Abstract
This paper addresses the need for diet assessment methods that capture the rapidly changing beverage consumption patterns in China. The objective of this study was to develop a 3-day smartphone-assisted 24-hour recall to improve the quantification of beverage intake amongst young Chinese adults (n=110) and validate, in a small subset (n=34), the extent to which the written record and smartphone-assisted recalls adequately estimated total fluid intake, using 24-hour urine samples. The smartphone-assisted method showed improved validity compared to the written-assisted method, when comparing reported total fluid intake to total urine volume. However, participants reported consuming fewer beverages on the smartphone-assisted method compared to the written-assisted method, primarily due to decreased consumption of traditional zero-energy beverages (i.e. water, tea) in the smartphone-assisted method. It is unclear why participants reported fewer beverages in the smartphone-assisted method than the written-assisted method. One possibility is that participants found the smartphone method too cumbersome, and responded by decreasing beverage intake. These results suggest that smartphone-assisted 24-hour recalls perform comparably but do not appear to substantially improve beverage quantification compared to the current written record based approach. In addition, we piloted a beverage screener to identify consumers of episodically consumed SSBs. As expected, a substantially higher proportion of consumers reported consuming SSBs on the beverage screener compared to either recall type, suggesting that a beverage screener may be useful in characterizing consumption of episodically consumed beverages in China’s dynamic food and beverage landscape.
Keywords: Diet assessment, nutrition epidemiology, mobile technology, sugar sweetened beverages, China
INTRODUCTION
During recent decades, the nutrition transition in China has been characterized by a shift towards energy dense diets, reduced physical activity, and increasing rates of obesity.1-3 This transition is often marked by increased consumption of caloric sweeteners and specifically sugar-sweetened beverages (SSBs) like soda and soft drinks.4-8 SSB consumption has been linked to increased risk of obesity, type II diabetes, and cardiovascular disease.9-11 However, evidence regarding SSB consumption in China is mixed: sales data show that sales of soft drinks and other beverages including fruit juice, sweetened tea, and bottled water are rapidly growing,12,13 yet dietary data show that SSB consumption in China remains quite low.14
The discrepancy between beverage sales and consumption data suggests that current methods of beverage intake assessment may not adequately capture all beverage consumption. Since 1989, the China Health and Nutrition Survey (CHNS) has used 3 consecutive 24-hour recalls, with written notes to aid recall, to capture short-term food and beverage intake. While the 24-hour recall is a widely used and relatively accurate method for obtaining diet intake data,15 it is prone to omissions and inaccurate portion size estimation,16,17 and the extent of underreporting varies by numerous factors, including sex, age, and overweight/obesity.18-22
The recent development of smartphone technology for diet assessment has offered a promising new way to record beverage consumption, as participants can easily capture images of beverages prior drinking.23,24 In particular, video records provide an enhanced ability to see all food items in a shot, and also can encompass voice annotation, allowing the participants to describe the foods or beverages consumed.25 These videos and vocal records can then be used during 24-hour recalls to prompt memory and aid portion size estimation, improving the accuracy of the 24-hour recall.26 In addition, Ecologic Momentary Assessment (EMA) periodically prompts participants to record beverages they have recently consumed, 27,28 further reducing the likelihood of omission. Because the smartphone video record provides a multi-pronged approach for memory enhancement, including visual and audio components and periodic prompts, it has the potential to improve 24-hour recalls beyond the written record that is currently used to enhance recalls in the China Health and Nutrition Survey. However, little worked has explored whether these features can be used to enhance recall and reduce omissions of beverages during 24-hour recalls in a Chinese population.
In addition, 24-hour recalls may miss beverages that are only sporadically consumed, potentially resulting in an underestimation of the proportion of SSB consumers in China, where such beverages are currently infrequently consumed. Accurately capturing intake of episodically consumed beverages such as SSBs is important in China, where rapid changes in the food and beverage landscape could mean that a beverage that is infrequently consumed today may be widely and readily consumed in the near future. Typically, food frequency questionnaires have provided a valid, reliable method to assess intake over longer periods of time and thus better capture infrequently consumed foods.29 However, to our knowledge, no work has tested the use of a short, beverage-specific food frequency questionnaire (i.e. beverage screener) in this population. Thus, a second key question is whether the use of a beverage screener can improve estimation of episodically consumed beverages to pinpoint emerging patterns in SSB consumption in China.
The objectives of this study are to 1) compare beverage consumption data collected using a 3-day smartphone-assisted 24-hour recall (SA-24R) vs. beverage data collected using the current CHNS gold standard of measuring dietary intake, the written record-assisted 24-hour recall (WA-24R) and 2) validate, in a small subset, the extent to which each recall method adequately estimates total beverage intake based on correlation with total urine volume measured in 24-hour urine samples. We hypothesized that the smartphone-assisted approach would improve the current written record-assisted approach to collecting beverage intake by minimizing omissions and improving quantification of beverages. Specifically, we hypothesized that participants would report higher intake of SSBs and total beverages in the SA-24R compared to the WA-24R. The third objective of this study is to pilot and evaluate the use of a beverage screener (BEVQ) to identify consumers of episodically consumed SSBs. We hypothesized that the proportion of participants consuming SSBs would be higher in the BEVQ than from either recall method.
MATERIALS AND METHODS
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the institutional review boards at University of North Carolina, Chapel Hill; University of California, Berkeley; and the Shanghai Center for Disease Control and Prevention. Written consent was obtained from all subjects.
A screenshot of the EMA as well as a supplemental document containing additional results will be available by emailing the corresponding author.
Study population
Healthy adults age 20 to 40y were recruited from communities in urban Shanghai and a nearby rural district between March and May of 2013 by contacting community leaders of registered residents in each neighborhood. Of 120 participants who were contacted and randomized, 117 signed the consent. One participant dropped out prior to dietary data collection, and 3 participants were excluded for having received prior diagnoses of hypertension or diabetes, leaving a sample of 110 participants (52 rural, 58 urban) (Supplement Figure 1). Forty-six participants (22 rural, 24 urban) volunteered to participate in two 24-hour urine collections.
Data Collection
Participation involved completion of a demographic questionnaire, anthropometry, BEVQ, SA-24R, and WA-24R. All questionnaires and interviews were conducted in Mandarin. Dietary data was collected Saturday evening to Tuesday evening of each week, for two consecutive weeks, in order to capture 1 weekend day and 2 weekdays for each recall type.30 Participants were randomized to participate in the SA24-R and WA-24R as follows: Sequence 1: (Week 1) SA-24R + BEVQ, (Week 2) WA-24R; or Sequence 2: (Week 1) WA-24R, (Week 2) SA-24R + BEVQ. Recalls collected on sequential periods that captured the same days of the week were used to minimize potential respondent fatigue, 31-34 as well as learning effects, since factors such as increased familiarity may influence reporting on subsequent recalls.30,35 As administering recall series within a one week timeframe could also lead to a learning effect, participants were randomized to either the WA-24R or the SA-24R first. Because beverage intakes may have varied across periods encompassed by the different recall types, the mean intake across both periods was used as the estimate of “usual intake”. Similar to other dietary validation studies, our aim was to assess the concordance of estimated usual intakes based on different assessment methods.36-38 Both methods were also validated against total urine volume in a subset of participants, as described below.
For all participants, Visit 1 included the completion of a demographic questionnaire about age, education, occupation, and disease history. Visit 1 also included anthropometric measurements. Height was measured to the nearest centimeter using a wall-mounted stadiometer and body weight was measured in light clothing without shoes to the nearest 0.1 kilogram using an electronic scale (Seca, Hanover,MD). Body mass index (BMI) was calculated as kg/m2 and overweight/obesity was defined as having a BMI ≥ 25 kg/m2.39 Sequence 1 participants then received training on how to complete the SA-24R and Sequence 2 participants received training on how to complete the WA-24R, including use of a guidebook to assist with portion size estimation. Each participant also received a user manual on smartphone operation. For each recall type, the 24-hour recalls were conducted each evening from Sunday to Tuesday.
During the SA-24R, participants were provided with a smartphone (Samsung Galaxy Y), and asked to wear it on their waist in a small belt during all waking hours and utilize the CalFit system of applications installed on each device.40-42 For all beverages and foods consumed, participants were instructed to place a provided fiduciary marker next to the items and take a brief video of the items. Using a provided script template, participants stated their location, the time, the items to be consumed, and the portion sizes of the items. In addition, on 4 occasions throughout the day, the participants were prompted to complete a brief EMA asking if they had consumed any beverages in the preceding hours, the beverage type, and if they added anything to the beverage (ice, sugar, cream, etc) (Supplement Figure 2). During the 24-hour recall, trained interviewers reviewed the videos with the participants to prompt their recall of foods and beverages consumed.
During the WA-24R, participants were asked to write notes on a paper log about all food and beverages consumed. The written notes included the general type of food but not portion size, condiments, or recipes (i.e. “bowl of noodles”). During the 24-hour recall, interviewers reviewed the written notes with the participants. All diet recall data were coded and entered by trained staff at the Shanghai CDC and checked for completeness.
Energy and water per 100 g for each beverage were based on a Chinese food composition table (FCT) in which all foods were measured using the Perkin-Elmer Analyst 800.43 For beverages which have not yet been updated in the Chinese FCT due to their new emergence in the food supply, composite nutrient values for similar foods from the USDA food database were used.44 Total fluid intake included all fluid in beverages, soups, and foods. Beverages were categorized into beverage groups and classified as an SSB or non-SSB based on their level of processing (fresh or packaged/bottled) and added sugar content (Supplement Table 1). SSBs include soda, sports drinks, sweetened fruit drinks, sweetened milk drinks, sweetened coffee and tea, and smoothies. Beverages with zero energy were categorized into traditional zero-energy beverages, which included water, loose-leaf tea, and soup (often consumed as a beverage in China), and bottled zero-energy beverages, which included diet soda and unsweetened bottled teas. A recall day was considered eligible for inclusion in the study if the participant completed the dietary interview, total kJ were >2092 kJ and <20920 kJ and total fluid intake were >500g and <4000 g, as values outside this range are considered extreme and may not reflect usual intake.45 Of 110 participants, 84% recorded 6 eligible recall days, 11% recorded 5 days, 3% recorded 4 days, and 2% recorded 2 or 3 recalls days.
To validate total fluid intake collected by the 24-hour recalls, volunteers participating in the urine sample sub-study provided two 24-hour samples, one each for the SA-24R and the WA-24R.46-49 Participants collected all urine beginning with the first urine of the second day of the recall until the first urine on the third day of the recall in provided leak-proof plastic containers, and recorded start and stop times.46 Urine samples were analyzed for total volume (mL). Urine samples were considered complete if the participant reported a duration between 22 and 26 hours and total volume was >500 mL.50 Using a power calculation for paired t-tests, to achieve 80% power at an alpha of 0.05 to detect a 50 mL difference between fluid intake and urine output, 32 volunteers were needed to participate in each urine sample.
BEVQ Development and Testing
The BEVQ was developed to capture episodic intake and estimate mean daily intake of beverage categories including water, sugar sweetened beverages, and alcohol and two open-ended questions for “other” beverages (Supplement Table 2). The beverage categories were adapted from a validated beverage questionnaire screener in consultation with a panel of experts about beverages that are commonly consumed in China.51 The BEVQ was piloted amongst staff at the Shanghai CDC to evaluate whether the questionnaire was understandable and comprehensive.52 For each beverage, participants selected whether they consume the specific category of beverage (yes/no), the frequency of intake (daily, weekly, monthly, yearly), how often they drink the beverage during the selected unit (1-7 occasions, with an open category for >7), and how much they drink when they drink the beverage (mL). For comparison with the SA-24R and WA-24R, traditional and bottled zero calorie beverages were combined into one category, since the BEVQ did not have a separate item for bottled water. In addition, soup intakes from the recalls were excluded in this comparison since soup was not an item on the BEVQ. Other categories included 100% juice, unsweetened milk, alcohol, and SSBs (including soda, fruit drinks, sweetened tea, smoothies, and sweetened coffee beverages).
To derive average daily intake, the unit of frequency was multiplied by the number of occasions the beverage is consumed during that unit and multiplied by the amount consumed during each occasion, then divided by the number of days in that unit of frequency. (For example, 1 week × 6 occasions/week × 100 mL/occasion × 1 week/7 days). Average daily grams and energy for each beverage was determined by multiplying the number of ml per day by the energy and grams per ml for each category.
For all participants, the BEVQ was administered on the last day of the SA-24R. However, because the BEVQ asks about each participant’s usual intake of beverages rather than recent or short-term intake, answers to the BEVQ refer to each participant’s long-term pattern of beverage intake rather than intake of beverages while they were participating in the study.
Statistical analyses
All statistical analyses were performed using STATA, version 12 (Stata Corporation, College Station, Texas). Mean daily intake was calculated as total intake (in grams and kJ) of each beverage group divided by number of eligible recall days for each participant. Mean intake in grams and kJ of total beverages and each beverage category for the SA-24R and WA-24R were compared using paired t-tests and Spearman rank correlation coefficients. Bland Altman plots were used to assess bias between SA-24R and WA-24R. Pearson correlation coefficients were calculated to assess total fluid intake reported in the SA-24R and WA-24R against total urine volume from the respective 24-hour urine samples. Quartiles of mean daily intake were used to derive weighted k statistics to assess the level of agreement between the SA-24R, WA-24R, and BEVQ for key beverage categories. Repeated measures mixed models were used to assess the effects of overweight/obese, urbanicity, and sequence on mean beverage intake in the SA-24R compared to the WA-24R.
RESULTS
The sample was 54% male and mean age was 29.6 y (± 0.29). Twenty-four percent of participants were overweight/obese (n=26).
Mean beverage intakes (g) from the SA-24R and the WA-24R are presented in Table 1. During the SA-24R, participants reported 222 fewer g/day total beverages than in the WA-24R (p <0.01). Differences in beverage intake reporting by recall method were largely attributable to traditional zero-energy beverages, as participants reported 229 fewer g/day of traditional zero-energy beverages during the SA-24R compared to the WA-24R (p <0.01). Mean intake of zero-energy bottled beverages was 12 g higher during the SA-24R compared to the WA-24R, but this difference was not statistically significant. Mean intakes of soda and soft drinks, sweetened tea and coffee, sweetened fruit drinks, sweetened milk, and total SSBs were not different between the SA-24R compared to the WA-24R. Examining caloric beverages only, participants reported mean ± SE 522±66 kJ/day total beverage intake during the WA-24R compared to 441±55 kJ/day during the SA-24R (p=0.226) ( Supplement Table 3). Mean intake of SSBs was 350 ± 56 kJ/day during the WA-24R compared to 296 ± 9 kJ/day during the SA-24R (p=0.492).
Table 1.
Mean daily beverage intake (g) from SA-24R compared to the WA-24R†
| SA-24R | WA-24R | |||||
|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Spearman rank | Mean difference (%)‡ |
|
|
|
|
|
|
|||
| All Beverages, Total | 1088* | 51 | 1310 | 53 | 0.60** | −222 (−17) |
| Traditional Zero -Energy Beverages | 761* | 48 | 990 | 59 | 0.64** | −229 (−23) |
| Zero-Energy Bottled Beverages | 102 | 20 | 90 | 25 | 0.42** | 12 (13) |
| 100% Fruit Juice | 22 | 6 | 27 | 6 | 0.210 | −4 (−19) |
| Milk, Unsweetened | 56 | 10 | 59 | 10 | 0.47** | −3 (−5) |
| Soda and Soft Drinks | 27 | 8 | 47 | 12 | 0.35** | −20 (−43) |
| Tea and Coffee, Bottled/Sweetened | 31 | 9 | 36 | 9 | 0.44** | −5 (−14) |
| Fruit Drinks, Sweetened | 7 | 3 | 6 | 2 | −0.060 | 1 (−17) |
| Milk, Sweetened | 54 | 12 | 51 | 13 | 0.45** | 3 (6) |
| Alcohol | 29 | 11 | 35 | 13 | 0.60** | −6 (−17) |
| SSB, Total | 137 | 20 | 162 | 25 | 0.50** | −25 (−15) |
Mean individual difference between SA-24R and WA-24R in grams and percentage in parentheses. For each individual, the percentage difference was calculated as (mean beverage intake from SA-24R - mean beverage from WA-24R/mean beverage from WA-24R)*100
From paired t-test, the mean from the SA-24R was significantly different from the mean from WA-24R for any beverage type (p<0.01)
Spearman rank correlation coefficient for beverage type between SA-24R and WA-24R was significant (p<0.01)
Spearman correlation coefficients (Table 1) ranged between 0.21 (fruit juice) and 0.60 (total beverages) for mean beverage intake (g) between the SA-24R and WA24R, with the exception of a correlation of −0.06 for sweetened fruit drinks. This latter beverage type was the smallest contributor (<3%) to beverage intake. SSBs had a correlation coefficient of 0.50 for mean grams of intake (p<0.001). Results were similar for kilojoules (data not shown).
Of 44 volunteers who agreed to provide 24 h urine samples during the SA-24R, 34 provided a complete urine sample and of 46 volunteers during the WA-24R, 36 provided a complete sample, providing >80% power to detect a 50mL difference between urine volume and total fluid output at an alpha of 0.05 for each recall type. Among subjects with complete samples, total urine volumes ranged from 528 to 2562 mL, with no meaningful difference in fluid intakes reported on urine sample collection days vs. other days among sub-study participants (data not shown). Total fluid intake during the SA-24R was 1208 ±140 mL compared to total urine volume of 1342±88 mL, with a Spearman correlation of 0.42 (p=0.014). Total fluid intake during the WA-24R was 1400±130 mL compared to total urine volume of 1336±93 mL, with a correlation of 0.31 (p=.0624). Scatter plots of urine volume vs. reported fluid intake suggested of presence of 4 individuals in each recall with extremely poor agreement (>1200ml or <−1200ml difference between total urine volume and total fluid intake). Excluding these individuals improved Spearman correlations to 0.58 for the SA-24R(p<0.01) and 0.46 for the WA-24R(p=0.01).
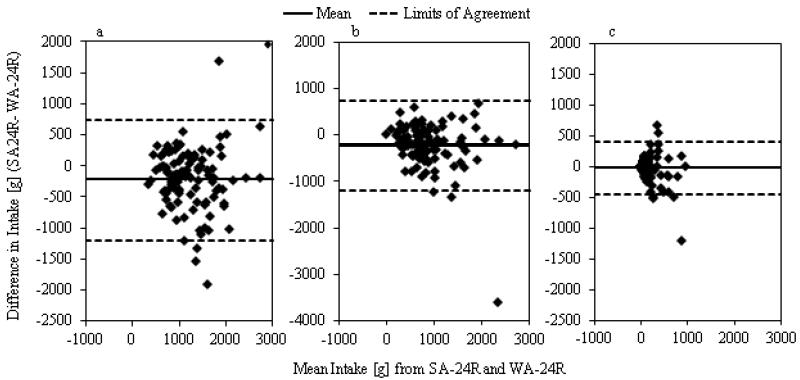
Figure 1a, b, and c showed the Bland Altman Plot comparing mean daily intake (g) from beverages in the SA-24R to the WA-24R. For total beverages, the mean bias was −222g (95% CI −313g to 131g). The mean bias for traditional zero-energy beverages was −228g (95%CI −321g to 137g) and for SSBs, the mean bias was −25g kJ (95% CI −64g to 15g), showing lower intakes for each beverage type in the SA-24R.
Figure 1a,b,c.
Bland-Altman Plot of a) Total Beverage Intake b) Traditional Zero Energy Beverage Intake and c) Sugar-Sweetened Beverage Intake between SA-24R and WA-24R[g/d]
The mixed models for repeated measures indicated that there was no difference in reporting of total beverages between the two recall types by urbanicity. Being overweight/obese was associated with decreased reporting of total beverage intake on the SA-24R (Supplement Figure 3). Overweight/obese participants reported 430 g/day fewer beverages on the SA-24R than on the WA-24R, while non-overweight participants underreported beverages on the SA-24 relative to the WA-24R by 158 g/day (p<0.01). Overweight/obese participants also reported 65 g/day fewer SSBs on the SA-24R relative to the WA-24R, while non-overweight participants reported 12 g/day fewer SSBs on the SA-24R relative to the WA-24R. However, these differences were not statistically significant (p=0.266). Sequence also mattered: overall, those who completed the SA-24R in the first week first reported 89 fewer g/day total beverages on the SA-24R compared to the WA-24R. However, those who completed the WA-24R in the first week reported 360 fewer g/day total beverages on the SA-24R than on the WA-24R (p<0.01) (not shown). There were no differences in reporting of SSBs on the SA-24R compared to the WA-24R by urbanicity, sequence, or overweight.
Since episodically consumed beverage types may not be captured with a limited number of recalls, we also compared intakes reported on BEVQ vs. the mean of three 24R collected using both methods. Percent consumers and weighted k statistics for the SA-24R, WA-24R, and BEVQ are reported in Table 2. With the exception of zero-energy beverages, more participants reported consuming other beverage types in the BEVQ than in either recall type. Notably, 88% of participants reported consuming SSB in the BEVQ compared to only 55% and 56% in the SA-24R and the WA-24R, respectively (p<0.05). Participants reported higher mean daily intakes of beverages in the BEVQ, including total beverages (1326 ± 90 g), water (1031 ± 79), 100% juice (18 ± 5 g), milk (56 ± 10 g), and SSBS (185 ± 26 g).The SA-24R and the WA-24R demonstrated similar fair levels of agreement with the BEVQ for quartiles of intake of total beverages, SSBs, and alcohol, with k statistics ranging from 0.27 to 0.36. Non-sweetened beverages including zero calorie beverages, 100% fruit juice, and unsweetened milk showed only slight agreement between recall types with the BEVQ. Total beverages and SSBs showed moderate correlation between the recall methods and the BEVQ, with Spearman correlations of 0.31 and 0.43 for total beverages for the SA-24R and WA-24R, respectively (p<0.01), and correlations of 0.48 and 0.43 for SSBs for the SA-24R and WA-24R, respectively (p<0.01).
Table 2.
Percent consumers and weighted κ statistics for the SA-24R, WA-24R, and BEVQ†
| % Consumer | SA-24R vs. WA-24R | SA24-R vs. BEVQ | WA24-R vs. BEVQ | ||||||
|---|---|---|---|---|---|---|---|---|---|
| SA-24R | WA-24R | BEVQ | κ | % Agreement | κ | % Agreement | κ | % Agreement | |
|
|
|
|
|
|
|||||
| Zero-Energy Beverages‡ | 100 | 100 | 99 | 0.51 | 80 | 0.21 | 67 | 0.33 | 72 |
| 100% Fruit Juice | 19ab | 23 | 44 | 0.19 | 73 | 0.21 | 69 | 0.13 | 64 |
| Milk, Unsweetened | 35b | 38a | 51 | 0.36 | 74 | 0.14 | 61 | 0.28 | 67 |
| Sugar Sweetened Beverages | 55ab | 56a | 88 | 0.38 | 72 | 0.29 | 68 | 0.30 | 69 |
| Alcohol | 8ab | 9a | 45 | 0.59 | 94 | 0.29 | 73 | 0.27 | 72 |
| All Beverages, Total | -- | -- | -- | 0.49 | 79 | 0.31 | 71 | 0.36 | 73 |
SA-24R is the 3-day consecutive smartphone-assisted 24-hour recall, WA-24R is the 3-day consecutive written-assisted 24-hour recall, and BEVQ is the China Beverage Validation Study beverage screener.
Zero calorie beverages includes traditional zero calorie beverages like water and tea, as well as bottled zero calorie beverages.
Significantly different from BEVQ, p <0.05 from χ2 test
Significantly different from WA-24R, p<0.05 from χ2 test
DISCUSSION
In this study, the SA-24R and WA-24R showed moderate correlation between reported fluid intake and total urine output. Correlations between the two methods showed moderate agreement across beverage categories, with an average Spearman rank correlation of 0.42. Despite these moderate correlations, mean beverage intake was significantly lower by 222 g/day in the SA-24R compared to the WA-24R. This study also showed significantly lower reporting of beverage intake on the SA-24R by overweight participants compared to normal weight participants.
Overall, the correlations between the SA-24R and WA-24R were similar to those found when comparing nutrients in short-term diet assessment methods across different time periods.36,37 For example, comparing two 24-hour recalls and a 4-day food record, Frankenfeld found Pearson correlations between 0.4 and 0.6 for most nutrients, with moderate to low k values for quartiles (k=0.11 to 0.52).36 The underreporting of mean intake on the SA-24R is similar to other studies of digital diet assessment when compared to paper-based methods. For example, participants underreported energy by 640 kJ on a record of voice-annotated photograph of food items compared to a concurrent written food diary .25 Lazarte, who also used a digital food record to enhance (rather than replace) 24-hour recalls, reported that despite high correlations for most nutrients, participants underreported nutrients when using the modified-24h recall method compared to a weighed food record.26
One explanation for the decreased reporting in the SA-24R is that when a participant forgets or chooses not to take a video of a beverage, and the video log is used to prompt memory during the 24-hour recall, the participant may be more likely to omit the beverage than they would if the participant were using a written log to jog the memory.27 Since the written record contains fewer details than the video record, participants may have been less reliant on the written record during a recall, and so less prone to omission of an absent beverage. Conversely, they may have had more familiarity with the written record and found it easier to briefly note the beverage than to take a voice-annotated video, increasing the memory-enhancement capability of the written record compared to the video record.
Another explanation is that the smartphone-based approach may have influenced consumption patterns, as participant reactivity to the method is unknown.27 One possibility is that the decreased reporting of traditional zero-energy beverages in the SA-24R was not misreporting, but a reflection of participants consuming fewer traditional zero-energy beverages when using the smartphone. Perhaps using a smartphone increased participant’s awareness of how much they were drinking, or was simply too cumbersome to use, resulting in decreased consumption of these beverages. For example, some participants reported that they felt embarrassed while taking videos of food in public places or at work. Higher respondent burden on the SA-24R may also explain why participants who completed the WA-24R first reported fewer beverages on the SA-24R than those who completed the SA-24R first. Since the SA-24R was more difficult to complete, participants who had already completed the WA-24R felt even more burdened by the SA-24R relative to the WA-24R and responded by reporting fewer beverages on the SA-24R.
It is possible that simply photographing beverages prior to consumption would yield the same benefit for enhancing memory during the 24-hour recall, but would be less cumbersome. Similarly, the use of EMA alone, without photos, to prompt participants to think about beverage intake throughout the day may achieve the same memory-enhancement benefit and be even less burdensome. Future work is required to understand which method provides the greatest benefit in terms of reducing omission and improving portion size estimation during the 24-hour recall, while minimizing respondent burden and remaining culturally acceptable.
Notably, however, the majority of underreporting in the SA-24R relative to the WA-24R was accounted for by differences in the reporting of traditional zero-energy beverages (water, tea) and there were no substantial differences in intake or energy for any other beverage. This suggests that both methods provide similar estimates of intakes of energy-containing beverages. The findings from SA-24R correlated with those of the WA-24R with regard to SSBs. One possibility is that respondents are more likely to record and also to remember beverages that are sold in discrete packaged containers, such as a can of Cola or a pouch of sweetened milk, than they are beverages that are consumed continuously, like tea and water. In addition, traditional zero-energy beverages are very frequently consumed in China, making them less memorable than rarely-consumed SSBs, and potentially contributing to increased omissions.
Despite the apparent decreased reporting in the SA-24R compared to the WA-24R, the SA-24R showed stronger correlation with total urine output than did the WA-24R, suggesting higher validity. One alternate explanation for the higher reported intake of traditional zero-energy beverages like water and tea in the WA-24R relative to the SA-24R is that when using the written method, participants overestimate their intake of these beverages. Such an effect could occur because the written record provides less detail than the smartphone video record, making it more difficult to accurately estimate portion size during the 24-hour recall. Although we were adequately powered to detect a 50 mL difference between total fluid intake and total urine volume, further research using additional validation methods such as hydration biomarkers is required to understand the nature of beverage intake misreporting using both of these instruments.
The Bland-Altman plots showed that for total beverages and for SSBs, the bias between the SA-24R and WA-24R was not consistent across levels of intake, with the bias increasing with higher intakes of beverages. Previous studies have shown that although portion size estimation from digital photography is valid,53,54 people are more likely to correctly estimate smaller portions and more likely to underestimate larger portions.54,55 In addition, most studies testing the validity of portion size estimation from digital photographs have compared estimation from photographs against direct estimation in real time. More research is needed to understand how estimation from digital images and direct estimation compare when recall occurs at a later time, such as during a typical 24-hour recall.
Decreased reporting on the SA-24R relative to the WA-24R by overweight/obese participants is not surprising, considering other digital diet assessment studies have shown that obese men showed more underreporting using personal digital assistant to record food intake than did normal weight men.56 Interestingly, however, we found that overweight/obese participants did not show decreased reporting of SSBs on the SA-24R relative to the WA-24R, compared to normal weight participants. This result is in contrast to previous work, which shows that overweight and obese individuals are more prone to social desirability bias, and tend to report lower energy from perceived “unhealthy foods” like snacks, high fat, and high carbohydrate foods.22,57,58 We would expect that taking videos of unhealthy beverages like SSBS would further exacerbate this bias if overweight or obese participants were more embarrassed to show videos of the foods they have consumed, resulting in decreased reporting of SSBs on the SA-24R relative to the WA-24R. One explanation for the lack of this effect in the current study is that the tendency to underreport SSBs increases with BMI, with obese participants showing greater underreporting than overweight or normal weight participants. However, due the limited sample size of obese participants in this study (n=5), we were unable to test whether obese participants respond differently to the SA-24R than the overweight participants.
The majority of respondents reported consuming SSBs. Although a number of studies have reported that the multiple-day 24-hour recall method can be a good estimator of usual nutrient intake at the population level,59,60 a much higher proportion of respondents reported consuming SSBs in the BEVQ than in either recall method. The recall methods showed moderate correlation with the BEVQ for total beverages and SSBs, consistent with results from Hedrick, who found correlations between 0.46- 0.49 for total beverage and SSB intake between a beverage screener and 4-day food record.51 The higher proportion of consumers in the BEVQ reflects the changing diet patterns in China: while the number of consumers of SSBs is increasing rapidly, many of these consumers still drink SSBs only episodically (less than once a week, usually on special occasions), and hence this consumption may not be reflected in 3-day consecutive recalls. Methods that incorporate both the probability of consumption based on frequency questionnaires, along with recalls, to estimate and the amount of intake, such as the NCI method or Multiple Source Method can provide a better estimation of emergent beverage consumption patterns in China’s dynamic food environment.61,62
This study had several important limitations. Due to rapid changes in China’s food supply, the FCT does not contain all the newly available beverages, making it difficult for interviewers to correctly identify emergent beverages like SSBs. In this study, all beverages were examined and coded to the appropriate beverage group, including new beverage groups created explicitly for this study, by trained researchers. However, it is possible that the discrepancy between the FCT and the current Chinese food supply accounts for more of the low reporting of SSBs in Chinese nutrition surveys than do issues with the current recall method. In addition, the recalls were conducted on consecutive days, and SA-24R and WA-24R were conducted on consecutive weeks, which reduces intra-individual variation in beverage intake. It is also unclear why underreporting on the SA-24R was greater when the WA-24R was completed first. One possibility is that, if the WA-24R was more difficult to complete, respondents who completed the WA-24R first felt more burdened by the study and thus reported fewer beverages during the SA-24R during the second week. While the EMA was helpful in prompting participants to recall their beverage intake, there is also a strong possibility that the receipt of reminders throughout the day altered beverage consumption of the respondents. Future research should address the extent to which the EMA and process of taking videos affects the type and amount of beverages and foods participants consume.
Conclusion
The use of a SA-24R does not appear to improve the quantification of beverage intake compared to a WA-24R recall in a Chinese population. The SA-24R may be a useful aid for capturing images of SSBs and other packaged beverages, but substantial underreporting or under-consumption of water and other non-caloric beverages, particularly by overweight individuals, poses a considerable barrier to future use of this instrument for overall beverage intake. The incorporation of a beverage screener may be useful in identifying episodic consumers of SSBs in addition to recall methods. More work is required to understand the optimal method for collecting information on beverage intake in the dynamic Chinese food environment.
Supplementary Material
ACKNOLWEDGEMENTS
We thank the staff at the Shanghai Municipal Center for Disease Control and Prevention for their help in the data design and collection process, and the staff at the Songjiang and Putuo district Health Centers for their assistance conducting interviews. We also wish to thank Dr. Phil Bardsley for assistance with the data management and programming and Mr. Tom Swasey for graphics support. This study was reviewed and approved by the Institutional Review Boards at University of North Carolina, Chapel Hill, University of California, Berkeley, and the Shanghai Municipal Center for Disease Control and Prevention.
This project was funded by Fogarty NIH grant #5 D43 TW009077-03. For LPS, we also thank the Carolina Population Center for training support (T32 HD007168) and for general support (R24 HD050924). No funder had a role in the design, analysis, or writing of this article.
Footnotes
CONFLICTS OF INTEREST AND FUNDING DISCLOSURE
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Popkin BM. Will China’s Nutrition Transition Overwhelm Its Health Care System And Slow Economic Growth? Health Aff. 2008;4:1064–76. doi: 10.1377/hlthaff.27.4.1064. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Popkin BM. The nutrition transition and obesity in the developing world. J Nutr. 2001;3:871S–73S. doi: 10.1093/jn/131.3.871S. doi: [DOI] [PubMed] [Google Scholar]
- 3.Du S, Lu B, Zhai F, Popkin BM. A new stage of the nutrition transition in China. Public Health Nutrition. 2002;1A:169–74. doi: 10.1079/PHN2001290. doi: [DOI] [PubMed] [Google Scholar]
- 4.Astrup A, Dyerberg J, Selleck M, Stender S. Nutrition transition and its relationship to the development of obesity and related chronic diseases. Obesity Reviews. 2008;s1:48–52. doi: 10.1111/j.1467-789X.2007.00438.x. doi: [DOI] [PubMed] [Google Scholar]
- 5.Rivera JA, Barquera S, González Cossío T, Olaiz G, Sepulveda J. Nutrition transition in Mexico and in other Latin American countries. Nutr Rev. 2004:S149–S57. doi: 10.1111/j.1753-4887.2004.tb00086.x. doi: [DOI] [PubMed] [Google Scholar]
- 6.Popkin BM, Nielsen SJ. The sweetening of the world's diet. Obes Res. 2003;11:1325–32. doi: 10.1038/oby.2003.179. doi: 10.1038/oby.2003.179. [DOI] [PubMed] [Google Scholar]
- 7.Barquera S, Hernandez-Barrera L, Espinosa J, Wen N, Rivera J, Popkin B. Energy Intake from Beverages Is Increasing among Mexican Adolescents and Adults. J Nutr. 2008:2454–61. doi: 10.3945/jn.108.092163. doi: [DOI] [PubMed] [Google Scholar]
- 8.Pereira RA, Duffey KJ, Sichieri R, Popkin BM. Sources of excessive saturated fat, trans fat and sugar consumption in Brazil: an analysis of the first Brazilian nationwide individual dietary survey. Public Health Nutr. 2012:1–9. doi: 10.1017/S1368980012004892. doi: doi:10.1017/S1368980012004892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malik VS, Popkin BM, Bray GA, Després JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;11:1356–64. doi: 10.1161/CIRCULATIONAHA.109.876185. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Odegaard AO, Koh WP, Arakawa K, Mimi CY, Pereira MA. Soft Drink and Juice Consumption and Risk of Physician-diagnosed Incident Type 2 Diabetes The Singapore Chinese Health Study. Am J Epidemiol. 2010;6:701–08. doi: 10.1093/aje/kwp452. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav. 2010;1:47. doi: 10.1016/j.physbeh.2010.01.036. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Euromonitor International Soft Drinks in China Country Report. 2012.
- 13.Kleiman S, Ng SW, Popkin B. Drinking to our health: can beverage companies cut calories while maintaining profits? Obesity Reviews. 2011 doi: 10.1111/j.1467-789X.2011.00949.x. no-no. doi: 10.1111/j.1467-789X.2011.00949.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adair LS, Popkin BM. Are child eating patterns being transformed globally? Obes Res. 2012;7:1281–99. doi: 10.1038/oby.2005.153. doi: [DOI] [PubMed] [Google Scholar]
- 15.Rutishauser IH. Dietary intake measurements. Public Health Nutrition. 2005;7A:1100. doi: 10.1079/phn2005798. doi: [DOI] [PubMed] [Google Scholar]
- 16.Chambers E, IV, Godwin SL, Vecchio FA. Cognitive strategies for reporting portion sizes using dietary recall procedures. Journal of the American Dietetic Association. 2000;8:891–97. doi: 10.1016/s0002-8223(00)00259-5. doi: [DOI] [PubMed] [Google Scholar]
- 17.Cypel YS, Guenther PM, Petot GJ. Validity of portion-size measurement aids: a review. J Am Diet Assoc. 1997;3:289–92. doi: 10.1016/S0002-8223(97)00074-6. doi: [DOI] [PubMed] [Google Scholar]
- 18.Subar AF, Kipnis V, Troiano RP, Midthune D, Schoeller DA, Bingham S, et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. American Journal of Epidemiology. 2003;1:1–13. doi: 10.1093/aje/kwg092. doi: [DOI] [PubMed] [Google Scholar]
- 19.Ferrari P, Slimani N, Ciampi A, Trichopoulou A, Naska A, Lauria C, et al. Evaluation of under-and overreporting of energy intake in the 24-hour diet recalls in the European Prospective Investigation into Cancer and Nutrition (EPIC) Public health nutrition. 2002;6b:1329–45. doi: 10.1079/PHN2002409. doi: [DOI] [PubMed] [Google Scholar]
- 20.Bingham S, Cassidy A, Cole T, Welch A, Runswick S, Black A, et al. Validation of weighed records and other methods of dietary assessment using the 24 h urine nitrogen technique and other biological markers. Br J Nutr. 1995;04:531–50. doi: 10.1079/bjn19950057. doi: [DOI] [PubMed] [Google Scholar]
- 21.Poslusna K, Ruprich J, de Vries JH, Jakubikova M, van't Veer P. Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr. 2009;S2:S73–S85. doi: 10.1017/S0007114509990602. doi: [DOI] [PubMed] [Google Scholar]
- 22.Tooze JA, Subar AF, Thompson FE, Troiano R, Schatzkin A, Kipnis V. Psychosocial predictors of energy underreporting in a large doubly labeled water study. Am J Clin Nutr. 2004;5:795–804. doi: 10.1093/ajcn/79.5.795. doi: [DOI] [PubMed] [Google Scholar]
- 23.Winter J, Boushey C. Workshop 1: use of technology in dietary assessment. Eur J Clin Nutr. 2009:S75–S77. doi: 10.1038/ejcn.2008.69. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matthiessen TB, Steinberg FM, Kaiser LL. Convergent validity of a digital image-based food record to assess food group intake in youth. J Am Diet Assoc. 2011;5:756–61. doi: 10.1016/j.jada.2011.02.004. doi: [DOI] [PubMed] [Google Scholar]
- 25.Rollo ME, Ash S, Lyons-Wall P, Russell A. Trial of a mobile phone method for recording dietary intake in adults with type 2 diabetes: evaluation and implications for future applications. J Telemed Telecare. 2011;6:318–23. doi: 10.1258/jtt.2011.100906. doi: [DOI] [PubMed] [Google Scholar]
- 26.Lazarte CE, Encinas ME, Alegre C, Granfeldt Y. Validation of digital photographs, as a tool in 24-h recall, for the improvement of dietary assessment among rural populations in developing countries. Nutrition Journal. 2012;1:61. doi: 10.1186/1475-2891-11-61. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martin CK, Correa JB, Han H, Allen HR, Rood JC, Champagne CM, Gunturk BK, Bray GA. Validity of the Remote Food Photography Method (RFPM) for Estimating Energy and Nutrient Intake in Near Real-Time. Obesity. 2011 doi: 10.1038/oby.2011.344. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavorial medicine. Ann Behav Med. 1994;3:199–202. doi: [Google Scholar]
- 29.Willett W. Nutritional Epidemiology. Oxford Scholarship Online; 2012. [Google Scholar]
- 30.Ma Y, Olendzki BC, Pagoto SL, Hurley TG, Magner RP, Ockene IS, Schneider KL, Merriam PA, Hebert JR. Number of 24-hour diet recalls needed to estimate energy intake. Ann Epidemiol. 2009;8:553–9. doi: 10.1016/j.annepidem.2009.04.010. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kirkpatrick SI, Midthune D, Dodd KW, Potischman N, Subar AF, Thompson FE. Reactivity and its association with body mass index across days on food checklists. Journal of the Academy of Nutrition and Dietetics. 2012;1:110–8. doi: 10.1016/j.jada.2011.10.004. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rebro SM, Patterson RE, Kristal AR, Cheney CL. The effect of keeping food records on eating patterns. J Am Diet Assoc. 1998;10:1163–5. doi: 10.1016/S0002-8223(98)00269-7. doi: [DOI] [PubMed] [Google Scholar]
- 33.Thompson FE, Subar AF. Dietary Assessment Methodology. Academic Press; San Diego, CA: 2008. [Google Scholar]
- 34.Goris AH, Meijer EP, Westerterp KR. Repeated measurement of habitual food intake increases under-reporting and induces selective under-reporting. Br J Nutr. 2001;5:629–34. doi: 10.1079/bjn2001322. doi: [DOI] [PubMed] [Google Scholar]
- 35.Novotny JA, Rumpler WV, Judd JT, Riddick PH, Rhodes D, McDowell M, Briefel R. Diet interviews of subject pairs: how different persons recall eating the same foods. J Am Diet Assoc. 2001;10:1189–93. doi: 10.1016/s0002-8223(01)00291-7. doi: [DOI] [PubMed] [Google Scholar]
- 36.Frankenfeld CL, Poudrier JK, Waters NM, Gillevet PM, Xu Y. Dietary Intake Measured from a Self-Administered, Online 24-Hour Recall System Compared with 4-Day Diet Records in an Adult US Population. Journal of the Academy of Nutrition and Dietetics. 2012 doi: 10.1016/j.jand.2012.06.003. doi: [DOI] [PubMed] [Google Scholar]
- 37.Posner BM, Martin-Munley SS, Smigelski C, Cupples LA, Cobb JL, Schaefer E, Miller DR, D'Agostino RB. Comparison of techniques for estimating nutrient intake: the Framingham Study. Epidemiology. 1992;2:171–77. doi: 10.1097/00001648-199203000-00016. doi: [DOI] [PubMed] [Google Scholar]
- 38.De Keyzer W, Huybrechts I, De Vriendt V, Vandevijvere S, Slimani N, Van Oyen H, De Henauw S. Repeated 24-hour recalls versus dietary records for estimating nutrient intakes in a national food consumption survey. Food Nutr Res. 2011;10:11. doi: 10.3402/fnr.v55i0.7307. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization Global Database on Body Mass Index:an interactive surveillance tool for monitoring nutrition transition. 2013.
- 40.Donaire-Gonzalez D, de Nazelle A, Seto E, Mendez M, Nieuwenhuijsen MJ, Jerrett M. Comparison of Physical Activity Measures Using Mobile Phone-Based CalFit and Actigraph. Journal of Medical Internet Research. 2013;6:e111. doi: 10.2196/jmir.2470. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Seto E, Martin E, Yang A, Yan P, Gravina R, Lin I, et al. Opportunistic strategies for lightweight signal processing for body sensor networks; Paper presented at: Proceedings of the 3rd International Conference on Pervasive Technologies Related to Assistive Environments.2010. [Google Scholar]
- 42.Seto EY, Giani A, Shia V, Wang C, Yan P, Yang AY, Jerrett M, Bajcsy R. A wireless body sensor network for the prevention and management of asthma; Paper presented at: Industrial Embedded Systems, 2009. SIES'09. IEEE International Symposium on2009. [Google Scholar]
- 43.Yang Y, Wang G, Pan X. China Food Composition 2002. Peking University Medical Press; Beijing: 2002. [Google Scholar]
- 44.U.S. Department of Agriculture ARS USDA National Nutrient Database for Standard Reference. Release 25 [cited; Available from: Nutrient Data Laboratory Home Page, http://www.ars.usda.gov/ba/bhnrc/ndl.
- 45.Willett W. Nutritional Epidemiology. Oxford University Press; Oxford, UK: 1998. [Google Scholar]
- 46.Perrier E, Rondeau P, Poupin M, Le Bellego L, Armstrong L, Lang F, et al. Relation between urinary hydration biomarkers and total fluid intake in healthy adults. Eur J Clin Nutr. 2013 doi: 10.1038/ejcn.2013.93. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Perrier E, Vergne S, Klein A, Poupin M, Rondeau P, Le Bellego L, et al. Hydration biomarkers in free-living adults with different levels of habitual fluid consumption. Br J Nutr. 2013;9:1678–87. doi: 10.1017/S0007114512003601. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Armstrong LE, Johnson EC, Munoz CX, Swokla B, Le Bellego L, Jimenez L, Casa DJ, Maresh CM. Hydration biomarkers and dietary fluid consumption of women. Journal of the Academy of Nutrition and Dietetics. 2012;7:1056–61. doi: 10.1016/j.jand.2012.03.036. doi: [DOI] [PubMed] [Google Scholar]
- 49.Armstrong LE. Hydration assessment techniques. Nutr Rev. 2005;6:S40–54. doi: 10.1111/j.1753-4887.2005.tb00153.x. Pt 2. doi: [DOI] [PubMed] [Google Scholar]
- 50.Meinders A, Meinders A. [How much water do we really need to drink?] [Article in Dutch] Ned Tijdschr Geneeskd. 2010;154:A1757. doi: [PubMed] [Google Scholar]
- 51.Hedrick VE, Comber DL, Estabrooks PA, Savla J, Davy BM. The beverage intake questionnaire: determining initial validity and reliability. J Am Diet Assoc. 2010;8:1227–32. doi: 10.1016/j.jada.2010.05.005. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alaimo K, Olson CM, Frongillo EA. Importance of cognitive testing for survey items: an example from food security questionnaires. Journal of Nutrition Education. 1999;5:269–75. doi: [Google Scholar]
- 53.Williamson DA, Allen HR, Martin PD, Alfonso AJ, Gerald B, Hunt A. Comparison of digital photography to weighed and visual estimation of portion sizes. J Am Diet Assoc. 2003;9:1139–45. doi: 10.1016/s0002-8223(03)00974-x. doi: [DOI] [PubMed] [Google Scholar]
- 54.Ovaskainen M, Paturi M, Reinivuo H, Hannila M, Sinkko H, Lehtisalo J, Pynnönen-Polari O, Männistö S. Accuracy in the estimation of food servings against the portions in food photographs. Eur J Clin Nutr. 2007;5:674–81. doi: 10.1038/sj.ejcn.1602758. doi: [DOI] [PubMed] [Google Scholar]
- 55.Nelson M, Atkinson M, Darbyshire S. Food photography I: the perception of food portion size from photographs. Br J Nutr. 1994;5:649–64. doi: 10.1079/bjn19940069. doi: [DOI] [PubMed] [Google Scholar]
- 56.Kikunaga S, Tin T, Ishibashi G, Wang D-H, Kira S. The application of a handheld personal digital assistant with camera and mobile phone card (Wellnavi) to the general population in a dietary survey. J Nutr Sci Vitaminol (Tokyo) 2007;2:109–16. doi: 10.3177/jnsv.53.109. doi: [DOI] [PubMed] [Google Scholar]
- 57.Mendez MA, Wynter S, Wilks R, Forrester T. Under-and overreporting of energy is related to obesity, lifestyle factors and food group intakes in Jamaican adults. Public Health Nutrition. 2004;1:9–20. doi: 10.1079/phn2003508. doi: [DOI] [PubMed] [Google Scholar]
- 58.Lissner L. Measuring food intake in studies of obesity. Public Health Nutrition. 2002;6a:889–92. doi: 10.1079/phn2002388. doi: [DOI] [PubMed] [Google Scholar]
- 59.Guenther PM, Kott PS, Carriquiry AL. Development of an approach for estimating usual nutrient intake distributions at the population level. J Nutr. 1997;6:1106–12. doi: 10.1093/jn/127.6.1106. doi: [DOI] [PubMed] [Google Scholar]
- 60.Carriquiry AL. Estimation of usual intake distributions of nutrients and foods. J Nutr. 2003;2:601S–08S. doi: 10.1093/jn/133.2.601S. doi: [DOI] [PubMed] [Google Scholar]
- 61.Harttig U, Haubrock J, Knüppel S, Boeing H. The MSM program: web-based statistics package for estimating usual dietary intake using the Multiple Source Method. Eur J Clin Nutr. 2011:S87–S91. doi: 10.1038/ejcn.2011.92. doi: [DOI] [PubMed] [Google Scholar]
- 62.Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith SM, Subar AF, Dodd KW. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: The NCI method. Stat Med. 2010;27:2857–68. doi: 10.1002/sim.4063. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.