and name | Count of genes | Percent of count of genes | Gene name | P value |
|---|---|---|---|---|---|
| Normal environment | Hsa04010: MAPK signaling pathway | 2 | 0.30% | CACNA2D3, PPM1B | 0.12000 |
| Hsa04620: toll-like receptor signaling pathway | 1 | 0.15% | TLR6 | 0.20000 | |
|
| |||||
| Inflammatory environment | Hsa04010: MAPK signaling pathway | 14 | 0.79% | GNA12, DUSP1, MAPK11, RAC1, MRAS, ELK1, ATF4, MAPK3, CDC25B, STMN1, MAX, TGFBR2, CACNB3, FGF8, and RASA2 | 0.00000 |
| Hsa04620: toll-like receptor signaling pathway | 8 | 0.45% | RAC1, TRAF3, MAPK3, IFNAR1, TICAM1, IL6, MAPK11, and IFNA1 | 0.00002 | |
Table 5.
Key gene list of signaling pathways related to AS.
| Signaling pathway | NCBI gene ID | Gene name | Fold change absolute | P value | Regulation | Description |
|---|---|---|---|---|---|---|
| MAPK | 1843 | DUSP1 | 3.89 | 0.02027 | Up | Dual specificity phosphatase 1 |
| MAPK | 2768 | GNA12 | 3.70 | 0.02885 | Up | Guanine nucleotide binding protein (G protein) alpha 12 |
| MAPK | 5879 | RAC1 | 3.15 | 0.00019 | Up | RAS-related C3 botulinum toxin substrate 1 (rho family, small GTP binding protein Rac1) |
| MAPK | 22808 | MRAS | 3.14 | 0.00491 | Up | Muscle RAS oncogene homolog |
| MAPK | 2002 | ELK1 | 2.80 | 0.01115 | Up | ELK1, member of ETS oncogene family |
| MAPK | 5595 | MAPK3 | 2.73 | 0.01417 | Up | Mitogen-activated protein kinase 3 |
| MAPK | 994 | CDC25B | 2.66 | 0.03507 | Up | Cell division cycle 25B |
| MAPK | 468 | ATF4 | 2.50 | 0.04995 | Up | Activating transcription factor 4 (tax-responsive enhancer element B67) |
| MAPK | 3925 | STMN1 | 2.47 | 0.01463 | Up | Stathmin 1/oncoprotein 18 |
| MAPK | 4149 | MAX | 2.31 | 0.00410 | Up | MYC associated factor X |
| MAPK | 7048 | TGFBR2 | 2.18 | 0.03642 | Up | Transforming growth factor, beta receptor II (70/80 kDa) |
| MAPK | 5600 | MAPK11 | 2.12 | 0.04901 | Up | Mitogen-activated protein kinase 11 |
| MAPK | 784 | CACNB3 | 2.04 | 0.03028 | Up | Calcium channel, voltage-dependent, beta 3 subunit |
| MAPK | 2253 | FGF8 | 3.49 | 0.03611 | Down | Fibroblast growth factor 8 (androgen-induced) |
| MAPK | 5922 | RASA2 | 2.83 | 0.01406 | Down | RAS p21 protein activator 2 |
| TLR | 7187 | TRAF3 | 2.86 | 0.03732 | Up | TNF receptor-associated factor 3 |
| TLR | 3454 | IFNAR1 | 2.37 | 0.01055 | Up | Interferon (alpha, beta, and omega) receptor 1 |
| TLR | 148022 | TICAM1 | 2.23 | 0.02105 | Up | Toll-like receptor adaptor molecule 1 |
| TLR | 3569 | IL6 | 2.18 | 0.01526 | Up | Interleukin 6 (interferon, beta 2) |
| TLR | 5879 | RAC1 | 3.15 | 0.00019 | Up | RAS-related C3 botulinum toxin substrate 1 (rho family, small GTP binding protein Rac1) |
| TLR | 5595 | MAPK3 | 2.73 | 0.01417 | Up | Mitogen-activated protein kinase 3 |
| TLR | 5600 | MAPK11 | 2.12 | 0.04901 | Up | Mitogen-activated protein kinase 11 |
| TLR | 3439 | IFNA1 | 2.62 | 0.03022 | Down | Interferon, alpha 1 |
Figure 3.
Verification of differentially expressed genes of MSCs in AS patients cultured in inflammatory environment. RNA was isolated from MSCs of HD (n = 5) and AS patients (n = 5) after MSCs were cultured in inflammatory environment mimicked by TNF-α (10 ng/mL) and IFN-γ (10 ng/mL). Comparison of the levels of differentially expressed genes in MSCs from both groups was based on quantitative real-time polymerase chain reaction (qRT-PCR). Beta-actin was used as an internal control. The results showed that when grown in inflammatory culture medium, 9 of 22 differentially expressed genes from whole genomic expression analysis in AS patients were truly differentially expressed. These genes include GNA12, DUSP1, MAPK11, RAC1, MAPK3, TRAF3, IFNAR1, IL6, and IFNA1. The symbol “∗” represents P < 0.05.
4. Discussion
Ankylosing spondylitis is a type of chronic inflammatory arthritis. Our previous work demonstrated its pathogenesis may be associated with immunomodulatory dysfunction of MSCs in AS patients [9]. The pathogenesis of dysfunctional immunoregulation of MSCs in AS is thought to be a complex process involving multiple genetic alterations. In this study we focused our interest on the difference in MSCs between AS patients and healthy donors and carried out whole genome expression profiling. Our study showed that there were 676 genes differentially expressed between the AS-Norm group and HD-Norm group, 354 upregulated and 322 downregulated. 1767 genes were differentially expressed between the AS-Infla group and HD-Infla group, 1230 upregulated and 537 downregulated. Furthermore, we found that when cultured in an inflammatory environment, MSCs from AS patients suggested an activation of the MAPK and TLR signaling pathways.
By GO analysis, differentially expressed genes involved in biological processes were mainly related to mRNA metabolic processes, nucleobase, nucleoside, nucleotide and nucleic acid metabolic processes, cell cycle, mitotic cell cycle, gene expression, and nitrogen compound metabolic processes. In addition, differentially expressed genes involved mainly in molecular functions were mainly related to protein binding, nucleic acid binding, structure-specific DNA binding, RNA binding, and hexosaminidase activity. Furthermore, KEGG pathway analysis showed that MAPK and TLR signaling pathways were significantly associated with MSCs from AS patients in an inflammatory environment.
Some early research has confirmed that TNF induces a response in MSCs by activating MAPK-dependent mechanisms [18]. In addition, whole blood transcriptional profiling of AS patients has also revealed inflammatory candidate genes including MAPK [19]. We have to consider that, under inflammatory conditions, the MAPK signaling pathway may play a key role in MSCs of AS patients. In this study 14 MAPK signaling genes were differentially expressed, including GNA12, DUSP1, MAPK11, RAC1, MRAS, ELK1, ATF4, MAPK3, CDC25B, STMN1, MAX, TGFBR2, CACNB3, FGF8, and RASA2 (P < 0.01). Some of these genes have been reported to have a relationship with the immune system or even with inflammatory autoimmune diseases. For example, GNA12 has been demonstrated to play a key role in barrier function in the development of ulcerative colitis [20]. DUSP1 (also referred to as MKP1) has been shown to be a critical negative regulator of inflammatory cytokines [21]. Increased expression of DUSP1 in group AS-Infla may be the result of systemic inflammation in AS patients. Moreover, RAC1 activation can be directly induced by IL17A [22] and RAC1 inhibitory peptide has been found to suppress T cell activation and autoantibody production in autoimmune disease [23]. MAPK11 (also referred to as p38BETA) is one of the four members of the p38MAPK family (p38alpha, p38beta, p38gamma, and p38delta). A large body of evidence now indicates that p38MAPK activity is critical for normal immune and inflammatory responses. The p38MAPK pathway is a key regulator of proinflammatory cytokine biosynthesis at both the transcriptional and translational levels, making components of this pathway attractive potential targets for the treatment of autoimmune and inflammatory diseases [24]. Furthermore, p38MAPK inhibitors have been verified to be efficacious in animal models of rheumatoid arthritis, such as collagen-induced arthritis in the mouse and adjuvant-induced arthritis in the rat [25, 26]. Our study has reported that the above-mentioned genes were significantly upregulated in MSCs from AS patients, suggesting a role in the pathogenesis of ankylosing spondylitis. However, the relationship between these differentially expressed genes and ankylosing spondylitis has not been previously reported.
It is well known that upregulation of TLR depends on MAPK signaling [27]. Our present study found that eight key genes from the TLR signaling pathway (including RAC1, TRAF3, MAPK3, IFNAR1, TICAM1, IL6, MAPK11, and IFNA1) were significantly differentially expressed (P < 0.01). Some previous studies have reported that IL6 may participate in the pathogenesis of rheumatoid arthritis (RA), and several clinical trials have been carried out evaluating safety and efficacy of Tocilizumab—an anti-IL6 antibody—in RA patients [28]. Increased IL6 expression in AS patients observed in our study may provide a helpful clue in illustrating its pathogenesis. In addition, tumor necrosis factor receptor-associated factor 3 (TRAF3) is a negative regulator of IL17 receptor (IL17R) signaling. TRAF3 suppresses IL17-induced NF-κB and mitogen-activated protein kinase activation and the subsequent production of inflammatory cytokines and chemokines [29]. Increased expression of TRAF3 observed in group AS-Infla may be due to persistent inflammation in AS patients. Moreover, Kole et al. demonstrated that IFN-1 plays an essential role in producing anti-inflammatory cytokines and maintaining intestinal T cell homeostasis by both limiting effector T cell expansion and promoting Treg stability [30]. Using a knockout mouse model, De Weerd et al. found that lipopolysaccharide-induced sepsis was ameliorated in Ifnar1−/− mice but not Ifnar2−/− mice, which suggests IFNAR1-IFN-β signaling plays a pathological role in inflammatory disease [31]. This study found that IFNA1 was significantly reduced while IFNAR1 was enhanced in MSCs derived from AS patients cultured in an inflammatory environment, which accounts for the increased proinflammatory ability and reduced anti-inflammatory status of AS patients.
5. Conclusions
Our present study confirmed that the pathogenesis of AS stems from multiple gene interactions and key signaling pathway activation. Our study found that an inflammatory environment may activate the MAPK and TLR signaling pathways in MSCs derived from AS patients and causes upregulation of inflammatory gene expression. This data provides suggestive clues in exploring the pathogenesis of ankylosing spondylitis. Finally, further verification and validation of these differentially expressed genes in the pathogenesis of AS will be needed in future research.
Supplementary Material
Supplementary Table 1: GO analysis of ankylosing spondylitis with different biological processes related to gene.
Acknowledgments
This work is supported by the National Natural Science Foundation of China (81271951, 81401850, 81101392), Guangdong Natural Science foundation (S2012010009654, S2012010008927, 10151008901000076) and the Guangzhou Science and Technology Foundation (2014J4100167). The authors thank Mingliang Ren for laboratory and technical support. In addition, the authors are grateful to all colleagues in the Centre for Biotherapy for supplying cells and coordination.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors’ Contribution
Yuxi Li and Peng Wang contributed equally to this work.
References
- 1.Braun J., Sieper J. Ankylosing spondylitis. The Lancet. 2007;369(9570):1379–1390. doi: 10.1016/S0140-6736(07)60635-7. [DOI] [PubMed] [Google Scholar]
- 2.Colbert R. A., Tran T. M., Layh-Schmitt G. HLA-B27 misfolding and ankylosing spondylitis. Molecular Immunology. 2014;57(1):44–51. doi: 10.1016/j.molimm.2013.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keidel S., Chen L., Pointon J., Wordsworth P. ERAP1 and ankylosing spondylitis. Current Opinion in Immunology. 2013;25(1):97–102. doi: 10.1016/j.coi.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Rashid T., Ebringer A. Ankylosing spondylitis is linked to Klebsiella—the evidence. Clinical Rheumatology. 2007;26(6):858–864. doi: 10.1007/s10067-006-0488-7. [DOI] [PubMed] [Google Scholar]
- 5.Taurog J. D., Richardson J. A., Croft J. T., Simmons W. A., Zhou M., Fernández-Sueiro J. L., Balish E., Hammer R. E. The germfree state prevents development of gut and joint inflammatory disease in HLA-B27 transgenic rats. The Journal of Experimental Medicine. 1994;180(6):2359–2364. doi: 10.1084/jem.180.6.2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zambrano-Zaragoza J. F., Agraz-Cibrian J. M., González-Reyes C., Durán-Avelar M. D. J., Vibanco-Pérez N. Ankylosing spondylitis: from cells to genes. International Journal of Inflammation. 2013;2013 doi: 10.1155/2013/501653.501653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luz-Crawford P., Kurte M., Bravo-Alegría J., Contreras R., Nova-Lamperti E., Tejedor G., Noël D., Jorgensen C., Figueroa F., Djouad F., Carrión F. Mesenchymal stem cells generate a CD4+CD25+Foxp3+ regulatory T cell population during the differentiation process of Th1 and Th17 cells. Stem Cell Research & Therapy. 2013;4(3, article 65) doi: 10.1186/scrt216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghannam S., Pene J., Torcy-Moquet G. Mesenchymal stem cells inhibit human Th17 cell differentiation and function and induce a T regulatory cell phenotype. Journal of Immunology. 2010;185(1):302–312. doi: 10.4049/jimmunol.0902007. [DOI] [PubMed] [Google Scholar]
- 9.Wu Y., Ren M., Yang R., Liang X., Ma Y., Tang Y., Huang L., Ye J., Chen K., Wang P., Shen H. Reduced immunomodulation potential of bone marrow-derived mesenchymal stem cells induced CCR4+CCR6+ Th/Treg cell subset imbalance in ankylosing spondylitis. Arthritis Research and Therapy. 2011;13(1, article R29) doi: 10.1186/ar3257. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 10.Wang P., Li Y., Huang L., et al. Effects and safety of allogenic mesenchymal stem cells intravenous infusion in active ankylosing spondylitis patients who failed NSAIDs: a 20 week clinical trial. Cell transplantation. 2014;23(10):1293–1303. doi: 10.3727/096368913X667727. [DOI] [PubMed] [Google Scholar]
- 11.Zhang C., Shen L. Functional modules analysis based on protein-protein network analysis in ankylosing spondylitis. European Review for Medical and Pharmacological Sciences. 2012;16(13):1821–1827. [PubMed] [Google Scholar]
- 12.Xu L., Sun Q., Jiang S., Li J., He C., Xu W. Changes in gene expression profiles of the hip joint ligament of patients with ankylosing spondylitis revealed by DNA chip. Clinical Rheumatology. 2012;31(10):1479–1491. doi: 10.1007/s10067-012-2038-9. [DOI] [PubMed] [Google Scholar]
- 13.Ma H., Xu D., Fu Q. Identification of ankylosing spondylitis-associated genes by expression profiling. International Journal of Molecular Medicine. 2012;30(3):693–696. doi: 10.3892/ijmm.2012.1047. [DOI] [PubMed] [Google Scholar]
- 14.Burton P. R., Clayton D. G., Cardon L. R., et al. Association scan of 14,500 nonsynonymous SNPs in four diseases identifies autoimmunity variants. Nature Genetics. 2007;39:1329–1337. doi: 10.1038/ng.2007.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown M. A. Genetics and the pathogenesis of ankylosing spondylitis. Current Opinion in Rheumatology. 2009;21(4):318–323. doi: 10.1097/BOR.0b013e32832b3795. [DOI] [PubMed] [Google Scholar]
- 16.Sieper J., Rudwaleit M., Baraliakos X., Brandt J., Braun J., Burgos-Vargas R., Dougados M., Hermann K.-G., Landewe R., Maksymowych W., Van Der Heijde D. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Annals of the Rheumatic Diseases. 2009;68(supplement 2):ii1–ii44. doi: 10.1136/ard.2008.104018. [DOI] [PubMed] [Google Scholar]
- 17.Colter D. C., Class R., DiGirolamo C. M., Prockop D. J. Rapid expansion of recycling stem cells in cultures of plastic-adherent cells from human bone marrow. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(7):3213–3218. doi: 10.1073/pnas.070034097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang M., Crisostomo P. R., Herring C., Meldrum K. K., Meldrum D. R. Human progenitor cells from bone marrow or adipose tissue produce VEGF, HGF, and IGF-I in response to TNF by a p38 MAPK-dependent mechanism. The American Journal of Physiology—Regulatory Integrative and Comparative Physiology. 2006;291(4):R880–R884. doi: 10.1152/ajpregu.00280.2006. [DOI] [PubMed] [Google Scholar]
- 19.Pimentel-Santos F. M., Ligeiro D., Matos M., Mourão A. F., Costa J., Santos H., Barcelos A., Godinho F., Pinto P., Cruz M., Fonseca J. E., Guedes-Pinto H., Branco J. C., Brown M. A., Thomas G. P. Whole blood transcriptional profiling in ankylosing spondylitis identifies novel candidate genes that might contribute to the inflammatory and tissue-destructive disease aspects. Arthritis Research and Therapy. 2011;13(2, article R57) doi: 10.1186/ar3309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lees C. W., Barrett J. C., Parkes M., Satsangi J. New IBD genetics: common pathways with other diseases. Gut. 2011;60(12):1739–1753. doi: 10.1136/gut.2009.199679. [DOI] [PubMed] [Google Scholar]
- 21.Zhao Q., Wang X., Nelin L. D., Yao Y., Matta R., Manson M. E., Baliga R. S., Meng X., Smith C. V., Bauer J. A., Chang C.-H., Liu Y. MAP kinase phosphatase 1 controls innate immune responses and suppresses endotoxic shock. Journal of Experimental Medicine. 2006;203(1):131–140. doi: 10.1084/jem.20051794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moran E. M., Connolly M., Gao W., McCormick J., Fearon U., Veale D. J. Interleukin-17A induction of angiogenesis, cell migration, and cytoskeletal rearrangement. Arthritis and Rheumatism. 2011;63(11):3263–3273. doi: 10.1002/art.30582. [DOI] [PubMed] [Google Scholar]
- 23.Abreu J. R. F., Dontje W., Krausz S., de Launay D., van Hennik P. B., van Stalborch A.-M., ten Klooster J.-P., Sanders M. E., Reedquist K. A., Vervoordeldonk M. J., Hordijk P. L., Tak P. P. A Rac1 inhibitory peptide suppresses antibody production and paw swelling in the murine collagen-induced arthritis model of rheumatoid arthritis. Arthritis Research and Therapy. 2010;12(1, article R2) doi: 10.1186/ar2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cuenda A., Rousseau S. p38 MAP-Kinases pathway regulation, function and role in human diseases. Biochimica et Biophysica Acta: Molecular Cell Research. 2007;1773(8):1358–1375. doi: 10.1016/j.bbamcr.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 25.Badger A. M., Bradbeer J. N., Votta B., Lee J. C., Adams J. L., Griswold D. E. Pharmacological profile of SB 203580, a selective inhibitor of cytokine suppressive binding protein/p38 kinase, in animal models of arthritis, bone resorption, endotoxin shock and immune function. The Journal of Pharmacology and Experimental Therapeutics. 1996;279(3):1453–1461. [PubMed] [Google Scholar]
- 26.Badger A. M., Griswold D. E., Kapadia R., et al. Disease-modifying activity of SB 242235, a selective inhibitor of p38 mitogen-activated protein kinase, in rat adjuvant-induced arthritis. Arthritis and Rheumatism. 2000;43(1):175–183. doi: 10.1002/1529-0131(200001)43:1<175::AID-ANR22>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 27.Chang J.-H., Park J.-Y., Kim S.-K. Dependence on p38 MAPK signalling in the up-regulation of TLR2, TLR4 and TLR9 gene expression in Trichomonas vaginalis-treated HeLa cells. Immunology. 2006;118(2):164–170. doi: 10.1016/j.annemergmed.2006.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-Shakarchi I., Gullick N. J., Scott D. L. Current perspectives on tocilizumab for the treatment of rheumatoid arthritis: a review. Patient Preference and Adherence. 2013;7:653–666. doi: 10.2147/PPA.S41433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhu S., Pan W., Shi P., Gao H., Zhao F., Song X., Liu Y., Zhao L., Li X., Shi Y., Qian Y. Modulation of experimental autoimmune encephalomyelitis through TRAF3-mediated suppression of interleukin 17 receptor signaling. The Journal of Experimental Medicine. 2010;207(12):2647–2662. doi: 10.1084/jem.20100703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kole A., He J., Rivollier A., Silveira D. D., Kitamura K., Maloy K. J., Kelsall B. L. Type I IFNs regulate effector and regulatory T cell accumulation and anti-inflammatory cytokine production during T cell-mediated colitis. The Journal of Immunology. 2013;191(5):2771–2779. doi: 10.4049/jimmunol.1301093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Weerd N. A., Vivian J. P., Nguyen T. K., Mangan N. E., Gould J. A., Braniff S.-J., Zaker-Tabrizi L., Fung K. Y., Forster S. C., Beddoe T., Reid H. H., Rossjohn J., Hertzog P. J. Structural basis of a unique interferon-β signaling axis mediated via the receptor IFNAR1. Nature Immunology. 2013;14(9):901–907. doi: 10.1038/ni.2667. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1: GO analysis of ankylosing spondylitis with different biological processes related to gene.