Abstract
Background: Gaining more weight during pregnancy than is recommended by the Institute of Medicine is prevalent and contributes to the development of obesity in women. This article describes the development and use of e-Moms of Rochester (e-Moms Roc), an electronic intervention (e-intervention), to address this health issue in a socioeconomically diverse sample of pregnant women. Materials and Methods: Formative research in the form of intercept interviews, in-depth interviews, and focus groups was conducted to inform the design of the e-intervention. The Web site continuously tracked each participant's use of e-intervention features. Results: An e-intervention, including Web site and mobile phone components, was developed and implemented in a randomized control trial. Formative research informed the design. Participants in all arms accessed blogs, local resources, articles, frequently asked questions, and events. Participants in the intervention arms also accessed the weight gain tracker and diet and physical activity goal-setting tools. Overall, 80% of women logged into the Web site and used a tool or feature at least twice. Among those in the intervention arm, 70% used the weight gain tracker, but only 40% used the diet and physical activity goal-setting tools. Conclusions: To maximize and sustain potential usage of e-Moms Roc over time, the e-intervention included customized reminders, tailored content, and community features such as blogs and resources. Usage was comparable to those in other weight studies with young adults and higher than reported in a published study with pregnant women. This e-intervention specifically designed for pregnant women was used by the majority of women.
Key words: : behavioral health, e-health, education, mobile health
Introduction
Avoiding excessive weight gain during pregnancy, defined as gaining above the Institute of Medicine's gestational weight gain recommendations, has become a priority in obesity prevention.1 Excessive gestational weight gain is a risk factor for postpartum weight retention that contributes to long-term weight gain.1 The prevalence of excessive gestational weight gain is high. In the United States, 38.4% of normal-weight women and 63% and 46.3% of overweight and obese women, respectively, gain more than is recommended.1
Systematic reviews and meta-analyses have examined the effects of interventions on risk of excessive weight gain during pregnancy.2–6 The results are mixed but generally indicate a positive effect on reduced risk. In their review, Gardner et al.2 called for the inclusion of more information on the design, content, and delivery of interventions as a way to explain variation in effectiveness. Morrison et al.7 and others8,9 have recently called for more explicit reporting of the development and implementation of e-health interventions.
Engagement with online or electronic pregnancy interventions has been examined only in a few studies and has been relatively low. Kelders et al.10 found that 64% of participants used their online Healthy Weight Assistant at least once and that half of that group (49%) used the site only once. A study of pregnant women also in The Netherlands found that only 9% used an online intervention program throughout their pregnancies.11
To address the call for more information on the design and implementation of e-health interventions, this article has three aims: (1) to describe the theoretical foundation for the formative research and summarize formative research findings that informed the development of the intervention, (2) to describe the intervention features, and (3) to provide results on participants' engagement with (use of) intervention features.
Materials and Methods
AIM 1: Development of the Intervention—Formative Research
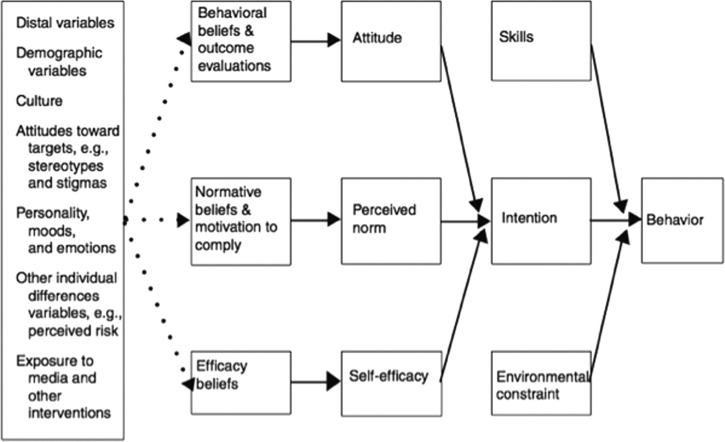
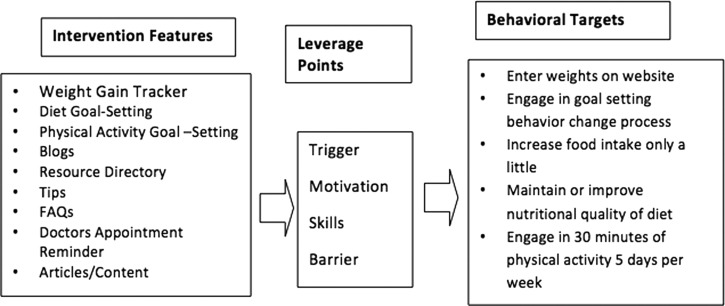
The Integrative Model of Behavioral Prediction of Fishbein and Yzer,12 shown in Figure 1, was the guiding theoretical framework for the formative research and the e-health intervention. We combined this framework with the Behavior Model for Persuasive Design of Fogg13 to link behaviors and their predictors to the electronic features of the intervention (Fig. 2).
Fig. 1.
An integrative model of behavioral prediction. Reprinted with permission from Fishbein and Yzer.12
Fig. 2.
Persuasive design applied to the pregnancy intervention. FAQs, frequently asked questions.
Formative research data collection and analysis
Based on these frameworks, quantitative (media use intercept interviews), qualitative (focus groups), and mixed-methods (media use and intervention feature interviews) research was conducted in 2010 with women 18–35 years of age in Rochester, NY. The goal of this formative research was to inform the development of an electronic intervention (e-intervention) for pregnant women. Methods for the formative research are briefly described here because the focus of this article is on the intervention and its use. Quantitative interview responses were entered into Microsoft (Redmond, WA) Excel. The electronic access and intervention feature interviews and focus groups were audio-recorded. Individual interviews were transcribed, and focus groups were listened to multiple times. Both qualitative interviews and focus groups were coded in matrices using Microsoft Excel and analyzed using the constant comparative method.
Media use intercept interview findings
One hundred ten women participated in 3–5-min intercept interviews at a childcare center or a bridal show about their current media usage (Table 1). Relevant results for the design of the intervention are as follows: 96% owned a cell phone, 94% texted, and 86% texted multiple times a day. Related to cell phone plans and types, 87% had a contract cell phone plan, 22% owned a smartphone, and 39% accessed the Internet from their phones. Related to computer and Internet usage, 98% used a computer at work, home, or somewhere else, and 89% accessed the Internet from home, with 72% of those connecting to the Internet from home 7 days a week. Access to and use of electronic communication media were high.
Table 1.
Sociodemographic Characteristics of Participants in the Formative Research and Randomized Trial
| FORMATIVE RESEARCHa | ||||
|---|---|---|---|---|
| SHORT INTERVIEWS (N=110) | IN-DEPTH INTERVIEWS (N=24) | FOCUS GROUPS (N=26) | RANDOMIZED TRIAL (N=1,689) | |
| Race/ethnicity | ||||
| White | 73 (66) | 15 (68) | 14 (56) | 1,054 (62) |
| Black | 21 (19) | 7 (32) | 11 (44) | 395 (23) |
| Other | 16 (15) | 240 (14) | ||
| Hispanic | 14 (13) | 2 (8) | 3 (12) | 212 (13) |
| BMI | ||||
| Normal weight | 0 | 18 (75) | 14 (54) | 901 (53) |
| Overweight/obese | 0 | 6 (25) | 12 (46) | 788 (47) |
| Unknown | 110 (100) | |||
| Parity | ||||
| Having 1st child | 57 (52) | 9 (38) | 16 (62) | |
| Having 2nd child or more | 53 (48) | 15 (62) | 10 (38) | |
| Lower income | ||||
| No | 14 (58) | 11 (42) | 955 (57) | |
| Yes | 10 (42) | 15 (58) | 734 (43) | |
| Unknown | 110 (100) | |||
| Age (years) | ||||
| 18–25 | 56 (51) | 9 (38) | 526 (31) | |
| 26–35 | 48 (44) | 15 (62) | 1,163 (69) | |
| Unknown | 6 (5) | 26 (100) | ||
Data are number (%).
Observed race, ethnicity, and body mass index (BMI), not self-reported.
Media use and feature preference interview findings
We conducted 25 mixed-method interviews asking pregnant women about their preferences for various potential intervention features (Table 1). Informed by these interviews, we incorporated the following features: healthy tips, articles, frequently asked questions (FAQs), a prenatal vitamin reminder, a water reminder, weight gain tracker, physical activity goal-setting tool, diet goal-setting tool, a local resources section, and blogs. In addition, several critical themes related to flexibility, variability, and personalization emerged from the interviews. For reminders, women wanted to select the frequency, time of delivery, and mode of delivery. In addition, they wanted to be able to opt out of receiving any reminders.
Focus groups: health-related attitudes, beliefs, and practices during pregnancy findings
We conducted nine focus groups with high- (n=4 groups) and low- (n=5 groups) income pregnant women (Table 1). The most relevant results from these groups were major differences between lower-income and higher-income women as described by Paul et al.14 Based on these results, a wide variety of content was included on the Web site to appeal to the diverse study population (Table 1). The barriers, strategies, and topics of interest that emerged from the focus groups were integrated into the diet and physical activity goal-setting tools, the resources and the articles, FAQs, and tips on the Web site.
Application of theoretical framework to intervention development
Figure 2 shows the target behaviors, proximal leverage points for promoting behavior change, and the main features of the pregnancy e-intervention that were decided upon after the formative research. Each intervention feature operates through specific leverage points to move women closer to the five behavioral targets. Some leverage points may be more important than others for achieving change in different behaviors. For instance, the Doctor Appointment Reminders are an important trigger for getting women to enter weights on the Web site. We design the e-intervention features and tools to encourage participants to reach the behavioral targets and in doing so to prevent excessive gestational weight gain.
Pilot test of intervention features
In February 2011, 21 pregnant women participated in a 4-week pilot study of e-Moms of Rochester (e-Moms Roc). Participants were recruited from a large hospital-based obstetrics clinic and a large private practice.
Overall, feedback on the Web site was positive. Most women rated the site highly and found it helpful. Only 1 subject did not rate it highly, and a few participants thought more information should be added. Participants liked the local focus of the Web site but consistently requested that we add reminders to use features. In addition, participants felt the need for of an introduction to Web site features.
Based on this feedback, three major changes were made; all were aimed at increasing the number of women who used e-Moms Roc. The first change was handing participants a timeline and a log-in screen card at the time of consent. Second, we added weekly e-mail reminders to visit the site. Each e-mail reminder highlighted Web site features as well as new articles, topics, resources, or blogs that had been added. Third, we added a “Help—What is this?” button so that a participant could read an overview of each Web site feature.
Form Collective, a local design and Web development firm, developed all Web site features to operate on desk and laptop computers, tablets, and smartphones. It was optimized for Chrome, Safari, and Firefox browsers. M.L.G., K.H.U., and C.M.O. described and detailed each Web site feature for Form Collective, who modified them following input from one of their user-centered design experts.
AIM 2: The e-Moms Roc Intervention and its Implementation
Upon recruitment and consent to participate in the randomized control trial that is described elsewhere,15,16 the Web site randomized participants to one of three arms: (1) intervention during pregnancy and after delivery, (2) intervention only during pregnancy and control after delivery, and (3) control both during pregnancy and after delivery. Once randomized, participants received an e-mail message that included a temporary password and described the e-intervention features particular to her assigned arm.
At first log-in, a participant was asked to create a personal password and a screen name and to upload an avatar. The site offered guidance about protecting privacy in creating a screen name and an avatar. The site then asked each participant to confirm the contact information on file as well as her estimated delivery date. The last phase of the first log-in experience allowed the participant to set her communication preferences for the frequency and mode of delivery for each of the reminders for which she was eligible. The site also asked the participant to select a time of day to receive reminders.
Web site content available to a participant was restricted by assigned treatment arm, blinding participants themselves to arm assignment. The intervention arms featured the following: (1) weight gain tracker, (2) diet goal-setting tool, and (3) physical activity goal-setting tool. All other intervention features, including the interactive and personalized participant homepage or dashboard, were available to both intervention and control arms, but the content was restricted by arm. Control content included maternal and infant health information and strategies, as well as nutrition, physical activity, and weight gain guidelines as information. For example, control content included information about smoking cessation, foods to avoid during pregnancy, physical activity recommendations during pregnancy, and weight gain guidelines by body mass index group. Any content that provided strategies, self-monitoring, or logistical tips related to diet, physical activity, and weight, however, was restricted to the intervention arm. M.L.G. coded all content by arm, and this determined who could view it.
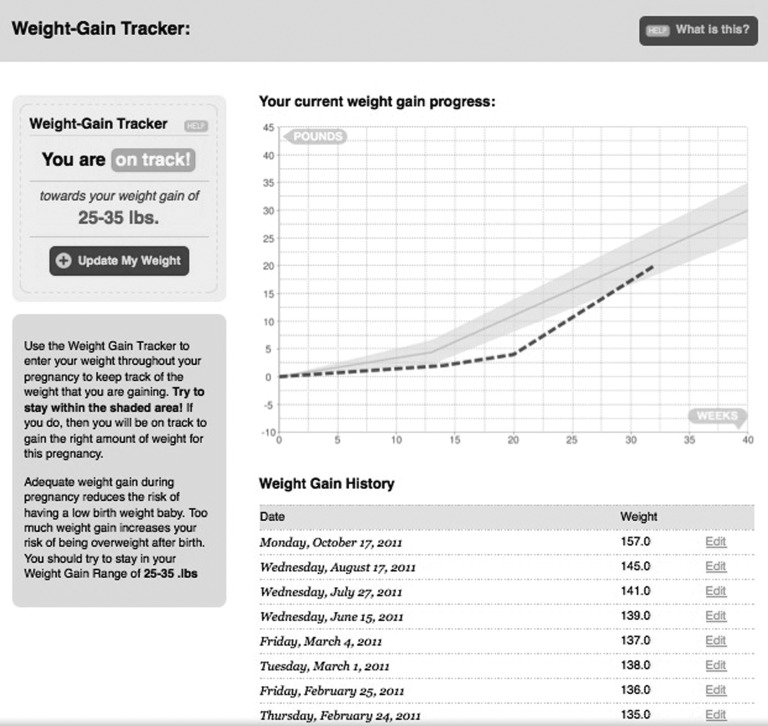
Weight gain tracker
The weight gain tracker used the prepregnancy body mass index collected at recruitment to determine a woman's weight gain recommendation1 and the prepregnancy weight to provide the starting point on the tracking graph. Figure 3 displays an example screenshot of the weight gain tracker, displaying the weight gain across 40 weeks of pregnancy.
Fig. 3.
Weight gain tracker.
Women could enter weights via text message or using a Web form. Each weight was plotted on the woman's personal graph throughout pregnancy. If a participant gained within the range, the bar below the recommended weight gain range stated that she was “on track.” If a woman was below or above the range for her stage, the bar stated that she was “off track.” M.L.G. monitored participants for inadequate gestational weight gain according to the protocol approved by the study's external data safety and monitoring board.
Diet goal-setting tool
We developed the diet and physical activity goal-setting tools based on diabetes self-management goal-setting tools by Glasgow et al.17 The diet goal-setting tool emphasizes assessment and strategies for achieving a dietary goal. Below are the steps included in the diet goal-setting tool, and an example is shown in Table 2:
Table 2.
Example of Diet-Goal Setting: Issue Area, Goal, Barriers, Content, Strategies, and Self-Monitoring
| ISSUE AREA | GOAL AREA | BARRIERS | RELATED CONTENT | STRATEGIES | BEHAVIOR TO MONITOR | SELF-MONITORING |
|---|---|---|---|---|---|---|
| Eating high-fat foods | Decrease the number of times/week that you eat high-fat processed meats like salami, bologna, and hot dogs | • Not the person who shops or prepares food • Local food environment • Food preferences • Social influences (partner/family) • Cost |
• Formation of food preferences • Effects of high-fat and high-sodium diet • Nutrition comparison between leaner processed meats and higher-fat meats • Impact of food availability |
• Try this instead of that • Locations and descriptions of low-fat sandwich options • Use low-fat processed meats rather than high-fat processed meats |
• Set maximum number of times per week that you eat high-fat processed meats like salami, bologna, and hot dogs | • Web or printout—check off from list which high-fat processed meats you ate and fill in number of times eaten per week/day? • For printout users, have blank box next to each meat to tally number of times eaten. Weekly prompt on dashboard to enter total number of times of all high-fat process meats eaten • Text or e-mail or dashboard—respond to prompt, “How many times did you eat high-fat processed meats this week/day?” |
1. The participant completed a 23-item dietary assessment. The dietary assessment included questions from the Rapid Eating Assessment for Participants—Shortened Version18 and from the Eating Stimulus Index for emotional eating and dietary restraint questions.19
2. The Web site calculated “issue area” scores from the assessment items to identify 10 potential issue areas that a participant could work on: Eating out frequently; Eating high-fat foods; Eating and drinking too much; Not eating enough whole grains; Not eating enough fruit; Not eating enough vegetables; Not eating enough calcium-rich foods; Eating high sugar foods; Eating low-nutrient density foods; and Emotional eating.
3. The intervention site displayed the issue areas that need attention (score of >2.5) and do not need attention. A participant then selected one issue area on which to focus.
4. Within that issue area, multiple prewritten goals were displayed, and the participant then selected a goal on which to work.
5. The Web site displayed barriers and strategies for the selected goal. These were based on the formative research. A participant had the option to add barriers or strategies.
6. The Web site displayed suggestions for setting the frequency for a goal and timeline for achieving it and allowed the participant to set an achievable number or proportion for the goal and timeline (see Behavior to Monitor in Table 2).
7. Based on the goal area selected, the Web site displayed different self-monitoring options, and participants selected their self-monitoring option.
8. The Web site displayed a list of potential rewards for achieving goals, and participants selected what reward they would like if/when they achieved their goal. Participants could also add a custom reward.
9. The Web site displayed an action plan for the participant to review and directed participants to content related to their goal.
Physical activity goal-setting tool
The physical activity goal-setting tool emphasized improving awareness about the safety of exercise during pregnancy because previous research found it to be a barrier to physical activity during pregnancy.20–22 In addition, the tool focused on assessing barriers to being active and identifying strategies specific to those barriers. Below are the steps that were part of the physical activity goal-setting feature:
1. The site displayed the National Institute of Diabetes and Digestive and Kidney Diseases' recommendations for physical activity during pregnancy.23
2. The tool asked participants whether or not they had been told by their prenatal care provider that they should avoid physical activity and/or have contraindications for physical activity. If a woman had contraindications, this information was reported back to her, and she was advised/reminded to avoid physical activity during pregnancy. If she had no contraindications, she assessed whether she was sedentary before getting pregnant using a validated question from the Pregnancy Risk Assessment Monitoring System. If a participant was not sedentary, she was asked in what types of activity she was currently engaged.
3. If a woman was sedentary, then the site recommended walking, swimming, cycling, and aerobics for 90–120 min per week. If a woman was not sedentary but wasn't meeting the recommendation, then the site recommended total activity of 150 min per week. If a woman was adequately active, she was congratulated and encouraged to self-monitor and continue physical activity for at least 150 min per week.
4. We assessed potential barriers to physical activity and displayed potential strategies to address them. Strategies were prepopulated based on our formative research and the research literature. Participants selected which strategies to apply and had the option of adding custom barriers and strategies.
5. Participants finalized their action plan by selecting the activities that will make up the 120 or 150 min of physical activity per week. Participants were shown a subset of appropriate activities from the Paffenbarger Physical Activity Questionnaire.24 Participants indicated how many weeks they would work on the goal.
6. The site displayed a list of potential rewards, and participants selected a reward. Participants could also add their own rewards.
7. The site displayed an action plan for the participant to review. Participants were directed to content related to their goal.
Blogs
Women conveyed an interest in discussion forums and blogging in the pregnancy interviews and focus groups. Participants could generate blogs and post comments to the Web site after M.L.G. approved blogs. As part of the blog entry approval process, the arm and key words associated with the post were coded. The Web site used the key words to display related blog entries, as search terms and as blog categories. Participants could also “like” blog posts.
Resources
e-Moms Roc's local focus was a unique feature of the participant Web site. The resource section of the site included local and national listings of services, Web sites, and information to provide logistical or informational support to pregnant women. The study team seeded the Web site with a variety of resources in over 20 categories, and participants were able to “like” and comment on each resource. Participants could also add resources with moderator approval.
Articles and FAQs
We wrote and compiled articles and FAQs for several hundred topics. Some of the articles and FAQs were informational, and some were focused on strategies to overcome barriers identified in the formative work. M.L.G. tagged each content page with key words and a category; this information was pushed to participants based on their goals, reading of other articles, FAQs, or blogs. Participants were able to comment on content articles and could “like” both articles and FAQs. New content pages are added throughout the study. We published new content of any type to the live feed on the participant's homepage or dashboard as it was added to the Web site.
Tips
We made over 1,500 pregnancy-related tips available for use on the Web site. They were broken down into two categories: knowledge/educational tips and practical/logistical tips. The site showed participants a new tip each time they logged onto the site and could click through tips at each log-on. M.L.G. also sent participants two or three tips as part of the weekly e-mail message.
Events
This section of the Web site offered a personal calendar for pregnancy. Participants could enter any type of event and have a reminder sent for the event based on the communication preferences that the participant set for event reminders. Events that participants entered included doctor's appointments, birthing classes, and hair appointments. For doctor's appointments, the site provided a checkbox that a participant could select, and, if selected by a participant in the intervention arm, she was prompted to enter her weight at the time of her appointment. The integration of this feature with the weight gain tracker aimed to promote weight tracking coordinated with doctor's appointments so that even participants without scales could monitor weight gain during pregnancy.
Achievements
We created a “virtual badge” section to encourage engagement on the site. Participants could earn virtual badges for using the weight gain tracker, goal-setting tools, setting event reminders, and reading articles or FAQs. The site made earned badges visible to the participant on her achievements page.
AIM 3: Participants’ Use of Or Engagement with Intervention Features
Data collection methods
For data collection on the use of or engagement with the intervention, the Web site continuously (and automatically) monitored each participant's online activities from study consent to delivery date, placing a timestamp on each Web site activity. All participants who were randomized, regardless of how long a participant remained in the study, are included in the results. Use of each feature is reported as proportions on dichotomous variables indicating whether or not a participant ever used a feature. Medians, 25th and 75th percentiles, means, and range for use of each feature were also calculated.
Results on Use of Intervention Features
Data for the 1,689 randomized participants are presented in this article: 1,126 in the pregnancy intervention arms and 563 in the control arm. Sociodemographic characteristics of this sample are shown in Table 1. Overall, 1,444 (85%) participants logged into the Web site during pregnancy (Table 3). Of those subjects who logged-in once, 1,357 (80.3%) logged-in at least one more time. Blogs were the most popular feature that was available across all arms. Participants posted 694 blogs entries, which generated over 3,000 comments (data not shown). Approximately 40% of participants viewed at least one article or resource.
Table 3.
Engagement in Pregnancy Electronic Intervention Across All Arms of the Randomized Trial
| WEB SITE ACTIVITY | N (% OUT OF 1,689 RANDOMIZED) | MEDIAN (25TH, 75TH PERCENTILE) | MEAN (MINIMUM, MAXIMUM) |
|---|---|---|---|
| Log-in | 1,444 (85%) | 8 (2, 19) | 14.9 (0, 388) |
| Article view | 766 (45%) | 0 (0, 4) | 5.1 (0, 152) |
| Blog view | 874 (52%) | 1 (0, 8) | 19.9 (0, 873) |
| Blog comment | 350 (21%) | 0 (0, 0) | 2.1 (0, 162) |
| Article comment | 119 (7%) | 0 (0, 0) | 0.17 (0, 16) |
| FAQs view | 554 (33%) | 0 (0, 2) | 3.1 (0, 134) |
| Resource view | 637 (38%) | 0 (0, 2) | 3.9 (0, 146) |
FAQs, frequently asked questions.
The weight gain tracker was the most popular feature among participants in the intervention arms and was used at least once by 787 (70%) participants (Table 4). In contrast, only 435 (39%) participants set either a diet or physical activity goal. There was considerable variability within the sample for how frequently the Web site features were used (Tables 3 and 4).
Table 4.
Engagement in Pregnancy Electronic Intervention Across Two Intervention Arms of the Randomized Trial
| WEB SITE ACTIVITY | N (% OUT OF 1,126 RANDOMIZED) | MEDIAN (25TH, 75TH PERCENTILE) | MEAN (MINIMUM, MAXIMUM) |
|---|---|---|---|
| Log-in | 957 (85%) | 9 (2, 20) | 16.1 (0, 388) |
| Weight gain entry | 787 (70%) | 3 (0, 9) | 6.2 (0, 190) |
| Set diet goal | 326 (29%) | 0 (0, 1) | 0.52 (0, 11) |
| Diet goal monitoring | 338 (30%) | 0 (0, 1) | 1.2 (0, 29) |
| Set PA goal | 327 (29%) | 0 (0, 1) | 1.1 (0, 30) |
| PA goal monitoring | 253 (22%) | 0 (0, 0) | 1.7 (0, 87) |
| Set diet or PA goal | 435 (39%) | 0 (0, 2) | 1.6 (0, 41) |
| Diet or PA monitoring | 392 (35%) | 0 (0, 1) | 2.8 (0, 96) |
PA, physical activity.
Discussion
Theory and formative research were used to design e-Moms Roc, an e-intervention to prevent excessive gestational weight gain in a diverse sample of pregnant women. Intervention features were aimed at influencing behavioral targets and included weight gain tracking, diet goal-setting, and physical activity goal-setting. The content and features promoted norms, attitudes, and efficacy related to the behavioral targets and built skills needed to address barriers. The local resources and strategies addressed building skills and environmental constraints. The blogs aimed to build social support and influence normative and efficacy beliefs for the behavioral targets. Formative research indicated that blogs were likely to be popular, and the engagement data support this contention. The success of the blogs exemplifies the importance of formative work in the design of the intervention.
The results on use of the e-intervention are comparable to or better than those for other online interventions. As in other online intervention studies, there is considerable variability within our sample for how frequently the Web site was used.25–29 Little is known about the most appropriate mix of features and their level of use as predictors of the effectiveness of online interventions, so there is much to learn from studies such as this one. Additional analyses related to patterns of engagement in the pregnancy intervention for appropriate gestational weight gain are underway. High engagement, as described in this article, is a promising sign for examining the effectiveness of the e-interventions for pregnant women.
Acknowledgments
Funding for this study was provided by the EARLY Trials, National Heart, Lung, and Blood Institute, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant HL096760). In addition, the authors wish to acknowledge the following individuals for their contributions to the study: Christian Schimke and Joe Tunis of Form Collective for the design, development, and maintenance of the participant Web site; Jeremy Larkin, formerly of Form Collective, for the development of the participant Web site; I. Diana Fernandez, Susan Groth, and Jennifer Reschke of University of Rochester for the implementation of the randomized control trial; and Kristine DiBitetto, University of Rochester, for recruitment of participants for the pilot study.
Disclosure Statement
No competing financial interests exist.
References
- 1.Institute of Medicine, National Research Council. Weight gain during pregnancy: Reexamining the guidelines. Washington, DC: The National Academies Press, 2009 [PubMed] [Google Scholar]
- 2.Gardner B, Wardle J, Poston L, Croker H. Changing diet and physical activity to reduce gestational weight gain: A meta-analysis. Obes Rev 2011;12:e602–e620 [DOI] [PubMed] [Google Scholar]
- 3.Streuling I, Beyerlein A, von Kries R. Can gestational weight gain be modified by increasing physical activity and diet counseling? A meta-analysis of interventional trials. Am J Clin Nutr 2010;92:678–687 [DOI] [PubMed] [Google Scholar]
- 4.Skouteris H, Hartley-Clark L, McCabe M, et al. . Preventing excessive gestational weight gain: A systematic review of interventions. Obes Rev 2010;11:757–768 [DOI] [PubMed] [Google Scholar]
- 5.Tanentspaf I, Heitmann BL, Adegboye ARA. Systematic review of clinical trials on dietary interventions to prevent excessive weight gain during pregnancy among normal weight, overweight and obese women. BMC Pregnancy Childbirth 2011;11:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thangaratinam S, Rogozinska E, Jolly K, et al. . Effects of intervention in pregnancy on maternal weight and obstetric outcomes: Meta-analysis of randomised evidence. BMJ 2012;344:e208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrison LG, Yardley L, Powell J, Michie S. What design features are used in effective e-health interventions? A review using techniques from critical interpretive synthesis. Telemed J E Health 2012;18:137–144 [DOI] [PubMed] [Google Scholar]
- 8.Michie S, Fixsen D, Grimshaw JM, Eccles MP. Specifying and reporting complex behavior change interventions. The need for a scientific method. Implement Sci 2009;4:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kraft P, Yardley L. Current issues and new directions in psychology and health: What is the future of digital interventions for health behaviour change? Psychol Health 2009;24:615–618 [DOI] [PubMed] [Google Scholar]
- 10.Kelders SM, Van Gemert-Pijnen JE, Werkman A, et al. . Effectiveness of a web-based intervention aimed at healthy dietary and physical activity behavior: A randomized controlled trial about users and usage. J Med Internet Res 2011;13:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Sutphen M, Milder IE, Bemelmans WJ. Usage of an online healthy lifestyle program by pregnant women attending midwifery practices in Amsterdam. Prev Med 2008;46:552–557 [DOI] [PubMed] [Google Scholar]
- 12.Fishbein M, Yzer MC. Using theory to design effective health behavior interventions. Communication Theory 2003;13:164–183 [Google Scholar]
- 13.Fogg B. Persuasive Technology. Using computers to change what we think and do. San Francisco: Morgan Kaufmann, 2002 [Google Scholar]
- 14.Paul KH, Graham ML, Olson CM. The web of risk factors for excessive gestational weight gain in low income women. Matern Child Health J 2013;17:344–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.e-Moms of Rochester Healthy Pregnancy Study. Available at www.emomsroc.org (last accessed January17, 2014)
- 16.Lytle L, Svetkey LP, Patrick K, et al. . The EARLY trials: A consortium of studies targeting weight control in young adults. Transl Behav Med 2014. Epub January28. doi: 10.1007/s13142-014-0252-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glasgow RE, Christiansen S, Smith KS, et al. . Development and implementation of an integrated, multi-modality, user-centered interactive dietary change program. Health Educ Res 2008;24:461–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Segal-Isaacson CJ, Wylie-Rosett J, Gans KM. Validation of a short dietary assessment questionnaire: The Rapid Eating and Activity Assessment for Participants Short Version (REAP-S). Diabetes Educ 2004;30:774–781 [DOI] [PubMed] [Google Scholar]
- 19.Cahill JM, Freeland-Graves JH, Shah BS, et al. . Development and validation of the eating stimulus index in low-income, minority women in early postpartum. J Am Diet Assoc 2009;109:1593–1598 [DOI] [PubMed] [Google Scholar]
- 20.Cioffi J, Schmied V, Dahlen H, et al. . Physical activity in pregnancy: Women's perceptions, practices, and influencing factors. J Midwifery Womens Health 2010;55:455–461 [DOI] [PubMed] [Google Scholar]
- 21.Evenson KR, Bradley CB. Beliefs about exercise and physical activity among pregnant women. Patient Educ Couns 2010;79:124–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evenson KR, Moos M-K, Carrier K, Siega-Riz AM. Perceived barriers to physical activity among pregnant women. Matern Child Health J 2008;13:364–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Weight-control Information Network (WIN). Fit for two. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases, 2009:12–15 [Google Scholar]
- 24.Paffenbarger RS, Blair SN, Lee IM, Hyde RT. Measurement of physical activity to assess health effects in free-living populations. Med Sci Sports Exerc 1993;25:60–70 [DOI] [PubMed] [Google Scholar]
- 25.Couper M, Alexander G, Zhang N, et al. . Engagement and retention: Measuring breadth and depth of participant use of an online intervention. J Med Internet Res 2010;12:e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bennett GG, Glasgow RE. The delivery of public health interventions via the Internet: actualizing their potential. Annu Rev Public Health 2009;30:273–292 [DOI] [PubMed] [Google Scholar]
- 27.Glasgow RE, Christiansen S, Kurz D, et al. . Engagement in a diabetes self-management website: Usage patterns and generalizability of program use. J Med Internet Res 2011;13:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glasgow RE, Nelson CC, Kearney KA, et al. . Reach, engagement, and retention in an Internet-based weight loss program in a multi-site randomized controlled trial. J Med Internet Res 2007;9:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hwang K, Ning J, Trickey A, Sciamanna C. Website usage and weight loss in a free commercial online weight loss program: Retrospective cohort study. J Med Internet Res 2013;15:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]