Abstract
Background
Optic neuritis is an inflammatory disease of the optic nerve. It occurs more commonly in women than in men. Usually presenting with an abrupt loss of vision, recovery of vision is almost never complete. Closely linked in pathogenesis to multiple sclerosis, it may be the initial manifestation for this condition. In certain patients, no underlying cause can be found.
Objectives
To assess the effects of corticosteroids on visual recovery of patients with acute optic neuritis.
Search methods
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register) (The Cochrane Library 2012, Issue 1), MEDLINE (January 1950 to February 2012), EMBASE (January 1980 to February 2012), Latin American and Caribbean Literature on Health Sciences (LILACS) (January 1982 to February 2012), the metaRegister of Controlled Trials (mRCT) (www.controlled-trials.com), ClinicalTrials.gov (www.clinicaltrials.gov) and the WHO International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en). There were no date or language restrictions in the electronic searches for trials. The electronic databases were last searched on 21 February 2012. We also searched reference lists of identified trial reports to find additional trials.
Selection criteria
We included randomized trials that evaluated corticosteroids, in any form, dose or route of administration, in people with acute optic neuritis.
Data collection and analysis
Two authors independently extracted the data on methodological quality and outcomes for analysis.
Main results
We included six randomized trials which included a total of 750 participants. Two trials evaluated low dose oral corticosteroids while one trial evaluated low dose intravenous corticosteroids across two treatment arms and two trials evaluated a higher dose of intravenous corticosteroids. One three-arm trial evaluated low-dose oral corticosteroids and high-dose intravenous corticosteroids against placebo. Trials evaluating oral corticosteroids compared varying doses of corticosteroids with placebo. Hence, we did not conduct a meta-analysis of such trials. In a meta-analysis of trials evaluating corticosteroids with total dose greater than 3000 mg administered intravenously, the relative risk of normal visual acuity with intravenous corticosteroids compared with placebo was 1.06 (95% confidence interval (CI) 0.89 to 1.27) at six months and 1.06 (95% CI 0.92 to 1.22) at one year. The risk ratio of normal contrast sensitivity for the same comparison was 1.10 (95% CI 0.92 to 1.32) at six months follow up. We did not conduct a meta-analysis for this outcome at one year follow up since there was substantial statistical heterogeneity. The risk ratio of normal visual field for this comparison was 1.08 (95% CI 0.96 to 1.22) at six months and 1.02 (95% CI 0.86 to 1.20) at one year. Quality of life was assessed and reported in one trial.
Authors' conclusions
There is no conclusive evidence of benefit in terms of recovery to normal visual acuity, visual field or contrast sensitivity with either intravenous or oral corticosteroids at the doses evaluated in trials included in this review.
Medical Subject Headings (MeSH): Adrenal Cortex Hormones [*therapeutic use], Contrast Sensitivity [drug effects], Optic Neuritis [*drug therapy], Randomized Controlled Trials as Topic, Visual Acuity [drug effects]
MeSH check words: Humans
Background
Description of the condition
Optic neuritis is an inflammatory disease of the optic nerve. It is second only to glaucoma as the most common acquired optic nerve disorder in persons under 50 years. The majority of patients with optic neuritis are between the ages of 20 and 50 years, with a mean age around 30 to 35 years. In population-based studies the annual incidence of optic neuritis in the US has been estimated to be between 1 and 5/100,000 (Beck 1998). Koch-Henriksen and Hyllested reported an annual incidence of 4 to 5/100,000 for new onset optic neuritis cases in Denmark in 1948 to 1964 (Koch-Henriksen 1988). In Olmstead County, Minnesota, USA the prevalence rate of optic neuritis was estimated as 115/100,000 (Rodriguez 1995). Women are more likely to be affected than men. Optic neuritis is closely linked to multiple sclerosis (MS) and in most cases has a similar pathogenesis. It may be the first manifestationof multiple sclerosisor occur later inits course (Ebers 1985).
The presenting symptom is usually abrupt visual loss in one eye over several hours or days, accompanied by mild pain. Symptoms can also occur in both eyes either simultaneously or sequentially. A clinical diagnosis of optic neuritis may be made based on the following: age between 18 and 45 years, sudden visual loss with progression for less than one week, pain on eye movement, no inflammation in the vitreous or anterior chamber, and improvement in vision that begins within three to four weeks. The prognosis for visual recovery after acute optic neuritis is generally good. However, most patients have some lasting visual impairment. Even when a patient's visual acuity does return to normal, abnormalities frequently remain in other measures such as contrast sensitivity, color vision, and visual field (Fleishman 1987; Sanders 1986).
Description of the intervention
Although corticosteroids have been used since the early 1950s to treat acute optic neuritis because of their anti-inflammatory effects, studies to demonstrate their effectiveness have not been satisfactory. Some experts advocated treatment with oral prednisone while others recommended no or other treatment. In the 1980s, anecdotal reports suggested that high-dose intravenous corticosteroids might be effective (Spoor 1988). In 1992, the National Eye Institute of the US National Institutes of Health funded a randomized controlled trial to test the efficacy of corticosteroids in the treatment of optic neuritis (ONTT 1992-2006). Based on results of this trial the current guidelines in the United States suggest either administration of high-dose intravenous methylprednisolone to hasten recovery of vision or no treatment. There are no other treatments with regard to recovery of vision in acute optic neuritis.
Why it is important to do this review
Prior to the Optic Neuritis Treatment Trial (ONTT) (ONTT 1992-2006), well-established guidelines for treating optic neuritis did not exist. Brusaferri and Candelise (Brusaferri 2000) published a meta-analysis of steroids for multiple sclerosis and optic neuritis with inclusion criteria for participants and treatment type different from those specified for this review. We systematically reviewed the evidence for the use of corticosteroid therapy in any form or dosage with the intention to treat or reduce the symptoms in patients with acute optic neuritis, compared with placebo or no treatment.
Objectives
The objective of this review was to assess the effects of corticosteroids on visual recovery of patients with acute optic neuritis.
Methods
Criteria for considering studies for this review
Types of studies
This review included only randomized controlled trials.
Types of participants
We included trials in which the participants had acute optic neuritis. There were no age limitations.
Types of interventions
We included trials in which the administration of corticosteroid therapy in any form or dosage with the intention to treat or reduce the symptoms of acute optic neuritis were compared to placebo, no treatment or other treatment. We did not limit inclusion of trials in this review based on the duration of treatment.
Types of outcome measures
Primary outcomes
The primary outcomes for this review were visual outcomes measured as:
Proportion of people with normal visual acuity at six months or more;
Proportion of people with normal contrast sensitivity at six months or more;
Proportion of people with normal visual field at six months or more.
Secondary outcomes
Secondary outcomes were immediate response (rate of recovery) measured as:
Proportion of people with normal visual acuity at one month;
Proportion of people with normal contrast sensitivity at one month;
Proportion of people with normal visual field at one month. We summarized adverse outcomes related to treatment with corticosteroids. When available, we planned to summarize data on quality of life.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) 2012, Issue 1, part of The Cochrane Library. www.thecochranelibrary.com (accessed 21 February 2012),MED-LINE (January 1950 to February 2012), EMBASE (January 1980 to February 2012), Latin American and Caribbean Literature on Health Sciences (LILACS) (January 1982 to February 2012), the metaRegister of Controlled Trials (mRCT) (www.controlled-trials.com), ClinicalTrials.gov (www.clinicaltrials.gov) and the WHO International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en). There were no language or date restrictions in the search for trials. The electronic databases were last searched on 21 February 2012.
See: Appendices for details of search strategies for CENTRAL (Appendix 1), MEDLINE (Appendix 2), EMBASE (Appendix 3), LILACS (Appendix 4), mRCT (Appendix 5), ClinicalTrials.gov (Appendix 6) and the ICTRP (Appendix 7).
Searching other resources
We searched the reference lists of identified trial reports to find additional trials and use the Science Citation Index to find studies that have cited the identified trials. We contacted investigators to identify additional published and unpublished studies. We did not conduct manual searches of conference proceeding abstracts specifically for this review.
Data collection and analysis
Selection of studies
Two review authors independently assessed the titles and abstracts of all reports identified by the electronic and other searches. We retrieved the full articles of potentially or definitely relevant studies and reviewed these according to the definitions in the ‘Criteria for considering studies for this review’. For non-English trials identified as potentially relevant, we translated the methods and results sections and then assessed the studies for inclusion. We categorized the reports as exclude, or unclear, or include. We excluded trial reports identified by both review authors as ‘exclude’ and documented the reasons for exclusion for trials excluded after full-text review in the ‘Characteristics of excluded studies’ table. A third review author resolved any disagreements.
Data extraction and management
We extracted data on the study characteristics, such as details of participants, the interventions, the outcomes, cost and quality of life data if available, and other relevant information.
Two review authors independently extracted data onto paper data collection forms and one review author double-entered the data into RevMan 4.2. During the update to this review, additional data were entered by one review author using RevMan 5.1(Review Manager 2011) and a second review author verified all values.
Assessment of risk of bias in included studies
Two review authors unmasked to the trialists, institutions and trial results assessed included studies for risk of bias according to methods set out in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). A third review author resolved any disagreements. We evaluated the studies for the following domains: sequence generation and allocation concealment (selection bias), masking of patients and outcome assessors (performance and detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other sources of bias. We reported the judgment for each domain as ‘Low risk’, ‘High risk’, or ‘Unclear risk’. We excluded trials that were judged to be ‘inadequate’ (high risk of bias) on randomization or allocation concealment. We contacted study investigators for additional information on issues that were unclear from information available in the original report. If the investigators did not respond within six weeks or if we were not able to communicate with them, we assigned a grade to the trial based on the information available.
Measures of treatment effect
We calculated summary risk ratios with 95% confidence intervals.
Unit of analysis issues
The unit of analysis was the individual participant for all outcomes.
Dealing with missing data
We contacted the primary authors of included studies to provide missing data such as standard deviations and intention-to-treat data. We used available data as reported in the original report If there was no response within six weeks.
Assessment of heterogeneity
We used the I2 statistic (%) to determine the proportion of variation due to heterogeneity with a value above 50% suggesting considerable statistical heterogeneity. We also examined the result of the Chi2 test for heterogeneity and the degree of overlap in confidence intervals of included studies. Poor overlap may also suggest the presence of heterogeneity. We assessed clinical heterogeneity by examining potential variations in participant characteristics, inclusion/exclusion criteria, and assessments of primary and secondary outcomes.
Assessment of reporting biases
We examined funnel plots to assess reporting biases. This was used in conjunction with study characteristics or other factors that may contribute to asymmetry of the funnel plot.
Data synthesis
If no statistical heterogeneity was detected and there was no clinical heterogeneity within the trials we summarized the results of the studies using risk ratios with 95% confidence intervals. We used a random-effects model or if there was no substantial heterogeneity (I2 > 50%). We used a fixed-effect model if there was no heterogeneity or there were fewer than three trials in the comparison.
Subgroup analysis and investigation of heterogeneity
We did not conduct subgroup analyses.
Sensitivity analysis
We did not conduct sensitivity analyses to determine the impact of exclusion of lower quality methodological studies, exclusion of unpublished studies, and exclusion of industry-funded studies because there were not enough studies.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Studies assessed for inclusion are described in the Characteristics of included studies and Characteristics of excluded studies tables.
Results of the search
The electronic searches identified 815 titles and abstracts. We screened the titles and abstracts according to the criteria outlined above and identified 51 potential trial reports. We obtained the full copies of these for further assessment. Twenty-nine were reports on different aspects of the included trials. One was a duplicate citation. We excluded 18 studies after a detailed review of the full text. Reasons for exclusion are listed in the ‘Characteristics of excluded studies’. Three studies that were awaiting further assessment as of the last publication of this review were translated in July 2010 and found not to be eligible for inclusion. These three studies have also been added to the ‘Characteristics of excluded studies’ table. We identified one eligible trial in the planning phase from ClinicalTrials.gov (NCT01524250) which is described in the ‘Characteristics of ongoing studies’ table. The databases were last searched in February 2012.
Included studies
We included six trials which randomized a total of 750 participants. Detailed characteristics of the included studies are presented in the ‘Characteristics of included studies’ table. A brief comment on variability between different trial characteristics is presented here.
Types of participants
Four trials (Kapoor 1998; ONTT 1992-2006; Menon 2007; Tubingen 1993) restricted inclusion to only those participants with no history of prior attacks of optic neuritis in the affected eye. Kapoor 1998 included only patients with confirmed multiple sclerosis, while the remaining trials included people with optic neuritis of unknown and demyelinating etiologies. Most trials included participants with a short duration of onset of visual symptoms. Participants had visual symptoms for less than two weeks in ONMRG 1999, less than eight days in ONTT 1992-2006, within eight days in Menon 2007, less than four weeks in Sellebjerg 1999 and less than three weeks in Tubingen 1993. Kapoor 1998, Menon 2007, and ONTT 1992-2006 specifically reported exclusion of participants with past history of optic neuritis in the same eye. Participants with a history of treatment with corticosteroids were excluded in Menon 2007, ONMRG 1999, ONTT 1992-2006, Sellebjerg 1999 and Tubingen 1993.
Types of interventions
The trials varied in the interventions compared, both in route of administration and dose administered. Intravenous methylprednisone was compared with placebo in Kapoor 1998. Intravenous dexamethasone was compared with intravenous methylprednisolone plus oral prednisolone in Menon 2007. Intravenous methylprednisone followed by tapering with oral prednisone was compared with placebo in ONTT 1992-2006 and ONMRG 1999. One of the three treatment arms in ONTT 1992-2006 administered oral prednisone while Sellebjerg 1999 and Tubingen 1993 compared oral methylprednisolone with placebo. Description of doses of corticosteroids evaluated in each of the trials in the text of the review refers to the total dose administered over the course of the entire regimens. The regimens in the individual trials are described in the ‘Characteristics of included studies’ table in greater detail.
The total dose of corticosteroid administered to patients in the treatment arms in the included trials varied from 200mginMenon 2007 to more than 3770 mg in the intravenous corticosteroid arm of the ONTT 1992-2006.
The control intervention was intravenous mecobalamin (B12) in ONMRG 1999 and oral thiamine (B1) in Tubingen 1993. Because of systemic treatment administration, randomization was by patient.
Types of outcomes
All trials examined and reported visual acuity as an outcome. Sellebjerg 1999 did not assess visual field in a systematic manner (personal communication with Dr. Sellebjerg) and contrast sensitivity was not reported in Tubingen 1993. There was also variability in the method employed to assess different outcomes as noted in the ‘Characteristics of included studies’ table.
Menon 2007 presented mean values for visual acuity, visual field (data not shown in report), and contrast sensitivity instead of defining normal values for each. Normal visual acuity was defined as 20/20 in all other included studies, normal visual field was defined as greater than -3.00 db, and measurement of contrast sensitivity was variable. Normal contrast sensitivity was defined as greater than 1.65 log units in ONTT 1992-2006 and ONMRG 1999. Sellebjerg 1999 measured contrast sensitivity using Arden gratings and defined normal as less than or equal to 80 points. Kapoor 1998 considered normal contrast sensitivity to be greater than 1.35 db.
Excluded studies
We excluded the remaining 21 studies, listed in the ‘Characteristics of excluded studies’ table with reasons for exclusion.
Risk of bias in included studies
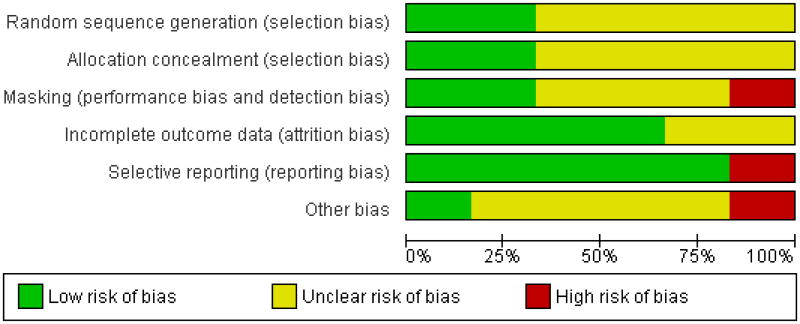
Figure 1 and Figure 2 present a summary of the risk of bias for the included studies.
Figure 1. Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
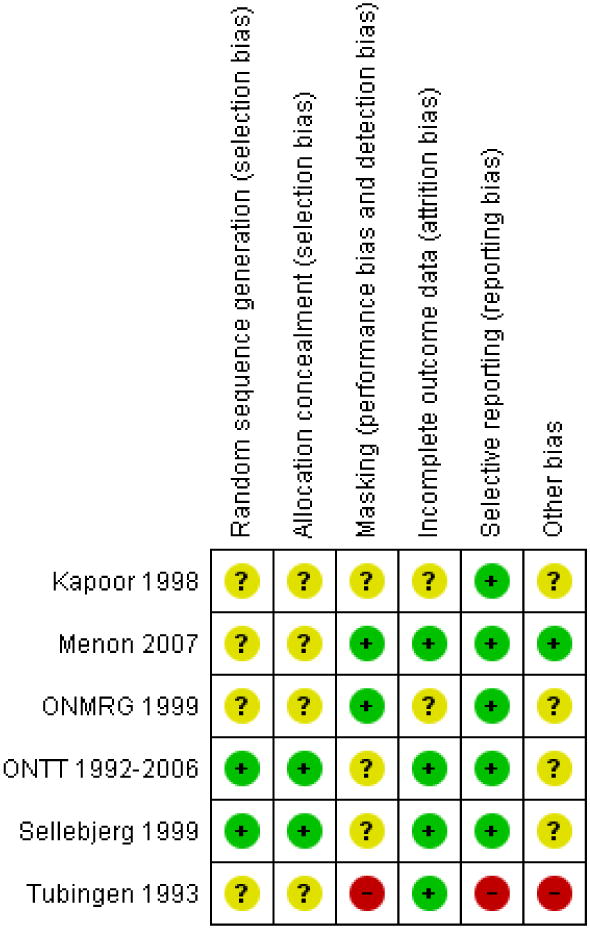
Figure 2. Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Random sequence generation (selection bias)
All trials were randomized, but only four reported the method of sequence generation (Menon 2007; ONMRG 1999; ONTT 1992-2006; Tubingen 1993). Block randomization was reported in three trials (Menon 2007; ONTT1992-2006; Sellebjerg 1999). However, the contact author of one trial (Menon 2007) reported they tossed a coin to initiate randomization sequence followed by alternating group allocation. Tubingen 1993 reported randomization sequence was generated by a pharmaceutical company though the specific method used was not reported.
Allocation
Of the six trials, three reported the method of allocation concealment in the published manuscript (ONMRG 1999; ONTT 1992-2006; Sellebjerg 1999). Two trials used numbered envelopes (ONMRG 1999; Sellebjerg 1999) but did not report whether they were sequentially numbered and opaque. One trial used a variation of sealed envelopes with information regarding each patient's allocated treatment (ONTT 1992-2006).
Masking (performance bias and detection bias)
Outcome assessment in three included trials was conducted in a masked fashion Menon 2007; ONMRG 1999; ONTT 1992-2006); except one of the three arms in ONTT 1992-2006 where the outcome assessors were not masked for the intravenous corticosteroid group.
In one trial, a group of non-randomized participants were allowed to choose their intervention although all outcome assessment was done in a masked manner (Tubingen 1993). Two trials reported the trial as “double-blind” or that the visual assessment was done by a technician who was unaware of the participant's treatment (Kapoor 1998; Sellebjerg 1999).
Incomplete outcome data
Two trials reported no loss to follow-up through six months (Menon 2007) and twelve months (ONMRG 1999); although not all participants were evaluated for all reported outcomes in ONMRG 1999. Three trials reported equal numbers of missing data across all treatment arms (Kapoor 1998; Sellebjerg 1999; and Tubingen 1993). One trial reported the total percentage of missing data, but did not report how they were distributed across treatment arms (ONTT 1992-2006).
Selective reporting
Both ONTT 1992-2006 and Sellebjerg 1999 reported primary and secondary outcomes of interest and were judged to have a ‘low risk’ of bias for selective outcome reporting. Three other trials (Kapoor 1998; Menon 2007; ONMRG 1999) were also judged to have a ‘low risk’ of bias for selective outcome reporting for reporting all outcomes described in the report. One trial (Tubingen 1993) was judged to have a ‘high risk’ of bias for adding additional unmasked patients following randomization to the analysis as well as altering the original analysis plan due to the length of time for “normalization” to occur.
Other potential sources of bias
Three trials reported receiving funding or study medication from the pharmaceutical industry and were judged to have an ‘unclear risk’ of bias because of this (ONTT 1992-2006; Sellebjerg 1999; Tubingen 1993). Two trials reported deviations in the analysis plan after looking at the results (Kapoor 1998; Tubingen 1993) and one trial used a different unit of analysis than what was used at the unit of randomization for some reported outcomes (ONMRG 1999).
Effects of interventions
After examining the included studies we determined that analysis of all included trials in a single meta-analysis was not clinically meaningful because the corticosteroids were administered in different doses and routes, constituting clinical heterogeneity. Studies evaluating oral administration of corticosteroids for optic neuritis were clinically heterogeneous since widely varied doses were evaluated in each trial. The total dose of oral corticosteroids administered was 355 mg, 3676 mg, and 1200 mg in Tubingen 1993, Sellebjerg 1999 and oral arm of ONTT 1992-2006, respectively.
For the purposes of this review, we conducted meta-analyses of trials with a total intravenous dose of 3000 mg corticosteroids or more including the IV arm of ONTT 1992-2006 (3770 mg), ONMRG 1999 (> 3000 mg) and Kapoor 1998 (3000 mg). These trials varied in the outcomes reported at different time points and thus data from all three trials were not available for all analyses.
Intravenous corticosteroids (total dose ≥ 3000 mg) versus placebo
Visual acuity
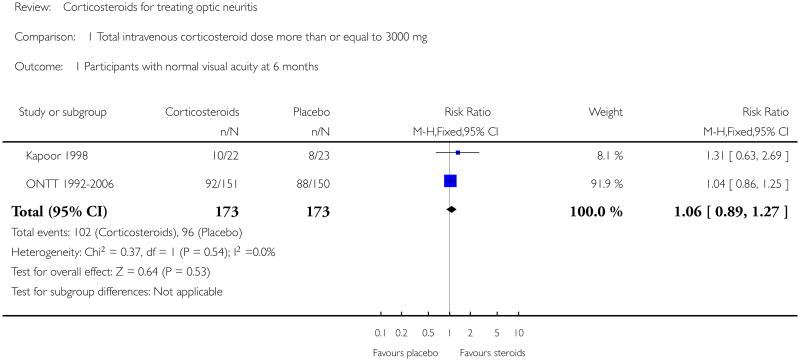
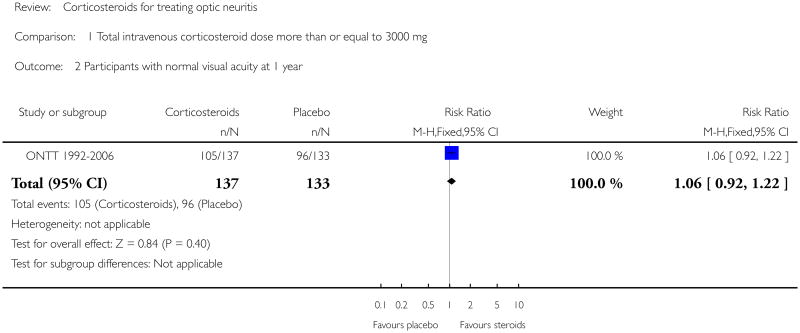
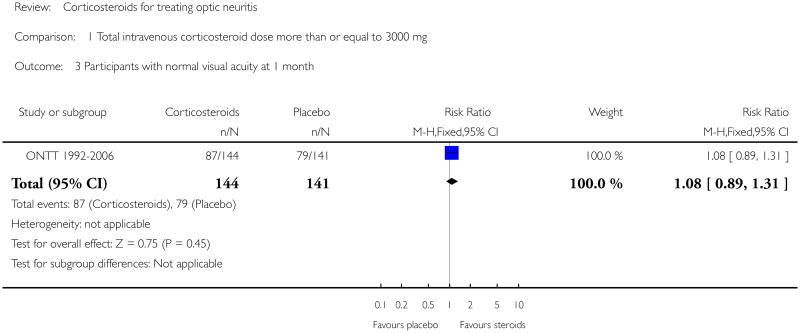
In a meta-analysis f trials evaluating corticosteroids of dose greater than 3000 mg administered intravenously, the risk ratio of normal visual acuity at six months follow up was 1.06 (95% confidence interval (CI) 0.89 to 1.27) (Analysis 1.1). The meta-analysis for this outcome included Kapoor 1998 and ONTT 1992-2006. There was no substantial statistical heterogeneity at any of the time-points for this outcome. The risk ratio of normal visual acuity was 1.06 (95% CI 0.92 to 1.22) at one year (Analysis 1.2), 1.08 (95% CI 0.89 to 1.31) (Analysis 1.3) at one month and included data from only ONTT (ONTT 1992-2006).
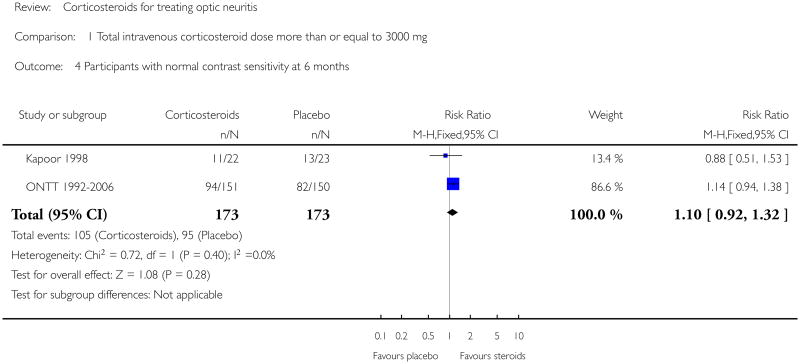
Contrast sensitivity
In a meta-analysis of Kapoor 1998 and ONTT 1992-2006, the risk ratio of normal contrast sensitivity was 1.10 (95% CI 0.92 to 1.32) at six months follow up (Analysis 1.4). There was no substantial statistical heterogeneity. At one year, data on normal contrast sensitivity were available only from ONMRG 1999 and ONTT 1992-2006.
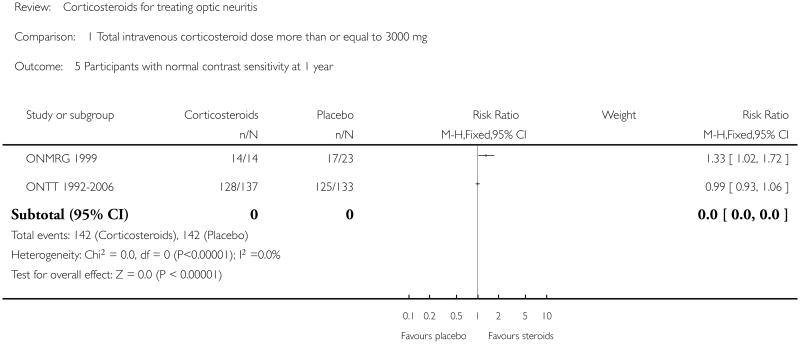
We do not report a meta-analysis for this outcome at one year since there was substantial statistical heterogeneity as evident from the I2 value of 83.4% and a P value of 0.01 for the Chi2 test for heterogeneity. The risk ratio of normal contrast sensitivity at one year follow up was 1.35 (95% CI 1.06 to 1.72) in ONMRG 1999 and 0.99 (95% CI 0.93 to 1.06) in ONTT 1992-2006 (Analysis 1.5).
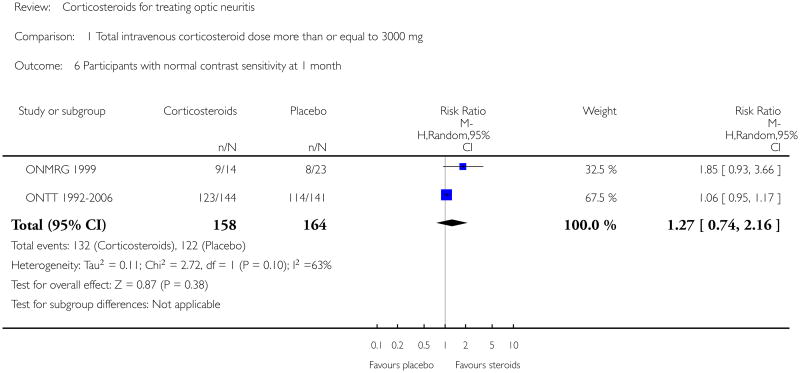
Similarly, we found substantial heterogeneity on this outcome at one month with data from ONMRG 1999 and ONTT 1992-2006 (I2 = 63.3% and P value for Chi2 test = 0.10). Though the P value for the Chi2 test is greater than 0.05, the test has low power with fewer studies and since the I2 value and the point estimates indicate presence of heterogeneity, we prefer not to report the meta-analysis. The risk ratio of normal contrast sensitivity at one month was 1.85 (95% CI 0.93 to 3.66) in ONMRG 1999 and 1.06 (95% CI 0.95 to 1.17) in ONTT 1992-2006 (Analysis 1.6).
Visual field
Data on visual field at six months was available from Kapoor 1998 and ONTT 1992-2006. The pooled risk ratio of normal visual field at six months follow up was 1.08 (95% CI 0.96 to 1.22) (Analysis 1.7). The P value for Chi2 test for heterogeneity was 0.84 and the I2 value was 0%. For analyses at one year and one month data were available from ONMRG 1999 and ONTT 1992-2006. At one year the pooled risk ratio of normal visual field was 1.02 (95% CI 0.86 to 1.20) (Analysis 1.8). The pooled relative risk was 1.43 and statistically significant in favor of intravenous corticosteroids (95% CI 1.12 to 1.84) at one month follow up (Analysis 1.9). There was no statistical heterogeneity in these analyses.
Intravenous dexamethasone versus intravenous methylprednisolone followed by oral prednisone
Visual acuity
One trial (Menon 2007) reported LogMAR mean values for visual acuity for both treatment arms. At one month follow-up the mean±SD in the methylprednisolone group was 0.42±0.42 and 0.29±0.29 in the dexamethasone group (P = 0.36). At three months of follow-up the mean±SD was 0.36±0.41 and 0.28±0.33 in the methylprednisolone and dexamethasone groups respectively (P = 0.56).
Contrast sensitivity
At one month of follow-up, mean±SD contrast sensitivities (by Pelli-Robson chart) were 1.16±0.48 and 1.25±0.43 (P = 0.61) in the methylprednisolone and dexamethasone treatment groups respectively. The mean±SD was 1.26±0.41 in the methylprednisolone group and 1.37±0.29 in the dexamethasone group (P = 0.42) at three months follow-up.
Visual field
Limited data were available from Menon 2007 regarding visual field outcomes. Of the two patients in the methylprednisolone group that it was possible to chart visual fields, both had a central scotoma observed in pretreatment visual field assessment. Following treatment at three months follow-up, the central scotoma failed to fully recover in one patient. In the dexamethasone treatment group, visual fields for six patients were assessed and four were determined to have a central scotoma. At three months follow-up, two patients failed to fully recover.
Oral corticosteroids versus placebo
Visual acuity
We did not conduct a meta-analysis for this outcome (Analysis 2.1). The relative risk for normal visual acuity at 6 months was 0.93 (95% CI 0.76 to 1.13) in ONTT 1992-2006 and 0.89 (95% CI 0.55 to 1.42) in Tubingen 1993. Relative risk of normal visual acuity at one year in ONTT 1992-2006 was 0.76 and was statistically significant in favor of placebo (95% CI 0.63 to 0.92). Relative risk of normal visual acuity at one year was 1.09 (95% CI 0.82 to 1.44) in Tubingen 1993 and 1.10 (95% CI 0.67 to 1.80) in Sellebjerg 1999. Relative risk of normal visual acuity at one month did not achieve statistical significance in any of the three trials. The relative risk was 0.95 (95% CI 0.77 to 1.18) in ONTT 1992-2006, 1.65 (95% CI 0.75 to 3.64) in Tubingen 1993 and 1.21 (95% CI 0.56 to 2.63) in Sellebjerg 1999.
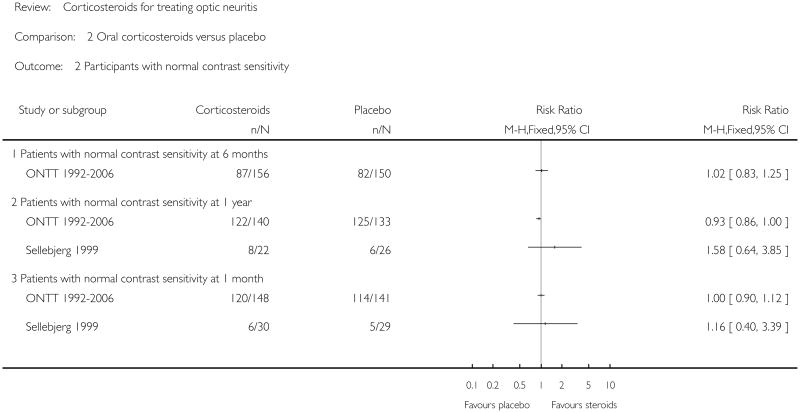
Contrast sensitivity
We report findings specific to contrast sensitivity in Analysis 2.2. ONTT 1992-2006 was the only trial that reported contrast sensitivity at six months (RR 1.02; 95% CI 0.83 to 1.25). The relative risk of normal contrast sensitivity at one year was 0.93 (95% CI 0.86 to 1.00) in ONTT 1992-2006 and 1.58 (95% CI 0.64 to 3.85) in Sellebjerg 1999. Relative risk of normal contrast sensitivity at one month was 1.00 (95% CI 0.90 to 1.12) in ONTT 1992-2006 and 1.16 (95% CI 0.40 to 3.39) in Sellebjerg 1999.
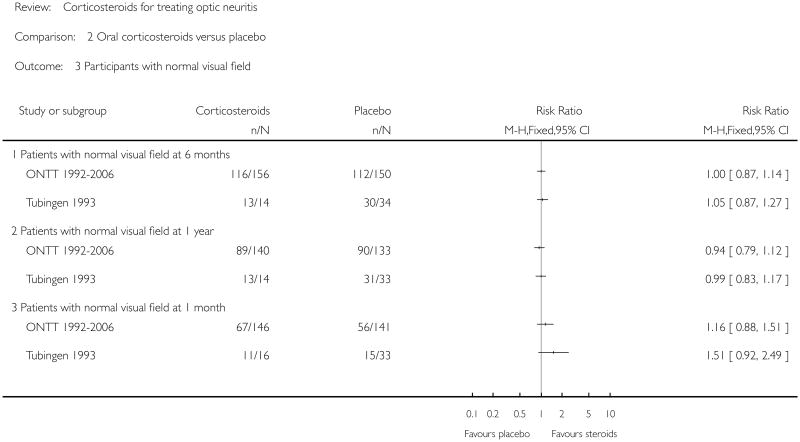
Visual field
None of the trials achieved statistical significance for this outcome (Analysis 2.3). The relative risk for normal visual field at six months was 1.00 (95% CI 0.87 to 1.14) in ONTT 1992-2006 and 1.05 (95% CI 0.87 to 1.27) in Tubingen 1993. Relative risk of normal visual field at one year was 0.94 (95% CI 0.79 to 1.12) in ONTT 1992-2006 and 0.99 (95% CI 0.83 to 1.17) in Tubingen 1993. Relative risk of normal visual field at one month was 1.16 (95% CI 0.88 to 1.51) in ONTT 1992-2006 and 1.51 (95% CI 0.92 to 2.49) in Tubingen 1993.
Adverse effects
Adverse effects were reported in four of the five included trials. Kapoor 1998 did not report adverse effects. Sellebjerg 1999 reported no serious adverse effects and Tubingen 1993 reported only acne. The ONMRG 1999 reported hyperglycemia, constipation, diarrhea, acneiform eruption, hyperlipidemia, headache, and fever. The ONTT 1992-2006 reported depression, acute pancreatitis, weight gain, sleep disturbance, mild mood change, stomach upset, and facial flushing. The proportion of participants experiencing adverse effects of corticosteroid therapy was not consistently reported by all trials, thereby precluding any comparison.
Quality of life
Quality of life was assessed and reported only in ONTT 1992-2006 using patient-reported responses to the National Eye Institute Visual Functioning Questionnaire (NEI-VFQ) (Mangione 1998). However, no comparative quality of life data by assigned treatment arm were available.
Discussion
Summary of main results
Acute demyelinating optic neuritis is a common form of optic neuritis, with inflammation of the optic nerve that may be associated with multiple sclerosis. Optic neuritis may be the initial manifestation of multiple sclerosis in some patients (Kurtzke 1985). In this systematic review evaluating the effects of corticosteroid therapy in patients with optic neuritis, we included six randomized controlled trials. We did not conduct a meta-analysis including all trials because of clinical heterogeneity resulting from variations in doses and routes of administration of corticosteroids. However, we conducted a meta-analysis of trials evaluating similar doses of corticosteroids (3000 mg or more) administered by the intravenous route. The ONTT (ONTT 1992-2006) was the largest of the included studies and contributed to most of the weight in all the meta-analyses. While none of the other included trials reported an evidence of benefit with intravenous corticosteroids, the results of their analyses were consistent with those in the ONTT (ONTT 1992-2006). Due to inverse variance weighting adopted in our meta-analyses, the smaller trials received much less weight compared with ONTT (ONTT 1992-2006).
The 95% confidence intervals for the pooled risk ratios of normal visual acuity, normal contrast sensitivity, and normal visual field at six months for the intravenous corticosteroids arm in ONTT (ONTT 1992-2006) include the null value. This suggests no evidence of benefit with either oral or intravenous corticosteroids compared to placebo for the outcomes described above. This observation is consistent with the adjusted analyses for the ONTT (ONTT 1992-2006) when adjusted for baseline visual acuity (ONTT 1992-2006). However, a life-table analysis reported in the same manuscript found that the rate of return of vision to normal was higher with intravenous corticosteroids compared with placebo (P = 0.09 for visual acuity, 0.02 for contrast sensitivity and 0.0001 for visual field). No statistically significant difference was found for the same outcomes for oral corticosteroids compared with placebo in a life-table analysis in the trial report. Further, patients treated with oral corticosteroids in the same trial had a higher rate of a new episode of optic neuritis compared with those in the placebo arm. A statistically significant benefit in terms of pooled relative risk of normal visual field at one month was observed in patients treated with intravenous corticosteroids (see Figure 9). Additionally, there was no evidence of benefit when intravenous corticosteroids were compared to intravenous followed by oral corticosteroids for the outcomes visual acuity and contrast sensitivity (Menon 2007).
The trials evaluating oral corticosteroids were very heterogeneous in the dose of the medication. There was no evidence of benefit with oral or intravenous corticosteroids for all outcomes considered. The 95% confidence intervals for the relative risk of normal visual acuity, contrast sensitivity and visual field included the null value. Oral corticosteroids, however, resulted in fewer patients achieving normal visual acuity compared with the placebo group at 1 year in ONTT 1992-2006 (see Figure 10). This difference was statistically significant.
Authors' Conclusions
Implications for practice
There is no conclusive evidence of benefit in terms of return to normal visual acuity, visual field or contrast sensitivity with either intravenous or oral corticosteroids at the doses evaluated by trials included in this review. Either no treatment or treatment with intravenous corticosteroid therapy followed by oral corticosteroids is appropriate; intravenous corticosteroids may benefit the patient in terms of faster recovery to normal vision. As suggested by analyses reported in the ONTT (ONTT 1992-2006), oral corticosteroid therapy may be associated with an increase in rate of new episodes of optic neuritis.
Implications for research
Among patient cohorts evaluated as part of this review, there was no conclusive treatment benefit with return to normal visual function measures as the outcome of interest. Future research efforts could focus on the identification of patient subgroups who might be predisposed to have permanent visual deficits and would benefit from some type of pharmacologic therapy which could reduce neural damage.
While neurological outcome was not the outcome of interest in this review, there are related areas, which may warrant future exploration. Future research to evaluate the role of high dose oral corticosteroids as a treatment option for optic neuritis may be warranted.
Plain Language Summary.
Corticosteroids for treating optic neuritis
Optic neuritis is an inflammatory disease of the optic nerve characterized by sudden vision loss over several hours or days. The objective of this review was to assess the effectiveness of corticosteroids for acute optic neuritis. We included six randomized controlled trials (750 participants) conducted in Denmark, Germany, India, Japan, UK, and USA. These trials compared corticosteroid therapy to placebo or other treatment with variations in the route of administration and dose administered. At six months and one year, participants randomized to corticosteroids were more likely to have normal vision, contrast sensitivity (ability to distinguish fine changes in the shading of letters on an eye chart), and visual field (area visible when looking straight ahead) compared to participants receiving placebo, but these differences were not clinically meaningful. Adverse effects, although not consistently reported, included acne, high blood sugar, gastrointestinal problems, headache, fever, and sleep and mood disturbances. The findings suggest that there is no evidence of benefit with either oral or intravenous corticosteroids compared to placebo for the outcomes visual acuity, visual field, and contrast sensitivity.
Acknowledgments
Kay Dickersin, PhD, was instrumental in conception of this review and Suzanne Brodney-Folse (SBF) and Satyanarayana Vedula (SSV) contributed as co-authors on the protocol and original version of this review. We are grateful to Graziella Filippini for peer review comments on the protocol for this review. Karen Blackhall and Iris Gordon at the editorial base of the Cochrane Eyes and Vision Group prepared and executed the electronic searches and Anupa Shah provided comments, guidance and support. We acknowledge assistance provided by Fabio Brusaferri and Livia Candelise in developing the protocol for this review. We thank Richard Wormald, Roberta Scherer, Kate Henshaw, Barbara Hawkins and Catey Bunce for their comments and input on earlier versions of this review. We acknowledge assistance and coordination provided by Stephen Gichuhi, Michael Marrone, Sueko Matsumura, and others at the Cochrane Eyes and Vision Group (CEVG) Editorial Base and CEVG US Project.
Richard Wormald (Co-ordinating Editor for CEVG) acknowledges financial support for his CEVG research sessions from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology. The views expressed in this publication are those of the authors and not necessarily those of the Department of Health.
Sources of Support
Internal sources:
Brown University, USA.
Johns Hopkins University, USA.
External sources:
Contract N-01-EY-2-1003 and Grant 1 U01 EY020522-01, National Eye Institute, National Institutes of Health, USA.
Characteristics of Studies
Characteristics of included studies [ordered by study ID]
Kapoor 1998.
| Methods | Method of
randomization: “Randomized” (method not
specified) Number randomized: 66 Exclusions after randomization: None Losses to follow up: 2 at last follow up (6 months) Method of allocation concealment: “Randomization was coordinated by the Hospitalpharmacy and the coding was not accessible to clinicians or patients taking part in thestudy until the data came to analysis” (Personal communication) Participant masking: YesProvider masking: YesOutcome assessor masking: Yes Intention to treat analysis: No |
|
| Participants | Country and period
of study: United Kingdom (March 1991 to June
1994) Age: 18 to 50 Sex: Short lesions: Overall, 74% were female |
|
| Interventions | Treatment:
Intravenous methylprednisolone (1 g/day given as a single
bolus) for 3 days Control: Intravenous saline for 3 days |
|
| Outcomes | Visual
acuity Contrast sensitivity (measured using circular patches of luminance modulated vertical sinewave gratings) Visual field (Humphrey automatic perimetry using 30-2 protocol) |
|
| Notes | Follow up at 4, 8 weeks and 6 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation was not reported |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment was not reported |
| Masking (performance bias and detection bias) | Unclear risk | “Patients in either subgroup were randomized double blind to receive IV saline or IVMP”; but specific details of masking was not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | “Sixty-four of 66
patients completed 6 months' clinical follow-up (33
treated, 31 placebo)” “The MRI was repeated after 6 months in 61 of 66 patients” “VEPs were repeated after 6 months in 43 of 66 cases” |
| Selective reporting (reporting bias) | Low risk | Outcomes reported were described in the methods section, though we did not have access to the original study protocol |
| Other bias | Unclear risk | “Because treatment did not appear to influence outcome, some of the results obtained in the treated and placebo groups were analyzed together” |
Menon 2007.
| Methods | Method of
randomization: coin toss followed by alternating group
assignment Number randomized: 21 Exclusions after randomization: no exclusions after randomization Losses to follow up: no loss to follow up reported Method of allocation concealment: Not specified Participant masking: Yes (author communication) Provider masking: Unknown Outcome assessor masking: Yes (author communication) Intention to treat analysis:Unknown |
||
| Participants | Country and period
of study: Tertiary care center in India (Period
unknown) Age: 7 to 53 (mean Group I 31.2 + 10.1 years, mean Group II 26.6 + 11.5 years) Sex: Overall, 57% were male (Group I 55% male, Group II 60% male) Inclusion:
Exclusions:
Evidence of systemic condition for which corticosteroids would be contraindicated |
||
| Interventions | Group I (11
subjects) - Intravenous dexamethasone 200mg (in 150ml
5% dextrose solution) given over 1.5-2 hours once a
day for 3 days Group II (10 subjects) - Intravenous methylprednisolone 250mg/six hourly (in 150ml 5% dextrose solution) given over 1.5-2 hours once a day for 3 days followed by oral prednisolone for 11 days |
||
| Outcomes | Visual acuity
(ETDRS at 4 m distance and Snellen at 6 m
distance) Visual field (Goldmann perimeter) Contrast sensitivity (Pelli-Robson chart at 1 m) Color vision (Ishihara pseudoisochromatic color vision plates) Stereoacuity (Randot stereoacuity test, Wirt circle) Visually evoked response (Lace electronica EREV m99 machine at 33cm) Other: hemogram, fasting blood glucose, Venereal diseases research laboratory, immuno-histocytological analysis for toxoplasmosis, chest X-ray, X-ray paranasal sinuses, aerobic and anaerobic blood cultures, orbital ultrasound and neuroimaging for cases not showing any improvement with standard therapy in either group |
||
| Notes | The study investigators were contacted for the proportion of patients with normal visual acuity, visual field, and contrast sensitivity, but no additional data were available | ||
| Risk of bias | |||
| Bias | Authors' judgement | Support for judgement | |
| Random sequence generation (selection bias) | Unclear risk | According to the published report: “The patients were randomized into two groups by block randomization”. However, in correspondence with the author “The first case was decided by a toss of a coin. All subsequent were by rotation of patients (patients were alternatively assigned to group 1 and group 2)” | |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment was not reported | |
| Masking (performance bias and detection bias) | Low risk | Both patients and outcome assessors were masked (blinded) to the treatment assignment. - author correspondence | |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow-up reported | |
| Selective reporting (reporting bias) | Low risk | Results for all outcomes were reported | |
| Other bias | Low risk | ||
ONMRG 1999.
| Methods | Method of
randomization: “Randomly assigned by the envelope
method” Number randomized: 102 Exclusions after randomization (total and per group): 32 dismissed after start of study due to different reasons including misdiagnosis and lost data. 2 patients excluded before treatment, 2 more during treatment due to waiver of consent by the patients. (Final: 66 - 33 Treatment, 33 Control groups). Exclusions per group not explicitly stated Losses to follow up: No loss to follow up Method of allocation concealment: Serially numbered in sealed opaque envelopes Participant masking: Yes Provider masking: No (attending physician was informed of the intervention) Outcome assessor masking: Yes Intention to treat analysis: No |
||||||
| Participants | Country and period
of study: 22 centers in Japan (March 1991 to December
1996) Age: 14 to 58 (Mean 36.3 years) Sex: Overall, 69% were female |
||||||
| Interventions | Treatment:
Intravenous methylprednisolone (1 g/d) for 3 days followed
by oral corticosteroid for 7 to 10 days. Intravenous
administration was carried out over 45 to 60 minutes once a
day in the morning Control: Intravenous mecobalamin (500 ug/d) for 3 days, followed by oral mecobalamin for at least 7 days. Intravenous administration was carried out over 45 to 60 minutes once a day in the morning |
||||||
| Outcomes | Visual acuity
(Measured using Landolt rings at 5 m after full refractive
correction. Results expressed as decimal
activity) Visual field (Humphrey 30-2 for central 30 degrees of visual field and Goldmann perimetry for peripheral field if HFA unsuitable) Contrast sensitivity (Visual Contrast Test System at a testing distance of 1 m) |
||||||
| Notes | Data provided by
Masato Wakakura about allocation concealment and
outcomes Follow up at 1, 3, 4, 12 weeks and 12 months Four patients had definite or probable multiple sclerosis |
||||||
| Risk of bias | |||||||
| Bias | Authors' judgement | Support for judgement | |||||
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation was not reported | |||||
| Allocation concealment (selection bias) | Unclear risk | “treatment was randomly assigned by the envelope method” - details of envelopes (e. g. sequentially numbered, opaque, sealed, etc.) were not reported | |||||
| Masking (performance bias and detection bias) | Low risk | “In this study, it was the policy to inform neither the patient nor examiner which treatment was being used, although it was known by the attending physician” | |||||
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | “Data for 70 patients
were analyzed in the baseline study. Four patients were
subsequently eliminated just before the start of treatment
(n=2) or during treatment (n=2), because
they had decided not to give their
consent” “HFA mean deviation could be determined for only 46 cases…Color vision could be examined in 52 eyes in the first 12 weeks of the study…Contrast sensitivity data were obtained for 37 eyes. CFF was measured for 51 eyes” “No patient was required to drop out of the study” |
|||||
| Selective reporting (reporting bias) | Low risk | Results for all outcomes were reported | |||||
| Other bias | Unclear risk | Some data were presented by eyes rather than by the unit of randomization, which was the individual | |||||
ONTT 1992-2006.
| Methods | Method of
randomization: Randomized using permuted block design,
stratified by clinical center Number randomized: 457 Exclusions after randomization: 2 patients found ineligible after randomization were excluded Losses to follow up: 17 at 6 months Method of allocation concealment: Bottles with pills prepared at a central location with a numbered envelope-type sealed label. Intact label was verified on return of the same to the central area Participant masking: Yes except for IV group Provider masking: Yes except for IV group Outcome assessor masking: Not for IV group. Only 6 % of testing in both the oral treatment arms at 6 months was performed by an individual who randomized the patient. Intention to treat analysis: Yes |
|
| Participants | Country and period
of study: 15 centers in USA (July 1988 to June
1991) Age: 18 to 46, (mean 32 years) Sex: Overall, 77% were female |
|
| Interventions | Treatment 1:
Intravenous methylprednisolone 250 mg every 6 hrs for 3 days
followed by 1 mg/kg body weight of oral prednisone for 11
days Treatment 2: Oral prednisone 1mg/kg/day for 14 days, tapered with administration of 20 mg on day 15 and 10 mg on days 16 and 18 Control: Oral placebo 1 mg/kg/day for 14 days with similar treatment as oral corticosteroid group on days 15, 16 and 18 Adherence: All but 14 patients (3%) completed their course of treatment. Compliance was evaluated via comparison of the number of pills in each bottle returned to study headquarters, with the number expected from that participant |
|
| Outcomes | Visual acuity
(Retro illuminated Snellen ETDRS chart) Visual field (Humphrey Visual Field Analyzer and Goldmann perimeter) Contrast sensitivity (Pelli-Robson chart) Quality of life: Assessed using National Eye Institute Visual Function Questionnaire (NEI-VFQ) - administered 5 to 8 years after acute optic neuritis, again at 10 to 12 years, and again at 15 to 18 years after acute optic neuritis |
|
| Notes | Data provided by
the Jaeb Center for Health Research in personal
communication Follow up at days 4, 15; weeks 7, 13, 19; months 1, 6, 12; 2 and yearly thereafter |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A permuted-blocks design with a separate sequence for each clinical centers was used to assign patients randomly in equal numbers to three treatment groups” |
| Allocation concealment (selection bias) | Low risk | “Each bottle for the prednisone and placebo groups had a numbered envelope type sealed label, within which the actual contents of the bottle was identified for emergency purposes. On dispensing the medication a portion of the label was torn off and placed in the patient's chart. Upon completion of treatment, the portion of the label that had been removed was returned to the DCC, which verified that the correct bottle had been dispensed to the patient and that masking had not been compromised (i.e., label intact)” |
| Masking (performance bias and detection bias) | Unclear risk | “Patients in the
oral-prednisone and placebo groups were blinded to their
treatment assignment, whereas those in the
intravenous-methylprednisolone group were
not” “The personnel assessing visual function were always unaware of whether the patient was assigned to the placebo or prednisone group, and as often as possible they were unaware of whether the patient was receiving methylprednisolone” “When examining visual function in the patients in the intravenous-methylprednisolone group, technicians were unaware of the patient's treatment assignment during 86 percent of all follow-up visits overall and 94 percent of the six-month visits” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | “The overall rate of visits missed among the seven scheduled follow-up visits in the first six months was 3.4 percent.” - It was unclear how these were distributed across the treatment arms and for what reasons they missed the scheduled follow-up visits |
| Selective reporting (reporting bias) | Low risk | “Visual field and contrast sensitivity were the primary measures of outcome; visual acuity and color vision were secondary measures” |
| Other bias | Unclear risk | Study medication was provided by industry |
Sellebjerg 1999.
| Methods | Method of
randomization: Random number table; randomized in blocks of
10 using random numbers table and stratified as visual
acuity < 0.1 and visual acuity of at least
0.1 Number randomized: 60, 30 to treatment; 30 to control Exclusions after randomization: No exclusions Losses to follow up: 5 in treatment group (1 patient after eight weeks and 4 after one year); 4 in control group at one year Method of allocation concealment: Numbered sealed envelopes, unopened by investigators until all patients completed the trial Participant masking: Yes Provider masking: Yes Outcome assessor masking: Yes Intention to treat analysis: No |
|
| Participants | Country and period
of study: Denmark (August 1993 to January 1997) Age: 18 to 55 (median 32 years) Sex: 60% were female in treatment group and 63% were female in control group |
|
| Interventions | Treatment:
Methylprednisolone tablets 500 mg once daily for 5 days,
followed by 400, 300, 200, 100, 64, 48, 32, 16, 8 and 8 mg
on each of the 10 following days Control: Identical looking tablets for 15 days (not explicitly stated) |
|
| Outcomes | Visual acuity
(Snellen) Visual field not measured systematically (personal communication) Contrast sensitivity (Arden gratings. Normal defined as 80 points or less) |
|
| Notes | Dr. Sellebjerg
provided 12 month data in personal communication We used 3 week data for 1 month outcome because data not collected at 1 month Follow up at weeks 1, 3, 8 and 12 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Individual randomization in blocks of 10 was performed by the producer using a random numbers table. Consecutive patients were allocated to consecutive randomization numbers in each stratum” |
| Allocation concealment (selection bias) | Low risk | “The treatment assignment of each patient was concealed in a numbered, sealed envelope at the department of neurology and was not opened by the investigators before all patients had completed the trial” |
| Masking (performance bias and detection bias) | Unclear risk | “Visual function was tested by a technician unaware of the clinical status of the patient” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | “Five patients in the
methylprednisolone group and four placebo-treated patients
did not participate in the 1-year follow-up study. Follow-up
data on one patient from each treatment arm was censored
because interferon treatment was initiated within 1
year” “One patient in the methylprednisolone group discontinued treatment after 4 days due to nausea, migraine, and diarrhea. Another methylprednisolone-treated patient discontinued treatment after 10 days due to heartburn, abdominal discomfort, palpitations, dysphoria, and insomnia. One patient in the placebo group discontinued treatment after 2 days due to vertigo, vomiting, and headache, presumably caused by a demyelinating lesion in the brainstem” Study reported ITT analysis in the methods |
| Selective reporting (reporting bias) | Low risk | “The four primary
efficacy measures were the spatial vision and VAS scores at
the 1-week and 3-week
visits” “Secondary outcome measures were changes in spatial vision, color vision, and VAS scores; normalization of the visual acuity, color vision, and contrast sensitivity scores at the individual visits; and an increase of one point in the visual functional system of Kurtzke's Expanded Disability Status Scale (EDSS)” “The primary efficacy measures were chosen before unblinding. In patients with bilateral symptoms only, the results obtained in the eye with the worse baseline visual acuity were analyzed” |
| Other bias | Unclear risk | Funded by pharmaceutical industry |
Tubingen 1993.
| Methods | Method of
randomization: “Randomization list was made by the
pharmaceutical company” (personal communication with
Dr. Trauzettel-Klosinski) Number randomized: 44 of planned 100 patients were admitted and randomized to the study in 7 years Exclusions after randomization: 6 excluded after randomization due to poor adherence (3 in treatment and 3 in control group) Losses to follow up: 6 months: 1 treatment, 2 control; 12 months: 3 treatment, 3 control Method of allocation concealment: The randomization list, prepared by the pharmaceutical company and placed in a closed envelope was kept by a third person of the research group. It was not seen by the investigators before and during the evaluation of the data (personal communication) Participant masking: Yes except for 12 that were unmasked and chose the intervention they would receive (2 treatment, 10 control) Provider masking: Yes except for 12 that were unmasked and chose the intervention they would receive (2 treatment, 10 control) Outcome assessor masking: Yes Intention to treat analysis: No Unusual study design: 12 refused to participate under double-masked conditions and treated in unmasked manner but all were combined for data analysis |
|
| Participants | Country and period
of study: Germany (1980 to 1986) Age: Mean age was 30.5 years and 29 years in treatment and control groups respectively Sex: 69% were female in treatment group and 74% were female in control group |
|
| Interventions | Treatment: Oral
methylprednisolone for 24 days: 100, 80, 60, 40, 30, 20, 10,
5 mg for 3 days each Control: Oral Vitamin B1 for 24 days (100 mg/d) |
|
| Outcomes | Visual acuity
(Snellen) Visual Field (Tubingen manual perimetry: profile perimetry and kinetic perimetry) Contrast sensitivity not reported |
|
| Notes | Dr.
Trauzettel-Klosinski provided data for 1 month and 6 months
in personal communication Criteria for diagnosis of optic neuritis employed for this study: Unilateral reduction of vision occurring over hours or days, at least two objective impairments on visual function including reduced and uncorrectable visual acuity, central scotoma, and pathological result of Aulhorn flicker test in patients with atypical scotoma, afferent pupil defect, normal or swollen optic disc Patients in treatment and control groups were given prophylactic aluminium-magnesium-silicate-hydrate, 550 mg three times a day Follow up at 1, 2, 3, 4, 6, 8 weeks and 3, 4, 5, 6, 9, 12 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomization was not reported |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment was not reported |
| Masking (performance bias and detection bias) | High risk | “In addition, 12 ON
patients who refused to participate under double-blind
conditions, were treated in an unmasked manner, two with
methylprednisolone and 10 with vitamin B1 according to their
own choice” “In all patients their treatment assignment was not known during data evaluation” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusion of six patients after randomization due to poor treatment compliance; three in each treatment arm |
| Selective reporting (reporting bias) | High risk | “Both randomized groups
(n=38) and unmasked group (n=12) were
combined to establish a valid comparative evaluation with
equal baseline conditions” “We observed in many patients that the parameters reached a nearly normal level very early, but complete normalization could take weeks or months. Therefore, we analyzed the data for each parameter according to the following questions: (1) How much time elapsed until the nearly normal level was reached…(2) How much time elapsed until the normal level was reach…” |
| Other bias | High risk | -Funded by pharmaceutical
industry -There was a deviation from randomization: twelve patients chose the assignment according to their decision (two in methylprednisolone group and ten in vitamin B1 group) |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alejandro 1994 | This article was translated and reviewed. It describes a study that examined two routes of administration of corticosteroids and hence is outside the scope of this review |
| Beran 1973 | This article is a retrospective comparison of those treated by glucocorticosteroids and foreign protein therapy |
| Bhatti 2005 | This article is a review with no additional trials |
| Bird 1976 | This article is a review and describes studies that were already reviewed by the authors of this study |
| Bowden 1974 | Evaluated adrenocorticotropic hormone, a precursor of corticosteroids |
| Brusa 1999 | This article examines a convenience sample from an RCT and hence does not satisfy the inclusion criteria for this review |
| Brusaferri 2000 | This article is a meta-analysis of RCT on steroid treatment for optic neuritis. The articles included in this paper have already been reviewed by the authors of this review and determined not to contain additional data |
| Chuman 2004 | This article reports a discussion on one of the included trials |
| Gould 1977 | This trial was originally selected for the included trials, but after detailed assessment of the methodological quality it was decided to exclude it because of inadequate randomization method. This trial included a single injection of triamcinolone into the orbit versus no injection |
| Hallermann 1983 | This study is not an RCT and hence does not satisfy the inclusion criteria for this review |
| Hickman 2002 | Trial was not initiated as per personal communication with Dr. Hickman |
| Katz 1994 | This is a critical appraisal and comment on an included trial |
| Kommerell 1994 | Summary and discussion of ONTT 1992-2006 |
| Kott 1997 | The intervention ‘copaxone’ is an amino acid polymer, not a corticosteroid and hence outside the scope of this review |
| Midgard 2005 | This article was translated and was determined not to be an RCT (retracted literature review) |
| Pirko 2004 | This is not a trial and discusses natural history of optic neuritis |
| Rawson (1966-69) | Evaluated adrenocorticotropic hormone, a precursor of corticosteroids |
| Roed 2005 | Compares interventions not eligible for inclusion in this review |
| Soderstrom 1995 | This article was translated and was determined not to be an RCT |
| Toczolowski 1995 | This article was translated and was determined not to be an RCT |
| Trobe 1996 | The articles examines vision tests in optic neuritis and hence is not within the scope of this review |
Characteristics of ongoing studies [ordered by study ID]
NCT01524250.
| Trial name or title | Optic Neuritis Recovery After Oral or IV Corticosteroids |
|---|---|
| Methods | Patients will be randomized to receive equivalent doses of either intravenous (IV) or oral corticosteroid treatment. Optic nerve function assessments will be compared at baseline, prior to treatment, one and six months post corticosteroid treatment. This will allow for a comparison on whether the route of medication plays a role in the effectiveness of treatment with high dose corticosteroids |
| Participants | Patients aged 18-65 with acute demyelinating optic neuritis already receiving high dose corticosteroids |
| Interventions | Intervention: 1250mg oral
prednisone daily for 3 days Active comparator: 1000mg IV methylprednisolone daily for 3 days |
| Outcomes | Primary Outcome: P100 latency
of the Visual Evoked Potential in the affected eye at 6
months Secondary Outcome: High contrast visual acuity; contrast sensitivity at one and six months, and P100 latency of the Visual Evoked Potential in the affected eye at one month |
| Starting date | March 2012 (estimated completion September 2014) |
| Contact information | Sarah A Morrow, MD, FRCPC, MSc; 519-663-2993; smorrow@uwo.ca |
| Notes |
Data and Analyses
Comparison 1. Total intravenous corticosteroid dose more than or equal to 3000 mg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants with normal visual acuity at 6 months | 2 | 346 | Risk Ratio (M-H, Fixed, 95% CI) | 1.06 [0.89, 1.27] |
| 2 Participants with normal visual acuity at 1 year | 1 | 270 | Risk Ratio (M-H, Fixed, 95% CI) | 1.06 [0.92, 1.22] |
| 3 Participants with normal visual acuity at 1 month | 1 | 285 | Risk Ratio (M-H, Fixed, 95% CI) | 1.08 [0.89, 1.31] |
| 4 Participants with normal contrast sensitivity at 6 months | 2 | 346 | Risk Ratio (M-H, Fixed, 95% CI) | 1.10 [0.92, 1.32] |
| 5 Participants with normal contrast sensitivity at 1 year | 2 | Risk Ratio (M-H, Fixed, 95% CI) | Subtotals only | |
| 6 Participants with normal contrast sensitivity at 1 month | 2 | 322 | Risk Ratio (M-H, Random, 95% CI) | 1.27 [0.74, 2.16] |
| 7 Participants with normal visual field at 6 months | 2 | 346 | Risk Ratio (M-H, Fixed, 95% CI) | 1.08 [0.96, 1.22] |
| 8 Participants with normal visual field at 1 year | 2 | 316 | Risk Ratio (M-H, Fixed, 95% CI) | 1.02 [0.86, 1.20] |
| 9 Participants with normal visual field at 1 month | 2 | 330 | Risk Ratio (M-H, Fixed, 95% CI) | 1.43 [1.12, 1.84] |
Comparison 2. Oral corticosteroids versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Participants with normal visual acuity | 3 | Risk Ratio (M-H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Patients with normal visual acuity at 6 months | 2 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Patients with normal visual acuity at 1 year | 3 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Patients with normal visual acuity at 1 month | 3 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Participants with normal contrast sensitivity | 2 | Risk Ratio (M-H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Patients with normal contrast sensitivity at 6 months | 1 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Patients with normal contrast sensitivity at 1 year | 2 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Patients with normal contrast sensitivity at 1 month | 2 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Participants with normal visual field | 2 | Risk Ratio (M-H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Patients with normal visual field at 6 months | 2 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Patients with normal | 2 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Patients with normal visual field at 1 month | 2 | Risk Ratio (M-H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 1.1. Comparison 1 Total intravenous corticosteroid dose more than or equal to 3000 mg, Outcome 1 Participants with normal visual acuity at 6 months.
|
Analysis 1.2. Comparison 1 Total intravenous corticosteroid dose more than or equal to 3000 mg, Outcome 2 Participants with normal visual acuity at 1 year.
|
Analysis 1.3. Comparison 1 Total intravenous corticosteroid dose more than or equal to 3000 mg, Outcome 3 Participants with normal visual acuity at 1 month.
|
Analysis 1.4. Comparison 1 Total intravenous corticosteroid dose more than or equal to 3000 mg, Outcome 4 Participants with normal contrast sensitivity at 6 months.
|
Analysis 1.5. Comparison 1 Total intravenous corticosteroid dose more than or equal to 3000 mg, Outcome 5 Participants with normal contrast sensitivity at 1 year.
|
Analysis 1.6. Comparison 1 Total intravenous corticosteroid dose more than or equal to 3000 mg, Outcome 6 Participants with normal contrast sensitivity at 1 month.
|
Analysis 1.7. Comparison 1 Total intravenous corticosteroid dose more than or equal to 3000 mg, Outcome 7 Participants with normal visual field at 6 months.
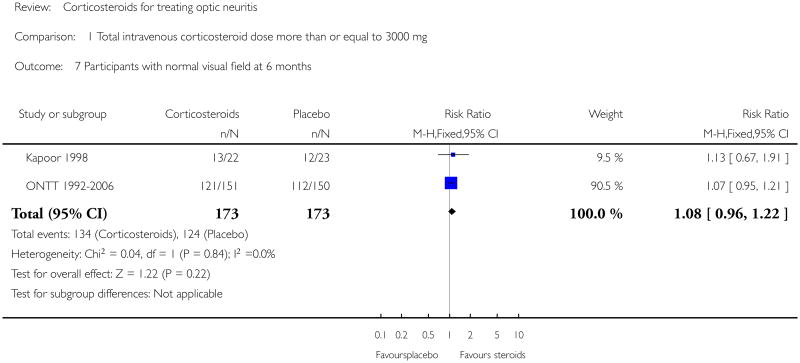
|
Analysis 1.8. Comparison 1 Total intravenous corticosteroid dose more than or equal to 3000 mg, Outcome 8 Participants with normal visual field at 1 year.
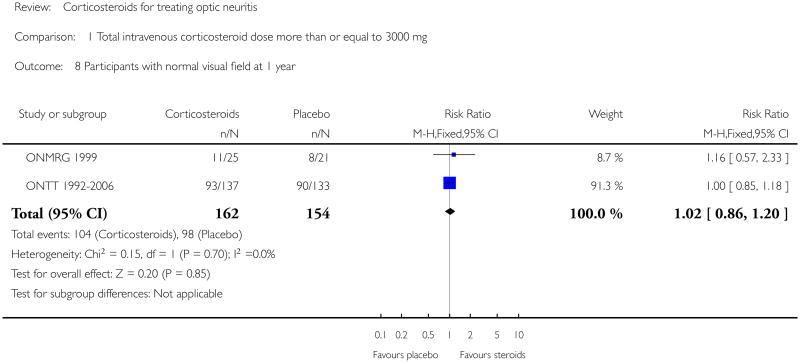
|
Analysis 1.9. Comparison 1 Total intravenous corticosteroid dose more than or equal to 3000 mg, Outcome 9 Participants with normal visual field at 1 month.
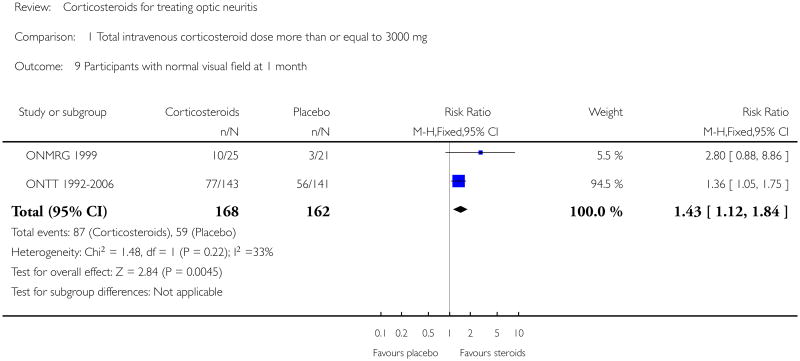
|
Analysis 2.1. Comparison 2 Oral corticosteroids versus placebo, Outcome 1 Participants with normal visual acuity.
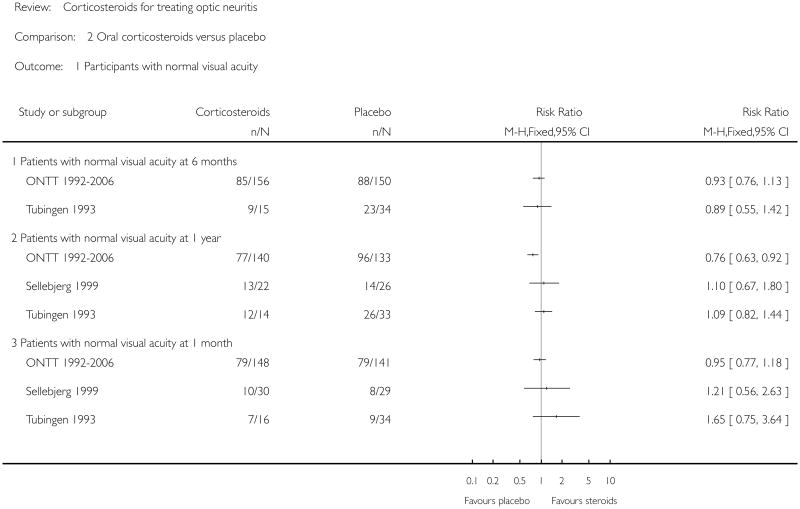
|
Analysis 2.2. Comparison 2 Oral corticosteroids versus placebo, Outcome 2 Participants with normal contrast sensitivity.
|
Analysis 2.3. Comparison 2 Oral corticosteroids versus placebo, Outcome 3 Participants with normal visual field.
|
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor Optic Neuritis
#2 (optic* or retrobul*) near/2 (neuritis)
#3 (#1 OR #2)
#4 MeSH descriptor Adrenal Cortex Hormones
#5 MeSH descriptor Glucocorticoids
#6 glucocorticoid*
#7 MeSH descriptor Pregnadienediols
#8 prednisone*
#9 prednisolone*
#10 methylprednisolone*
#11 triamcinolone*
#12 dexamethasone*
#13 anecortave*
#14 (#4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13)
#15 (#3 AND #14)
Appendix 2. MEDLINE (OvidSP) search strategy
randomized controlled trial.pt.
(randomized or randomised).ab,ti.
placebo.ab,ti.
dt.fs.
randomly.ab,ti.
trial.ab,ti.
groups.ab,ti.
or/1-7
exp animals/
exp humans/
9 not (9 and 10)
8 not 11
exp optic neuritis/
((optic$ or retrobul$) adj2 neuritis).tw.
or/13-14
exp adrenal cortex hormones/
exp glucocorticoids/
glucocorticoid$.tw.
exp pregnadienediols/
prednisone$.tw.
prednisolone$.tw.
methylprednisolone$.tw.
triamcinolone$.tw.
dexamethasone$.tw.
anecortave$.tw.
or/16-25
15 and 26
12 and 27
The search filter for trials at the beginning of the MEDLINE strategy is from the published paper by Glanville et al (Glanville 2006).
Appendix 3. EMBASE (OvidSP) search strategy
exp randomized controlled trial/
exp randomization/
exp double blind procedure/
exp single blind procedure/
random$.tw.
or/1-5
(animal or animal experiment).sh.
human.sh.
7 and 8
7 not 9
6 not 10
exp clinical trial/
(clin$ adj3 trial$).tw.
((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
exp placebo/
placebo$.tw.
random$.tw.
exp experimental design/
exp crossover procedure/
exp control group/
exp latin square design/
or/12-21
22 not 10
23 not 11
exp comparative study/
exp evaluation/
exp prospective study/
(control$ or prospectiv$ or volunteer$).tw.
or/25-28
29 not 10
30 not (11 or 23)
11 or 24 or 31
exp optic neuritis/
((optic$ or retrobul$) adj2 neuritis).tw.
or/33-34
exp corticosteroid/
exp glucocorticoid/
glucocorticoid$.tw.
prednisone$.tw.
prednisolone$.tw.
methylprednisolone$.tw.
triamcinolone$.tw.
dexamethasone$.tw.
exp pregnane derivative/
exp anecortave/
anecortave$.tw.
or/36-46
35 and 47
32 and 48
Appendix 4. LILACS search strategy
(optic or retrobul$) and neuritis
Appendix 5. metaRegister of Controlled Trials search strategy
optic neuritis and corticosteroid
Appendix 6. ClinicalTrials.gov search strategy
Optic Neuritis AND Corticosteroid
Appendix 7. ICTRP search strategy
optic neuritis and corticosteroid
Footnotes
Indicates the major publication for the study
Contributions of Authors: Conceiving the review: SBF
Designing the review: RB, RG, SBF
Coordinating the review: SBF, SSV
- Designing search strategies: RG, SBF, Trials Search Co-ordinators*
- Undertaking searches: CEVG Trials Search Co-ordinators*
- Screening search results: SBF, RG
- Organizing retrieval of papers: SBF, RG
- Screening retrieved papers against inclusion criteria: SBF, RG
- Appraising quality of papers: SBF, RG, SSV
- Extracting data from papers: SBF, RG
- Writing to authors of papers for additional information: SBF, SSV
- Providing additional data about papers: SBF, SSV
- Obtaining and screening data on unpublished studies: RG, SBF
- Entering data into RevMan: SBF, SSV
- Analysis of data: SBF, SSV, RG, RB
- Providing a methodological perspective: SBF, RG, SSV, RB
- Providing a clinical perspective: RB
- Providing a policy perspective: RB
- Providing a consumer perspective: SBF, RG, SSV, RB
Writing the review SBF, SSV, RG, RB
Securing funding for the review SBF, RB, RG, SSV
Performing previous work that was the foundation of the current study: N/A
Guarantor for review: RG
Updating the review: RG, SV, Cochrane Eyes and Vision Group US Project (Michael Marrone, Sueko Matsumura, and Ann-Margret Ervin)
*Karen Blackhall and Iris Gordon
Declarations of Interest: Roy Beck is the primary investigator for the Optic Neuritis Treatment Trial.
Differences Between Protocol and Review: Cochrane methodology regarding assessments of the risk of bias in included studies have been modified and the review authors updated the ‘Assessment of risk of bias in included studies’ section of the methods to reflect updated methodological considerations.
References to studies included in this review
- Hickman SJ, Kapoor R, Jones SJ, Altmann DR, Plant GT, Miller DH. Corticosteroids do not prevent optic nerve atrophy following optic neuritis. Journal of Neurology, Neurosurgery and Psychiatry. 2003;74(8):1139–41. doi: 10.1136/jnnp.74.8.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones SJ, Miller DH, Kapoor R, Brusa A, Plant G. Double-blind controlled trial of methylprednisolone treatment for acute optic neuritis: 6-month follow-up with visual evoked potential measurement. Multiple Sclerosis. 1996;2 Suppl:32–3. [Google Scholar]
- *.Kapoor R, Miller DH, Jones SJ, Plant GT, Brusa A, Gass A, et al. Effects of intravenous methylprednisolone on outcome in MRI-based prognostic subgroups in acute optic neuritis. Neurology. 1998;50(1):230–7. doi: 10.1212/wnl.50.1.230. [DOI] [PubMed] [Google Scholar]
- Menon V, Mehrotra A, Saxena R, Jaffery NF. Comparative evaluation of megadose methylprednisolone with dexamethasone for treatment of primary typical optic neuritis. Indian Journal of Ophthalmology. 2007;55(5):355–9. doi: 10.4103/0301-4738.33821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabuchi A, Kimura H, Inoue M. Optic neuritis treatment trial: Contrast sensitivity; assessment and results. Neuro-Ophthalmology Japan. 1998;15(1):30–6. [Google Scholar]
- *.Wakakura M, Mashimo K, Oono S, Matsui Y, Tabuchi A, Kani K, et al. Multicenter clinical trial for evaluating methylprednisolone pulse treatment of idiopathic optic neuritis in Japan. Optic Neuritis Treatment Trial Multicenter Cooperative Research Group (ONMRG) Japanese Journal of Ophthalmology. 1999;43(2):133–8. doi: 10.1016/s0021-5155(98)00071-9. [DOI] [PubMed] [Google Scholar]
- Wakakura M, Minei Higa R, Oono S, Matsui Y, Tabuchi A, Kani K, et al. Baseline features of idiopathic optic neuritis as determined by a multicenter treatment trial in Japan. Optic Neuritis Treatment Trial Multicenter Cooperative Research Group (ONMRG) Japanese Journal of Ophthalmology. 1999;43(2):127–32. doi: 10.1016/s0021-5155(98)00072-0. [DOI] [PubMed] [Google Scholar]
- Beck R. The optic neuritis treatment trial: three-year follow-up results. Archives of Ophthalmology. 1995;113(2):136–7. doi: 10.1001/archopht.1995.01100020014004. [DOI] [PubMed] [Google Scholar]
- Beck RW, Cleary PA. Optic neuritis treatment trial. One year follow-up results. Archives of Ophthalmology. 1993;111(6):773–5. doi: 10.1001/archopht.1993.01090060061023. [DOI] [PubMed] [Google Scholar]
- *.Beck RW, Cleary PA, Andersen MMJ, Keltner JL, Shults WT, Kaufman DI, et al. A randomized controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. New England Journal Of Medicine. 1992;326(9):581–8. doi: 10.1056/NEJM199202273260901. [DOI] [PubMed] [Google Scholar]
- Beck RW, Cleary PA, Backlund JC. The course of visual recovery after optic neuritis. Experience of the Optic Neuritis Treatment Trial. Ophthalmology. 1994;101(11):1771–8. doi: 10.1016/s0161-6420(94)31103-1. [DOI] [PubMed] [Google Scholar]
- Beck RW, Cleary PA, Trobe JD, Kaufman DI, Kupersmith MJ, Paty DW, et al. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. New England Journal of Medicine. 1993;329(24):1764–9. doi: 10.1056/NEJM199312093292403. [DOI] [PubMed] [Google Scholar]
- Beck RW, Gal RL, Bhatti MT, Brodsky MC, Buckley EG, Chrousos GA, et al. Visual function more than 10 years after optic neuritis: experience of the optic neuritis treatment trial. American Journal of Ophthalmology. 2004;137(1):77–83. doi: 10.1016/s0002-9394(03)00862-6. [DOI] [PubMed] [Google Scholar]
- Chrousos GA, Kattah JC, Beck RW, Cleary PA. Side effects of glucocorticoid treatment. Experience of the Optic Neuritis Treatment Trial. JAMA. 1993;269(16):2110–2. [PubMed] [Google Scholar]
- Cleary PA, Beck RW, Anderson MMJ, Kenny DJ, Backlund JY, Gilbert PR. Design, methods, and conduct of the Optic Neuritis Treatment Trial. Controlled Clinical Trials. 1993;14(2):123–42. doi: 10.1016/0197-2456(93)90015-6. [DOI] [PubMed] [Google Scholar]
- Cole SR, Beck RW, Moke PS, Gal RL, Long DT. The National Eye Institute Visual Function Questionnaire: experience of the ONTT. The Optic Neuritis Treatment Trial. Investigative Ophthalmology and Visual Science. 2000;41(5):1017–21. [PubMed] [Google Scholar]
- Keltner JL, Johnson CA, Spurr JO, Beck RW. Visual field profile of optic neuritis. One year follow-up in the Optic Neuritis Treatment Trial. Archives of Ophthalmology. 1994;112(7):946–53. doi: 10.1001/archopht.1994.01090190094027. [DOI] [PubMed] [Google Scholar]
- Noseworthy J. Corticosteroids for optic neuritis and subsequent development of multiple sclerosis. Annals of Neurology. 1994;120(Suppl 3):61. [Google Scholar]
- The Optic Neuritis Study Group. Multiple sclerosis risk after optic neuritis: final optic neuritis treatment trial follow-up. Archives of Neurology. 2008;65(6):727–32. doi: 10.1001/archneur.65.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Optic Neuritis Study Group. The 5-year risk of MS after optic neuritis: Experience of the optic neuritis treatment trial. Neurology. 1997;49(5):1404–13. doi: 10.1212/wnl.49.5.1404. [DOI] [PubMed] [Google Scholar]
- The Optic Neuritis Study Group. Visual function 15 years after optic neuritis: a final follow-up report from the Optic Neuritis Treatment Trial. Ophthalmology. 2008;115(6):1079–82. doi: 10.1016/j.ophtha.2007.08.004. [DOI] [PubMed] [Google Scholar]
- The Optic Neuritis Study Group. Visual function 5 years after optic neuritis: Experience of the Optic Neuritis Treatment Trial. Archives of Ophthalmology. 1997;115(12):1545–52. [PubMed] [Google Scholar]
- Trobe JD, Arbor A. The Optic Neuritis Study Group. One-year results in the optic neuritis treatment trial. Neurology. 1993;43:A280. [Google Scholar]
- Frederiksen JL. A double-blind randomized study of oral prednisolone versus placebo in patients with acute optic neuritis. Canadian Journal of Neurological Sciences. 1993;20(Suppl 4) Abstract no. 7-18-15. [Google Scholar]
- Sellbjerg F, Jensen CV, Larsson HB, Frederiksen JL. Gadolinium-enhanced magnetic resonance imaging predicts response to methylprednisolone in multiple sclerosis. Multiple Sclerosis. 2003;9(1):102–7. doi: 10.1191/1352458503ms880sr. [DOI] [PubMed] [Google Scholar]
- Sellebjerg F, Christiansen M, Jensen J, Frederiksen J. Immunological effects of oral high-dose methylprednisolone in acute optic neuritis and multiple sclerosis. European Journal of Neurology. 2000;7(3):281–9. doi: 10.1046/j.1468-1331.2000.00074.x. [DOI] [PubMed] [Google Scholar]
- *.Sellebjerg F, Nielsen HS, Frederiksen JL, Olesen J. A randomized, controlled trial of oral high-dose methylprednisolone in acute optic neuritis. Neurology. 1999;52(7):1479–84. doi: 10.1212/wnl.52.7.1479. [DOI] [PubMed] [Google Scholar]
- Sellebjerg F, Schaldemose Nielsen H, Frederiksen JL, Olesen J. A placebo-controlled treatment trial of oral high-dose methylprednisolone in acute optic neuritis. Multiple Sclerosis. 1998;4:381. [Google Scholar]
- Trauzettel-Klosinski S. The Aulhorn flicker test: possibilities and limits. Its use in optic neuritis for diagnosis, differential diagnosis, monitoring the course of the disease, and assessing the effect of oral prednisolone. German Journal of Ophthalmology. 1992;1(6):415–23. [PubMed] [Google Scholar]
- Trauzettel-Klosinski S, Aulhorn E, Diener HC, Minder C, Pfluger D. The influence of prednisolone on the course of optic neuritis. Results of a double-blind study [Dereinfluss von prednisolon auf den verlauf der neuritis nervi optici. Ergebnisse einer doppelblindstudie] Fortschritte Der Ophthalmologie. 1991;88(5):490–501. [PubMed] [Google Scholar]
- *.Trauzettel-Klosinski S, Axmann D, Diener HC. The Tubingen study on optic neuritis treatment - A prospective, randomized and controlled trial. Clinical Vision Sciences. 1993;8(4):385–94. [Google Scholar]
- Trauzettel-Klosinski S, Diener HC, Dietz K, Zrenner E. The effect of oral prednisolone on visual evoked potential latencies in acute optic neuritis monitored in a prospective, randomized, controlled study. Documenta Ophthalmologica. 1996;91(2):165–79. doi: 10.1007/BF01203696. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Alejandro PM, Castanon Gonzalez JA, Miranda Ruiz R, Edgar Echeverria R, Adriana Montano M. Comparative treatment of acute optic neuritis with “boluses” of intravenous methylprednisolone or oral prednisone [Tratamiento comparativo de la neuritis optica aguda con “bolos” de metilprednisolona endovenosa o prednisona oral.] Gaceta Medica de Mexico. 1994;130(4):227–30. [PubMed] [Google Scholar]
- Beran V, Hradecka V, Kohoutova O. Comparison of stimulation therapy with glucocorticoid therapy in optic nerve inflammation [Porovnani popudove terapie s lecbou glukokortikoidy u zanetu zrakoveho nervu] Ceskoslovenska Oftalmologie. 1973;29(5):372–4. [PubMed] [Google Scholar]
- Bhatti MT, Schmitt NJ, Beatty RL. Acute inflammatory demyelinating optic neuritis: current concepts in diagnosis and management. Optometry. 2005;76(9):526–35. doi: 10.1016/j.optm.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Bird AC. Treatment of acute optic neuritis. Transactions of the Ophthalmological Societies of the United Kingdom. 1976;96(3):412–4. [PubMed] [Google Scholar]
- Bowden AN, Bowden PMA, Friedman AI, Perkin GD, Rose FC. A trial of corticotrophin gelatin injection in acute optic neuritis. Journal of Neurology, Neurosurgery and Psychiatry. 1974;37(8):869–73. doi: 10.1136/jnnp.37.8.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brusa A, Jones SJ, Kapoor R, Miller DH, Plant GT. Long-term recovery and fellow eye deterioration after optic neuritis, determined by serial visual evoked potentials. Journal of Neurology. 1999;246(9):776–82. doi: 10.1007/s004150050454. [DOI] [PubMed] [Google Scholar]
- Brusaferri F, Candelise L. Steroids for multiple sclerosis and optic neuritis: a meta-analysis of randomized controlled clinical trials. Journal of Neurology. 2000;247(6):435–42. doi: 10.1007/s004150070172. [DOI] [PubMed] [Google Scholar]
- Chuman H. 41st Annual Meeting of the Japanese Neuro-Ophthalmology Society, Kyoto, Japan, December 12-13, 2003. Journal of Neuro-Ophthalmology. 2004;24(2):170–4. doi: 10.1097/00041327-200406000-00013. [DOI] [PubMed] [Google Scholar]
- Gould ES, Bird AC, Leaver PK, McDonald WI. Treatment of optic neuritis by retrobulbar injection of triamcinolone. British Medical Journal. 1977;1(6075):1495–7. doi: 10.1136/bmj.1.6075.1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallermann W, Haller P, Krüger C, Schiemann M, Patzold U. Progress of optic neuritis with and without corticosteroid treatment. Findings in a long-term investigation with static perimetry. Fortschritte der Ophthalmologie. 1983;80(1):30–4. [PubMed] [Google Scholar]
- Hickman S. NOON Nitric oxide in optic neuritis: A phase I randomised double-blind study of rapid corticosteroid treatment of optic neuritis. National Research Register; UK: 2002. [Google Scholar]
- Katz B. The Tubingen Study on Optic Neuritis Treatment - a prospective, randomized and controlled trial. Survey of Ophthalmology. 1994;39(3):262–3. doi: 10.1016/0039-6257(94)90201-1. [DOI] [PubMed] [Google Scholar]
- Kommerell G. Treatment of optic neuritis with corticosteroids. Discussion at the 10th Meeting of the International Neuro-ophthalmological Society (Freiburg 5 to 9 June 1994) [Die Behandlung der Neuritis nervi optici mit Kortikosteroiden. Diskussion bei der 10. Tagung der International Neuro–ophthalmological Society (Freiburg, 5. bis 9. Juni 1994)] Klinische Monatsblatter Fur Augenheilkunde. 1994;205(3):126–7. [PubMed] [Google Scholar]
- Kott E, Kessler A, Biran S. Optic neuritis in multiple sclerosis patients treated with copaxone. Journal of Neurology. 1997;244:S23–4. [Google Scholar]
- Midgard R, Seland JH, Hovdal H, Celius EG, Eriksen K, Jensen D, et al. Optic neuritis: diagnosis, treatment and follow-up. Tidsskrift for Den Norske Laegeforening. 2005;125(4):425–8. [PubMed] [Google Scholar]
- Midgard R, Seland JH, Hovdal H, Celius EG, Eriksen K, Jensen D, et al. Retraction of article [Tilbaketrekking av artikkel.] Tidsskrift for den Norske Laegeforening. 2005;125(15):2056. [PubMed] [Google Scholar]
- Pirko I, Blauwet LK, Lesnick TG, Weinshenker BG. The natural history of recurrent optic neuritis. Archives of Neurology. 2004;61(9):1401–5. doi: 10.1001/archneur.61.9.1401. [DOI] [PubMed] [Google Scholar]
- Rawson M, Liversedge LA, Goldfarb G. Treatment of acute retrobulbar neuritis with corticotrophin. Lancet. 1966;2(7472):1044–6. doi: 10.1016/s0140-6736(66)92025-3. [DOI] [PubMed] [Google Scholar]
- Rawson MD, Liversedge LA. Treatment of retrobulbar neuritis with corticotrophin. Lancet. 1969;294(7613):222. doi: 10.1016/s0140-6736(69)91469-x. [DOI] [PubMed] [Google Scholar]
- Roed HG, Langkilde A, Sellebjerg F, Lauritzen M, Bang P, Morup A, et al. A double-blind randomized trial of IV immunoglobulin treatment in acute optic neuritis. Neurology. 2005;64(5):804–10. doi: 10.1212/01.WNL.0000152873.82631.B3. [DOI] [PubMed] [Google Scholar]
- Soderstrom M. Corticosteroids and acute optic nerve neuritis. A therapeutic method requiring further studies [Kortikosteroider och akut opticusneurit. Behandlingsmetod kräver ytterligare studier] Lakartidningen. 1995;92(5):387–90. [PubMed] [Google Scholar]
- Toczolowski J, Lewandowska-Furmanik M, Stelmasiak Z, Wozniak D, Chmiel M. Treatment of acute optic neuritis with large doses of corticosteroids [Leczenie ostrego zapalenia nerwu wzrokowego za pomoca duzych dawek kortykosterydow.] Klinika Oczna. 1995;97(5):122–5. [PubMed] [Google Scholar]
- Trobe JD, Beck RW, Moke PS, Cleary PA. Contrast sensitivity and other vision tests in the optic neuritis treatment trial. American Journal of Ophthalmology. 1996;121(5):547–53. doi: 10.1016/s0002-9394(14)75429-7. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
- [accessed 22 February 2012];Optic neuritis recovery after oral or IV corticosteroids. NCT01524250. http://clinicaltrials.gov/ct2/show/NCT01524250.
Additional references
- Beck RW. Optic Neuritis. In: Miller NR, Newman NJ, editors. Walsh and Hoyt's Neuro-ophthalmology. 5th. Baltimore: Williams and Wilkins; 1998. pp. 599–647. [Google Scholar]
- Ebers GC. Optic neuritis and multiple sclerosis. Archives of Neurology. 1985;42(7):702–4. doi: 10.1001/archneur.1985.04060070096025. [DOI] [PubMed] [Google Scholar]
- Fleishman JA, Beck RW, Linares OA, Klein JW. Deficits in visual function after resolution of optic neuritis. Ophthalmology. 1987;94(8):1029–35. doi: 10.1016/s0161-6420(87)33349-4. [DOI] [PubMed] [Google Scholar]
- Glanville JM, Lefebvre C, Miles JN, Camosso-Stefinovic J. How to identify randomized controlled trials in MEDLINE: ten years on. Journal of the Medical Library Association. 2006;94(2):130–6. [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Sterne JAC, Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; Chichester, UK: John Wiley & Sons, Ltd; 2011. Chapter 8: Assessing risk of bias in included studies. updated March 2011. Available from www.cochrane-handbook.org. [Google Scholar]
- Koch-Henriksen N, Hyllested K. Epidemiology of multiple sclerosis: incidence and prevalence rates in Denmark 1948-64 based on the Danish Multiple Sclerosis Registry. Acta Neurologica Scandinavica. 1988;78(5):369–80. doi: 10.1111/j.1600-0404.1988.tb03672.x. [DOI] [PubMed] [Google Scholar]
- Kurtzke JF. Optic neuritis or multiple sclerosis. Archives of Neurology. 1985;42(7):704–10. doi: 10.1001/archneur.1985.04060070098026. [DOI] [PubMed] [Google Scholar]
- Mangione CM, Lee PP, Pitts J, Gutierrez P, Berry S, Hays RD. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Archives of Ophthalmology. 1998;116(11):1496–504. doi: 10.1001/archopht.116.11.1496. [DOI] [PubMed] [Google Scholar]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan) 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2011. [Google Scholar]
- Rodriguez M, Siva A, Cross SA, O'Brien PC, Kurland LT. Optic neuritis: a population-based study in Olmsted County, Minnesota. Neurology. 1995;45(2):244–50. doi: 10.1212/wnl.45.2.244. [DOI] [PubMed] [Google Scholar]
- Sanders EA, Volkers AC, van der Poel JC, van Lith GH. Estimation of visual function after optic neuritis: a comparison of clinical tests. British Journal of Ophthalmology. 1986;70(12):918–24. doi: 10.1136/bjo.70.12.918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoor TC, Rockwell DL. Treatment of optic neuritis with intravenous megadose corticosteroids. A consecutive series. Ophthalmology. 1988;95(1):131–4. doi: 10.1016/s0161-6420(88)33220-3. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Vedula SS, Brodney Folse S, Gal RL, Beck R. Corticosteroids for treating optic neuritis. Cochrane Database of Systematic Reviews. 2007;(1) doi: 10.1002/14651858.CD001430.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]