Editor:
Bacterial peritonitis is the most common infectious complication of continuous ambulatory peritoneal dialysis (CAPD) and often leads to significant morbidity, catheter loss, ultrafiltration failure, and mortality, despite standard intraperitoneal antibiotics (1,2). Abdominal hernias are fairly common noninfectious complications related to the increased intraperitoneal pressure of CAPD and may lead to technique failure and strangulation in serious cases (3). Given the high prevalence of these 2 complications, concurrent peritonitis and abdominal hernia may occur in uremic patients on CAPD. However, abscess formation in an umbilical hernia resulting from concomitant peritonitis has not been reported before.
Case Reports
Case 1: A 72-year-old uremic male on CAPD was admitted with CAPD-related peritonitis. The initial abdominal examination revealed diffuse tenderness with rebound. His white blood cell (WBC) count was 10,500/μL and C-reactive protein (CRP) 23.4 mg/dL. Culture of the dialysate effluent yielded group D Streptococcus, which was susceptible to vancomycin. After 5 days of intraperitoneal vancomycin, the peritonitis remained uncontrolled and a swollen umbilical stump was noted. The abdominal computed tomography (CT) is shown in Figures 1A and B. He underwent CAPD catheter removal and intravenous vancomycin. Three days later, the tender, swollen hernia was excised and turbid fluid drained. However, he responded poorly to intensive management and died of septic shock on the tenth hospital day.
Figure 1 —
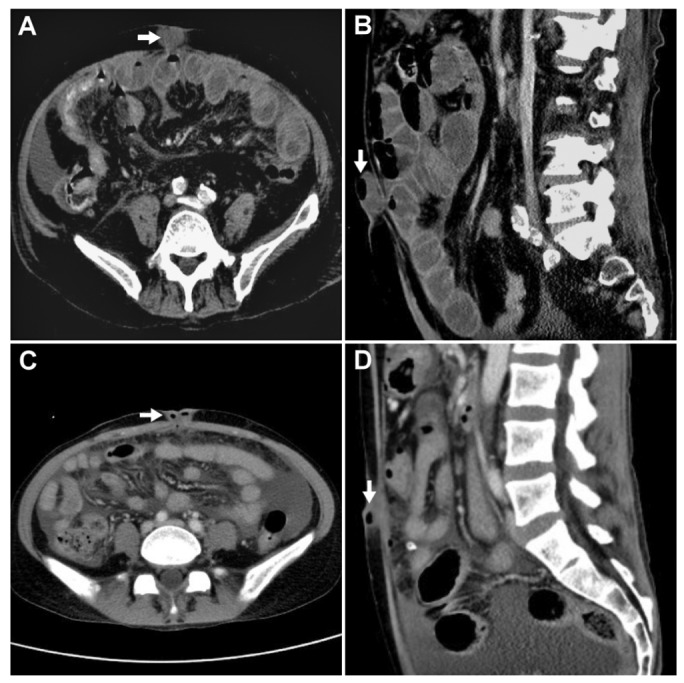
Abdominal CT of Case 1 in axial (A) and sagittal (B) views showing gas and variable attenuation in a fluid collection in the umbilical hernia (3.5 × 3.2 × 1.7 cm) along with peritoneal thickening. Abdominal CT of Case 2 in axial (C) and sagittal (D) views showing an umbilical hernia with gas bubbles inside (2.7 × 2.5 × 1.1 cm) and fatty stranding of the omentum just beneath the umbilicus. CT = computed tomography.
Case 2: A 35-year-old uremic female on CAPD was diagnosed with CAPD-related peritonitis. The initial physical examination revealed diffuse abdominal tenderness with rebound. Her WBC count was 19,330/μL and CRP 34.7 mg/dL. Vancomycin and ceftazidime were given intraperitoneally. The dialysate culture showed no growth. On the fifth hospital day, she was found to have redness and tenderness around the umbilicus. Abdominal CT is shown in Figures 1C and D. She was managed with surgical excision of the abscess and mesh repair of the hernia. She fully recovered and eventually resumed CAPD.
Discussion
With effective antimicrobial therapy, CAPD-related peritonitis usually improves within 1 to 2 days. Failure of response to appropriate treatment after 5 days is defined as refractory peritonitis (1). Traditionally, many clinicians opt for early peritoneal catheter removal in patients with refractory peritonitis (1). On rare occasions, refractory peritonitis may be complicated by intra-abdominal or abdominal wall abscesses, which should be treated with percutaneous or surgical drainage (4).
Due to their isolation and low flow, abdominal hernias in CAPD patients are areas of stagnant peritoneal fluid and potentially provide a nidus for microorganisms. Sometimes microorganisms may spread from the peritoneum to the abdominal hernia, leading to abscess formation due to poor antibiotic penetration into the hernia sac. It has been reported that pre-existing inguinal hernias in the presence of repeated peritonitis may become infected and form abscesses and adhesions in the inguinal rings in CAPD patients (5). On the other hand, it is possible that the umbilical hernia became infected first, through folliculitis, carbuncles, or pilonidal cyst. The infected umbilicus may progress to abscess formation, erode the peritoneum, and cause dialysate leakage, repeated omphalitis and peritonitis (6,7).
A detailed physical examination and contrast-enhanced CT scan can help identify anatomic abnormalities and infected fluid collections which may explain the failure of antibiotics. Beyond appropriate antibiotics, early surgical excision of the abscess and repair of contributory hernias are important (4,7). Early removal of the peritoneal catheter, as suggested by the International Society for Peritoneal Dialysis (ISPD) guidelines, may not be applicable in the setting of peritonitis with concurrent umbilical abscess as the catheter can facilitate peritoneal drainage.
Conclusions
These 2 cases illustrate the importance of broadening the differential diagnosis of refractory peritonitis in patients on CAPD. Early recognition of these complications and timely surgical intervention to remove the infectious source may improve clinical outcomes.
Disclosures
The authors have no financial conflicts of interest to declare.
References
- 1. Li PK, Szeto CC, Piraino B, Bernardini J, Figueiredo AE, Gupta A, et al. Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int 2010; 30:393–423. [DOI] [PubMed] [Google Scholar]
- 2. Perez Fontan M, Rodriguez-Carmona A, Garcia-Naveiro R, Rosales M, Villaverde P, Valdes F. Peritonitis-related mortality in patients undergoing chronic peritoneal dialysis. Perit Dial Int 2005; 25:274–84. [PubMed] [Google Scholar]
- 3. Leblanc M, Ouimet D, Pichette V. Dialysate leaks in peritoneal dialysis. Semin Dial 2001; 14:50–4. [DOI] [PubMed] [Google Scholar]
- 4. Boroujerdi-Rad H, Juergensen P, Mansourian V, Kliger AS, Finkelstein FO. Abdominal abscesses complicating peritonitis in continuous ambulatory peritoneal dialysis patients. Am J Kidney Dis 1994; 23:717–21. [DOI] [PubMed] [Google Scholar]
- 5. Chang YP, Chen TW, Chen CP, Ng YY, Yang WC. Inguinal abscess in a CAPD patient secondary to inguinal hernia and repeated episodes of peritonitis: a case report. Perit Dial Int 1999; 19:177–8. [PubMed] [Google Scholar]
- 6. Yap DY, Ma MK, Yip TP, Lui SL, Lo WK. Peritoneal dialysis-related peritonitis caused by erosion of umbilical abscess into the peritoneal cavity. Perit Dial Int 2012; 32:483–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chiu YW, Chen HC. Dialysate leakage through umbilicus in a CAPD patient with repeated omphalitis and peritonitis—a case report. Nephrol Dial Transplant 2006; 21:3001. [DOI] [PubMed] [Google Scholar]


