Abstract
As antibiotic resistance continues to increase among Gram-negative organisms such as Acinetobacter baumannii there is a growing need for novel therapies to overcome these resistance mechanisms. Antibiotics active against multidrug-resistant A. baumannii (MDRAB) are few, and agents in development are primarily active against other multidrug-resistant Gram-negative organisms. The combinations of colistin and antimicrobials such as glycopeptides and lipopeptides are unique potential treatment modalities against MDRAB. For both lipopeptides and glycopeptides in vitro data have demonstrated significant synergy, resulting in rapid bactericidal activity in time-kill curves. Several invertebrate in vivo models have also demonstrated increased survival compared to colistin alone. Currently, very little clinical data have focused on using these combinations for infections caused exclusively by multidrug-resistant Gram-negatives. The combination of vancomycin and colistin has been studied with conflicting results regarding both improved outcomes and risk of nephrotoxicity. Although in vitro and in vivo models have proved promising, further investigation is required to provide clinical data necessary to support the use of these combinations. The objective of this review is to summarize literature currently available for the novel combination of lipopeptides or glycopeptides with colistin for the treatment of A. baumannii, in particular MDRAB.
Electronic supplementary material
The online version of this article (doi:10.1007/s40121-014-0051-9) contains supplementary material, which is available to authorized users.
Keywords: Acinetobacter baumannii, Combination therapy, Daptomycin, Vancomycin
Introduction
Antibiotic resistance continues to be a global public health crisis [1]. The Centers for Disease Control and Prevention (CDC) state that resistant bacteria cause over two million infections in the United States annually, with a mortality rate of over 20,000 individuals per year [2, 3]. Curtailing resistance through infection control measures is key to mitigating the threat and decreasing the spread of these organisms [4]. Once patients are infected, however, optimizing antimicrobial therapy becomes paramount. This is a challenge secondary to the declining availability of active agents and dwindling pipeline of novel antibiotics. As such, antibiotic-resistant bacterial infections can result in significant morbidity and mortality, often requiring the use of second- or third-line antibiotic agents that are more toxic and/or less effective. According to the CDC’s Antibiotic Resistance Threat Assessment, multidrug-resistant Acinetobacter baumannii (MDRAB) pose a serious threat that may become urgent without public health monitoring and intervention [2]. Although there are currently antimicrobials in the later stages of development with promising activity against drug-resistant Gram-negatives, the activity against MDRAB is minimal [5, 6]. The Infectious Diseases Society of America (IDSA), in their update entitled Bad Bugs, No Drugs: No ESKAPE, states that Acinetobacter baumannii (ACB) is “emblematic of the mismatch between unmet medical needs and current antimicrobial research…” [7]. This is echoed in the 2010 update of the IDSA’s 10 ×’20 Initiative that shows eight antimicrobials in phase II or III development with none demonstrating activity against MDRAB [8]. With the rise of multidrug, extensively drug, and pandrug-resistant Acinetobacter spp. there is a critical need to discover safe and effective therapeutic strategies.
The Challenge of Acinetobacter Infections
Initially considered to have low pathogenicity, ACB is now one of the most important nosocomial pathogens, especially intensive care unit (ICU)-associated infections such as bacteremia, pneumonia, and wound infections. Often a colonizer of skin and sputum, ACB also has the ability to live on fomites, such as ventilator equipment, for prolonged periods of time [9]. Clinically, ACB infections have demonstrated increased lengths of mechanical ventilation, hospital/ICU stays, and mortality rates of 30–70% [9–12]. These organisms often harbor multiple resistance mechanisms through both selective pressures secondary to antibiotic exposure and transmission from other highly resistant organisms. A recent genomic study of Acinetobacter spp. found that these organisms has the ability to acquire over 40 resistance genes from other pathogenic Gram-negative bacteria [13]. Three main resistance mechanisms permit ACB to circumvent antimicrobial treatment: hydrolyzing enzymes, such as beta-lactamases; condensed porin channel proteins on its surface that decrease target entry sites; and alteration of cellular functions and antimicrobial targets [14]. Increasingly, multidrug- and extensively drug-resistant ACB isolates have been reported, with the incidence of carbapenem resistance exceeding 75–90% in some Asian countries [15]. There are limited therapeutic options for carbapenem-resistant isolates and these infections are associated with a high morbidity and mortality. Merely repurposing existing FDA-approved agents to treat carbapenem-resistant ACB has proved less than favorable [16]. Polymyxin antimicrobials have lost favor in treating infections secondary to toxicities associated with higher doses [17, 18]. These agents are generally considered a last resort for the treatment of multidrug-resistant Gram-negative infections such as carbapenem-resistant ACB, or after other treatments have proven ineffective. Colistin, a cationic polypeptide, interacts with anionic lipopolysaccharide (LPS) layer of Gram-negative bacteria leading to osmotic lysis of the cell. Research has focused primarily on combination therapy versus monotherapy with colistin as the primary active agent. Promising in vitro results have been demonstrated with colistin in combinations with fosfomycin, tigecycline, and carbapenems. Clinical results, primarily associated with the endpoint of mortality, have been mixed [19–22]. This review will focus on several unconventional combinations with colistin that have demonstrated possible clinical utility.
Methods
Literature associated with the combination of colistin and glycopeptides, lipopeptides, and lipoglycopeptides for the targeted treated of ACB was included in this review. All relevant English-language peer-reviewed publications were accessed through PUBMED using the following medical subject heading (MeSH) terms: vancomycin, daptomycin, telavancin, glycopeptide, lipopeptide, lipoglycopeptide, colistin, Acinetobacter baumannii, and combination therapy. Citations within these references were also assessed for inclusion. Publications in abstract form were included in the review if these abstracts were presented as part of professional meetings.
The analysis in this article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Discussion
Unconventional Approaches to Treatment
Studies with Glycopeptide Antibiotics
Until recently little was known about combinations of colistin and antimicrobials with exclusive activity against Gram-positive bacteria. Novel combinations of colistin plus glycopeptide and lipopeptide antibiotics have recently been examined, yielding positive results [23, 24]. Vancomycin is a glycopeptide antibiotic that has become a mainstay in the treatment of methicillin-resistant Staphylococcus aureus (MRSA) over the past two decades that works by inhibiting peptidoglycan synthesis in the bacterial cell wall [25, 26]. The proposed mechanism of synergy relates to the cell-membrane permeabilizing ability of colistin. Colistin causes an electrostatic interaction with LPS (lipid A), disrupting the outer membrane of the Gram-negative bacteria. This allows the otherwise large and hydrophobic vancomycin molecules to pass through the outer LPS layer and reach the site of action at the cell wall [23, 24].
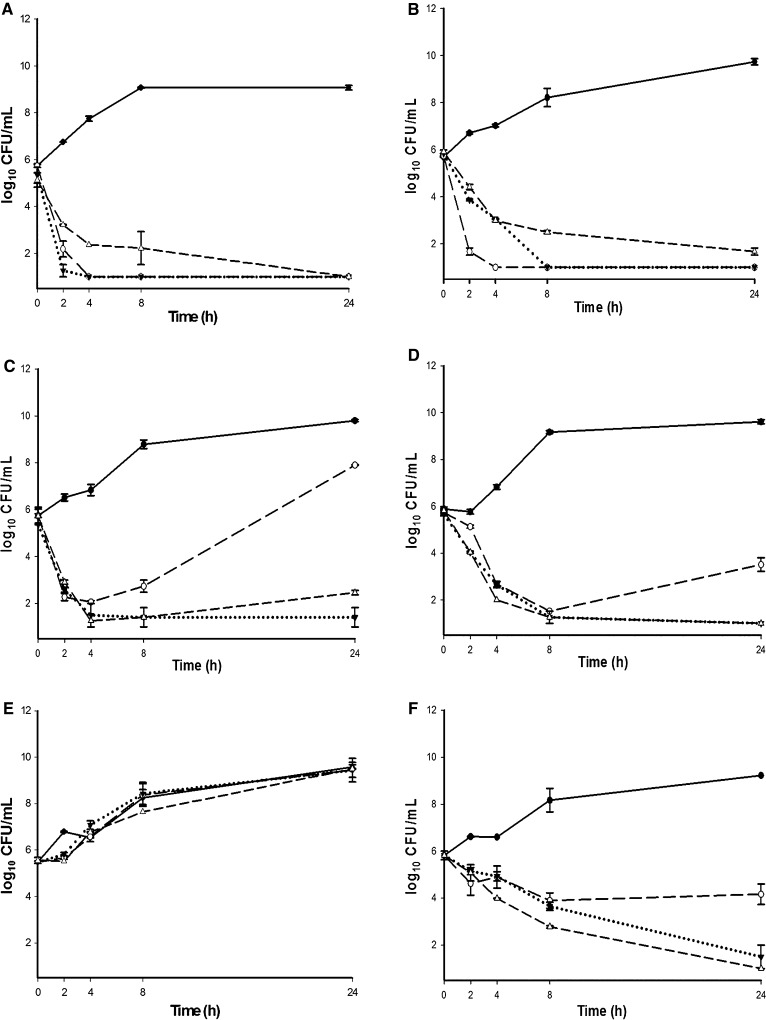
Synergy between vancomycin and colistin in MDRAB was first described by Gordon et al. [23] with in vitro checkerboard assays, synergy Etests, and time-kill curves, against 39 MDRAB isolates; five epidemic strains and 34 clinical, and one reference isolate [American type culture collection (ATCC) 19606]. For the checkerboard assays, synergy was first defined by the lowest fractional inhibitory concentration index (FICI) of ≤0.5. The FICI was calculated as [(minimum inhibitory concentration [MIC] colistin with vancomycin)/(MIC colistin alone) + (MIC vancomycin combined with colistin)/(MIC vancomycin alone)]. The second method was the two-well method wherein the absence of growth in wells containing 0.25 × MIC of both drugs and 2 × MIC of both drugs was deemed synergistic. These tests were completed on the five epidemic strains and ATCC 19606. Synergy by the Etest method was tested as the change in vancomycin MIC in colistin-supplemented versus unsupplemented agar plates. Time-kill curves against the five epidemic strains were conducted with colistin alone and with the combination of colistin and vancomycin at amounts that mimic steady-state concentrations at standard dosing—colistin 1 mg/L and vancomycin 20 mg/L. Samples were removed as 1 mL aliquots at times 0, 2, 4, 8, 24, and 48. Synergy was found by both the checkerboard assay and the two-well method, demonstrating a decrease in vancomycin MIC in four of the six tested isolates. Etest synergy was performed on all isolates. Vancomycin MICs were >256 mg/L on unsupplemented agar, while MICs in the presence of colistin ranged from 48 to <0.016 mg/L. In the time-kill curves of the five epidemic strains, colistin alone was initially bactericidal, however, regrowth occurred as early as 4 h. The combination was bactericidal and was able to suppress regrowth during the entire 48 h of incubation for all except one isolate. This isolate was plated and demonstrated a sevenfold increase in colistin MIC. A similar in vitro study was conducted using teicoplanin, a glycopeptide antibiotic with a mechanism of action similar to vancomycin [27]. Again, significant in vitro synergy with colistin was demonstrated in checkerboard assays, synergy Etests, and time-kill curves. Several other in vitro studies of similar design have also demonstrated synergy between either vancomycin or teicoplanin and colistin (Table 1 [23, 24, 27–31]) [28–30]. Of note, the study by Vidaillac et al. demonstrates the enhanced activity of the combination in ACB compared to other Gram-negative isolates (Fig. 1 [29]). Additionally, significantly enhanced survival has been demonstrated with in vivo Galleria mellonella invertebrate models during combination therapy in the treatment of ACB infections [32]. The survival rate of larvae inoculated with MDRAB treated with colistin monotherapy was 48%, compared to >90% in the vancomycin combination and 67% in teicoplanin combination.
Table 1.
Summary of in vitro studies of vancomycin (VAN), teicoplanin (TEC), telavancin (TLV), and daptomycin (DAP) in combination with colistin (COL)
| References | Isolates tested (n) | Antimicrobials tested | Synergy studies performed | Results |
|---|---|---|---|---|
| Gordon et al. [23] |
ACB ATCC 19606 Epidemic MDRAB [5] Clinical MDRAB [35] |
VAN + COL |
Checkerboard assay with FICI 2-well synergy Synergy Etest (0.5 × MIC COL) Synergy time-kill curves (1 mg/L COL, 20 mg/L VAN, 48 h) |
Checkerboard and two-well demonstrated synergy in 4/6 isolates tested Synergy kill curves resulted in sustained bactericidal activity for 48 h for 5/6 isolates tested Synergy Etest on all 40 isolates resulted in VAN MIC decrease from >256 mg/L to range 48–0.016 mg/L |
| Wareham et al. [27] |
ACB ATCC 19606 Epidemic MDRAB [5] |
TEC + COL |
Checkerboard assay with FICI Synergy Etest (0.5 × MIC COL) Synergy time-kill curves (1 mg/L COL, 20 mg/L TEC, 24 h) |
Checkerboard demonstrated synergy in all 6 isolates tested Synergy time-kill curves resulted in sustained bactericidal activity for 24 h for all 6 isolates tested Synergy Etest on all 6 isolates resulted in TEC MIC decrease from >256 mg/L to 1–2 mg/L |
| Vidaillac et al. [29] |
ACB ATCC 19606 Clinical ACB isolates [2]* PSA ATCC 27853 Clinical PSA isolates [2]* KP ATCC 7000603 Clinical KP isolates [2]* |
VAN + COL |
Checkerboard assay with FICI Synergy time-kill curves (0.25 × MIC and 0.5 × MIC each agent, 24 h) |
Checkerboard assay demonstrated synergy in all ACB isolates tested but not KP or PSA isolates (FICI >0.5) Synergy time-kill curves achieved bactericidal activity in 2–4 h and sustained through 24 h in ACB, no synergy demonstrated in COL-resistant KP or PSA |
| Hornsey et al. [30] |
ACB ATCC 19606 E. coli NCTC 12241 E. coli NCTC 11954 E. cloacae NCTC 13380R KP NCTC 13368 P. mirabilis NCTC 13376R PSA NCTC 27853 S. maltophilia NCTC 10258 S. marcescens NCTC 13382R |
TLV + COL |
Checkerboard assay with FICI Synergy time-kill curves 0.5 × MIC COL, 20 mg/L TLV, 24 h) Synergy Etest (0.5 × MIC COL) |
Checkerboard assay failed to demonstrated synergy in COL-resistant isolates, synergy per FICI seen in ACB ATCC 19606, E. coli NCTC 12241, E. coli NCTC 11954, S. maltophilia NCTC 10258, KP NCTC 13368 Similar results seen in synergy time-kill curves |
| O’Hara et al. [28] | Clinical ACB isolatesR [3] |
VAN + COL VAN + COL + DOR |
Checkerboard assay with FICI Synergy time-kill curves (2 mg/L COL, 20 mg/L VAN, 8 mg/L DOR, 24 h) |
Checkerboard demonstrated synergy in all ACB isolates Synergy time-kill curves achieved bactericidal activity in two strains with regrowth at 24 h in one strain, bacteriostatic in third isolate. The combination of VAN + COL + DOR was bactericidal in all three isolates |
| Malmberg et al. [39] | Clinical ACB isolates [15] | DAP + COL | Time-kill curve (COL 2.3 mg/L, DAP 2.1 mg/L, 8 h) | Rapid bactericidal activity (1–4 h) seen in 13 of 15 isolates, regrowth in resistant isolates |
| Phee et al. [24] |
ACB ATCC 19606 Clinical ACB isolates [5] Epidemic ACB isolates [6] Epidemic ACB isolatesR [2] Epidemic E. coli [7] Epidemic K. pneumoniae [3] Epidemic E. cloacae [2] Epidemic PSA [4] |
DAP + COL | Synergy Etest (0.125–0.75 mg/L COL), sensitization factor | DAP MIC decreased to 4–64 mg/L in COL-susceptible ACB, sensitization factor ≥2 for all COL-susceptible ACB not COL-resistant, no increase in sensitization factor for other isolates |
| Galani et al. [31] |
Clinical ACB isolates [10] Clinical ACB isolatesR [4] |
DAP + COL |
Synergy Etest (0.5 × MIC COL, 5 mg/L COL) Synergy time-kill curves 0.25×, 0.5×, and 1 × MIC COL, 5 mg/L COL, 10 mg/L DAP, 24 h) |
Etest synergy demonstrated with subinhibitory concentrations of COL for only COL-susceptible isolates Sustained killing seen in 9 of 10 COL-susceptible with 1 × MIC COL, killing was not achieved again COL-resistant isolates |
ACB Acinetobacter baumannii, ATCC American type culture collection, DOR doripenem, FICI fractional inhibitory concentration index, KP Klebsiella pneumoniae, MIC minimum inhibitory concentration, NCTC national collection of type cultures, PSA Pseudomonas aeruginosa, R COL-resistant isolate
*1/2 clinical isolates COL R
Fig. 1.
Vancomycin and colistin in Gram-negative reference and MDR isolates. In vitro evaluation of the bactericidal activity of colistin combinations at 0.5× MIC against A. baumannii ATCC 19606 (a), K. pneumoniae ATCC 700603 (b), P. aeruginosa ATCC 27853 (c), ABm1 [COL MIC = 8] (d), KPm1 [COL MIC = 32] (e), and PAm1 [COL MIC = 8] (f). Filled circle growth control, open circle colistin plus vancomycin, inverted filled triangle colistin plus trimethoprim, open triangle colistin plus trimethoprim–sulfamethoxazole. ATCC American type culture collection, COL combination with colistin, MDR multidrug resistant, MIC minimum inhibitory concentration. Reproduced with permission from Antimicrobial Agents and Chemotherapy [29]
Although the combination of glycopeptide antibiotics and colistin has demonstrated promising in vitro and in vivo results there are concerns regarding its clinical application; in particular, the risk of combining two agents with known risk of nephrotoxicity. To date there have been few clinical studies directly evaluating the efficacy and safety of this combination. In a retrospective review of patients who received at least 5 days of combination therapy against MDRAB investigators noted no significant difference in ICU length of stay or 28-day mortality (48% versus 50%) [33]. This lack of clinical correlation may be secondary to the small sample size of 57 patients. There was, however, still a significant increase in the risk of developing renal failure across any acute kidney injury network (AKIN) stage (p = 0.04). The combination was then studied in a larger cohort of critically ill patients infected with Gram-negative bacteria, including, but not limited to, patients with MDRAB [34]. Of the 184 patients included, 99 patients were infected with MDRAB, 48 received the combination of glycopeptide and colistin. The remaining patients were primarily infected with carbapenem-resistant Klebsiella pneumoniae and MDR P. aeruginosa. Overall, 68 (40.9%) of included patients received combination therapy, primarily with vancomycin. The most notable difference between patients treated with colistin alone and those treated with combination therapy was the presence of Gram-positive co-infection (41.2% versus 0.0%, p < 0.001). Thirty-day mortality was not significantly different between those treated with the combination and those treated with monotherapy (33.8% versus 29.6%). Although infection with MDRAB was an independent predictor of mortality, through cox regression the receipt of the combination for ≥5 days was shown to be protective for 30-day survival. There was no difference in renal toxicity between the patients who received glycopeptides and those that did not.
Studies with Lipopeptide Antibiotics
In addition to the glycopeptides, the lipopeptide antibiotic daptomycin and lipoglycopeptide antibiotic telavancin have been investigated in combination with colistin (Table 1). Telavancin has a dual mechanism of action wherein it acts as glycopeptide antibiotics by inhibiting transpeptidation and transglycosylation, the peptidoglycan polymerization step of cell wall synthesis, as well as altering cell membrane permeability via changing membrane potential [35, 36]. Similar to vancomycin and teicoplanin, the combination with colistin has demonstrated significant synergy in vitro and improved survival in an in vivo invertebrate model [30, 37]. Daptomycin has a unique and not yet fully elucidated mechanism of action that causes calcium-dependent destabilization of the cell membrane as well as altering the cell wall through septal defects [38]. As is the case with glycopeptides, the presence of a LPS outer membrane in Gram-negative bacteria protects against daptomycin binding to the cellular membrane.
In a 2012 abstract, Malmberg et al. [39] initially demonstrated possible synergistic activity of daptomycin in combination with colistin against 15 clinical isolates of MDRAB. The combination of 2.3 mg/L colistin and 2.1 mg/L daptomycin was effective in 13 isolates, however, regrowth after 4 h was seen. Galani et al. [31] studied the combination of daptomycin and colistin against 14 MDRAB clinical isolates. Of these, four were resistant to colistin. Synergy was tested using Etests, MICs, and time-kill curves. Daptomycin Etests were placed on agar supplemented with subinhibitory concentrations (0.5 × MIC) of colistin. The time-kill curves were completed with cation-adjusted Muller–Hinton broth over a 24-h period using 0.25×, 0.5×, and 1 × MIC of colistin for susceptible strains, 5 mg/L colistin for resistant strains, and 10 mg/L of daptomycin. In the Etests, subinhibitory concentrations of colistin were able to decrease the daptomycin MIC to 4–128 mg/L in the colistin-susceptible isolates but colistin concentrations upwards of 5 mg/L had no effect on daptomycin MICs for resistant isolates. A total of 30 isolate–concentration combinations were performed in the time-kill curves. Daptomycin and colistin demonstrated synergy against 16 of the 30 (53.3%) combinations. Among ten colistin-susceptible isolates that were exposed to 0.5 × MIC colistin bactericidal activity occurred in five (50%), compared to zero isolates exposed without daptomycin. Nine of 10 isolates exposed to colistin at 1 × MIC demonstrated bactericidal activity with no regrowth at 24 h. It appears the possible benefits of the daptomycin–colistin combination were limited to colistin-susceptible isolates and favorable results were demonstrated at 0.5 × MIC and 1 × MIC for colistin.
Phee et al. [24] tested susceptibility to the daptomycin–colistin combination in 30 Gram-negative isolates, including Escherichia coli, K. pneumoniae, and ACB. Among the fourteen ACB isolates tested was ATCC strain 19606 and two colistin-resistant isolates. Synergy was tested using daptomycin Etests on agar supplemented with subinhibitory concentrations (0.125–0.75 mg/L) of colistin versus unsupplemented agar. The results for each were compared using a “sensitization factor” (ratio daptomycin MIC alone to MIC in combination with colistin) with a factor ≤2 noting a lack of synergy. MICs for daptomycin on colistin-supplemented agar were compared to Clinical and Laboratory Standards Institute (CLSI) breakpoints for both S. aureus and enterococci spp. Daptomycin MICs for all isolates were initially >256 mg/L, a decrease in MIC (4–64 mg/L) and increase in sensitization factor (8–128) were observed in all colistin-susceptible ACB isolates, but not the two colistin-resistant or any other Gram-negatives tested. The author hypothesized that although potent synergy was demonstrated in ACB isolates the target for daptomycin may be absent in other Gram-negative bacteria.
Although most antibiotic agents possessing activity limited to Gram-positive pathogens may become active against Gram-negatives if allowed to pass the outer LPS layer, this is not true for daptomycin [40]. Daptomycin has to interact with the negatively charged phospholipids within the cell membrane. Randall et al. [40] hypothesized that the substantially lower amount of phospholipids (one-third that of S. aureus) in Gram-negatives such as E. coli may result in the lack of activity of daptomycin. After an in vitro study of the destabilizing effects of daptomycin against liposomes comprised both E. coli and S. aureus, the authors concluded that major differences in phospholipid composite affect daptomycin activity in Gram-negatives.
Conclusion
Gram-negative organisms such as ACB, in particular MDRAB, represent a serious threat to public health. Currently, fighting these infections often requires using last resort agents, such as colistin, that often have suboptimal activity when used as monotherapy and are associated with serious toxicities such as nephrotoxicity. Combination therapy with various antimicrobial agents has proven beneficial in the treatment of MDRAB; however, data are limited to retrospective studies of small sample sizes. Promising novel combinations of colistin with Gram-positive active agents such as glycopeptide or lipopeptide antibiotics have been studied primarily in vitro and in vivo. Future investigation to gain insight on the clinical impact of these combinations is required to determine the possible benefits associated with use of such combinations. In particular, elucidation of the mechanism by which these combinations seem to work best in ACB as opposed to other MDR Gram-negative pathogens and further investigation of whether higher doses of daptomycin will improve results in MDRAB [24, 40, 41]. Additionally, further description of use of these combinations in monomicrobial MDRAB infections without de-escalation to colistin monotherapy following eradication of co-infecting Gram-positive pathogens would be beneficial from a clinical perspective. It is also unclear if utilizing polymyxin B in lieu of colistin would provide similar synergistic activity against ACB or other MDR Gram-negative pathogens. Lastly, triple therapy with colistin, a lipopeptide or glycopeptide, and another agent active against MDRAB such as tigecycline or carbapenems should also be investigated in the clinical setting. With a dwindling pipeline of agents with novel mechanisms of action, finding new and unique means to employ antibiotics that are currently available is crucial to improve outcomes in these life-threatening infections.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article. All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Conflict of interest
Michael J. Rybak has received grant support, speaker or consulting fees from Cubist, Durata, Forest, Melinta, Sunovian and Theravance in addition to grant support from the NIH.
Kimberly C. Claeys and Anna D. Fiorvento have no potential conflicts of interest to declare.
Compliance with ethics guidelines
The analysis in this article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
References
- 1.Cooper MA, Shlaes D. Fix the antibiotics pipeline. Nature. 2011;472(7341):32. doi: 10.1038/472032a. [DOI] [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention (CDC). Antibiotic Resistance Threats in the United States. http://www.cdc.gov/drugresistance/threat-report-2013/ (2013).
- 3.May M. Drug development: time for teamwork. Nature. 2014;509(7498):S4–S5. doi: 10.1038/509S4a. [DOI] [PubMed] [Google Scholar]
- 4.Enfield KB, Huq NN, Gosseling MF, Low DJ, Hazen KC, Toney DM, et al. Control of simultaneous outbreaks of carbapenemase-producing enterobacteriaceae and extensively drug-resistant Acinetobacter baumannii infection in an intensive care unit using interventions promoted in the centers for disease control and prevention 2012 carbapenemase-resistant enterobacteriaceae toolkit. Infect Control Hosp Epidemiol. 2014;35(7):810–817. doi: 10.1086/676857. [DOI] [PubMed] [Google Scholar]
- 5.Farrell DJ, Sader HS, Flamm RK, Jones RN. Ceftolozane/tazobactam activity tested against Gram-negative bacterial isolates from hospitalised patients with pneumonia in US and European medical centres (2012) Int J Antimicrob Agents. 2014;43(6):533–539. doi: 10.1016/j.ijantimicag.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 6.Flamm RK, Farrell DJ, Sader HS, Jones RN. Ceftazidime/avibactam activity tested against Gram-negative bacteria isolated from bloodstream, pneumonia, intra-abdominal and urinary tract infections in US medical centres (2012) J Antimicrob Chemother. 2014;69(6):1589–1598. doi: 10.1093/jac/dku025. [DOI] [PubMed] [Google Scholar]
- 7.Boucher HW, Talbot GH, Bradley JS, Edwards JE, Gilbert D, Rice LB, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(1):1–12. doi: 10.1086/595011. [DOI] [PubMed] [Google Scholar]
- 8.Boucher HW, Talbot GH, Benjamin DK, Jr, Bradley J, Guidos RJ, Jones RN, et al. 10 × ’20 Progress–development of new drugs active against gram-negative bacilli: an update from the Infectious Diseases Society of America. Clin Infect Dis. 2013;56(12):1685–1694. doi: 10.1093/cid/cit152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Villegas MV, Hartstein AI. Acinetobacter outbreaks, 1977–2000. Infect Control Hosp Epidemiol. 2003;24(4):284–295. doi: 10.1086/502205. [DOI] [PubMed] [Google Scholar]
- 10.Nutman A, Glick R, Temkin E, Hoshen M, Edgar R, Braun T, et al. A case-control study to identify predictors of 14-day mortality following carbapenem-resistant Acinetobacter baumannii bacteremia. Clin Microbiol Infect. 2014. doi:10.1111/1469-0691.12716. [DOI] [PubMed]
- 11.Michalopoulos A, Falagas ME, Karatza DC, Alexandropoulou P, Papadakis E, Gregorakos L, et al. Epidemiologic, clinical characteristics, and risk factors for adverse outcome in multiresistant gram-negative primary bacteremia of critically ill patients. Am J Infect Control. 2011;39(5):396–400. doi: 10.1016/j.ajic.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 12.Eberle BM, Schnuriger B, Putty B, Barmparas G, Kobayashi L, Inaba K, et al. The impact of Acinetobacter baumannii infections on outcome in trauma patients: a matched cohort study. Crit Care Med. 2010;38(11):2133–2138. doi: 10.1097/CCM.0b013e3181f17af4. [DOI] [PubMed] [Google Scholar]
- 13.Fournier PE, Vallenet D, Barbe V, Audic S, Ogata H, Poirel L, et al. Comparative genomics of multidrug resistance in Acinetobacter baumannii. PLoS Genet. 2006;2(1):e7. doi: 10.1371/journal.pgen.0020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh H, Thangaraj P, Chakrabarti A. Acinetobacter baumannii: a brief account of mechanisms of multidrug resistance and current and future therapeutic management. J Clin Diagn Res. 2013;7(11):2602–2605. doi: 10.7860/JCDR/2013/6337.3626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kiratisin P, Chongthaleong A, Tan TY, Lagamayo E, Roberts S, Garcia J, et al. Comparative in vitro activity of carbapenems against major Gram-negative pathogens: results of Asia-Pacific surveillance from the COMPACT II study. Int J Antimicrob Agents. 2012;39(4):311–316. doi: 10.1016/j.ijantimicag.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Chopra S, Torres-Ortiz M, Hokama L, Madrid P, Tanga M, Mortelmans K, et al. Repurposing FDA-approved drugs to combat drug-resistant Acinetobacter baumannii. J Antimicrob Chemother. 2010;65(12):2598–2601. doi: 10.1093/jac/dkq353. [DOI] [PubMed] [Google Scholar]
- 17.Velkov T, Roberts KD, Nation RL, Thompson PE, Li J. Pharmacology of polymyxins: new insights into an ‘old’ class of antibiotics. Future Microbiol. 2013;8(6):711–724. doi: 10.2217/fmb.13.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dhariwal AK, Tullu MS. Colistin: re-emergence of the ‘forgotten’ antimicrobial agent. J Postgrad Med. 2013;59(3):208–215. doi: 10.4103/0022-3859.118040. [DOI] [PubMed] [Google Scholar]
- 19.Paul M, Carmeli Y, Durante-Mangoni E, Mouton JW, Tacconelli E, Theuretzbacher U, et al. Combination therapy for carbapenem-resistant Gram-negative bacteria. J Antimicrob Chemother. 2014;69(9):2305–2309. doi: 10.1093/jac/dku168. [DOI] [PubMed] [Google Scholar]
- 20.Sirijatuphat R, Thamlikitkul V. Colistin versus colistin plus fosfomycin for treatment of carbapenem-resistant Acinetobacter baumannii infections: a preliminary study. Antimicrob Agents Chemother. 2014;58(9):5598–5601. doi: 10.1128/AAC.02435-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poulikakos P, Tansarli GS, Falagas ME. Combination antibiotic treatment versus monotherapy for multidrug-resistant, extensively drug-resistant, and pandrug-resistant Acinetobacter infections: a systematic review. Eur J Clin Microbiol Infect Dis. 2014;33(10):1675–1685. doi: 10.1007/s10096-014-2124-9. [DOI] [PubMed] [Google Scholar]
- 22.Batirel A, Balkan II, Karabay O, Agalar C, Akalin S, Alici O, et al. Comparison of colistin-carbapenem, colistin-sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur J Clin Microbiol Infect Dis. 2014;33(8):1311–1322. doi: 10.1007/s10096-014-2070-6. [DOI] [PubMed] [Google Scholar]
- 23.Gordon NC, Png K, Wareham DW. Potent synergy and sustained bactericidal activity of a vancomycin-colistin combination versus multidrug-resistant strains of Acinetobacter baumannii. Antimicrob Agents Chemother. 2010;54(12):5316–5322. doi: 10.1128/AAC.00922-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Phee L, Hornsey M, Wareham DW. In vitro activity of daptomycin in combination with low-dose colistin against a diverse collection of Gram-negative bacterial pathogens. Eur J Clin Microbiol Infect Dis. 2013;32(10):1291–1294. doi: 10.1007/s10096-013-1875-z. [DOI] [PubMed] [Google Scholar]
- 25.Rybak MJ, Rotschafer JC, Rodvold KA. Vancomycin: over 50 years later and still a work in progress. Pharmacotherapy. 2013;33(12):1253–1255. doi: 10.1002/phar.1382. [DOI] [PubMed] [Google Scholar]
- 26.Koyama N, Inokoshi J, Tomoda H. Anti-infectious agents against MRSA. Molecules. 2012;18(1):204–224. doi: 10.3390/molecules18010204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wareham DW, Gordon NC, Hornsey M. In vitro activity of teicoplanin combined with colistin versus multidrug-resistant strains of Acinetobacter baumannii. J Antimicrob Chemother. 2011;66(5):1047–1051. doi: 10.1093/jac/dkr069. [DOI] [PubMed] [Google Scholar]
- 28.O’Hara JA, Ambe LA, Casella LG, Townsend BM, Pelletier MR, Ernst RK, et al. Activities of vancomycin-containing regimens against colistin-resistant Acinetobacter baumannii clinical strains. Antimicrob Agents Chemother. 2013;57(5):2103–2108. doi: 10.1128/AAC.02501-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vidaillac C, Benichou L, Duval RE. In vitro synergy of colistin combinations against colistin-resistant Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae isolates. Antimicrob Agents Chemother. 2012;56(9):4856–4861. doi: 10.1128/AAC.05996-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hornsey M, Longshaw C, Phee L, Wareham DW. In vitro activity of telavancin in combination with colistin versus Gram-negative bacterial pathogens. Antimicrob Agents Chemother. 2012;56(6):3080–3085. doi: 10.1128/AAC.05870-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Galani I, Orlandou K, Moraitou H, Petrikkos G, Souli M. Colistin/daptomycin: an unconventional antimicrobial combination synergistic in vitro against multidrug-resistant Acinetobacter baumannii. Int J Antimicrob Agents. 2014;43(4):370–374. doi: 10.1016/j.ijantimicag.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 32.Hornsey M, Wareham DW. In vivo efficacy of glycopeptide-colistin combination therapies in a Galleria mellonella model of Acinetobacter baumannii infection. Antimicrob Agents Chemother. 2011;55(7):3534–3537. doi: 10.1128/AAC.00230-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garnacho-Montero J, Amaya-Villar R, Gutierrez-Pizarraya A, Espejo-Gutierrez de Tena E, Artero-Gonzalez ML, Corcia-Palomo Y, et al. Clinical efficacy and safety of the combination of colistin plus vancomycin for the treatment of severe infections caused by carbapenem-resistant Acinetobacter baumannii. Chemotherapy. 2013;59(3):225–231. doi: 10.1159/000356004. [DOI] [PubMed] [Google Scholar]
- 34.Petrosillo N, Giannella M, Antonelli M, Antonini M, Barsic B, Belancic L, et al. Clinical experience of colistin-glycopeptide combination in critically ill patients infected with Gram-negative bacteria. Antimicrob Agents Chemother. 2014;58(2):851–858. doi: 10.1128/AAC.00871-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhanel GG, Calic D, Schweizer F, Zelenitsky S, Adam H, Lagace-Wiens PR, et al. New lipoglycopeptides: a comparative review of dalbavancin, oritavancin and telavancin. Drugs. 2010;70(7):859–886. doi: 10.2165/11534440-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 36.Saravolatz LD, Stein GE, Johnson LB. Telavancin: a novel lipoglycopeptide. Clin Infect Dis. 2009;49(12):1908–1914. doi: 10.1086/648438. [DOI] [PubMed] [Google Scholar]
- 37.Hornsey M, Phee L, Longshaw C, Wareham DW. In vivo efficacy of telavancin/colistin combination therapy in a Galleria mellonella model of Acinetobacter baumannii infection. Int J Antimicrob Agents. 2013;41(3):285–287. doi: 10.1016/j.ijantimicag.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 38.Pogliano J, Pogliano N, Silverman JA. Daptomycin-mediated reorganization of membrane architecture causes mislocalization of essential cell division proteins. J Bacteriol. 2012;194(17):4494–4504. doi: 10.1128/JB.00011-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Malmberg CAL, Bertiolsson-Forsberg P, Lagerback P. Colistin in combination with daptomycin enhances the effect against A. baumannii. London: European Congress of Clinical Microbiology and Infectious Diseases (ECCMID); 2012.
- 40.Randall CP, Mariner KR, Chopra I, O’Neill AJ. The target of daptomycin is absent from Escherichia coli and other gram-negative pathogens. Antimicrob Agents Chemother. 2013;57(1):637–639. doi: 10.1128/AAC.02005-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tangden T, Hickman RA, Forsberg P, Lagerback P, Giske CG, Cars O. Evaluation of double- and triple-antibiotic combinations for VIM- and NDM-producing Klebsiella pneumoniae by in vitro time-kill experiments. Antimicrob Agents Chemother. 2014;58(3):1757–1762. doi: 10.1128/AAC.00741-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.