Abstract
Rift valley fever (RVF) is a mosquito-borne disease of domestic and wild ruminants caused by RVF virus (RVFV), a phlebovirus (Bunyaviridae). RVF is widespread in Sub-Saharan Africa. In September of 2010, an RVF outbreak occurred in northern Mauritania involving mass abortions in small ruminants and camels (Camelus dromedarius) and at least 63 human clinical cases, including 13 deaths. In camels, serological prevalence was 27.5–38.5% (95% confidence interval, n=279). For the first time, clinical signs other than abortions were reported in this species, including hemorrhagic septicemia and severe respiratory distress in animals. We assessed the presence of RVFV in camel sera sampled during this outbreak and generated whole-genome sequences of RVFV to determine the possible origin of this RVFV strain. Phylogenetic analyses suggested a shared ancestor between the Mauritania 2010 strain and strains from Zimbabwe (2269, 763, and 2373), Kenya (155_57 and 56IB8), South Africa (Kakamas, SA75 and SA51VanWyck), Uganda (Entebbe), and other strains linked to the 1987 outbreak of RVF in Mauritania (OS1, OS3, OS8, and OS9).
Key Words: : Rift Valley fever virus, Camelus dromedarius, Mauritania, Phylogenetic analysis
Introduction
Rift valley fever (RVF) is an acute disease of domestic and wild ruminants caused by RVF virus (RVFV), a mosquito-borne virus of the Bunyaviridae family and the genus Phlebovirus. Like other members of the genus Phlebovirus, RVFV has a negative-sense single-stranded RNA genome comprising L (large), M (medium), and S (small) segments. The L segment encodes the viral RNA polymerase, whereas the M segment encodes two major envelope surface glycoproteins, Gc and Gn, the 14-kDa NSm nonstructural protein, and a 78-kDa fusion protein. The S segment encodes for the nonstructural protein and the nucleocapsid (Schmaljohn 1996).
RVF is widespread in Sub-Saharan Africa and has expanded its geographic range to Egypt (including the River Nile Delta), the Arabian Peninsula, the Comoros archipelago, and Madagascar (Bird et al. 2009, Cêtre-Sossah et al. 2012). It causes mass abortions and neonatal mortality in ruminants. Humans become infected mainly by direct contact with infected animals (tissues, aerosols) or by the bites of infected mosquitoes.
In western Africa, suspicions of RVF were reported in the early 1930s and considered as an endemic infection (Curasson 1934). Serological surveys demonstrated RVFV circulation in western Africa between 1981 and 1985, particularly in southern Mauritania, with a prevalence of 18% in the ruminants and 13% in ruminant farmers (Saluzzo et al. 1987). In autumn of 1987, a major RVF epizootic was observed in ruminants of the Senegal River Valley, followed by human outbreaks (Digoutte et al. 1989). Subsequent RVF epizootics associated with human cases occurred in 1993, 1998, and 2003 (Soumaré et al. 2012). Favorable environmental conditions, mainly rainfall, are the key factors causing unusual viral emergence of mosquito vectors, leading to a larger number of infected domestic animals being considered as amplifying hosts.
In September, 2010, an RVF outbreak occurred in northern Mauritania following unusually high rainfall in this desertic area. Mass abortions were observed in small ruminants and camels (Camelus dromedarius), and there were at least 63 human clinical cases, including 13 deaths (Faye et al. 2014). In camels, serological prevalence was 27.5–38.5% (95% confidence interval [CI], n=279). For the first time, clinical signs other than abortions were reported in this species, including hemorrhagic septicemia and severe respiratory distress in animals (El Mamy et al. 2011). We assessed the presence of RVFV in camel sera sampled during this outbreak, and generated whole-genome sequences of RVFV to determine the possible origin of this RVFV. Rainfall conditions associated with this outbreak are presented and discussed.
Materials and Methods
On October 6, 2010, serum samples collected from 14 sick camels and 21 sick goats were transferred to the Senegalese National Laboratory of Livestock and Veterinary Research (ISRA/LNERV, Dakar). Viral isolation was attempted on samples that tested positive by nested RT-PCR (Sall et al. 2001). Briefly, RVFV isolates were obtained with a single passage on Vero cells from the serum of four camels, two originating from Lemsayddi (13.38556W, 19.84030N) and two from Agjatt (13.00370W, 20.63496N) (Fig. 1A). The animal serum (100 μL) was mixed with 200,000 Vero cells maintained in Dulbecco Minimum Essential Medium (D-MEM; Life Technologies, France) supplemented with 5% fetal bovine serum (FBS), 1000 U/mL penicillin, 1 mg/mL streptomycin, and 1 mM l-glutamine, in a six-well-format plate at 37°C, 5% CO2. After 72 h of incubation at 37°C, 5% CO2, cell supernatants were harvested when 80% of cytopathogenic effect (CPE) was observed, centrifuged for 3 min at 1500×g to remove cell debris, and finally stored at −80°C. Viral RNA was extracted from infected cell supernatants using the RNeasy Mini Kit (Qiagen, USA) according to the manufacturer's instructions. Reverse transcription and amplification were performed using SuperScript III/Platinum Taq High Fidelity (Invitrogen, San Diego, CA) with primers targeting the complete S and M segments (Cêtre-Sossah et al. 2012), leading to the generation of whole-segment sequences (Beckman Genomics, France).
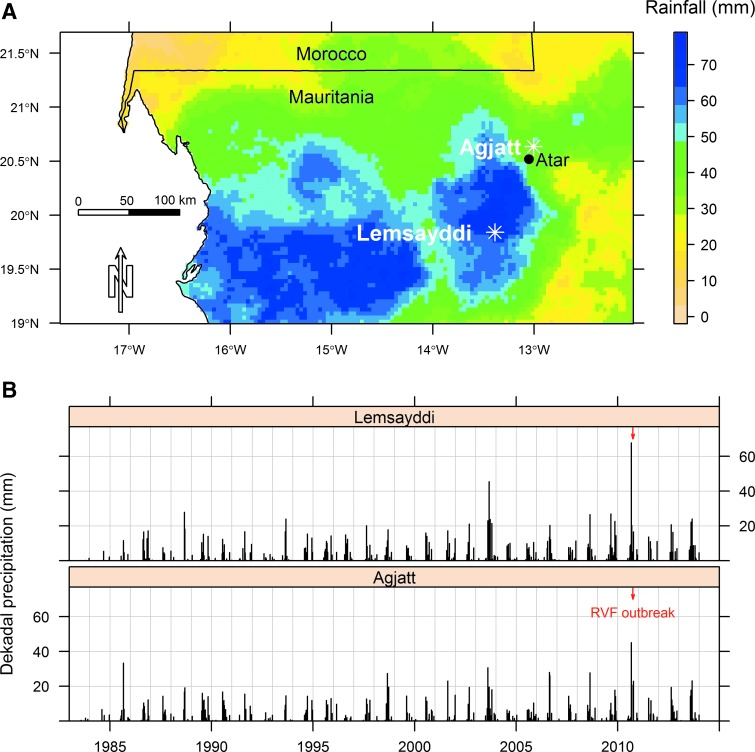
FIG. 1.
(A) Location of Rift Valley fever (RVF) cases in camels with respect to cumulative precipitations in September of 2010. Data source for precipitation: Tropical Applications of Meteorology using SATellite data and ground-based observations (TAMSAT; (www.met.reading.ac.uk/tamsat). (B) Time series for dekadal precipitations in Agjatt and Lemsayddi, Mauritania, from 1983 to 2014. The time for the 2010 RVF outbreak is indicated with a red arrow. Data source for precipitation: Tropical applications of meteorology using satellite data and ground-based observations (TAMSAT). Color images available online at www.liebertpub.com/vbz
To compare the genetic relatedness of the isolated viruses, phylogenetic analyses were performed against a panel of 50 published RVFV sequences. Before phylogenetic inference, datasets and multiple sequence alignments were examined thoroughly to eliminate misalignments and ensure correct framing of coding sequences. Sequences were aligned by ClustalW, edited using MEGA software version 5, and concatenated. GenBank accession numbers for the 25010-24 Mauritania 2010 isolate segments S and M are, respectively, KM210508 and KM210509. Putative recombination events in sequence alignments were assessed using RDP4 (Heath et al. 2006). Recombinant sequences were discarded.
Phylogenetic reconstructions were carried out by the maximum likelihood (ML) method implemented in the Treefinder (March, 2011) software package, as previously described (Cêtre-Sossah et al. 2012). The 100% nucleotide identity observed for the four isolates led us to choose the isolate 25010-24 for further phylogenetic analysis. Because RVF is a mosquito-borne disease, its occurrence is closely related to mosquito density and therefore surface water (Linthicum et al. 1999). In this desertic area of Mauritania, without any lake or river, surface water is mainly related to rainfall. The 1983–2014 time series of precipitation data for Africa provided by the TAMSAT Research Group (Tropical Applications of Meteorology using SATellite data and ground-based observations) hosted by the University of Reading, United Kingdom (Grimes et al. 1999) was used to obtain the rainfall pattern of northern Mauritania. This dataset has a dekadal time resolution, and a 0.0375-degree spatial resolution. A buffer with a 10-km radius around the reported locations of RVF outbreaks was drawn. The mean precipitation for each dekade and location between the beginning of July and the end of November was computed.
Results and Discussion
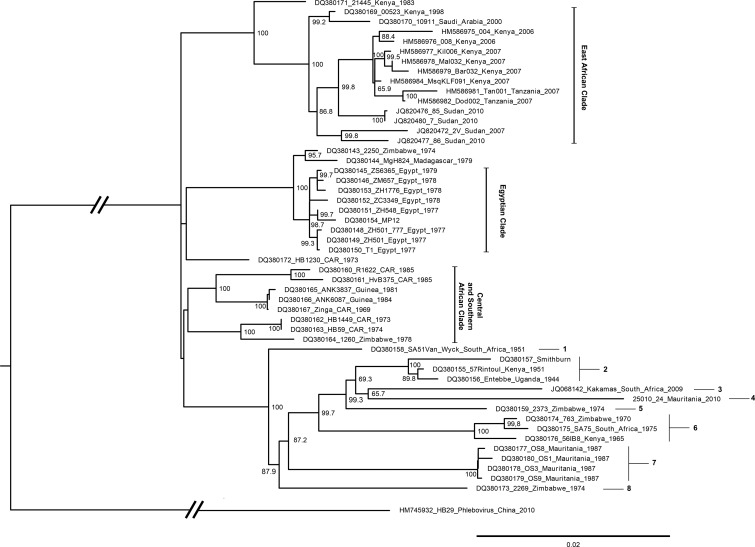
Maximum likelihood phylogenetic analyses suggested a shared ancestor between the 25010_24 Mauritania 2010 strain and strains from Zimbabwe (2269, 763 and 2373), Kenya (155_57 and 56IB8), South Africa (Kakamas, SA75 and SA51VanWyck), and Uganda (Entebbe), and other strains linked to the 1987 outbreak of RVF in Mauritania (OS1, OS3, OS8, and OS9) (Fig. 2). Specific amino acid signatures on the full small and medium segments indicated in the Table 1 show that the Mauritania 2010 strain is most closely related to the four strains of Mauritania 1987 and the 2269_Zimbabwe 1974 (eight mutations) and the Van Wyck_South Africa 1951 and Kakamas_South Africa 2009 strains (nine mutations), which is not in complete accordance with what was described in the phylogenetic trees based on human isolates (Faye et al. 2014).
FIG. 2.
Phylogenetic tree based on the concatenated small (S) and medium (M) segments of Rift Valley fever virus (RVFV) relationships. The neighbor-joining method was used for phylogenetic analysis; evolutionary distances were computed by using the Tamura 3-parameter method and a gamma distribution parameter with a value of 5. GenBank accession numbers for the Mauritania 2010 segment S and M are, respectively, KM210508 and KM210509. Scale bar indicates nucleotide substitutions per site. CAR, Central African Republic.
Table 1.
Specific Molecular Signatures on the Complete Rift Valley Fever S and M Concatenated Segments
| Haplotype | Associated strains | Positions | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Position on concatenated S and M sequence | 271 | 313 | 334 | 355 | 356 | 422 | 430 | 453 | 485 | 535 | 824 | 828 | 833 | 851 | 885 | 935 | 995 | 1051 | 1058 | 1102 | 1306 | 1316 | |
| Position on segment S sequence | 271 | 313 | 334 | 355 | 356 | 422 | 430 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | — | |
| Position on segment M sequence | — | — | — | — | — | — | — | 9 | 41 | 91 | 380 | 384 | 389 | 407 | 441 | 491 | 551 | 607 | 614 | 658 | 862 | 872 | |
| Consensus residue | P | I | I | R | N | Q | N | S | G | H | Y | M | T | H | I | V | I | K | R | V | I | I | |
| (% consensus among the 50 aligned sequences) | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 98% | 100% | 100% | 96% | 100% | 100% | 100% | 94% | 58% | 100% | 92% | |
| 1 | DQ380158_VanWyck_South Africa_1951 | — | — | — | — | — | — | — | — | — | — | — | — | — | R | — | — | — | — | — | A | V | — |
| 2 | DQ380156_Entebbe_Uganda_1944 | — | — | — | — | — | — | — | — | — | — | — | — | I | — | — | — | — | — | — | — | — | V |
| DQ380155_Rintoul_Kenya_1951 | — | — | — | — | — | — | — | — | — | — | — | — | I | — | — | — | — | — | — | — | — | V | |
| DQ380157_ Smithburn | — | — | — | — | — | — | — | — | — | — | — | — | I | — | — | — | — | — | — | — | — | V | |
| 3 | JQ068142_South Africa_2009 | — | — | — | — | — | — | — | — | — | — | — | I | — | — | — | — | — | R | K | A | — | — |
| 4 | 25010_24_Mauritania_2010 | — | V | V | — | — | — | — | — | R | — | — | — | — | — | — | I | — | — | K | A | — | — |
| 5 | DQ380159_2373_Zimbabwe_1974 | S | — | — | K | — | — | S | — | — | Y | — | — | — | — | — | — | M | — | — | A | — | L |
| 6 | DQ380176_56IB8_Kenya_1965 | — | — | — | — | S | — | — | T | — | — | — | — | — | — | — | — | — | — | — | A | — | — |
| DQ380175_SA75_1975 | — | — | — | — | S | — | — | T | — | — | — | — | — | — | — | — | — | — | — | A | — | — | |
| DQ380175_763_Zimbabwe_1970 | — | — | — | — | S | — | — | T | — | — | — | — | — | — | — | — | — | — | — | A | — | — | |
| 7 | DQ380177_OS08_Mauritania_1987 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | V | — | — | — | — | A | — | — |
| DQ380178_OS03_Mauritania_1987 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | V | — | — | — | — | A | — | — | |
| DQ380179_OS09_Mauritania_1987 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | V | — | — | — | — | A | — | — | |
| DQ380180_OS01_Mauritania_1987 | — | — | — | — | — | — | — | — | — | — | — | — | — | — | V | — | — | — | — | A | — | — | |
| 8 | DQ380173_2269_Zimbabwe_1974 | — | — | — | — | — | R | — | — | — | — | H | — | — | — | — | — | — | — | K | A | — | — |
The amplification of the viral load for each of the isolates through one single Vero cell passage has to be strengthened, leading to a limited effect on potential genetic changes that could occur via these amplification methods. Until the 2010 outbreak, the risk of RVF occurrence in the northern part of Mauritania was considered negligible, because of unfavorable meteorological conditions for grasslands and surface water, which are prerequisites for the vectors and the domestic ruminants. However, heavy rainfall was observed in early September of 2010 in the region of Atar (Fig. 1A). In the resulting abundance of grasslands and surface waters, there was an increase in animal movements (camels and small ruminants) from the Senegal River Valley to northern Mauritania, because farmers brought their animals to benefit from these resources.
The retrospective study of dekadal precipitations in this area (Fig. 1B) revealed the heavy rainfall observed in Agjatt (45 mm) and Lemsayddi (68 mm) during the first dekade of September, 2010, which was the heaviest rainfall recorded in a long time in these two locations between 1983 and 2014. Investigations led the farmers to report the density of mosquitoes following this heavy rainfall. There is no doubt that this mosquito proliferation triggered RVFV transmission. However, the time when RVFV was introduced is questionable. Indeed, the outbreaks occurred in distinct places (ca. 100 km away from each other) shortly after the rainfall (Fig. 1B). Two explanations are possible: (1) RVFV was introduced after the rainfall with recently infected animals that traveled via trucks from the Senegal River Valley, or (2) the outbreaks were the result of the increase of a low activity of the virus. Indeed, vertical transmission of RVFV has been described for some Aedes mosquito species that are well adapted to arid conditions; desiccated eggs are known to survive for years in dried mud of temporary ponds (Romoser et al. 2011). Further work is needed to assess these two hypotheses. Indeed, RVFV cases are sometimes reported in Mauritanian oases and other arid areas without any clear explanation of the epidemiologic pattern (Diallo et al. 2005).
Camels are known to be susceptible to RVFV infection (El Mamy et al. 2011). The virus has been isolated from apparently healthy camels (Imam et al. 1979) , but their epidemiological role is uncertain. High seroprevalence has been reported in camels on several occasions: 22% and 57% in Kenya and 1978 and 2006 outbreaks, respectively (Davies et al. 1985, Britch et al. 2013), and 15% in Morocco from camels imported from Mauritania after the 2010 RVF outbreak (El Harrak et al. 2011). Our study provided evidence that clinical disease in camels coincided with RVFV viremia during the 2010 outbreak in Mauritania. These sick animals were probably infected by mosquitoes taking their blood meals and were thus a probable source of infection for human handlers. Intensive human and animal movements between western African countries have predominated for centuries in combination with high vector density. The RVFV surveillance improvement via less than 1-year-old sentinel herds and entomological studies looking at vector diversity and abundance linked to climatic conditions analysis is crucial to better anticipate the risk of a new outbreaks, prevent the disease to spread, and strengthen control measures. Group discussions with remote rural human populations (breeders and butchers) and society officials before the occurrence of new outbreaks will favor the socio-ecological context, making it easier to handle the disease if it occurs.
Acknowledgments
We thank the National Centre of Livestock and Veterinary Research, Nouakchott, and the Mauritanian surveillance network for animal diseases for their support as well as the farmers.
This study was partially funded by CIRAD grant ATP Emergence and EU grant FP7 613996 Vmerge (www.vmerge.eu). The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the views of the European Commission. E.M.A.B. received a scholarship granted by the French Embassy in Nouakchott (Service de Coopération et d'Action Culturelle).
Author Disclosure Statement
No competing financial interests exist.
References
- Bird BH, Ksiazek TG, Nichol ST, Maclachlan NJ. Rift Valley fever virus. J Am Vet Med Assoc 2009; 234:883–893 [DOI] [PubMed] [Google Scholar]
- Britch SC, Binepal YS, Ruder MG, Kariithi HM, et al. Rift Valley fever risk map model and seroprevalence in selected wild ungulates and camels from Kenya. PLoS One 2013; 8:e66626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cêtre-Sossah C, Zeller H, Grandadam M, Caro V, et al. Genome analysis of Rift Valley Fever Virus, Mayotte. Emerg Infect Dis 2012; 18:969–972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curasson G. La fièvre de la Vallée du Rift existe-elle au Soudan français ? [Does Rift Valley fever exist in French Sudan?]. Bull Soc Pathol Exot, 1934; 27:599–602 [Google Scholar]
- Davies FG, Koros J, Mbugua H. Rift Valley fever in Kenya: The presence of antibody to the virus in camels (Camelus dromedarius). J Hyg (Lond) 1985; 94:241–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diallo M, Nabeth P, Ba K, Sall AA, et al. Mosquito vectors of the 1998–1999 outbreak of Rift Valley fever and other arboviruses (Bagaza, Sanar, Wesselsbron and West Nile) in Mauritania and Senegal. Med Vet Entomol 2005; 19:119–126 [DOI] [PubMed] [Google Scholar]
- Digoutte JP, Peters CJ. General aspects of the 1987 Rift Valley fever epidemic in Mauritania. Res Virol 1989; 140:27–30 [DOI] [PubMed] [Google Scholar]
- El-Harrak M, Martín-Folgar R, Llorente F, Fernández-Pacheco P, et al. Rift Valley and West Nile virus antibodies in camels, North Africa. Emerg Infect Dis 2011; 17:2372–2374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Mamy AB, Baba MO, Barry Y, Isselmou K, et al. Unexpected Rift Valley fever outbreak, northern Mauritania. Emerg Infect Dis 2011; 17:1894–1896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faye O, Ba H, Ba Y, Freire CC, et al. Reemergence of Rift Valley fever, Mauritania, 2010. Emerg Infect Dis 2014; 20:300–303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimes D, Pardo-Iguzquiza E, Bonifacio R. Optimal areal rainfall estimation using raingauges and satellite data. J Hydrol 1999, 222:93–108 [Google Scholar]
- Heath L, van der Walt E, Varsani A, Martin DP. Recombination patterns in aphthoviruses mirror those found in other picornaviruses. J Virol 2006; 80:11827–11832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linthicum KJ, Anyamba A, Tucker CJ, Kelley PW, et al. Climate and satellite indicators to forecast Rift Valley fever epidemics in Kenya. Science 1999; 285:397–400 [DOI] [PubMed] [Google Scholar]
- Romoser W, Oviedo M, Lerdthusnee K, Patrican L, et al. Rift Valley fever virus-infected mosquito ova and associated pathology: Possible implications for endemic maintenance. J Res Rep Trop Med 2011; 2:121–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sall AA, Thonnon J, Sene OK, et al. Single-tube and nested reverse transcriptase-polymerase chain reaction for detection of Rift Valley fever virus in human and animal sera. J Virol Methods. 2001; 91:85–92 [DOI] [PubMed] [Google Scholar]
- Saluzzo JF, Digoutte JP, Chartier C, Martinez D, et al. Focus of Rift Valley fever virus transmission in southern Mauritania. Lancet 1987; 1:504. [DOI] [PubMed] [Google Scholar]
- Schmaljohn CS, Bunyaviridae: The viruses and their replication. In: Fields BN, Knipe DM, Howley PM, Chanock RM, et al.Fields Virology, 3rd ed. Philadelphia: Lippincott-Raven Publishers, 1996:1447–1471 [Google Scholar]
- Soumaré POL, Freire CCM, Faye O, Diallo M, et al. Phylogeography of Rift Valley fever virus in Africa reveals multiple introductions in Senegal and Mauritania. PLoS One 2012; 7:e35216. [DOI] [PMC free article] [PubMed] [Google Scholar]