Abstract
Objective: The aim of the study was to verify the effects of patient factors perceived by emergency medical technicians (EMTs) as well as their social and organizational factors on prehospital telemetry use intention based on the technology use intention and elaboration likelihood models. Materials and Methods: This is a retrospective empirical study. Questionnaires were developed on the basis of clinical factors of 72,907 patients assessed by prehospital telemetry from January 1, 2009 to April 30, 2012 by reviewing their prehospital medical care records and in-hospital medical records. Questionnaires regarding the social and organizational factors of EMTs were created on the basis of a literature review. To verify which factors affect the utilization of telemetry, we developed a partial least-squares route model on the basis of each characteristic. In total, 136 EMTs who had experience in using prehospital telemetry were surveyed from April 1 to April 7, 2013. Reliability, validity, hypotheses, and the model goodness of fit of the study tools were tested. Results: The clinical factors of the patients (path coefficient=−0.12; t=2.38), subjective norm (path coefficient=0.18; t=2.63), and job fit (path coefficient=0.45; t=5.29) positively affected the perceived usefulness (p<0.010). Meanwhile, the clinical factors of the patients (path coefficients=−0.19; t=4.46), subjective norm (path coefficient=0.08; t=1.97), loyalty incentives (path coefficient=−0.17; t=3.83), job fit (path coefficient=−0.32; t=7.06), organizational facilitations (path coefficient=0.08; t=1.99), and technical factors (i.e., usefulness and ease of use) positively affected attitudes (path coefficient=0.10, 0.58; t=2.62, 5.81; p<0.010). Attitudes and perceived usefulness significantly positively affected use intention. Conclusions: Factors that influence the use of telemetry by EMTs in ambulances included patients' clinical factors, as well as complex organizational and environmental factors surrounding the EMTs' occupational environments. This suggests that the rapid use intention and dissemination of such systems require EMTs to be supported at both the technical and organizational levels.
Key words: : acceptance of healthcare, emergency medical technician, telemetry, telemedicine
Introduction
A real-time telemetry system (RTS) is an effective technology that enables emergency medical technicians (EMTs) to provide evidence-centered on-site prehospital care by objectively measuring patient information such as blood pressure, oxygen saturation, and electrocardiogram (ECG); this information is subsequently transferred to doctors upon arriving at the hospital.1,2 Despite advantages such as providing evidence-centered prehospital care, the utilization rate of this technology in Republic of Korea is only 6.7%.1 To accept this new technology, a variety of associated factors should be taken into consideration.3–6 As an RTS is used for patients at the scene of an emergency, its successful introduction requires consideration of the individual characteristics4,7 of both the patient and the environment.
Unlike the scene of an emergency, the regular clinical setting affords the technology that is used in a stable environment, reducing the relevance of complex effects second to unique environmental characteristics. However, an RTS is intended to be used at the scene of an emergency, and therefore environmental factors should be considered.5,8–10 In other words, individual variations in the responder's skills and education with respect to the responsibility for emergency response, social influences such as the recommendations of peers or superiors, and organizational characteristics such as the level of educational and administrative support may also affect the use of telemetry. However, not only is there little research concerning which factors EMTs consider important for the use of new technology in the prehospital setting, but also there is no systemic management of the promotion and maintenance of such use.
The technology acceptance model (TAM) is used in order to elucidate which major factors underlie the successful introduction of general medical technologies.3–8,11–14 Previous studies related to health information technology indicate that the influential factors for information technology use intention (UI) include individual factors, as well as social, organizational, and environmental factors.7,15–22 However, an RTS, unlike other technologies, presents a clear division between users and subjects. Because of this, an elaboration likelihood theory is required to explain the user (EMT) and subject (patient) factors involved in the use of RTS.
Therefore, in this research, we applied a TAM, an elaboration likelihood model (ELM), to analyze the effects of the EMT's social and organizational factors, as well as the patient factors recognized by the EMT, on the acceptance of RTS to help establish an effective plan for improving the administration of telemetry.
Materials and Methods
Literature Review
The TAM is the optimal simplest model based on the theory of reasoned action and focuses mainly on the possible impact of belief variables on the actual use of information technology. In TAM, external variables affect belief variables that go on to affect UI and, consequently, actual system use. Current research in the field of information technology considers UI, the belief variable perceived usefulness (PU), and perceived ease of use (PEOU).3,13 Previous research on technology acceptance has focused on user characteristics. In both the technology acceptance theory and rational behavior theory, the subjective norm (SN) has both direct and indirect impacts on the PU of a technology.4 Other research has shown that SN affects PU and acceptance.18 Expectation confirmation (EC), loyalty incentives (LI), and job fit (JF) had a positively effect on the PU and UI.19 Organizational facilitation (OF) prevents job-related stress and contributes to job satisfaction. Furthermore, the degree of facilitation positively affects the PEOU and the actual use of technology.12
Prehospital telemedicine differs from other clinical technologies in the strict separation between the user and the subject. Telemetry is a technology provided for the patient by the EMT, so both patient and EMT factors must be considered. Individual EMTs differ in their abilities to process work and intention. Existing TAMs only explain the impacts of user's individual factors on the successful implementation of a new technology and cannot account for the correlations relationships among patient (subject) and EMT (user) factors. The attitudes of EMTs toward using telemetry differ according to their abilities to process work and intention, and the ability to process work is determined, in turn, by the EMT's educational and professional qualifications.17 In previous analysis of the factors affecting the reception of RTS, patient mental status, which directly affects the reception, was considered as a central route factor, and transport time, which indirectly affects reception, was considered as a peripheral route factor; however, the choice of route depended on the qualifications of the EMT.7
This research developed a model incorporating technology acceptance theory, ELM in order to analyze the impact of patient factors and EMT-specific individual, social, and organizational factors on the use of RTS. The factors were defined as shown in Table 1, and we established the hypotheses shown in Table 2.
Table 1.
Operational Definition
| FACTORS | DEFINITION | REFERENCES |
|---|---|---|
| Patient factors | ||
| Clinical factors | Mental status (AVPU), GCS | Kim et al.,1Kim and Song,6 Gravel et al.16 |
| Nonclinical factors | Transport distance, transport time, EMT's qualifications | |
| Social factors | ||
| Subjective norm | Recognition of the expectations of the EMT's behaviors by others whose opinions critically influence them | Chen et al.,18Smucker and Creekmore20 |
| Expectation confirmation | Conformance between the EMT's expectations of and satisfaction with the technology | Bhattacherjee,19 Lin et al.21 |
| Organizational factors | ||
| Loyalty incentives | Material loyalty incentives for continued utilization | Bhattacherjee19 |
| Job fit | Increased efficacy of job performance because of repeated utilization | Bhattacherjee19 |
| Organizational facilitation | General support for technology management, education, and utilization | Bhattacherjee19 |
| Perceived usefulness | Degree of recognition that technology utilization is associated with improvements in the user's job performance | Davis et al.,3 Venkatesh and Davis13 |
| Perceived ease of use | Degree of perceived ease of technology utilization | |
| Attitude | The individual's feelings regarding the technology (e.g., positive/negative and in favor of/against) | Davis et al.,3 Venkatesh and Davis13 |
| Use intention | Influenced by attitudes and closely related to actual and predicted behavior | Davis et al.,3 Venkatesh and Davis13 |
AVPU, alert, (responsive to) voice, (responsive to) pain, unresponsive; EMT, emergency medical technician; GCS, Glasgow Coma Scale.
Table 2.
Hypotheses Proposed by This Study
| Hypothesis |
| 1-1. Clinical factors will have a positive effect on the PU. |
| 1-2. Clinical factors will have a positive effect on the ATT. |
| 1-3. Nonclinical factors will have a positive effect on the PU. |
| 1-4. Nonclinical factors will have a positive effect on the ATT. |
| 2-1. The EMT's SN will have a positive effect on the PU. |
| 2-2. The EMT's SN will have a positive effect on the ATT. |
| 2-3. The EMT's EC will have a positive effect on the PU. |
| 2-4. The EMT's EC will have a positive effect on the ATT. |
| 3-1. LI will have a positive effect on the PU. |
| 3-2. LI will have a positive effect on the ATT. |
| 3-3. The EMT's JF will have a positive effect on the PU. |
| 3-4. The EMT's JF will have a positive effect on the ATT. |
| 3-5. The EMT's OF will have a positive effect on the PU. |
| 3-6. The EMT's OF will have a positive effect on the ATT. |
| 4-1. The EMT's PEOU will have positive effects on the PU. |
| 4-2. The EMT's PEOU will have positive effects on the ATT. |
| 5-1. The EMT's PU will have positive effects on the ATT. |
| 5-2. The EMT's PU will have positively effects on the UI. |
| 6. The EMT's ATT will have positive effects on the UI. |
ATT, attitude; EC, expectation confirmation; EMT, emergency medical technician; JF, job fit; LI, loyalty incentives; OF, organizational facilitation, PEOU, perceived ease of use; PU, perceived usefulness; SN, subjective norm; UI, use intention.
Questionnaire Design and Survey Method
In this study, we designed integrated research models by combining retrospective and empirical studies. First, the prehospital medical records, telemetry, and in-hospital medical records of the patients who used RTS from January 1, 2009 to April 30, 2012 were examined retrospectively. The prehospital medical records were written by the EMTs, and telemetry data were measured by the telemetry system in the ambulance.1 The in-hospital medical records were written by doctors and nurses. A questionnaire was prepared by dividing the factors of the extracted patients into clinical factors (i.e., the central route) and nonclinical factors (i.e., the peripheral route) on the basis of the ELM.1,4,7,16
Second, a questionnaire to assess EMTs' social and organizational factors was developed through a literature review. A structural equating model was created on the basis of the produced questionnaire tools (Appendix).
Surveys were administered to EMTs who had experience with using RTS from April 1, 2012 to April 7, 2013. The questionnaire comprised a total of 60 topics and included demographic questions and EMT-identified patient factors as well as the EMT's social and organizational factors. For all responses except the demographic factors, a nominal Likert scale was used, with “Not at all” scored as 1 point and “Very true” as 7 points. The demographic profile included a total of seven questions, including questions related to the EMT's age, experience, and job qualifications, and the patient factors included four clinical factors and four nonclinical factors.1 The questions related to social factors included two concerning the SN and three concerning EC.18,19 The questions related to organizational factors included two concerning LI, six concerning JF, and four concerning OF.12,19 The survey also included three PU questions, three PEOU questions, two attitude (ATT) questions, and two intent to use questions.10 The collected demographic factors of respondents were analyzed by crosstabs (SPSS Windows version 18.0; SPSS Inc., Chicago, IL). We compared the differences between the usage group and the nonusage group for statistical significance. Categorical variables (i.e., sex, mental status, EMT grade, medical directions) were compared using the chi-squared test and continuous variables (i.e., age, Glasgow Coma Scale [GCS], transport time to hospital) were compared using a one-way analysis of variance test.
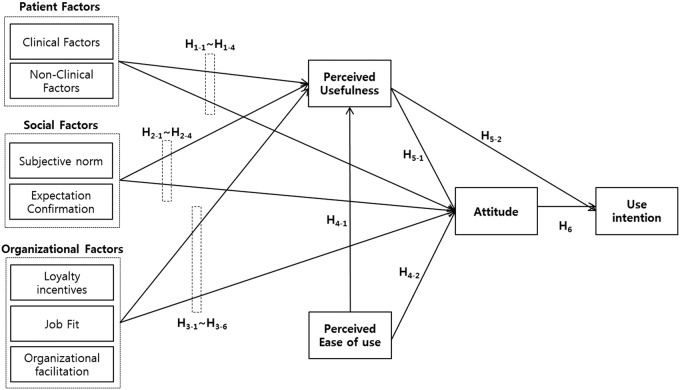
SmartPLS version 2.0 (SmartPLS Inc., Hamburg, Germany) was used to test the reliability, validity, hypotheses, and model goodness of fit of the research tools. The convergent and discriminant validity of the research tools were tested. Convergent validity was analyzed using the average extracted variance, common variance, factor loadings between each measurement item and relevant variables, and cross-factor loadings for other variables. Average variance extracted was used to analyze discriminant validity.23,24 To test the study hypotheses, the significances of path coefficients and t values were calculated using structural equations. The significance levels of t values were set to 2.58 (p<0.010) and 1.96 (p<0.050).24 In addition, the goodness of fit of the model was tested (Fig. 1).25
Fig. 1.
Research method. ANOVA, analysis of variance.
Results
Descriptive Statistics of Patients
In total, 72,907 patients were transported to a hospital via ambulance, and of these, 6,306 patients (8.6%) had EMTs who used the RTS in the Republic of Korea. The average age of patients who were transferred was 56 years. There was no significant difference in age and sex between the usage and nonusage groups. The mental status of the usage group was significantly lower than that of the nonusage group (p<0.010). Furthermore, there was a significant difference in RTS use by the level of the EMT (p<0.010). The average GCS score of the usage group was significantly lower than that of the nonusage group (p<0.010). The medical directions of the use group were significantly higher than those of the nonusage group (p<0.010) (Table 3).
Table 3.
Demographics of Patients (n=72,907)
| MEASURE, CATEGORIES | USAGE GROUP | NONUSAGE GROUP | P VALUE |
|---|---|---|---|
| Total patients (% total) | 6,306 (8.6) | 66,001 (91.4) | |
| Male:female ratio [n (%)] | 3,771 (59.8):2,535 (40.2) | 39,095 (58.7):27,506 (41.3) | 0.285 |
| Age (years) | 56 (21) | 57 (23) | 0.372 |
| Mental status [n (%)] | |||
| Alert | 788 (12.5) | 21,516 (32.6) | <0.001 |
| Verbal response | 460 (7.3) | 15,840 (24) | |
| Pain response | 2,604 (41.3) | 11,286 (17.1) | |
| Unresponsiveness | 2,453 (38.9) | 17,358 (26.3) | |
| GCS | 5 (4) | 8 (5) | <0.001 |
| EMT grade [n (%)] | |||
| Paramedic, nurse | 2,768 (43.9) | 16,698 (25.3) | <0.010 |
| Basic | 3,784 (50) | 40,195 (60.9) | |
| Firefighter (with first-aid certification) | 385 (6.1) | 9,174 (13.9) | |
| Transport time (min) | 9.1 (9.9) | 5.8 (4.9) | 0.331 |
| Medical directions for [n (%)] | |||
| Treatment | 2,333 (37.0) | 20,856 (31.6) | 0.211 |
| Ambulance diversion | 3,437 (55.5) | 15,444 (23.4) | <0.001 |
Data are mean (standard deviations) values unless indicated otherwise.
EMT, emergency medical technician; GCS, Glasgow Coma Scale.
Descriptive Statistics of Respondents
Out of the 136 respondents, there were more men (n=125, 91.9%) than women (n=11, 8.1%). Regarding education, graduates of a 4-year college course were predominant (n=50, 50%), and the mean duration of experience was 5.2±5.5 years. Regarding qualifications, EMT-basics were predominant (n=53, 39.0%) followed by EMT-paramedics (n=29, 21.3%). The mean number of times in using the RTS was 2.5±2.1 times per week, and the mean number of times of participation in telemetry education was 2.0±0.8 times annually (Table 4).
Table 4.
Demographics of Respondents (n=136)
| MEASURE, CATEGORIES | NUMBER | PERCENTAGE |
|---|---|---|
| Gender | ||
| Male | 125 | 91.9% |
| Female | 11 | 8.1% |
| Attainments in scholarship | ||
| High school | 26 | 19.1% |
| College | 42 | 30.9% |
| University | 50 | 50.0% |
| EMT grade | ||
| Paramedic | 29 | 21.3% |
| Nurse | 4 | 2.9% |
| Basic | 53 | 39.0% |
| Other | 50 | 36.8% |
| Experience (years) ina | ||
| Industry | 5.2±5.5 (3.5) | |
| Telemetry | 2.5±2.1 (1.5) | |
| Education | 2.0±0.8 (2) | |
Data are mean±standard deviation (median) values.
EMT, emergency medical technician.
Reliability and Validity Evaluation
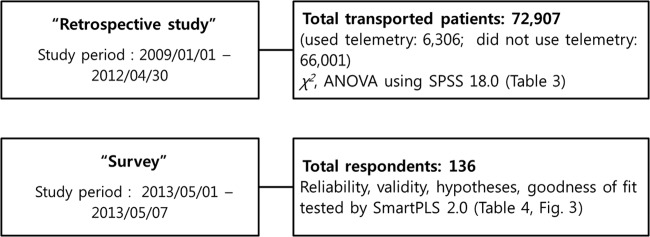
Convergent and discriminant validity were analyzed to determine the validity of the concepts regarding study variables. The average variance extracted and the common variance of each variable all exceeded 0.7, and factor loadings for the variables in each measurement item all exceeded 0.6; these results verify the convergent validity of the concepts. The squared average variance extracted values all exceeded 0.7; thus, the concepts have discriminant validity because these values exceeded the correlation coefficients of the other variables.23,24 The goodness-of-fit test of the model yielded a p value of 0.803, suggesting that the model fit the data well (>0.7).25
Hypotheses Testing
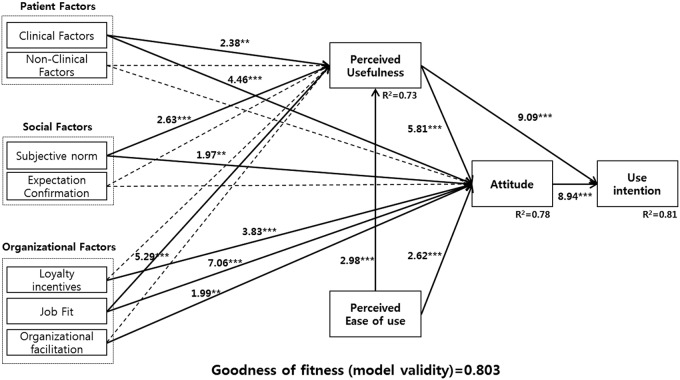
On the basis of the validity tests of the measurement items, the significances of the routes among all variables were analyzed with SmartPLS version 2.0 (Fig. 2). The routes between patients' clinical factors and PU (path coefficient=−0.12; t=2.38; p<0.050) as well as patients' clinical factors and ATT (path coefficient=−0.19; t=4.46; p<0.010) were significant, supporting both hypotheses 1-1 and 1-2. Significance was verified for SN and PU (path coefficient=0.18; t=2.63; p<0.010) as well as SN and ATT (path coefficient=0.08; t=1.97; p<0.050), supporting both hypotheses 2-1 and 2-2.
Fig. 2.
Hypothetical research framework.
Significance was verified for LI and ATT (path coefficient=−0.17; t=3.83; p<0.010), supporting hypothesis 3-2. Significance was verified for EMTs' JF and PU (path coefficient=0.45; t=5.29; p<0.010) as well as EMTs' JF and ATT (path coefficient=−0.32; t=7.06; p<0.010), supporting both hypotheses 3-3 and 3-4. Significance was verified for OF and ATT (path coefficient=0.08; t=1.99; p<0.050), supporting hypothesis 3-6. Significance was verified for PEOU and PU (path coefficient=0.18; t=2.98; p<0.010) as well as PEOU and ATT (path coefficient=0.10; t=2.62; p<0.010), supporting both hypotheses 4-1 and 4-2. Significance was verified for PU and ATT (path coefficient=0.58; t=5.81; p<0.010) as well as PU and UI (path coefficient=0.21; t=9.09; p<0.010), supporting hypotheses 5-1 and 5-2. Finally, significance was verified for ATT and UI (path coefficient=0.71; t=8.94; p<0.010), supporting hypothesis 6 (Fig. 3).
Fig. 3.
Research results. ***p<0.01, **p<0.05.
Discussion
This study was developed as a follow-up of the study of Kim et al.7 based on the TAM and extended ELM. Previous studies did not include the clinical characteristics of the patients; EMTs' social and organizational factors were added. We extracted relevant patient factors from their prehospital records, telemetry, and in-hospital medical records.17 EMTs' social and organizational factors included in the model were designed based on previous studies3–6 that have demonstrated the feasibility. Factors that influence the PU and ATT of telemetry by EMTs in ambulances included clinical factors, SN, and JF. Also, LI, JF, and OF all had a positive effect on the PU of telemetry. The UI was impacted by the PU and the ATT toward its use.
Therefore, successful implementation of RTS requires transformation of the ATT toward its use, and a plan considering the factors that might change the users' ATTs should be constructed. The severity of the patient has previously been shown to have a positive impact on the UI and the ATT toward its use for telemetry.5 The patient's clinical factors included the patient's mental status and GCS. The rate of use of prehospital telemedicine was associated with the severity of the patient's condition. Successful implementation of RTS will require both an accurate way to evaluate and a comprehensive way to manage the patient's mental status. Accurate evaluation of the patient will increase the frequency with which necessary emergency treatment is provided. Therefore, we need to enhance education about patient assessment. The SN had a positive effect on the PU and ATT of telemetry.18,20 EMTs exposed to various environments such as on-site emergency situations and hospitals are considered to be more strongly affected by SN than other variables. Therefore, it is important to focus on the social relationships for EMTs' SN. JF had a positive effect on the PU of telemetry and the ATT toward its use. A better JF was associated with greater UI.19 Telemetry measured the patient's vital signs and thus was effective for helping the EMT to prepare for the patient assessment that is used prehospital. Moreover, increasing the work productivity of RTS would be useful. For example, an EMT-paramedic often provides treatment with the system, so new telemetry functions such as an automatic blood pressure measuring device could increase productivity.
The clinical, social, and organizational factors that had a positive effect on the intent to use telemetry can be used to construct a management plan to promote telemetry use more successfully.
Limitations and Future Work
One limitation of the present study is that data for EMTs from only one region were analyzed; therefore, studies on EMTs from other regions need to be conducted in the future. In addition, we analyzed individual effects among the characteristics; therefore, it is necessary to conduct studies to verify the complex impacts of interactions between factors.
EMTs have relationships with a relatively wide variety of people, and they are more strongly influenced by SN than other professionals. Therefore, it is necessary for subjects who influence EMTs to show increased interest and trust toward them. Technological equipment capable of reducing work overload is required to increase JF and the usefulness of RTS; for example, an automated blood pressure measurement device can be used when only EMTs are dispatched to emergency sites. Moreover, recognition of the value of EMTs as well as physical, educational, and technological support for telemetry utilization needs to be provided simultaneously to improve OF.
This study verifies that patients' characteristics perceived by EMTs (i.e., prehospital) as well as EMTs' social and organizational characteristics (i.e., occupational and environmental factors) substantially affect the UI of RTS. In turn, this suggests that the successful implementation of telemetry requires simultaneous attention to on-site as well as occupational and environmental factors.
Appendix: Scales Used
1. Measure of patient's factors
• Clinical factors
○ The patient's mental status (alert, voice, pain, unresponsive [AVPU]) was alert.
○ The scale of the patient's eye opening response (Glasgow Coma Scale) was higher.
○ The scale of the patient's verbal response score (Glasgow Coma Scale) was higher.
○ The scale of the patient's motor response (Glasgow Coma Scale) was higher.
• Nonclinical factors
○ My role has its effects on the treatment of patients at the emergency scene.
○ My ability has its effects on the treatment of patients at the emergency scene.
○ The transport distance has its effects on the treatment of patients at the emergency scene.
○ The transport time has its effects on the treatment of patients at the emergency scene.
2. Measure of social factors
• Subjective norm (SN)
○ People who affect me expect me to use interactive RTS.
○ The patient or patient's legal guardian does not refuse to use RTS.
• Expectation confirmation (EC)
○ Execution of the RTS meets my expectations.
○ RTS gives me all the information and tools needed for patients.
○ I generally get the level of service from my expectation from RTS.
3. Measure of organizational factors
• Loyalty incentives (LI)
○ My structure offers incentives for its continued use, such as frequent RTS.
○ I get rewarded for my continued patronage of RTS.
• Job fit (JF)
○ Use of an RTS will have effect on the performance of my job.
○ Use of an RTS can decrease the time needed for my important job responsibilities.
○ Use of an RTS can significantly increase the quality of output of my job.
○ Use of an RTS can increase the effectiveness of performing job tasks.
○ An RTS can increase the quantity of output for same amount of effort.
○ RTS is of help to ambulance services.
• Organizational facilitation (OF)
○ The senior management of this business unit has been helpful in introducing RTS.
○ My boss is very supportive on usage of RTS for my job.
○ The organization has supported the introduction of RTS.
4. Measure of perceived ease of use (PEOU)
• Learning to use RTS will be easy for me.
• I will be skillful in using RTS.
• RTS will be easy to use for me.
5. Measure of perceived usefulness (PU)
• Using RTS will improve my job performance.
• RTS will be useful to my life in general.
• Using the interactive RTS service will enhance my effectiveness on the job.
6. Measure of attitude (ATT) toward a telemetry
• I think positively about RTS.
• I consider it a good RTS.
7. Measure of use intention (UI) of a telemetry
• I have intention to use RTS.
• I will be using more RTS in the future.
Acknowledgments
This study was supported by grant HI10C0051 (A100054) from the Korea Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea.
Disclosure Statement
No competing financial interests exist.
References
- 1.Kim YK, Kim KY, Lee KH, Kim SC, Kim H, Hwang SO, Cha KC. Clinical outcomes on real-time telemetry system in developing emergency medical service system. Telemed J E Health 2010;17:247–253 [DOI] [PubMed] [Google Scholar]
- 2.Scholz KH, von Knobelsdorff G, Ahlersmann D, Keating FK, Jung J, Werner GS, et al. Optimizing systems of care for patients with acute myocardial infarction. STEMI networks, telemetry ECG, and standardized quality improvement with systematic data feedback [in German]. Herz 2008;33:102–109 [DOI] [PubMed] [Google Scholar]
- 3.Davis FD, Bagozzi RP, Warshaw PR. User acceptance of computer technology: A comparison of two theoretical models. Manag Sci 1989;35:982–1003 [Google Scholar]
- 4.Hu PJH, Chau PTK, Sheng ORL. Adoption of telemedicine technology by health care organizations: An exploratory study. J Organ Comput Electron 2002;12:197–222 [Google Scholar]
- 5.Karsh B, Holden RJ. The technology acceptance model: Its past and its future in health care. J Biomed Inform 2010;43:159–172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim DG, Song IK. A study on the effect of healthcare-based IPTV quality on intention to use. J Inform Process Syst 2011;18:185–196 [Google Scholar]
- 7.Kim KY, Kim YK, Lee KH, Yong SJ. Factors affecting the use of a realtime telemetry system in emergency medical services. J Telemed Telecare 2011;17:441–445 [DOI] [PubMed] [Google Scholar]
- 8.Calvin KLO, Karsh B. A systematic review of patient acceptance of consumer health information technology. J Am Med Inform Assoc 2009;16:550–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karsh B, Holden R. New technology implementation in health care. In: Handbook of human factors and ergonomics in patient safety. Mahwah, NJ: Lawrence Erlbaum Associates, 2007:391–408 [Google Scholar]
- 10.Lorenzi NM, Riley RT, Blyth AJ, Southon G, Dixon BJ. Antecedents of the people and organizational aspects of medical informatics: Review of the literature. J Am Med Inform Assoc 1997;4:79–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee SM, Hwang HJ. An analysis on structural relationship between CRS technology acceptance and reuse intention—Targeting employees for domestic airlines. J Korean Soc Aeronaut Sci Aeronaut Oper 2011;19:29–30 [Google Scholar]
- 12.Thompson RL, Higgins CA, Howell JM. Personal computing: Toward a conceptual model of utilization. Manag Inform Syst Q 1991;15:124–143 [Google Scholar]
- 13.Venkatesh V, Davis F. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Health Care Manag Sci 2000;46:186–204 [Google Scholar]
- 14.Bhattacherjee A, Premkumar G. Understanding changes in belief and attitude toward information technology usage: A theoretical model and longitudinal test. Manag Inform Syst Q 2004;28:229–254 [Google Scholar]
- 15.Cacioppo JT, Petty RE. The elaboration likelihood model of persuasion. Adv Consum Res 1984;11:673–675 [Google Scholar]
- 16.Gravel J, Fitzpatrick E, Gouin S, Millar K, Curtis S, Joubert G, Boutis K, Guimont C, Goldman RD, Dubrovsky AS, Porter R, Beer D, Doan Q, Osmond MH. Performance of the Canadian Triage and Acuity Scale for Children: A multicenter database study. Ann Emerg Med 2012;60:27–32 [DOI] [PubMed] [Google Scholar]
- 17.Wood W. Attitude change: Persuasion and social influence. Annu Rev Psychol 2000;51:539–570 [DOI] [PubMed] [Google Scholar]
- 18.Chen Y, Chen M, Chou F, Sun F. Chen P, Tsai K. Chao S. The relationship between quality of life and posttraumatic stress disorder or major depression for fire fighters in Kaohsiung, Taiwan. Qual Life Res 2007;16:1289–1297 [DOI] [PubMed] [Google Scholar]
- 19.Bhattacherjee A. An empirical analysis of the antecedents of electronic commerce service continuance. Decis Support Syst 2001;32:201–214 [Google Scholar]
- 20.Smucker B, Creekmore AM. Adolescents' clothing conformity, awareness, and peer acceptance. Fam Consum Sci Res J 1972;1:92–97 [Google Scholar]
- 21.Lin CS, Wu S, Tsai RJ. Integrating perceived playfulness into expectation—Confirmation model for Web portal context. Inform Manag 2005;42:683–693 [Google Scholar]
- 22.Igbaria M, Parsuraman S. A path analytic study of individual characteristics, computer anxiety and attitudes toward microcomputers. J Manag 1989;15:373–388 [Google Scholar]
- 23.Barclay DW, Higgins CA, Thompson RL. The partial least squares (PLS) approach to causal modeling: Personal computer adaptation and use as an illustration. Technol Stud 1995;2:285–324 [Google Scholar]
- 24.Chin WW, Todd PA. On the use, usefulness, and ease of use of structural equation modeling in MIS research: A note of caution. Manag Inform Syst Q 1995;19:237–246 [Google Scholar]
- 25.Tenenhausa M, Vinzia VE, Chatelinc YM, Laurob C. PLS path modeling. Comput Stat Data Anal 2004;48:159–205 [Google Scholar]