Abstract
The age of the European population is rising and percentage of adults aged 65 years and older is projected to increase from 16% in 2000 to 20% in 2020. It has been estimated that older subjects spend approximately 19 to 20 h/d indoors. Older individuals may be particularly at risk for detrimental effects from pollutants, even at low concentrations, due to reduced immunological defenses and multiple underlying chronic diseases. Six Porto, Portugal, urban area elderly care centers (ECC), housing a total of 425 older persons, were studied to assess indoor air quality (IAQ) and thermal comfort (TC) in two seasons. This study presents the IAQ and TC results in 36 rooms and constitutes part of a wider and ongoing study. The study areas were all naturally ventilated, and indoor concentrations in winter were within Portuguese reference values. However, 42% of the participants were dissatisfied with indoor thermal conditions, rating it “slightly cool.” In summer, the index rate of dissatisfied individuals was lower (8%). Significant differences were found between seasons in predicted percent of dissatisfied people (PPD) and predicted mean vote (PMV) indices. Fungal concentrations frequently exceeded reference levels (>500 colony-forming units [CFU]/m3). In addition, other pollutants occasionally exceeded reference levels. To our knowledge, this is the first study in Portugal to assess effects of indoor air contaminants on the health status and quality of life in older subjects living in ECC. Although IAQ and TC parameters were mostly within reference values, the results suggest a need to improve the balance between IAQ and TC in ECC, a critical environment housing a susceptible population.
The air one breathes inside buildings dominates overall inhalation exposure of most air pollutants, whether of indoor or outdoor origin (Corsi et al., 2012). As levels of outdoor ambient pollution have decreased in many areas, the relative impact of indoor air pollution has grown, and thus indoor air quality (IAQ) has increasingly gained importance. Indoor environments are often considered to be among the healthiest and safest places, particularly for older individuals who possess unique health needs and environmental sensitivities. In addition to IAQ, thermal comfort (TC) is a key indoor factor that might affect comfort, health, and performance. TC is chiefly determined by temperature, humidity, and air movement. Although the thermal environment found in residential settings does not usually produce serious adverse health effects, this atmosphere exerts a significant impact on the general well-being and daily performance of building occupants. Poor thermal environments might also aggravate the impact of air pollutants on health (Mendes and Teixeira, 2012).
The age of the European population is rising, and the percentage of adults aged 65 years and older is projected to increase from 16% in 2000 to 20% in 2020 (Adan et al., 2006). Older individuals spend approximately 19–20 h/d indoors (WHO, 2003). Elderly care centers (ECC) and homes have the potential to influence people’s lives socially, physically, and psychologically (Bradshaw et al., 2012). Older subjects may be particularly at risk of detrimental effects from air pollutants, even at low concentrations, due to their reduced immunological defenses and multiple underlying chronic diseases. Exposure to poor IAQ may produce or exacerbate eye irritation, nausea, upper respiratory complications, cognitive impairment, asthma, respiratory infections, cardiovascular disease, chronic obstructive pulmonary disease, and cancer (Ferng and Lee, 2002). Thus, IAQ is a special concern for ECC residents, important for both health and quality of life.
Risk assessment processes inadequately address susceptibility of older populations. Many factors may affect health and quality of life, pollutant exposure, and an individual’s response to these stimuli. While considerable evidence indicates that low concentrations of air pollutants are associated with increased risks of morbidity and mortality, particularly for respiratory and cardiovascular disease and cancer (Pope and Dockery, 2006; Miller et al., 2007; Krewski et al, 2004; Samet and Krewski, 2007), information on the elderly in indoor settings is limited. Adverse health effects associated with indoor air pollutants were investigated among some susceptible populations, especially children (Neas et al., 1994; Nafstad et al., 1996; 1997; Bruce et al., 2000; Jaakkola et al., 2001; Jaakkola and Jaakkola, 2002; Foos et al, 2008; Selgrade et al, 2008; Madureira et al., 2009). However, few studies evaluated adults and older people (Xu and Wang, 1993; Moran et al., 1999; Pilloto et al., 1999; Venners et al., 2001; Simoni et al., 2003). No apparent study was identified that jointly considered IAQ and TC among the elderly. Further, evidence remains sparse regarding the role of indoor pollutants on preexisting diseases common among the elderly, such as particulate matter (PM), bioaerosols, and volatile organic compounds (VOC). Thus, a need exists to examine IAQ, TC, and the health of older persons. The identification of subgroups that are susceptible to pollutants and TC is particularly important for designing appropriate and efficient interventions aimed at maintaining a healthy and comfortable environment.
Active aging implies growing old in good health and as a full member of society, feeling fulfilled, independent in daily life, and more involved as citizens. No matter how old, the elderly still play an active part in society and enjoy a better quality of life. The challenge is to make the most of the enormous potential that older citizens harbor even at an advanced age (European Union [EU], 2012). Health declines as people grow old, but much can be done to cope with this decline. Further, rather small changes in the environment may make a great difference to individuals suffering from health impairments and disabilities. Research to understanding such effects, especially taking into account that older individuals often have multiple diseases and live in restricted indoor environments that place them at increased risk of exposure to indoor pollutants, is an important endeavor and a natural shift in the focus of IAQ and TC studies.
OBJECTIVES AND STUDY DESIGN
This study characterizes effects of IAQ and TC among older individuals residing in Portugal. Ultimately, this ongoing study called GERIA—Geriatric Study in Portugal on Health Effects of Air Quality in Elderly Care Centers—will examine 20 ECC among 60 selected in Porto and Lisbon, the two largest cities in Portugal, and will include measures of cardio-respiratory health and quality of life. Table 1 presents the information used to calculate the sample size required for the study. To our knowledge, this is the first such study in Portugal, and one of the first with these objectives and study design. The GERIA study uses a prospective cohort design. This investigation presents measurements of IAQ and TC in 36 rooms in 6 ECC in 2 seasons. Our main aim is to present the overall results of environmental monitoring and TC assessment in these ECC.
Table 1.
Study Design Estimates
| Porto elderly population living in ECCs (number)a | 1574 |
| ECCs in Porto (number)a | 57 |
| Lisbon elderly population living in ECCs (number)a | 3646 |
| ECCs in Lisbon (number)a | 95 |
| Estimated elderly dementia (%)b | 53 |
| Estimated sample size population with 95% CI in Porto (number)c | 309 |
| Estimated sample size population with 95% CI in Lisbon (number)c | 348 |
Note. Sources:
, Social, 2010 [http://www.cartasocial.pt];
, estimated based on data provided by the ECCs managers;
, OpenEpi, Version 2.3.1, 2011 [www.OpenEpi.com] (Dean et al., 2001).
The following data sets and samples were collected at each ECC: (1) building characteristics; (2) environmental parameters, such as formaldehyde, particulate matter up to 10 µm in size (PM10), total volatile organic compounds (TVOC), carbon monoxide (CO), carbon dioxide (CO2), total bacteria, fungi, temperature, relative humidity (RH), and air velocity; and (3) predicted mean vote (PMV) and predicted percent of dissatisfied people (PPD).
MATERIAL AND METHODS
Walk-Through Survey
The building characteristics included the following information: type of building construction (concrete, or masonry); thermal isolation of the building; characteristics of building envelope (type of windows and doors, presence of weather stripping, etc.); ventilation system (natural, mechanical, or hybrid); types of indoor materials; use of gas burning appliances; evidence of dampness or mold; and ventilation practices (opened windows).
Indoor Air Monitoring and Thermal Comfort Assessment
IAQ parameters were measured twice, during winter 2011 (November–December) and summer 2012 (May–June), and included chemical parameters (CO2, CO, formaldehyde, TVOC, PM10), and biological contaminants (bacteria and fungi). TC parameters determined at the same time (following ISO 7730:2005) included the PMV index, which predicts the mean response of a larger group of people according to a 7-point thermal sensation scale (ISO 7730:2005), and the PPD index as a quantitative measure of the TC of a group of subjects at a particular thermal environment relative humidity (RH), temperature, and air velocity. The monitoring was performed in dining rooms, drawing rooms, medical offices, and bedrooms. Ambient air samples were also collected for comparison to indoor measurements. All active sampling and associated analytical measurements were performed in replicate and duplicate. This investigation was performed by the Environmental Health Department of the National Health Institute using methodologies accredited by NP EN ISO/IEC 17025:2005, “General requirements for the competence of testing and calibration laboratories.”
Sampling Schedule and Locations
The monitoring phase included daytime air sampling (starting at 10 a.m. and continuing for at least 4 h during normal activities) conducted in a discreet fashion in order not to disturb occupants’ normal behavior. Samplers were placed at a height of 0.6–1.5 m above the floor, approximately at the breathing zone level of elderly, and as close as possible to the center of the main area of the room. Sampling points were no closer than 1 m to walls, windows, doors, or an active heating system.
Suspended Particle Matter (PM10)
PM10 samples were collected using polytetrafluoroethylene (PTFE) filters on personal environmental monitors (PEM), Gilian personal pumps, and a sample flow rate of 2 L/min following U.S. Environmental Protection Agency (EPA) Method 10-A, “Determination of Respirable Particulate Matter in Indoor Air Using Size Specific Impaction” (Winberry et al., 1993). Pumps were calibrated and checked prior and after each sample using a Gillian Gilibrator-2 air flow calibrator. Before sampling, filters were stored in a desiccator for equilibration. At least one field blank per sampling event was used. Exposed and unexposed filters were transported, protected from dust and sunlight, and kept away from air in a closed filter holder. Each filter was weighed under controlled temperature (20 ± 1°C) and RH (50 ± 5%) before and after sampling using an electronic microbalance. Static charges were eliminated using a nonradioactive, ionizing air blower (EXAIR, model number 7907). Concentrations were calculated from the difference in filter weight and sample air volume.
TVOC and Formaldehyde
TVOC samples were collected by drawing air through a stainless-steel sampling tube containing Tenax TA using a personal air sampling pump (SKC Pocket pump) at a flow rate of 0.05 L/min for a period of 45 min. These pumps were calibrated and checked daily prior to and after each sample using a Gilian Gilibrator-2 air flow calibrator. Before sampling, each tube was conditioned at 250, 300, and 330°C for 30 min consecutively using helium carrier gas flow. Analysis of TVOC was performed by automatic thermal desorption coupled with capillary gas chromatography (GC) using a Perkin Elmer ATD 400 and AutoSystem GC fitted with flame ionization detector (FID) and an SE30 column, according to ISO 16000, part 6, and an internal method (ECA, 1997). TVOC was quantified using the toluene response factor, and concentrations were calculated as the sum of identified and unidentified compounds eluting between hexane and hexadecane (included), expressed as toluene.
Formaldehyde was measured by active sampling using 2,4-dinitrophenylhydrazinecoated glass fiber filters in Millipore Swinnex-13 filter holders, personal pumps (SKC AirChek 2000), and a flow rate of 0.8 L/min (calibrated and checked daily prior to and after each sampling with Gilian Gilibrator-2 air flow calibrator). Concentrations were determined by high-performance liquid chromatography (HPLC) using the methods described by Levin et al. (1986) and the National Institute for Occupational Safety and Health (NIOSH) 2016:2003. This method is well established in the lab and meets the quality criteria defined by it and accepted by independent audit entities. Each analysis used certified reference standards as well as duplicate and recovery samples.
Carbon Dioxide, Carbon Monoxide, and Thermal Comfort Parameters
CO2 and CO concentrations were determined using a portable IAQ monitor (GasData, model PAQ) during the occupied period. Shortterm measurements (30 min average) were collected in each room. After the equipment stabilized, measurements were recorded continuously using PCLogger 32 V3.0 software.
TC parameters (temperatures, RH, and air velocity) were measured using a Delta Ohm HD 32.1 data logger. After stabilization (25 min) in each room, 10-min measurements were recorded using the software just described. According to ISO 7730 and confirmed by observation, elderly occupants’ daily activity was considered to have a metabolic rate of 1 met, and their clothing a thermal insulation of 1 clo in summer and 1.3 clo in winter.
Bacteria and Fungi
Microorganism air sampling was conducted following NIOSH Method 0800, Bioaerosol Sampling (Indoor Air), using a microbiological air sampler (Merck air sampler MAS-100), an airflow rate of 100 L/min, and 2 agars, tryptic soy agar (TSA) for total bacteria and malt extract agar (MEA) for fungi. Both indoor and outdoor samples (250 L) were collected in duplicate and with one field blank per culture medium per day. To quantify fungi, samples were incubated at 25°C. Identification of fungal colonies was based upon phenotypic characteristics and followed standard mycological procedures. Bacteria were incubated at 37°C. Results were expressed as colony-forming units per cubic meter of air (CFU/m3).
Data Analysis
Descriptive analyses were used to obtain insight into the ECC characteristics and environmental monitoring results. Uncertainty was reported as 95% confidence intervals (CI) based on error propagation of multiple samples and instrumental uncertainty. Paired t-tests were used to test for indoor/outdoor differences and Spearman’s correlation for seasonal effects. A .05 level of significance was used for all analyses. All data were analyzed using SPSS 16.0.
RESULTS
Characterizations of Elderly Care Centers
The 6 ECC were located in an urban area of Porto and housed a total of 425 aged individuals with a range of 7 to 136 occupants per building. Table 2 presents selected building characteristics of the ECC sampled. Most ECC (78%) were in older buildings (up to 60 years old) using stone masonry construction and single pane windows. All buildings had been adapted for the purpose of ECC. Only 33% had insulation on the roof and walls. Most of the buildings presented leaks (67%) and condensation (56%) in interior walls and ceilings. The studied rooms were naturally ventilated with a mean floor area of 30 m2. Floor coverings were mainly wood, tile/stone, or polyvinyl chloride (PVC). The ECC were all equipped with heating systems (30% central heating and 70% gas and electric heaters). None of the buildings had cooling systems apart from the natural ventilation and some passive measures, such as blinds and curtains on the windows. Occupancy rates per room during monitoring were 3.8 persons in dining rooms, 7.2 in drawing rooms, 1.5 in medical offices, and 0.4 in bedrooms. All ECC were smoke free and 89% were near roads with heavy traffic.
Table 2.
ECC Building Characteristics, Expressed as Percentage
| Heating systems | |
| Central | 30 |
| Gas and oil heaters | 70 |
| Interior conditions | |
| Condensation | 56 |
| Leaks | 67 |
| Insulation | 33 |
| Power supply | |
| Electricity | 56 |
| Gas | 67 |
| Proximity to traffic | 89 |
| Single pane glass | 78 |
| Stone masonry | 78 |
| Window frames (wood) | 67 |
TVOC, Formaldehyde, and CO
Table 3 summarizes results of the environmental monitoring at the six ECC. The mean TVOC concentration was within Portuguese and international reference values in both winter and summer seasons, although maximal levels (0.5 mg/m3) considerably exceeded the WHO (2010) reference value of 0.2 mg/m3. On average, indoor TVOC levels were approximately threefold higher than outdoor levels, indicating the presence of indoor sources, such as emissions from construction materials, furniture, cleaning products, and cosmetics (Spengler et al. 2001; Martínez and Gómez, 2007).
Table 3.
Overall IAQ Chemical and Biological Parameters Results (Indoor and Outdoor) and Reference Levels
| Indoor | Outdoor | Indoor reference levels | |||||
|---|---|---|---|---|---|---|---|
| Parameter | Season | Average | SD (range) | Average | SD (range) | Portuguesea | International |
| Formaldehyde (mg m−3) | Summer | <0.0002 | — | — | — | 0.1 | 0.1b |
| Winter | <0.0002 | — | — | — | |||
| TVOC (mg m−3) | Summer | 0.07 | 0.09 (0.03–0.5) | 0.04 | 0.01 (0.02–0.06) | 0.6 | 0.2c |
| Winter | 0.08 | 0.07 (0.02–0.32) | 0.02 | 0.01 (0.01–0.03) | |||
| PM10 (mg m−3) | Summer | 0.074 | 0.04 (0.02–0.2) | 0.08 | 0.02 (0.05–0.11) | 0.15 | 0.05b |
| Winter | 0.064 | 0.071 (0.01–0.43) | 0.05 | 0.03 (0.02–0.12) | |||
| CO (mg m−3) | Summer | 1.3 | 2.47 (0.01–10.4) | 1.2 | 1.61 (0.01–4.8) | 12.5 | 7b |
| Winter | 0.5 | 0.68 (0.01–4.08) | 0.8 | 0.81 (0.01–2.56) | |||
| CO2 (mg m−3) | Summer | 996 | 436 (512–3568) | 669 | 91 (512–951) | 1800 | 1080d |
| Winter | 1196 | 512 (512–3842) | 712 | 344 (457–3751) | |||
| Bacteria (CFU m−3) | Summer | 397 | 237 (6–830) | 166 | 126 (68–336) | 500 | 500b |
| Winter | 329 | 280 (32–996) | 52 | 20 (30–84) | |||
| Fungi(CFU m−3) | Summer | 525 | 533 (6–2224) | 476 | 726 (20–1314) | 500 | 300e |
| Winter | 296 | 263 (90–1218) | 225 | 146 (114–478) | |||
DL 79/2006, 4 April 2006 (Decree-Law 2006a).
Of the 66 indoor formaldehyde samples collected, 60 were below the method limit of quantification (LOQ; 0.0002 mg/m3). These findings were consistent with the age of the buildings, old furniture, and absence of plywood, carpets and environmental tobacco smoke (ETS), all known formaldehyde sources. The elderly do not appear to be hypersensitive to formaldehyde (Paustenbach et al., 1997); rather, these subjects may be generally less sensitive to sensory irritation (WHO, 2010).
Outdoor CO levels exceeded indoor levels by approximately 1.3-fold, reflecting traffic pollution and absence of indoor CO sources. Apart from cooking restricted to the kitchens with proper exhaust and some gas heaters, there were no other combustion sources in the buildings. Maximal summer CO level (10.4 mg/m3) exceeded the WHO reference value of 7 mg/m3 at one site. This value was measured in a bedroom with an open window next to a road with heavy traffic, which likely influenced results for this room.
Particulate Matter and CO2
The mean indoor summer (0.074 mg/m3) and winter (0.064 mg/m3) PM10 concentration were within the Portuguese reference concentration of 0.15 mg/m3, but above the 24-h average interim WHO guideline of 0.05 mg/m3, which is intended as a target for outdoor air but which generally relates to both acute and chronic adverse health effects. Of the 93 PM10 measurements in both seasons, 54% exceeded the WHO guidelines. Maximal concentrations measured (0.43 mg/m3) occurred in winter in a busy drawing room.
The mean indoor CO2 winter (1196 mg/m3) and summer (996 mg/m3) concentrations fell below the Portuguese reference level (1800 mg/m3), but the winter concentration was numerically above the international reference level of 1080 mg/m3 (Burton, 1995). Indoor levels exceeded outdoor levels in both seasons. These concentrations of CO2 are not harmful, but are indicators of occupancy and ventilation in the study areas. Some guidance is given by the Finnish Society of Indoor Air Quality and Climate, suggesting 1300 mg/m3 for “very good,” 1650 mg/m3 for “good,” and 2200 mg/m3 for “satisfactory” indoor air quality (Säteri, 2002).
Bioaerosols
Table 3 shows that average airborne levels of bacteria and fungi fell below reference levels (500 CFU/m3). In summer, fungi concentrations reached 2224 CFU/m3. All of the highest indoor levels (10% of samples exceeded 1000 CFU/m3) were associated with high outdoor levels (38% of samples above reference levels). The most prevalent mold species were Cladosporium species (found in 41% of the samples), Penicillium species (24%), and Aspergillus fumigatus (8%). The last species produces mycotoxins (Ayanbimpe et al., 2010), may induce invasive lung infections, and is a potential cause of morbidity and mortality in susceptible and immunodeficiency individuals, including the elderly. The outdoor main species were Cladosporium species and Penicillium species in both seasons.
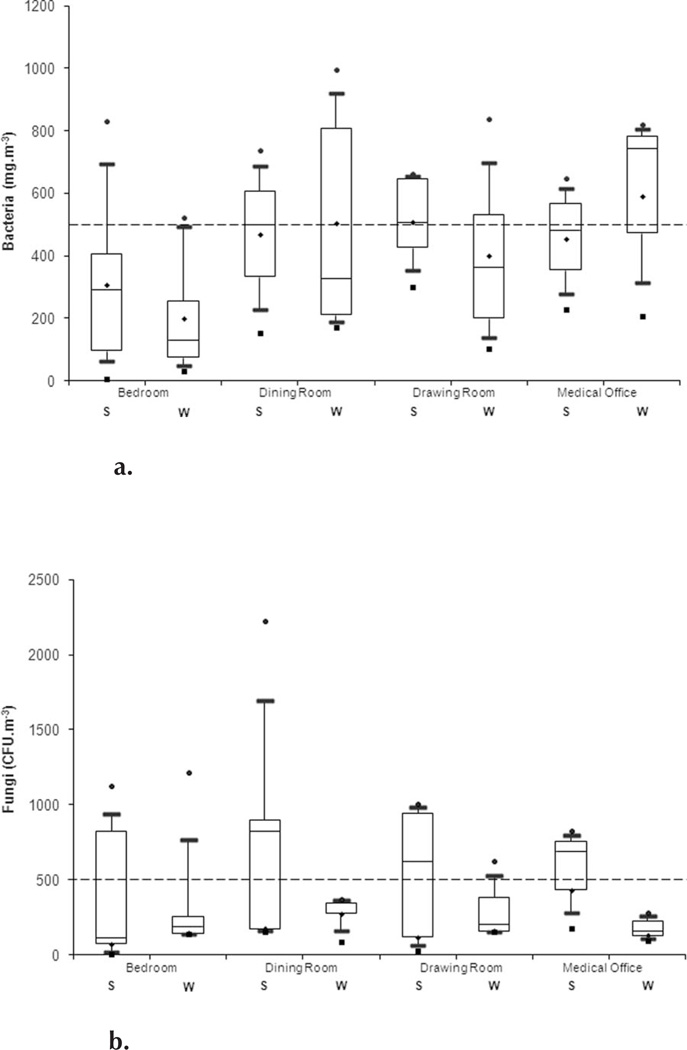
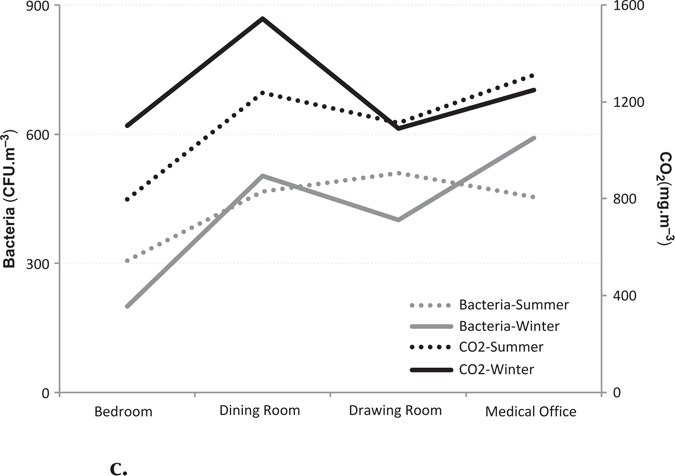
Figures 1a and 1b represent the distribution of the bioaerosols by room and season. The total bacteria concentration was below the reference level, but indoor levels were twofold higher than levels outdoors. Bacteria concentrations were highest in the dining room (467 CFU/m3) in the winter; in contrast, drawing-room levels were highest in the summer (509 CFU/m3). Fungi showed a wider distribution in all areas analyzed in the summer season (Figure1b). Figure 1c presents bacteria and CO2 levels by season and by room. Although bacteria and CO2 concentrations show some similar trends by room, the correlation coefficient was not significant (Figure 1c).
FIGURE 1.
a. Bacteria concentration distribution by room and season (● Max; ■ Min; S – summer; W – winter; — high reference level).
b. Fungi concentrations distribution by room and season (● Max; ■ Min; S – summer; W – winter; — high reference level).
c. Bacteria and CO2 concentrations by room and season.
Thermal Comfort
During monitoring, the mean daily ambient air temperatures in Porto ranged from 16 to 28°C in summer, and from 4 to 14°C in winter. In the ECC, temperatures ranged between 16 to 30°C in summer and 12 to 16°C in winter.
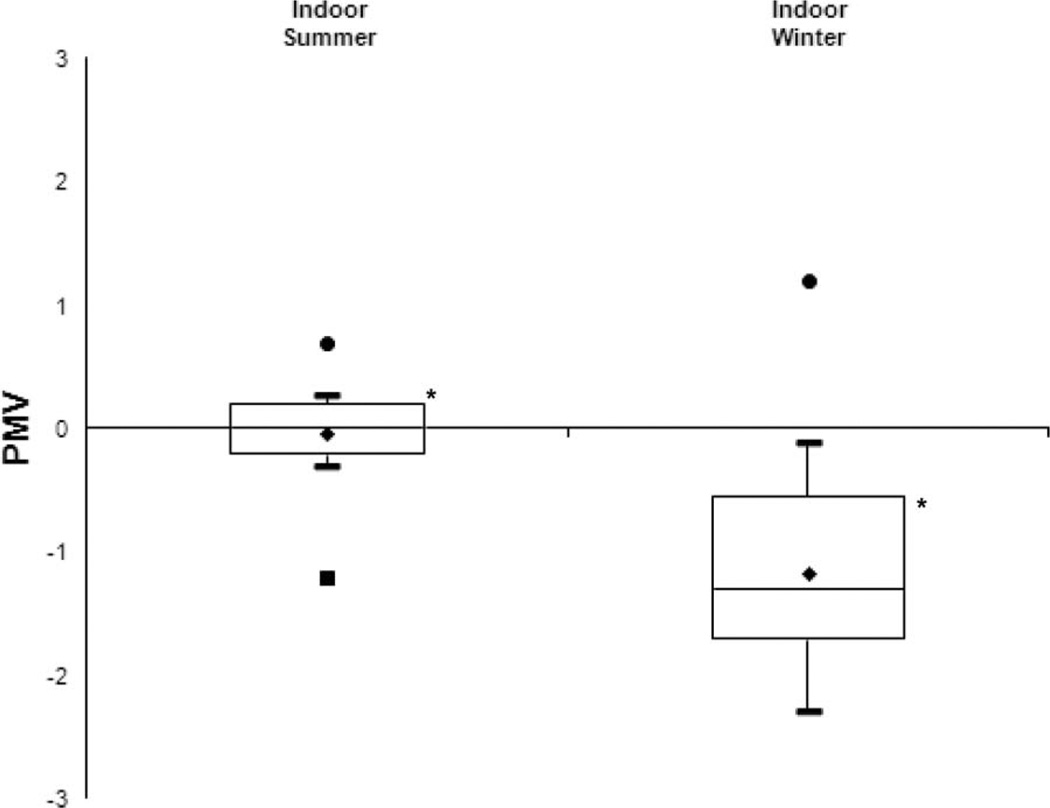
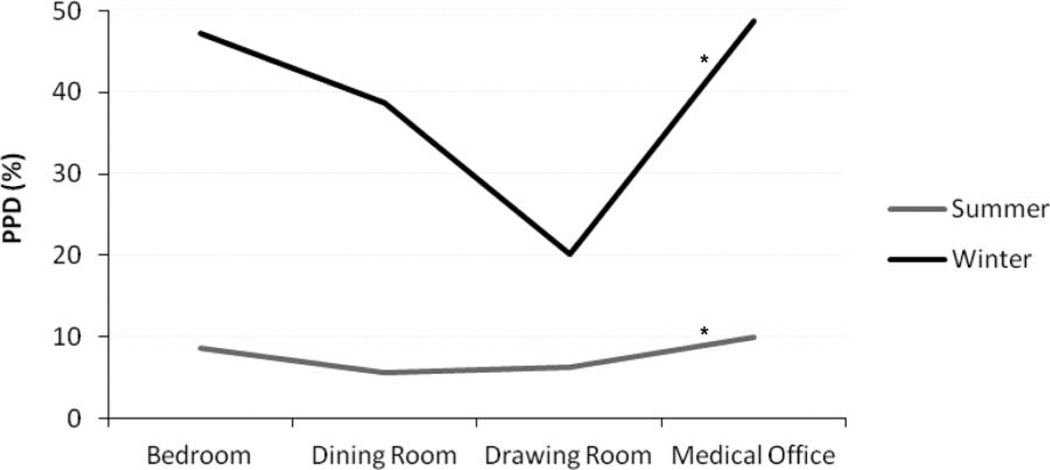
Both PPD and PMV varied significantly by season. In winter, 42% of residents were dissatisfied (PPD) with indoor TC, rating it “slightly cool” (PMV = −1.2) (Figure 2). As noted earlier, only 33% of the ECC buildings were insulated, 30% had central heating, and visible inspection suggested leaks and condensation problems were common. In summer, the dissatisfaction index presented a lower rate of (PPD = 8%), reflecting a “neutral” PMV index (PMV = −0.03). Analysis of PPD by room (Figure 3) showed that medical offices (winter: 49%; summer: 10%) and bedrooms (winter: 47%; summer: 9%) were the areas with the highest percent of dissatisfied residents in both seasons. Dining and drawing rooms had the lowest PPD, likely due to higher occupancy rates in these rooms that may disguise the lack of insulation present in most of the buildings. Our results indicate that maintenance of a comfortable indoor environment with good IAQ for elderly populations living in ECC in Portugal may be a substantial challenge, especially in winter.
FIGURE 2.
Overall PMV indexes (*P < 0.05) (● Max; ■ Min).
FIGURE 3.
PPD by room and season (*P = 0.013).
DISCUSSION
The indoor environment has special significance for elderly persons, who are particularly susceptible to TC concerns as well as adverse respiratory and cardiovascular effects associated with IAQ pollutants, and who are likely to spend most of their day indoors. Currently, few reports have addressed IAQ and TC concerns among older subjects or in elderly care centers (ECC). Simoni et al. (2002) showed an association of relatively low levels of indoor pollutants, such as PM, with acute respiratory symptoms and reduced peak expiratory flow in an older population. Later, Simoni et al. (2003) suggested the need for further studies on indoor pollutants and health in the elderly, including a focus on improved exposure assessment, various short-term and long-term health outcomes, and identification of those characteristics potentially associated with susceptibility of adverse effects. The indoor environment may also affect the development of preexisting diseases in the elderly, an unstudied and potentially important research area.
Air quality monitoring in a small set of Portuguese ECC showed that PM10, TVOC, formaldehyde, CO, bacteria, and fungi levels were often, but not always, within reference values. These pollutants have been associated with a variety of effects, where airborne bacteria are confirmed or presumed causative agents of several infectious diseases, and also with the development and exacerbation of chronic respiratory illness, including asthma (Peccia et al., 2008). The same concern was reported in a review by Tang (2009) for fungi and their spores, which may trigger hypersensitivity reactions such as rhinitis, sinusitis, or asthma, and also for viruses such as the severe acute respiratory syndrome-associated coronavirus with a 50% fatality rate for those over 65 years old. Further, the role of human occupancy as a source of indoor biological aerosol is poorly understood. Size-dependent particle behavior often might be associated with specific chemical and biological components of PM. The strong signal of human microbiological contaminants as far as airborne PM is concerned in an occupied room demonstrates that the inhalation route might be a source of exposure to microorganisms emitted from the skin, hair, nostrils, and mouths of their occupants (Qian et al., 2012).
In our study, while the total bacterial concentration was almost always below the reference level, indoor levels were twofold greater than those outdoors, due to a result of occupancy (e.g., direct human shedding), or resuspension (e.g., from carpet, and potentially other sources (Hospodsky et al. 2012). The similar trends of bacteria and CO2 concentrations by room in our study indicate possible human source of the bacteria. Low ventilation rates and crowded conditions increase CO2 levels, and bioeffluent concentrations, potentially including bacteria, gases, odors, PM, and viruses (Mendes and Teixeira, 2012). With respect to bacteria, inhalation of infectious microorganisms from individuals and animals is a primary mechanism of contagion for most acute respiratory infections. Such risks may increase in indoor environments that have low ventilation rates and use untreated and recirculated air (Franchi et al., 2006).
In general, the elderly seem to perceive TC differently from the young due to a combination of physical aging and behavioral differences (Hoof and Hensen, 2006). Our findings show a PPD index of 42% dissatisfied residents in winter, a high rate that may partially be explained by cooler outdoor temperatures found (average of 13°C) and the ECC building characteristics, including use of natural ventilation, stone masonry, and lack of insulation. Several investigators found that older adults have a lower activity level and metabolic rate than younger persons, and thus require higher ambient temperatures (Havenith, 2001; Tsuzuki and Iwata, 2002). Further, the ability to regulate body temperature tends to decrease with age (Hoof and Hensen, 2006). Tsuzuki and Ohfuku (2002) also found that older adults have reduced warmth sensitivity in cold seasons, and similarly reduced cold sensitivity in hot seasons. Physiologically older adults preferred a warmer environment (+2°C) than younger people. Enomoto-Koshimizu et al. (1997) suggested that a 20–24°C comfort zone is not warm enough for older adults, and specified an optimal temperature of 25.3°C for sedentary older adults.
The IAQ and TC measurements suggest the difficulty of maintaining indoor environmental conditions in ECC that are suitable to this susceptible population, especially in winter. Individual differences among older persons may be large with respect to the requirements and preferences of TC parameters, and more research is needed on this topic, for example, using studies allowing older adults personal control over their thermal environment (Hoof and Hensen, 2006). Further, Raymann and Van Someren (2008) presented temperature and TC as major issues for the elderly population where cardio-mortality was associated with (1) ambient temperature (Halonen et al., 2010) and (2) indoor climate with low temperatures due to poor insulated houses (Bøkenes et al., 2009).
Strengths and Limitations of the Study
This study investigated both IAQ and TC parameters in occupied ECC in both in summer and winter seasons. Sampling could not be conducted simultaneously in the ECC due to equipment and logistical limitations; thus, temporal variation in outdoor pollutant levels and weather over the measurement period may have affected indoor results. In addition, measurements were short-term in nature, and only a subset of rooms within ECC and a small number of ECC in one city were studied. This limitation will be addressed in further research in which 20 ECC will be studied in two cities, and the larger data set will allow a number of additional analyses.
CONCLUSIONS
IAQ and TC have been rarely evaluated in ECC. Characterization of IAQ and TC in six ECC in Portugal revealed several concerns. Not surprisingly, concentrations of CO2, TVOC, and bacteria were above outdoor levels, indicating indoor sources, and these and other pollutants (PM10, CO and fungi) sometimes exceeded reference levels. Perhaps most significantly, TC PPD index was classified as “slightly cool” in the winter season. Although these results suggest that indoor concentrations of most parameters were generally within reference values, the results suggest the need to improve the balance between IAQ and TC parameters. Potentially, simple measures could provide health benefits to ECC residents and workers, such as insulating ceilings, walls, and windows, without giving up natural and passive ventilation solutions that are common in Portugal due to the advantage of the country’s generally mild weather. The present study suggests that further study is needed to analyze the interaction between TC and IAQ variables in order to improve the well-being of our elderly population.
Acknowledgments
Our current research is supported by Fundação para a Ciência e Tecnologia (FCT) through GERIA Project PTDC/SAUSAP/116563/2010 and a PhD grant (SFRH/BD/72399/2010).
REFERENCES
- Ayanbimpe G, Wapwera S, Kuchin D. Indoor air mycoflora of residential dwellings in Jos metropolis. African Health Sci. 2010;10:172–176. [PMC free article] [PubMed] [Google Scholar]
- Adan O, Ng-A-Tham J, Hanke W, Sigsgaard T, Hazel P, Wu F. In search of a common European approach to a healthy indoor environment. Environ. Health Perspect. 2006;115:983–988. doi: 10.1289/ehp.8991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bøkenes L, Mercer JB, MacEvilly S, Andrews JF, Bolle R. Annual variations in indoor climate in the homes of elderly persons living in Dublin, Ireland and Tromsø, Norway. Eur. J. Public Health. 2009;21:526–531. doi: 10.1093/eurpub/ckp109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradshaw S, Playford E, Riazi A. Living well in care homes: A systematic review of qualitative studies. Age Ageing. 2012;41:429–440. doi: 10.1093/ageing/afs069. [DOI] [PubMed] [Google Scholar]
- Bruce N, Perez-Padilla R, Albalak R. Indoor air pollution in developing countries: A major environmental and public health challenge. Bull. WHO. 2000;78:1078–1092. [PMC free article] [PubMed] [Google Scholar]
- Burton DJ. IAQ and HVAC workbook, Library of Congress cataloging in publication data. (2nd ed.) 1995 [Google Scholar]
- Corsi R, Kinney K, Levin H. Microbiomes of built environments: 2011 symposium highlights and workgroup recommendations. Indoor Air. 2012;22(1):71–172. doi: 10.1111/j.1600-0668.2012.00782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version 2.3.1. 2001 www.OpenEpi.com. [Google Scholar]
- Decree-Law. DR I Série A no. 67 of 4th April 2006. Ministry of Public Works, Transport and Communications; 2006a. Decree-Law No. 79/2006 of April 4th, Annex VII—Reference concentration levels of indoor pollutants within the existing buildings. [Google Scholar]
- Decree-Law. Ministry of Public Works, Transport and Communications; 2006. Decree-Law No. 80/2006 of April 4th. DR I Série A no. 67 of 4th April 2006. [Google Scholar]
- Enomoto-Koshimizu H, Kubo H, Isoda N, Yanase T. Effect of the radiant heating on the elderly. In: Seppälä P, Luoparjärvi T, Nygård C-H, Mattila M, editors. Proceedings, 13th Triennial Congress of the International Ergonomics Association. Vol. 5. Tampere, Finland: 1997. pp. 433–435. edited by P. Seppälä, T. Luoparjärvi, C.-H. Nygård, and M. Mattila. [Google Scholar]
- European Collaborative Action. European Commission, Joint Research Centre, Environment Institute. Luxembourg: Office for Official Publications of the European Communities; 1997. Indoor air & its impact on man. Report 19. Total volatile organic compounds (TVOC) in indoor air quality Investigations. [Google Scholar]
- European Union. European year for active ageing and solidarity between generations. 2012 http://europa.eu/ey2012/ey2012main.jsp?langId=en&catId=971. [Google Scholar]
- Ferng SF, Lee LW. Indoor air quality assessment of daycare facilities with carbon dioxide, temperature, and humidity as indicators. J. Environ. Health. 2002;65:14–18. 22. [PubMed] [Google Scholar]
- Foos B, Marty M, Schwartz J, Bennett W, Moya J, Jarabek AM, Salmon AG. Focusing on children’s inhalation dosimetry and health effects for risk assessment: An introduction. J. Toxicol. Environ. Health A. 2008;71:149–165. doi: 10.1080/15287390701597871. [DOI] [PubMed] [Google Scholar]
- Franchi M, Carrer P, Kotzias D, Rameckers E, Seppänen O, Bronswijk J, Viegi G, Gilder JA, Valovirta E. Working towards healthy air in dwellings in Europe. Allergy. 2006;61:864–868. doi: 10.1111/j.1398-9995.2006.01106.x. [DOI] [PubMed] [Google Scholar]
- Havenith G. Temperature regulation and technology. Gerontechnology. 2001;1:41–49. [Google Scholar]
- Halonen J, Zanobetti A, Sparrow D, Vokonas P, Schwartz J. Associations between outdoor temperature and markers of inflammation: A cohort study. Environ. Health. 2010;9:42. doi: 10.1186/1476-069X-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hospodsky D, Qian J, Nazaroff WW, Yamamoto N, Bibby K, Rismani-Yazdi H, Peccia J. Human occupancy as a source of indoor airborne bacteria. PLoS ONE. 2012;7:e34867. doi: 10.1371/journal.pone.0034867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoof van J, Hensen JLM. Thermal comfort and older adults. Gerontechnology. 2006;4:223–228. [Google Scholar]
- International Standard ISO 16000-6:2004 Indoor air—Part 6: Determination of volatile organic compounds in indoor and test chamber air by active sampling on Tenax TA sorbent, thermal desorption and gas chromatography using MS/FID. International Organization for Standardization. Available at http://www.iso.org/iso/home/standards.htm.
- International Standard ISO 7730:2005 Ergonomics of the thermal environment—Analytical determination and interpretation of thermal comfort using calculation of the PMV and PPD indices and local thermal comfort criteria. International Organization for Standardization. Available at http://www.iso.org/iso/home/standards.htm.
- Jaakkola JJK, Jaakkola MS. Effects of environmental tobacco smoke on respiratory health in children. Scand. J. Work Environ. Health. 2002;28(suppl. 2):71–83. [PubMed] [Google Scholar]
- Jaakkola JJK, Nafstad P, Magnus P. Environmental tobacco smoke, parental atopy, and childhood asthma. Environ. Health Perspect. 2001;109:579–582. doi: 10.1289/ehp.01109579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korhonen I, Parkka J, Gils M. van. Health monitoring in the home of the future. IEEE Eng. Med. Biol. Mag. 2003;22:66–73. doi: 10.1109/memb.2003.1213628. [DOI] [PubMed] [Google Scholar]
- Krewski D, Burnett RT, Jerrett M, Pope A, Rainham DG, Calle EE, Thurston GD. Mortality and long-term exposure to ambient air pollution: Ongoing analyses based on the American Cancer Society cohort. J. Toxicol. Environ. Health A. 2004;68:1093–1109. doi: 10.1080/15287390590935941. [DOI] [PubMed] [Google Scholar]
- Levin J, Lindahl R, Andersson K. A passive sampler for formaldehyde in air using 2,4 dinitrophenylhydrazine-coated glass fiber filters. Environ Sci Technol. 1986;20:1273–1276. [Google Scholar]
- Madureira J, Alvim-Ferraz MCM, Rodrigues S, Gonçalves C, Azevedo MC, Pinto E, Mayan O. Indoor air quality in schools and health symptoms among Portuguese teachers. Hum. Ecol. Risk Assess. 2009;15:159–169. [Google Scholar]
- Martínez FJR, Gómez VE. Calidad de ambientes interiores. Madrid, Spain: Thomson Editores; 2007. [Google Scholar]
- Mendes A, Teixeira JP. Encyclopedia of toxicology. 3rd ed. Elsevier; 2012. Sick building syndrome. [Google Scholar]
- Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JD. Long-term exposure to air pollution and incidence of cardiovascular events in women. N. Engl. J. Med. 2007;356:447–458. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- Moran SE, Strachan DP, Johnston ID, Anderson HR. Effects of exposure to gas cooking in childhood and adulthood on respiratory symptoms, allergic sensitization and lung function in young British adults. Clin. Exp. Allergy. 1999;29:1033–1041. doi: 10.1046/j.1365-2222.1999.00561.x. [DOI] [PubMed] [Google Scholar]
- Nafstad P, Jaakkola JJK, Hagen JA, Botten G, Kongerud J. Breastfeeding, maternal smoking and lower respiratory tract infections. Eur Respir J. 1996;9:2623–2629. doi: 10.1183/09031936.96.09122623. [DOI] [PubMed] [Google Scholar]
- Nafstad P, Kongerud J, Botten G, Hagen JA, Jaakkola JJK. The role of passive smoking in the development of bronchial obstruction during the first 2 years of life. Epidemiology. 1997;8:293–297. doi: 10.1097/00001648-199705000-00011. [DOI] [PubMed] [Google Scholar]
- Neas LM, Dockery DW, Ware JH, Spengler JD, Ferris BG, Speizer FE. Concentration of indoor particulate matter as a determinant of respiratory health in children. Am. J. Epidemiol. 1994;139:1088–1099. doi: 10.1093/oxfordjournals.aje.a116952. [DOI] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health. NIOSH manual of analytical methods (NMAM) 4th ed. Washington, DC: Government Printing Office; 1994. [Google Scholar]
- Paustenbach D, Alarie Y, Kulle T, Schachter N, Smith R, Swenberg J, Witschi H, Horowitz SB. A recommended occupational exposure limit for formaldehyde based on irritation. J. Toxicol. Environ. Health. 1997;50:217–263. [PubMed] [Google Scholar]
- Peccia J, Milton DK, Reponen T, Hill J. A role for environmental engineering and science in preventing bioaerosol-related disease. Environ. Sci. Technol. 2008;42:4631–4637. doi: 10.1021/es087179e. [DOI] [PubMed] [Google Scholar]
- Pilotto LS, Smith BJ, Nitschke M, Ruffin RE, Mitchell R. Industry, air quality, cigarette smoking and rates of respiratory illness in Port Adelaide. Aust. N. Z. J. Public Health. 1999;23:657–660. doi: 10.1111/j.1467-842x.1999.tb01556.x. [DOI] [PubMed] [Google Scholar]
- Pope CA, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J. Air Waste Manage. Assoc. 2006;56:709–742. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- Qian J, Hospodsky D, Yamamoto N, Nazaroff WW, Peccia J. Size-resolved emission rates of airborne bacteria and fungi in an occupied classroom. Indoor Air. 2012;22:339–351. doi: 10.1111/j.1600-0668.2012.00769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymann R, Van Someren E. Diminished capability to recognize the optimal temperature for sleep initiation may contribute to poor sleep in elderly people. Sleep. 2008;31:1301–1309. [PMC free article] [PubMed] [Google Scholar]
- Robertson LD. Monitoring viable fungal and bacterial bioaerosols concentrations to identify acceptable levels for common indoor environments. Indoor Environ. 1997;6:295–300. [Google Scholar]
- Samet J, Krewski D. Health effects associated with exposure to ambient air pollution. J. Toxicol. Environ. Health A. 2007;70:227–242. doi: 10.1080/15287390600884644. [DOI] [PubMed] [Google Scholar]
- Säteri J. Finnish classification of indoor climate 2000: Revised target values. Proc. Indoor Air. 2002;3:512–517. [Google Scholar]
- Selgrade MK, Plopper CG, Gilmour MI, Conolly RB, Foos BS. Assessing the health effects and risks associated with children’s inhalation exposures—Asthma and allergy. J. Toxicol. Environ. Health A. 2008;71:196–207. doi: 10.1080/15287390701597897. [DOI] [PubMed] [Google Scholar]
- Simoni M, Carrozzi L, Baldacci S, Scognamiglio A, Di Pede F, Sapigni T, Viegi G. The Po River delta (North Italy) epidemiological study: effect of pollutant exposure on acute respiratory symptoms and respiratory function in adults. Arch. Environ. Health. 2002;57:130–136. doi: 10.1080/00039890209602928. [DOI] [PubMed] [Google Scholar]
- Simoni M, Jaakkola MS, Carrozzi L, Baldacci S, Di Pede F, Viegi G. Indoor air pollution and respiratory health in the elderly. Eur. Respir. J. 2003;21(suppl. 40):15s–20s. doi: 10.1183/09031936.03.00403603. [DOI] [PubMed] [Google Scholar]
- Spengler JD, Samet JM, McCarthy JF. Indoor air quality handbook. New York, NY: McGraw-Hill; 2001. [Google Scholar]
- Tang JW. The effect of environmental parameters on the survival of airborne infectious agentes. J. R. Soc. Interface. 2009;6:S737–S746. doi: 10.1098/rsif.2009.0227.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuzuki K, Iwata T. Thermal comfort and thermoregulation for elderly people taking light exercise. In: Levin H, editor. Proc. Indoor Air 02. Vol. 4. Monterey, CA: 2002. pp. 647–652. [Google Scholar]
- Tsuzuki K, Ohfuku T. Thermal sensation and thermoregulation in elderly compared to young people in Japanese winter season. In: Levin H, editor. Proc. Indoor Air 02. Vol. 4. Monterey, CA, USA: 2002. pp. 659–664. [Google Scholar]
- Venners SA, Wang B, Ni J, Jin Y, Yang J, Fang Z, Xu X. Indoor air pollution and respiratory health in urban and rural China. Int. J. Occup. Environ. Health. 2001;7:173–181. doi: 10.1179/107735201800339380. [DOI] [PubMed] [Google Scholar]
- Winberry WT, Murphy N, Phinney B, Forehand L, Ceroli A, Evans A. Methods for Determination of Indoor Air Pollutants: EPA Methods. Noyes Data Corporation; 1993. [Google Scholar]
- World Health Organization. Housing and health: Identifying priorities; Meeting Report; 20–22 October 2003; Bonn, Germany. 2003. [Google Scholar]
- World Health Organization. The World Health Organization quality of life (WHOQOL)-BREF. 2004 Available at http://www.who.int/substance_abuse/research_tools/whoqolbref/en/
- World Health Organization. WHO guidelines for indoor air quality: selected pollutants. Copenhagen, Denmark: WHO Regional Office for Europe; 2010. [PubMed] [Google Scholar]
- Xu X, Wang L. Association of indoor and outdoor particulate level with chronic respiratory illness. Am. Rev. Respir. Dis. 1993;148:1516–1522. doi: 10.1164/ajrccm/148.6_Pt_1.1516. [DOI] [PubMed] [Google Scholar]