Abstract
Nutritional and developmental insults in the first few years of life have profound public health implications, including substantial contributions to neonatal, infant, and early childhood morbidity and mortality, as well as longer term impacts on cognitive development, school achievement, and worker productivity. Optimal development that can lead to the attainment of the individual's fullest potential therefore requires a combination of genetic capacity, adequate nutrition, psychosocial stimulation, and safe, clean physical environments. Researchers and policymakers have called for integrated child nutrition and development interventions for more than twenty years, yet there are only a handful of efficacy trials and even fewer examples of integrated interventions that have been taken to scale. While a critical component to the design of such interventions is formative research, there is a dearth of information in both the literature and policy arenas to guide this phase of the process. To move the field forward, this paper first provides an overview of formative research methods with a focus on qualitative inquiry, a description of the critical domains to be assessed (infant and young child feeding, responsive feeding, and child development), and currently available resources. Application of these methods is provided through a real-world case study—the design of an integrated nutrition and child development efficacy trial in Andhra Pradesh, India. Recommendations for next steps are discussed, the most important of which is the need for a comprehensive set of formative guidelines for designing locally tailored, culturally appropriate integrated interventions.
Nutritional and developmental insults in the first few years of life have profound public health implications. Nearly eight million children under the age of five die each year from mostly preventable causes, the top killers being neonatal disorders, pneumonia, diarrhea, and malaria.1 A major risk factor underlying one-third of all such deaths is undernutrition, which includes stunting, severe wasting, and vitamin and mineral deficiencies.2 Worldwide, there are 200 million children under the age of five that fail to reach their cognitive developmental potential due to a variety of factors, including poor infant and child nutrition and sub-optimal caregiver-child interactions.3
Two fairly separate arms of research (nutrition/growth and child development) have been ongoing and have identified effective interventions to either reduce child morbidity and mortality4 or to prevent against the loss of developmental potential.5 Key strategies in each area target the care and feeding behaviors of the caregivers most proximal to the child. For example, improving breastfeeding and complementary feeding practices are key strategies for reducing child mortality, while enhancing the quality of caregiver-child interactions is a key component of developmental interventions. These two efforts are further intertwined as caregivers and young children spend a large proportion of time interacting in the feeding domain. Despite the recognition of this synchrony in both the literature6-10 and the policy arena,11-13 only a handful of efficacy trials have tested the effects of integrated child growth and development interventions,14-17 and even fewer interventions have been taken to scale. The WHO Care for Development (CFD) guidelines are a later addition and were developed to support health professionals in counseling parents on how to stimulate their child's development, as well as growth.18
A critical element in the design of such interventions is formative research, which aims to determine how best to fit aspects of program design and/or implementation to the environmental and cultural contexts of its beneficiaries.19 While health researchers often assert the importance of cultural context, many do not understand how to ‘investigate’ culture or how to subsequently apply the findings to the design of an intervention. Aside from a few excellent examples,20-23 the formative research process is often relegated to only a few sentences in a manuscript. The primary aim of this manuscript is therefore to provide an overview of the formative research process required for integrated interventions, focusing in particular on qualitative inquiry—the use of specialized methods to develop context-specific descriptions of a given problem. We begin by defining the meaning of integrated child growth and development interventions and by providing a brief overview of examples from the literature. We then provide a review of qualitative inquiry methods, a synopsis of the formative research domains for integrating nutrition and child development, and illustrate a case study, based on our experiences designing and implementing an integrated feeding and care intervention in Andhra Pradesh, India.
Integration across domains of nutrition, development and culture
Optimal development that can lead to the attainment of the individual's fullest potential requires a combination of genetic capacity, adequate nutrition, psychosocial stimulation, and safe, clean physical environments.24 Nutritional demands change in synchrony with physiologic and cognitive capacity and each is responsive to previous environments (e.g. pre- and peri-conceptual environments) as well as the current social, physical and cultural ecology.25 For example, at birth, developing infants typically are born with rooting, suckling and extrusor reflexes, as well as the gastrointestinal maturity to consume and digest human milk (i.e. developmental and physiological capacities). Additionally, social interactions between caregivers and infants during feeding, like gazing, smiling and verbalizations, promote infant intake.16,26,27 It is the interplay among these factors that best facilitates healthy infant consumption (of human milk), psychosocial development and growth. As the infant grows older, nutrient needs change, as do the motor skills and capacity of the infant. Head control and the palmar and pincer grasp are motor milestones that emerge between 4–12 months and each helps to facilitate the transition to consumption of complementary foods. Concurrently, micronutrient needs (i.e. nutritional demands such as iron and zinc) increase beyond that which can be supplied by human milk and therefore must be met by other complementary food sources. These micronutrients are especially critical to optimal infant cognitive and motor development. In fact, shortfalls in micronutrient intakes during the time period of birth to two years of age are considered to lead to lasting deficits in cognitive development,28 morbidity and mortality in infants.29 During this period, infants develop the capacity to engage in exploratory learning and benefit from caregiver encouragement and participation in developmentally appropriate play.11,13
Abundant research has demonstrated that nurturing and responsive interactions between caregivers and infants promote optimal growth and development.11,13,30,31 Interventions that have encouraged positive play and communication between caregivers and infants have resulted in improvements in child language, cognitive, social and motor dimensions of development. Similar to nutrition interventions, programs that focus upon improvements in development and long-term social outcomes have targeted the early childhood years (birth to 2 years of age period) as a critical intervention time point.
Thus, intervention in early childhood requires integration across the fields of nutrition and development and a continuity of experiences for young children to set the stage for biological as well as neurodevelopmental foundations for the lifecourse.32 The first two years are the period of most rapid development and constitute a time when optimal levels of biochemical (including nutritional) and environmental stimuli (physical, cognitive and social) are required for individuals to meet their fullest potential.33 Therefore, for interventions to optimize success for infant growth and development, they must integrate principles and information from many domains (nutrition, child development, psychosocial stimulation, responsive feeding).5,6,8,24 However, synchronicity and synergism across the various domains can promote optimal development only to the extent that intervention messages and practices are consonant with cultural norms, attitudes, beliefs and practices. Different socio-cultural and environmental settings will require attention to and tailoring of various aspects and therefore interventions must be adapted via systematic formative research.
Current State of Formative Research Methods for Integrated Interventions
There are few examples of integrated interventions in the literature and even fewer examples of formative research for such interventions. Penny, Creed-Kanashiro, Robert, Narro, Caulfield, and Black (2005) published one of the first efficacy trials containing a responsive feeding message: “Teach your child to eat with love, patience, and good humour” (p. 1864).14 While the study, conducted in Peru, utilized formative research to inform message development and implementation, the process is not described in any published, peer-reviewed manuscripts. Similarly, Jin, Sun, Jiang, Ma, Morgan, and Shen (2007) reported findings from an efficacy trial which incorporated an “adapted” (p. 213) version of CFD into existing clinic-based health and nutrition services in China, but no description of the adaptation process is provided.31 More recently, Vazir, Engle, Balakrishna, Griffiths, Johnson, Creed-Kanashiro, Fernandez-Rao, Shroff, and Bentley (2012) published findings of an integrated nutrition and child development efficacy trial in India.17 The authors provide an overview of the formative research timeline, purpose, and end products, yet the process is not fully described.
A promising scale-up effort currently underway is the Sustainable Program Incorporating Nutrition & Games for Maximizing Child Development, Growth and Survival (SPRING), a five-year effectiveness trial of an integrated intervention through existing community-based programs in two countries: the ASHA and Angawadi workers in India and the Lady Health Worker Program in Pakistan.34 Key elements include promoting key newborn and child survival interventions; enhancing care-giving skills; support for optimal infant and young child feeding practices; and the use of a problem solving/supportive counseling approach to help mothers play with their children. Extensive formative research was conducted to answer a set of specific questions with the following aims: 1) adapt the existing care for development package to the local context; 2) determine visit timing and target audience; 3) identify activities in communities and health facilities that support the intervention; 4) integrate SPRING within existing activities; 5) identify health system strengthening requirements for implementing the intervention and for scale-up if the intervention is found to be effective. Formative phase methodologies include in-depth interviews, child care narratives, observations, and workshops. The results of the formative research for this integrated intervention are described in the paper by Lingam, Gupta, Zafar, Hill, Yousafzai, Iyengar, Sikander, ul Haq and Skordis-Worrall (2013) contained in this series.35
Developing a conceptual framework
The starting point for conducting formative research that integrates nutrition and child development is to develop or adapt a conceptual framework informed by information about the specific setting.19 This would include any data available that describe cultural norms of caregiving and gender roles, information about infant and young child feeding, food availability and food security, and nutrition status of the population, particularly for maternal caregivers, etc. Even if there are categories of information where literature is scarce, the framework will help guide the research, indicate gaps of knowledge that need to be filled, and the choice of methods.
There are a number of theoretical models available that can help one to conceptualize how nutrition and care for development can be integrated in the construction and implementation of programs to improve child outcomes.36 In our work, we have frequently drawn upon the social-ecological model (SEM).37 SEM is based upon the theory that children's outcomes (e.g. growth, development, cognition, and health) are impacted by a variety of inputs, including the individual's genetic makeup, as well as the family, organizational (e.g. school) and community (e.g. built, geographical, cultural) environments.
The Formative Research Toolbox
Qualitative methods commonly employed in formative research for nutrition and child development can be broadly classified into three categories: individual interviews, focus group interviews, and observations of the feeding environment and caregiver-infant feeding interactions.19,38,39 A brief overview of each method is provided below, and throughout the next few sections, we reference a variety of resources for conducting qualitative and formative research.
Individual Interviews
Interviews are one of the most important tools for the qualitative researcher. Open-ended interviews, when done well, provide deep insight into individual-level attitudes, beliefs, and behaviors, as well as cultural and social norms surrounding selected beliefs and behaviors. They can also be helpful when exploring sensitive topics that individuals would be reticent to discus in a group setting. To achieve high quality results, we recommend utilizing medical anthropologists or others who are highly trained in interviewing techniques and rapport-building skills.
Common interviewing techniques include in-depth interviews and semi-structured interviews. The principal difference between the two is the conversational nature of the interview. In-depth interviews are free-flowing and flexible. They are usually based on an interview guide containing a bulleted list of topics or a set of research questions, but the interviewer has high discretion in choosing the sequence of topics and/or wording of the questions. In contrast, semi-structured interviews are more standardized, with the interviewer following closely to the wording and sequencing of a pre-determined set of open-ended questions. Semi-structured interviews provide a tool for focused qualitative research when a good understanding of the phenomena to be explored already exists. Semi-structured interviews often take less time to administer and the analysis is much quicker since all respondents are asked the same set of questions. Both types of interviews are typically audio-recorded for subsequent transcription and analysis.
For research on caregiving, feeding, and child development, a wide variety of respondents may be appropriate, including mothers, who are typically primary caregivers, fathers, mothers-in-law, community health workers, midwives and other health care providers. A more sophisticated categorization beyond broad types of respondents is often desired, such that interviews are often conducted with caregivers from varying educational backgrounds, caregivers or health workers in urban versus rural settings, first-time versus multi-gravid mothers, caregivers in food secure versus insecure households/communities or caregivers of infants with varying levels of malnutrition or developmental delay.
Focus Group Interviews
Guided group discussions, or ‘focus groups,’ are another tool for understanding “public values” related to the feeding and care of infants and young children—the things mothers and caregivers feel they should say when gathered together.40 Focus groups are conducted with 6-8 individuals that share some set of traits or experiences, such as the categories outlined previously for individual interviews. A trained moderator initiates discussion using a semi-structured guide containing a series of open-ended questions and probes. As with individual interviews, focus groups are often audio-recorded and then later transcribed for reflection and analysis.
Observations
Direct or structured observations are appropriate as an exploratory method to understand ‘what is going on’ through visual documentation. Observational methods can provide a rich description of behaviors and interactions among individuals in a particular environment. Observations can be recorded as narrative script of happenings within a venue or can utilize a pre-coded data collection instrument. 26,41,42 Observations of the caregiver-infant feeding and caring behaviors will complement interview data, and are particularly essential for understanding styles of parental care – the ‘how’ and not just the ‘what’ and ‘why.’
Because each method in the formative research toolbox has different strengths and weaknesses, it is common for qualitative researchers to use multiple methods to study the same phenomenon19, which is commonly referred to as triangulation. A benefit of triangulation is deeper insight into the phenomenon— individual interviews are essential and provide data on individual-level attitudes, beliefs and behaviors as well as social norms, observations provide visual documentation and are particularly important for examining caregiver-child interactions, and focus groups are particularly helpful in elucidating “public values.” Regardless of the design chosen, one can typically begin with approximately five interviews/observations per type of respondent or two focus groups per each type of respondent, increasing the sample size until “saturation” is reached—the point at which no new information is being revealed through additional interviews. A thorough description of the techniques used to analyze qualitative data is beyond the scope of this paper, but several excellent resources are available.19,43,44
Formative Research Domains for Integrating Nutrition and Child Development
Several domains of inquiry are needed to develop effective, integrated interventions aimed at improving child growth, health and development outcomes. At a minimum, these include individual attitudes, beliefs and behaviors about infant and young child feeding (IYCF) and child development, as well as facilitators and barriers to optimal care, feeding, and early child development practices within the local context. Key concepts, according to their respective domains, are summarized below and sample interview questions for each domain are provided in Table 1.
Table 1.
Sample interview questions in the India study, by formative research domain.
| Infant and Young Child Feeding (IYCF) | Child Development (CD) | Correlates of IYCF and CD Behaviors |
|---|---|---|
|
Breastfeeding and Complementary Feeding 1.Breastfeeding/other milks: •Are you breast, formula or mixed feeding? (probe: why, why not; how long intend, how do you feel about breastfeeding?) 2.Introduction first foods: •What is the best age to begin giving other foods/fluids (in addition to infant formula/milk)? (probe: why, what food/fluids, at what age? Get lists and reasons) 3.Frequency of feeds: • Is it important to have a schedule or routine for feeding? Why/why not? • What happens to your schedule/routine (if any) when you must go out (to work, other venue)? How do you feel about that? Responsive Feeding 1. Cues - hunger/appetite/satiety: • How do you know when your infant is hungry? What happens? • Let's imagine that your child isn't accepting very much food you offer for 1-2 days, what should happen? (probe: pressure to eat; not concerned; talk w others, etc.) 2. Styles of feeding: • When do you think a child can begin to self-feed, at least some foods? • What are all the different ways a mother can encourage her child to eat? (probe: on strategies, such as helping, verbalization, role playing, pressuring etc.) |
1.Local developmental milestones •When do you think babies should be able to: crawl, walk, turn over, eat with a spoon, eat alone, etc.? •Are there specific things a mother could or should do to be sure a baby develops 'on time' (or probe, does it not matter)? •Ethno-theories of development - on physical development, feeding behaviors (e.g., teeth, holding, grabbing, language), mouthing - benefits and costs. 2.Infant crying and management • Tell me about your baby's sleep patterns? (probe: sleeps well, sleeps through night, wakes often, sleeps with mom, own crib, own room, etc.) • What do you do to help your child sleep well? • Most babies cry sometimes. Why do you think babies cry? • What about your baby? When does your baby cry, how often, etc.? 3. Environmental factors • Where does the baby spend most of her time while in the house? What do you do with her? What does she do? (Opportunities for play in the house) • Do you take your baby outside? Where do you take her? What do you do with her? (Outside opportunities for play) |
1.Multiple Caregivers: •Tell me about who takes care of your baby? When/how often? •Under what circumstances do others feed the baby? How do you feel about it? What about in daycare? 2.Advice and Experience: •Were you given advice about how to feed your baby? What was it? From whom? (Find out about peoples' ages, relation to respondent, etc.) •What advice did you keep? How do you know what to keep and what to ignore? 3. Meal Patterns: • Are there different patterns for different family members? If so why? 4. Maternal Diet and Activity pattern: • Do you think that how you eat influences what you feed baby? 5. Food Shopping Patterns: • Where are the main places you shop? How often do you shop? (probe: travel to shop) 6. Mother's Autonomy and health seeking behavior • How much of a say do you have in childcare – take the baby to the doctor, to allow baby to play with others, the foods that are being feed to the baby, etc. • What kind of permission do you require to carry out day-to-day activities related to household matters, other special occasions or festivities, to keep natal connection? |
Source: Vazir S, Engle P, Balakrishna N, et al. Cluster-randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural indian toddlers. Matern Child Nutr. 2013;9(1):99-117.
Infant and Young Child Feeding
Important concepts within this domain include: 1) attitudes and perceived social norms related to breastfeeding; 2) beliefs about the introduction of complementary foods and which foods to feed first; 3) knowledge of infant cues of hunger and satiety and attitudes toward responsive feeding techniques; 4) sources of infant feeding advice and subjective norms related to IYCF; 5) beliefs about safe food preparation; and 6) the quality and adequacy of foods available within the household. Resources for this portion of the formative research phase are readily available—a full review is beyond the scope of this paper, but references to a few examples are provided.45-48 Generally, these resources include guidance on mixed methods (quantitative and qualitative approaches) for developing IYCF interventions.
Child Development
Important concepts in this domain are caregivers’ awareness of developmental processes and milestones, including gross motor (head control, sitting, crawling, standing, walking), fine motor (reaches, grasps, picks up objects), language (sounds, words, receptive and expressive language, verbal interaction), feeding/swallowing reflexes, and infant emotional states and cues. In addition, household availability of toys for play and the extent to which the child is provided with ‘toys’ or common household items to enhance child development are important elements. Unlike for IYCF, there are few published formative research tools for assessing the domain of child development. While several IYCF resources provide guidance on assessing responsive feeding practices—the integration of IYCF and child development—they do not include guidance on assessing caregivers’ knowledge, attitudes, beliefs, and behaviors about child development concepts that fall outside the feeding domain. In the absence of such tools, we suggest readers consult the literature on the methodologies used to adapt child development indicators to different settings and cultural contexts. Many such references can be found in the review in this series by Frongillo, Tofail, Hamadani, Warren and Mehrin (2013) on measures and indicators for integrated interventions.49
Maternal/Caregiver Characteristics
Evidence suggests that several factors are associated with maternal and caregiver knowledge, attitudes, beliefs, and behaviors related to child nutrition and development. These factors include education, income, and depression/psycho-social health.5, 50-52 Therefore the formative research process should include understanding how these factors influence local care and feeding practices. Stratifying participants according to the factors of interest, for example by conducting observations and semi-structured interviews with mothers from varying educational/income backgrounds, and then comparing and contrasting the findings across the groups, can elucidate differences among these groups that are related to this factor. These data help to inform whether a universal package or tailored approaches, messaging or delivery channels, are needed across groups.
Household, Community, and Environmental Characteristics
Household- and community-level, as well as cultural, economic, and physical characteristics of the environment are important to include in the formative research phase as these environmental components also influence intervention development and delivery.51 In many contexts, women (mothers, grandmothers) are the primary targets of nutrition and development interventions, yet their autonomy in making household decisions may be very limited due to cultural norms related to gender roles and decision-making.53-55 Beliefs and norms related to household food allocation and sharing—e.g., men and older children are served before women and infants—can also impact the context and content of intervention messages.56 Women's work expectations and routines, whether inside or outside of the home, can compete with the time allocated to childcare and whether and to what extent implementation of optimal IYCF and child development practices are implemented.56,57 Opportunities and constraints within the health care and community system also should be assessed, such as the number of organizations and types of providers available to deliver health and developmental services to families, the extent of local providers’ knowledge, attitudes, and beliefs about infant nutrition and development, the content of counseling materials and sessions, and opportunities for synergy between existing IYCF and child development programs. Broader environmental characteristics, such as seasonal food production cycles or disease burden (e.g. ALRI, HIV, malaria), must also be considered.52,58
A Case Study—Designing an Integrated Feeding and Care Intervention in Andhra Pradesh, India
As part of the planning and design of a cluster-randomized controlled trial to improve infant growth and development in Andrha Pradesh, India, formative research was conducted six months prior to trial implementation to describe and document current practices for child feeding, responsiveness in child feeding, caregivers’ awareness of child developmental milestones, as well as to identify the underlying beliefs, attitudes and norms for these practices.17 The interdisciplinary research team included anthropologists, nutritionists, and developmental psychologists. Through the formative research process, the research team identified local constraints and opportunities for changing behaviors related to IYCF and child development, selected those practices with potential for change, developed and tested the intervention messages, and defined behavioral indicators for evaluation.
Sampling Strategy and Research Protocol
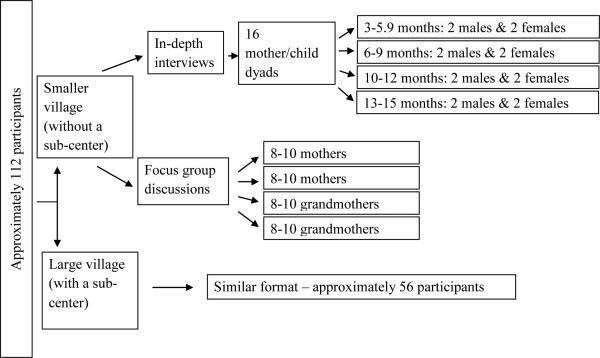
Two villages were selected that differed in population size, one with less than 1,000 people and the other with greater than 5,000 people, to take into account differences in availability of resources according to the size of the village and to include different castes, which may have different practices and beliefs (Figure). Using convenience sampling, women were recruited through local “Mothers’ Committees” until the desired sample size of 32 women, 16 from each of the two villages, was reached. In each village, four mothers of children in the following age groups were included: 3-5, 6-9, 10-12, and 13-15 months. In each age group, mothers of two male and two female children were included to explore any differences related to gender. Inclusion criteria required that participants must be mothers or the principal caregivers (e.g. grandmother) with a child in the study age range and a willingness to participate in home interviews and all assessments.
Figure.
Sampling strategy for the formative phase of the India study.
Mothers and principal caregivers participated in a minimum of two face-to-face home visits which included a 24 hour dietary recall, in-depth interview, and observations of feeding and play. Following completion of the in-depth interviews and a preliminary analysis of the transcripts, four focus group discussions in each village were conducted, stratified with respondents from different socioeconomic status levels. Two focus groups were conducted with mothers and two with grandmothers, each including 8-10 participants. In addition, one in-depth interview was conducted with the local leader in each of the villages. An overview of the formative research methods is given in Table 2.
Table 2.
Overview of formative research tools and application in the India study to integrate complementary and responsive feeding and child development to improve child growth and development.
| Assessment Tool | Application |
|---|---|
| 24-hour dietary recall | To give a rapid assessment of the current feeding pattern of the child. The instrument included a tool that facilitated a rapid summary description of the actual breastfeeding and complementary feeding practices. |
| Home observations | To evaluate the current feeding styles, videotaped observations were made of the principal feeding episode during the day (most often the midday meal). The observations were coded using a structured observation form developed for a previous study (Vietnam ref). Observations were also made relating to child development, specifically in relation to feeding. |
| Semi-structured interviews |
Mothers To explore in depth the feeding practices and caregiver-child interactions related to feeding and play and the perceptions, attitudes and reasons around these practices. Aspects of hygiene, sources of information and contact with Anganwadi workers, and women's were explored through the interviews. Photos of contrasting caregiver-child situations during a feeding episode were selected to be presented to the mother during the interview, to explore with her what she sees and her opinion of the presented situations. Similarly, photos of different sized (thin – chubby) young children were used to explore perceptions of a “healthy” child and to understand the expectations of mothers in the community and potential motivations for behavior change. A free-listing attributes exercise was also included in which a list of selected nutrient rich, locally available foods was used to explore caregivers’ perceptions of their use with infants and young children and potential for promotion in the complementary food intervention component. Key informants Interviews with Anganwadi workers and local health workers to learn of their activities with caregivers in the village including the current recommendations they are giving regarding infant and young child nutrition and feeding. Interviews with local leaders explored community norms and traditions, the mapping of the community, and costs and availability of foods in local markets. |
| Focus group discussions | Conducted with mothers and grandmothers to confirm and explore further some of the results/themes identified in the individual interviews and to assess comprehension and feasibility of behaviour change messages. |
Source: Vazir S, Engle P, Balakrishna N, et al. Cluster-randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural indian toddlers. Matern Child Nutr. 2013;9(1):99-117.
Application of Formative Methods for Message Development
Using data collected, the study investigators developed a series of matrices containing evidence-based, or ideal IYCF, responsive feeding, and child development practices for each of the infant and toddler age ranges. Using data from the dietary recalls, interviews, and observations, the investigators then worked collaboratively amongst themselves to fill in the cells of the matrices, including a summary of the actual behaviours practiced locally, the constraints and opportunities, and the implications of these findings for intervention strategies and message development.
An illustrative matrix is shown in Table 3. The first example demonstrates the process for an ideal behaviour in the IYCF domain—give an iron-rich animal source food (ASF) daily or as frequently as possible. Dietary recall and interview data documented a normative practice of feeding animal milks, while avoiding iron-rich meats or egg yolks. Due to difficulty chewing, meats were delayed until infants had teeth, and eggs were classified as “hot” foods believed to cause diarrhea for young children. Potential strategies, subsequently tested in focus groups, were to link iron-rich ASF to less fussy, stronger infants and to provide recipes for preparing minced meats and scrambled eggs. Scrambling the eggs addressed the strong belief that eggs were considered to be ‘hot’.
Table 3.
Example of matrix constructed from formative data in the India study, by domain, to identify feasible, observable and important opportunities for intervention.
| Ideal Behaviors | Actual Behaviors | Constraints | Opportunity for change | Potential |
|---|---|---|---|---|
| Infant and Young Child Feeding – Complementary Feeding | ||||
| Give an animal source food (ASF) daily or as frequently as possible | 1. Only ASF given until infant has teeth is milk, which is a poor source of iron | 1.Meats are hard consistency; infants cannot swallow; give only when infant has teeth; 2.ASF other than milk are costly 3.Egg yolk is “hot”; gives diarrhoea |
1.Minced meats and soft foods are appropriate if no teeth 2.Unaware of importance of iron, and which ASF are good source of iron |
1.Link iron-rich ASF to less fussy, stronger baby 2.Recipe creation and demonstration of appropriate textures; iron-rich ASF that are soft and/or minced 3.Eggs are less expensive than meat, chicken, liver; teach scrambled egg recipe |
| Responsive Feeding | ||||
| Respond to appetite cues of hunger or rejection | 1.Food/drink offered if child cries, reaches, indicate wants food (may mean - wants second helping) if child is still hungry after feeding; 2.Response to child rejection of food by strategies like forcing, distracting, etc. |
1.Mothers aware of child's hunger & give meal; but second helping rare; 2.Pressure/force if food rejected; some use strategies like -switch position, -switch food, -distract; 3.Do not respond to child's cues as not in a face- to- face position |
1.Some strategies when food rejected -switch position, -switch food, -distract; 2.Wants to finish quickly & do other work |
1.Discourage force feeding; as it disrupts feeding & is distressing; child will reject food more; 2.Build on existing feeding strategies; link healthy baby with happy feeding. Well-fed baby less of bother, & more time for work. 3.Face- to- face position: feeding |
| Child Development | ||||
| Caregiver engages with and talks to child | Rare – but those who do, talked a lot | The child does not understand and so we don't try to talk to him. | The child will listen to you later when you start teaching them. We teach words like Ammma, (Mother) Tatha (Grand father) |
1. Even before child can talk, the child can understand (i.e. receptive language before expressive language). 2. Talking to the child helps them learn to talk and learn well (i.e. language acquisition will help them learn better [in school]). |
Source: Vazir S, Engle P, Balakrishna N, et al. Cluster-randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural indian toddlers. Matern Child Nutr. 2013;9(1):99-117.
A similar matrix was developed for each ideal behavior in each of the core study domains (responsive feeding and child development). The next example demonstrates the process for an ideal behaviour in the Responsive Feeding domain—the caregiver interacts responsively to the child's signals of hunger and satiety. Observational and interview data documented that caregivers sometimes responded appropriately by offering the child food or drink in response to early hunger cues or signs of interest, such as gazing at or reaching for food. A responsive feeding technique was also observed for children's food refusals, in which caregivers distracted the child, pointing to something colorful or interesting in the immediate environment, and then followed with an additional feeding attempt; stopping the feeding if the child remained uninterested. Conversely, instances of nonresponsive feeding techniques were documented—i.e., caregivers initiating a feeding or offering additional food only in response to late hunger cues, such as infant fussing and crying, as well as the use of forceful feeding strategies when infants and toddlers showed disinterest in food or drink. Constraints and opportunities on responsive feeding also emerged from the formative data, namely that caregivers have competing demands on their time and that few caregivers sat face-to-face with children during feeding episodes, thereby reducing the likelihood that they could attend to hunger and satiety cues in an appropriate and timely manner. Based on these findings, the study investigators developed several potential messages that were tested in focus groups. These messages linked responsive feeding practices to positive outcomes with high relevance for this audience—responsive/“happy” feeding techniques lead to healthy, well-fed babies, allowing more time for work; verbalization and praise during feeding episodes would increase acceptance of food by the infant, etc.
The example highlighted in Table 3 for Child Development relates to verbal interaction and engagement with the child in order to promote language development as well as pleasant interactions during feeding and play. The ideal behavior is for caregivers to speak with the child, even before the child can be expected to say words. Interviews indicated that this kind of transaction with infants was rare because of the prevailing idea that infants do not understand language and therefore it was not fruitful to speak to them. Caregivers who already engaged in verbal interactions with their children indicated that children may be more like to respond and listen better when spoken to early and perhaps would even be “more intelligent” later as a result of early verbal interactions with adults. The messages created supported engaging with children, even before they can speak, to improve receptive language and that early verbal interactions with children promote language acquisition; two messages supported by research related to language development.59 The complete set of study messages across the domains of IYCF, Responsive Feeding and Child Development are listed in Table 4.17
Table 4.
Messages in the intervention flip chart used by village workers in the India study to deliver the intervention to mothers/caregivers (messages varied by child age)
| Complementary feeding messages (11) | Responsive feeding messages (8) | Developmental stimulation messages (8) |
|---|---|---|
| Continue frequent on demand breastfeeding Give food of soft, thick consistency Give pulses daily Give animal foods: egg, milk, meat, liver when you eat them Give X (age-appropriate amount) of food at each meal Give dark green/orange vegetables/fruits Give food three times a day Continue feeding during illness; increase during convalescence Give spoonful of oil or ghee Give ICDS fortified food Wash your and child's hands before preparing food and feeding |
Smile and respond to your baby during feeding Teach your child to eat patiently and lovingly Actively help your child to eat Respond to cues of hunger, satiety and rejection Help, but do not physically restrain the child Praise, encourage child to eat; give positive comments Response to child refusal is to offer one more bite |
Smile and look into your child's eyes Respond to child's sounds, gestures and interests Give time to explore objects/persons/things Help your child find new things to do with familiar toys Play simple games e.g. Peek-a boo Talk to child and give names for things and people Ask your child simple questions Explain things and show children how to do things Encourage self-feeding and give child chewable ‘finger-foods’ to eat |
Source: Vazir S, Engle P, Balakrishna N, et al. Cluster-randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural indian toddlers. Matern Child Nutr. 2013;9(1):99-117.
Discussion
As we and others in this volume have noted, there are limited examples of interventions to improve nutrition or child development that are truly integrated and more work on how this can be done to maximize health outcomes is needed. Such research requires a team-based, interdisciplinary approach, with researchers from the social sciences, nutrition, and child development working together from the beginning (just as we are as co-authors of this paper). We have emphasized the importance of doing formative data collection prior to developing an integrated intervention. While intervention components from prior studies can be adapted, socio-cultural and environmental settings will certainly vary and the intervention approach, messages and materials should be contextualized to maximize the opportunities for behavior change. In this chapter we have provided guidelines on how this can be done, with the application of qualitative research methods at the center of the formative research.
The starting point should be to develop a conceptual framework that draws upon a theoretical model or models that will guide the formative research and intervention approach. Such a framework should include individual, household, community, and environmental factors that influence nutrition, growth, and developmental outcomes, with a particular emphasis on care-giving practices in the context of a particular socio-cultural setting. For example, the intervention described in India required formative data on issues related to household decision-making/gender, household access to high quality complementary foods and how these could be promoted for infants, and how responsive feeding and developmental messages could be woven together for the intervention delivery.
We have briefly reviewed the qualitative ‘toolbox of methods’ that can guide the formative research, including the use of individual and group interviews and observational methods. The use of interviews in formative research is very important for understating cultural beliefs and ‘ethnotheories’ of care, parenting, and feeding that guide caregiver behavior. Interview methods are much more common than the use of observational methods, but observations are needed to fully understand styles of feeding and caregiving.41 There are some examples of these in the literature, 26,42 and we suggest the use of videotape, where culturally appropriate. A mix of methods, even for a small formative research study, allows for triangulation of data.19
The lack of guidelines on ‘how’ to do formative research for integrated research and interventions is problematic. There are excellent ‘manuals’ for conducting trials for IYCF, some of which include gathering information on responsive feeding.45-48 The Care for Development manual provides an overview of what to include for a generic intervention aimed at enhancing psycho-social stimulation, with a focus on the use of counseling cards and observations of dyadic interactions.60 We believe there is an important need for guidelines on how the Care for Development manual can be adapted to local settings through formative research, as was done in the Indian trial and for the SPRING effectiveness interventions. What is needed to move the field forward, however, is a comprehensive ‘manual’— a practical set of formative guidelines — for designing locally tailored, culturally appropriate, integrated interventions.
Acknowledgements
We would like to thank other investigators of the research team who participated in the India research that formed the basis of the case study (in addition to authors Bentley, Creed-Kanashiro, Fernandez Rao, and Shroff). This includes two colleagues from the National Institute of Nutrition, Hyderabad, India: co-principal investigator Shahnaz Vazir and Nagalla Balakrishna. Other India team members include Paula L.Griffiths (University of Loughborough, United Kingdom) and Patrice Engle (deceased; California Polytechnic State University).We would also like to thank the anonymous reviewers, whose keen insights added substantially to the quality of the manuscript.
References
- 1.Liu L, Johnson HL, Cousens S, et al. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 2.Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet. 2008;371(9608):243–260. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 3.Grantham-McGregor S, Cheung YB, Cueto S, et al. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369(9555):60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhutta ZA, Ahmed T, Black RE, et al. What works? interventions for maternal and child undernutrition and survival. Lancet. 2008;371(9610):417–440. doi: 10.1016/S0140-6736(07)61693-6. [DOI] [PubMed] [Google Scholar]
- 5.Walker SP, Wachs TD, Grantham-McGregor S, et al. Inequality in early childhood: Risk and protective factors for early child development. Lancet. 2011;378(9799):1325–1338. doi: 10.1016/S0140-6736(11)60555-2. [DOI] [PubMed] [Google Scholar]
- 6.Black MM, Walker SP, Wachs TD, et al. Policies to reduce undernutrition include child development. Lancet. 2008;371(9611):454–455. doi: 10.1016/S0140-6736(08)60215-9. [DOI] [PubMed] [Google Scholar]
- 7.Engle PL, Menon P, Haddad L. Care and nutrition: Concepts and measurement. World Development. 1999;27(8):1309. [Google Scholar]
- 8.Engle PL, Bentley M, Pelto G. The role of care in nutrition programmes: Current research and a research agenda. Proc Nutr Soc. 2000;59(1):25–35. doi: 10.1017/s0029665100000045. [DOI] [PubMed] [Google Scholar]
- 9.Engle PL, Pelto GH. Responsive feeding: Implications for policy and program implementation. J Nutr. 2011;141(3):508–511. doi: 10.3945/jn.110.130039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Engle P, Dustagheer A, Shrivastava D. Malnutrition--importance of care. J Indian Med Assoc. 2000;98(9):514–515. [PubMed] [Google Scholar]
- 11.Department of Child and Adolescent Health, WHO A critical link: Interventions for physical growth and psychosocial development. 1999 [Google Scholar]
- 12.Save the Children The child development index. 2012 [Google Scholar]
- 13.Department of Child and Adolescent Health, WHO The importance of caregiver-child interactions for the survival and healthy development of young children. 2004 [Google Scholar]
- 14.Penny ME, Creed-Kanashiro HM, Robert RC, Narro MR, Caulfield LE, Black RE. Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: A cluster-randomised controlled trial. Lancet. 2005;365(9474):1863–72. doi: 10.1016/S0140-6736(05)66426-4. [DOI] [PubMed] [Google Scholar]
- 15.Aboud FE, Moore AC, Akhter S. Effectiveness of a community-based responsive feeding programme in rural bangladesh: A cluster randomized field trial. Matern Child Nutr. 2008;4(4):275–86. doi: 10.1111/j.1740-8709.2008.00146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aboud FE, Shafique S, Akhter S. A responsive feeding intervention increases children's self-feeding and maternal responsiveness but not weight gain. J Nutr. 2009 doi: 10.3945/jn.109.104885. [DOI] [PubMed] [Google Scholar]
- 17.Vazir S, Engle P, Balakrishna N, et al. Cluster-randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural indian toddlers. Matern Child Nutr. 2013;9(1):99–117. doi: 10.1111/j.1740-8709.2012.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization IMCI Care for Development. 2001 [Google Scholar]
- 19.Bentley ME, Tolley EE, Pequegnat W. Qualitative inquiry: An end not just a means. In: Pequegnat W, Stover E, Boyce CA, editors. How to Write a Successful Research Grant Application: A Guide for Social and Behavioral Scientists. 2nd ed. Springer; New York, NY: 2011. [Google Scholar]
- 20.Gove S, Pelto GH. Focused ethnographic studies in the WHO programme for the control of acute respiratory infections. Medical Anthropology. 1994;15:409–424. doi: 10.1080/01459740.1994.9966102. [DOI] [PubMed] [Google Scholar]
- 21.Menon P, Ruel MT, Loechl C, Pelto G. From research to program design: use of formative research in Haiti to develop a behavior change communication program to prevent malnutrition. Food Nutr Bull. 2005;26(2):241–2. doi: 10.1177/156482650502600210. [DOI] [PubMed] [Google Scholar]
- 22.Pelto GH, Armar-Klemesu M. Balancing nurturance, cost and time: complementary feeding in Accra, Ghana. Matern Child Nutr. 2011;7(S3):66–81. doi: 10.1111/j.1740-8709.2011.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pelto GH, Armar-Klemesu M, Siekmann J, Schofield D. The focused ethnographic study ‘assessing the behavioral and local market environment for improving the diets of infants and young children 6 to 23 months old’ and its use in three countries. Matern Child Nutr. 2013;9(S1):35–46. doi: 10.1111/j.1740-8709.2012.00451.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Engle PL, Black MM, Behrman JR, et al. Strategies to avoid the loss of developmental potential in more than 200 million children in the developing world. Lancet. 2007;369(9557):229–242. doi: 10.1016/S0140-6736(07)60112-3. [DOI] [PubMed] [Google Scholar]
- 25.Johnson SL. Children's food acceptance patterns: The interface of ontogeny and nutrition needs. Nutr Rev. 2002;60(5 Pt 2):S91–4. doi: 10.1301/00296640260130812. [DOI] [PubMed] [Google Scholar]
- 26.Dearden KA, Hilton S, Bentley ME, et al. Caregiver verbal encouragement increases food acceptance among vietnamese toddlers. J Nutr. 2009;139(7):1387–92. doi: 10.3945/jn.108.102780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Black MM, Aboud FE. Responsive feeding is embedded in a theoretical framework of responsive parenting. J Nutr. 2011;141(3):490–494. doi: 10.3945/jn.110.129973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lozoff B, Clark KM, Jing Y, Armony-Sivan R, Angelilli ML, Jacobson SW. Dose-response relationships between iron deficiency with or without anemia and infant social-emotional behavior. J Pediatr. 2008;152(5):696–702. doi: 10.1016/j.jpeds.2007.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gibson RS. Zinc deficiency and human health: Etiology, health consequences, and future solutions. Plant Soil. 2012;361:291–8. [Google Scholar]
- 30.Engle PL, Lhotska L. The role of care in programmatic actions for nutrition: Designing programmes involving care. Food Nutr Bull. 1999;20:121–14. [Google Scholar]
- 31.Jin X, Sun Y, Jiang F, Ma J, Morgan C, Shen X. “Care for development” intervention in rural china: A prospective follow-up study. J Dev Behav Pediatr. 2007;28(3):213–218. doi: 10.1097/dbp.0b013e31802d410b. [DOI] [PubMed] [Google Scholar]
- 32.Heckman J, Masterov DV. The productivity argument for investing in young children. University of Chicago; Chicago, IL: 2005. [Google Scholar]
- 33.Evans JL, Myers RG, Ilfeld EM. Early Childhood Counts: A Programming Guide on Early Childhood Care for Development. World Bank Publications; Washington, D.C.: 2000. [Google Scholar]
- 34.London School of Hygiene & Tropical Medicine SPRING: Sustainable Programme Incorporating Nutrition and Games for Maximising Child Development, Growth and Survival. http://spring.lshtm.ac.uk Published 2012.
- 35.Lingam, Gupta, Zafar, Hill, Yousafzai, Iyengar, Sikander, ul Haq, Skordis-Worrall Understanding care and feeding practices: building blocks for a sustainable intervention in India and Pakistan. Ann. N. Y. Acad. Sci. 2013 doi: 10.1111/nyas.12326. (under review) [DOI] [PubMed] [Google Scholar]
- 36.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research and Practice. 4th edition Jossey-Bass; San Francisco, CA: 2008. [Google Scholar]
- 37.Bronfenbrenner U. International Encyclopedia of Education. 2nd ed. Vol. 3. Elsevier; Oxford: 1994. Ecological models of human development. pp. 37–7. [Google Scholar]
- 38.Schensul JJ, LeCompte MD. Essential Ethnographic Methods: A Mixed Methods Approach. AltaMira Press; Lanham, MD: 2012. [Google Scholar]
- 39.Pelto PJ. Applied Ethnography: Guidelines for Field Research. Left Coast Press, Inc.; Walnut Creek, CA: 2013. [Google Scholar]
- 40.Goffman E. The presentation of self in everyday life. Doubleday; New York, NY: 1990. [Google Scholar]
- 41.Bentley ME, Wasser HM, Creed-Kanashiro HM. Responsive feeding and child undernutrition in low- and middle-income countries. J Nutr. 2011;141(3):502–507. doi: 10.3945/jn.110.130005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moore AC, Akhter S, Aboud FE. Responsive complementary feeding in rural bangladesh. Soc Sci Med. 2006;62(8):1917–30. doi: 10.1016/j.socscimed.2005.08.058. [DOI] [PubMed] [Google Scholar]
- 43.Ulin PR, Robinson ET, Tolley EE. Qualitative Methods in Public Health. Jossy-Bass; San Francisco, CA: 2005. [Google Scholar]
- 44.Miles BM, Huberman A, Saldana J. Qualitative Data Analysis: A Methods Sourcebook. Third ed. Sage Publications, INC.; Thousand Oaks, CA: 2013. [Google Scholar]
- 45.Pelto GH, Gove S. Developing a focused ethnographic study for the WHO Acute Respiratory Infection Control Programme. In: Scrimshaw NS, Gleason GR, editors. Rapid Assessment Procedures: Qualitative Methodologies for Planning and Evaluation of Health Related Programmes. International Nutrition Foundation; Boston, MA: 1992. pp. 215–226. [Google Scholar]
- 46.Pan-American Health Organization ProPAN: Process for the Promotion of Child Feeding. http://www.paho.org/common/Display.asp?Lang=E&RecID=6048. Published October 15, 2003.
- 47.CoreGroup Nutrition Progam Design Assistant. http://www.coregroup.org/component/content/article/119. Published April 23, 2010.
- 48.UNICEF The Community Infant and Young Child Feeding Package: Adaptation Guide. http://www.unicef.org/nutrition/index_58362.html. Updated 2012.
- 49.Frongillo EA, Tofail F, Hamadani JD, Warren AM, Mehrin SF. Measures and indicators for assessing impact of interventions integrating nutrition, health, and early childhood development. Ann. N. Y. Acad. Sci. doi: 10.1111/nyas.12319. (under review) [DOI] [PubMed] [Google Scholar]
- 50.Boyle MH, Racine Y, Georgiades K, et al. The influence of economic development level, household wealth and maternal education on child health in the developing world. Soc Sci Med. 2006;63(8):2242–2254. doi: 10.1016/j.socscimed.2006.04.034. [DOI] [PubMed] [Google Scholar]
- 51.Heaton TB, Forste R, Hoffmann JP, Flake D. Cross-national variation in family influences on child health. Soc Sci Med. 2005;60(1):97–108. doi: 10.1016/j.socscimed.2004.04.029. [DOI] [PubMed] [Google Scholar]
- 52.Wuehler SE, Ouedraogo AW. Situational analysis of infant and young child nutrition policies and programmatic activities in Burkina Faso. Matern Child Nutr. 2011;7(S1):35–62. doi: 10.1111/j.1740-8709.2010.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Becker S, Fonseca-Becker F, Schenck-Yglesias C. Husbands’ and wives’ reports of women's decision-making power in western guatemala and their effects on preventive health behaviors. Soc Sci Med. 2006;62(9):2313–2326. doi: 10.1016/j.socscimed.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 54.Shroff M, Griffiths P, Adair L, Suchindran C, Bentley M. Maternal autonomy is inversely related to child stunting in andhra pradesh, india. Matern Child Nutr. 2009;5(1):64–74. doi: 10.1111/j.1740-8709.2008.00161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shroff MR, Griffiths PL, Suchindran C, Nagalla B, Vazir S, Bentley ME. Does maternal autonomy influence feeding practices and infant growth in rural india? Soc Sci Med. 2011;73(3):447–455. doi: 10.1016/j.socscimed.2011.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Messer E. Intra-household allocation of food and health care: Current findings and understandings--introduction. Soc Sci Med. 1997;44(11):1675–1684. doi: 10.1016/s0277-9536(96)00370-x. [DOI] [PubMed] [Google Scholar]
- 57.Thompson JE. Poverty, development, and women: Why should we care? J Obstet Gynecol Neonatal Nurs. 2007;36(6):523–530. doi: 10.1111/j.1552-6909.2007.00184.x. [DOI] [PubMed] [Google Scholar]
- 58.Wuehler SE, El Hafed Ould Dehah CM. Situational analysis of infant and young child nutrition policies and programmatic activities in the Islamic Republic of Mauritania. Matern Child Nutr. 2011;7(S1):113–132. doi: 10.1111/j.1740-8709.2010.00308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Conti-Ramsden G, Durkin K. Language development and assessment in the preschool period. Neuropsychol Rev. 2012;22(4):384–401. doi: 10.1007/s11065-012-9208-z. [DOI] [PubMed] [Google Scholar]
- 60.World Health Organization Care for child development: Improving the care of young children. http://www.who.int/maternal_child_adolescent/documents/care_child_development/en/index.html Published 2012.